Abstract
Post-acute care, encompassing long-term care hospitals, home health, inpatient rehabilitation, and skilled nursing facilities, is increasingly employed as an integral part of management for more complicated patients, particularly as hospitals seek to maintain costs and decrease length of stay. Skilled nursing facilities (SNFs) in particular are progressively utilized for patients with complex medical processes, including today's growing population of older hospitalized heart failure (HF) patients who pose a prominent challenge due to their high risks of mortality, 30-day readmissions, and substantial aggregate cost burden to the healthcare system. Publications to date have largely grouped post-hospitalized HF patients together when reporting demographic or outcome data, without differentiating those at SNFs from those at traditional nursing homes or other post-acute care settings. SNF patients suffer distinctive vulnerabilities and needs, and understanding these distinctions has implications for determining goals of care. In this review we evaluate HF patients referred to SNFs, and discuss the characteristics, outcomes, and management challenges associated with this particular population.
Keywords: Heart failure, Skilled nursing facility, Nursing home, Post-acute care, Long-term care
Introduction
The last two decades have witnessed an impressive increase in post-acute care provision [1], with marked rise in the utilization of skilled nursing facility (SNF) care [2]. Changes to Medicare payment policies as well as implementation of the Readmissions Reduction Program under the Affordable Care Act (which imposes financial penalties on hospital based on 30-day readmissions) have contributed to this expansion. In 2015, 2592 eligible hospitals will face financial penalties, resulting in a combined loss of $420 million [3]. Heart failure (HF) is a major driver of readmissions [4] and related penalties [5], and as a consequence, hospitals have become highly incentivized to prioritize HF quality and performance improvements [6•]. Discharge to SNFs for select HF patients with greater disease severity and comorbidity is one strategy many hospitals use to reduce acute management length of stay and hospital costs, and to thereby improve their ratings on quality of care and performance metrics. Nonetheless, the management of HF patients in SNFs also involves downstream complexities that can detract from many assumed benefits.
Publications tend to report collectively on HF patients in the various post-acute healthcare settings of subacute/inpatient rehabilitation and home health programs, and/or traditional nursing homes or long-term care settings (i.e. nursing homes with custodial care) [7]. Skilled nursing facilities are distinct relative to other long-term care options as they provide a specified level of skilled nursing and/or skilled rehabilitation services. In concept, SNFs provide a suitable level of care to discharge sicker patients more quickly [8]. Ironically, SNFs often remain hindered by limitations that can ultimately exacerbate aggregate costs and morbidity of referred patients. Notably, impending legislative reforms will soon be linking SNF payments to outcome and quality [9•], so improving care of the post-hospitalized HF patient has been a substantial priority of SNF providers. This review considers the characteristics, outcomes, and management issues distinctive to the subset of HF patients specifically in the SNF setting.
Quality Imperative
Approximately 40 % of hospitalized Medicare beneficiaries are discharged to post-acute settings [10] and about 20 % enter a setting that provides skilled services [11]. In 2013, almost 1.7 million beneficiaries used SNF services at least once, costing the United States $28.7 billion dollars [12]. As the current Medicare payment system for SNFs does not differentiate between high- and low-quality SNF providers, the Center for Medicaid and Medicare Services (CMS) issued a rule adopting a new Value-Based Purchasing Program, under which payments will be made to SNFs based on performance currently scheduled to begin in 2019 [13]. The Skilled Nursing Facility 30-Day All-Cause Readmission Measure, an estimate of all-cause hospital readmissions for SNF beneficiaries within 30 days of discharge from their prior proximal short-stay acute hospital discharge, is a proposed measure to be included in the payment program [13]. Pressure is mounting for SNFs to demonstrate quality improvement as well as maintain preferred partnerships with local hospitals via competitive outcomes and low readmission rates. Heart failure, as a reportable diagnosis, is a key focus for quality improvement in SNFs, and recent release of guidelines on HF management in SNFs attests to the interest of this subject among the medical community [14•, 15].
Heart Failure Trends, Epidemiology, and Burden in SNFs
As medical care has evolved over the last decade, HF hospitalizations, readmissions, and survival have progressively improved, even among elderly HF patients [1, 16–18]. In contrast to the increase in HF hospitalizations between 1979 and 2004 [19], national HF hospitalization rates decreased 19 % in patients over age 65 years and 10 % for those over age 85 between 2000 and 2010 [20]. Similarly, HF readmission rates for Medicare patients have decreased from 23.4 % in 2010 to 21.9 % in 2013 [21]. However, the mortality rate among hospitalized HF Medicare patients has not significantly changed (11.8 % in 2010 compared to 12.0 % in 2013) [21], and earlier studies that showed a decrease in in-hospital mortality rates noted an associated increase in post-discharge mortality (from discharge to the 30th day after admission) [22].
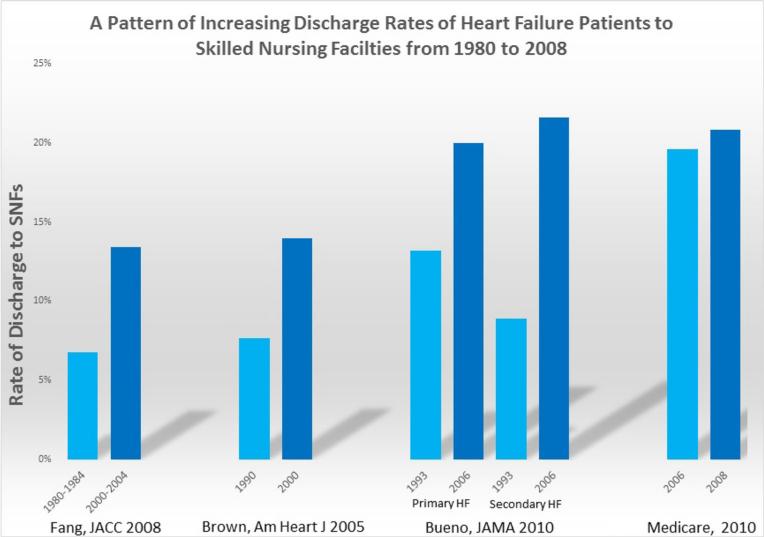
Hospitals are variable in their use of SNFs for HF patients; some refer twice as many patients to SNFs as others [23]. Overall, however, utilization of SNF care for HF patients has steadily increased in recent decades (Fig. 1). From 1980 to 1984, only 6.8 % of hospitalized HF patients were discharged to SNFs [19], but more recently, the median rate of discharge to SNFs for hospitalized HF Medicare beneficiaries aged ≥65 was 20.8 % in 2008 [23]. Moreover, hospitalized HF patients aged 85 years or older were found to be 3.8 times more likely to be discharged to SNFs than younger patients [24]. As the population of vulnerable, elderly, high risk, hospitalized HF patients expands, such reliance on SNFs is expected to expand.
Fig. 1.
Studies demonstrating increasing rates of hospital discharge rates to skilled nursing facilities for heart failure patients over the last three decades. Numbers are rounded to the nearest percentage. From 1980 to 1984, 6.8 % of hospitalized HF patients were discharged to SNFs compared to 13.4 % in 2000 to 2004 (Fang et al.) [19]. In 1990, 7.7 % of elderly hospitalized Medicare HF patients were discharged to SNFs compared to 14.0 % in 2000 (Brown et al.) [24]. In 1993, 13.2 % of hospitalized Medicare patients with a primary diagnosis of HF were discharged to a SNF compared to 19.6 % in 2006; percent discharge rates for the same time period for patients with a secondary diagnosis of HF were 8.9 and 21.6 %, respectively, (Bueno et al.) [4]. The median rate of discharge to SNFs for Medicare beneficiaries aged ≥65 increased from 19.6 % in 2006 to 20.8 % in 2008 (Centers for Medicare and Medicaid Services) [23]
The prevalence of HF specifically among SNF residents has not been well described, but estimates suggest it is upwards of 25 % [14•]. These estimates are substantially above the 6–10 % HF prevalence in the general population aged 65 or older [25], as well as the 12 % HF prevalence among those 80 and older [26]. In 2004, the National Nursing Home survey estimated 4.3 % of long-term SNF residents had a primary diagnosis of HF when admitted to their facility [27]. Data derived from the National Hospital Discharge Survey from 2005 to 2006 showed the prevalence of HF among NH patients requiring hospitalization to be near 30 % [28]. The Medicare Payment Advisory Committee (MEDPAC) published a report showing HF prevalence among 1,836,189 SNF stays was 25 % in 2012 [29]. Many SNF residents with HF are admitted for reasons other than complications of cardiovascular disease, but the prevalence of HF as a secondary diagnosis has not been well defined.
The HF population in SNFs is heterogeneous. The recent AHA/ACC guidelines on HF management in SNFs describe three subsets of patients [14•]. (1) The “long-term care” subset of HF patients, not to be confused with LTC patients in traditional nursing homes offering custodial care, is characterized by SNF HF residents with frailty and cognitive or medical dependency who are expected to remain in long-term care until death, yet require skilled services, meaning care provided by registered nurses, physicians, or physical and/or occupational therapists daily. While not directly comparable to the SNF setting, estimates of the incidence of HF in LTC have been reported to be 20 % [30], or as high as 45 % if HF assessment was done by a geriatrician [31]. (2) The “rehabilitation group” (those discharged after an acute event requiring ongoing skilled medical or surgical needs but expected to be discharged to the community) typically needs titration of medical therapy, additional diuresis until euvolemic, continued monitoring of labs, patient education, and/or rehabilitation after prolonged hospitalization. (3) The “uncertain prognosis group” consists of patients who were recently discharged from the hospital but with issues of frailty, advanced disease, and/or multiple morbidities that complicate their care. They may be discharged after one or many acute hospitalizations with ongoing skilled needs, and while improvement and recovery in the SNF is possible, their clinical trajectory is less certain and will vary depending on each individual's day-to-day progress (or lack thereof). These patients are at the highest risk for both mortality and rehospitalization, and will likely contribute largely to the increasing SNF discharge trends. The burden of these patients in the SNF setting is not precisely known, and data to better define SNF HF patients is needed.
Distinctive Patterns of SNF HF Patients
In order to qualify for admission to a SNF, usually defined as a Medicare-certified post-hospital care unit or long-term care facility with at least 16 hours per day of licensed nursing care daily [14•], patients need to have been hospitalized for at least 3 days and require daily rehabilitation services or skilled services offered by either registered nurses, licensed practical and/or vocational nurses, or physicians [32]. By this selection process, SNF HF patients have clinical needs distinct from non-hospitalized HF patients as well as from hospitalized HF patients who can be discharged home. While understanding the distinctive patterns of SNF HF patients has implications for outcomes and management strategies, few studies have delineated the differences that characterize them.
Patients selected for SNF admission after a HF hospitalization are more likely to be older, suffer from more comorbidities, and have greater clinical complexity [33, 34••]. In a large study using a Medicare database of patients discharged after their first cardiac event, 25 % of 1,188,711 HF patients were discharged to a SNF and distinguished by longer and more costly hospital stays; the presence of greater than two comorbidities, being female, and being older increased this risk, with age greater than 80 years increasing the likelihood for SNF discharge five- to sevenfold [33]. An evaluation of 15,459 Medicare beneficiaries found that the 24 % of hospitalized HF patients discharged to SNFs had significantly longer lengths of stay (6 vs 5 days); advanced age (84 vs 79 years); higher proportions of females (65.5 vs 52 %); and a variety of comorbidities including depression (14.8 vs 7.7 %), stroke (19.9 vs 13.9 %), anemia (23 vs 16.1 %), atrial fibrillation (37.2 vs 34 %), non-insulin-dependent diabetes (16.4 vs 15.4 %), and chronic renal insufficiency (20.1 vs 18.1 %) [34••]. Patients with HF discharged to SNFs in this study were less likely to be taking guideline-directed medical therapy including angiotensin-converting enzyme inhibitor (ACE inhibitor)/angiotensin receptor blocker therapy (ARB) (24.5 vs 32 %) or beta-blockers (26.9 vs 35.2 % [34••], although in general SNF patients tend to take multiple other medications [14•], provoking risks associated with polypharmacy.
Functional and cognitive impairments are commonly seen in older patients with HF [35], and those selected for SNF admission after hospitalization often have additional functional limitations compounded by frailty. Acute illness with ensuing hospitalization can lead to a dynamic course of declining physical function, and in general, only 30 % of older patients discharged from the hospital with a new disability will return to their prior level of functioning [36]. Concomitant frailty, defined as a state of individual vulnerability due to reduced physiological reserve that predisposes a person to poor health outcomes when challenged by a health stressor [37], can further impact potential for rehabilitation and prognosis for community discharge.
Most old HF patients admitted to SNFs after hospitalization are frail. While the effect of frailty on outcomes among HF patients in SNFs has not been explicitly studied, it is clear that frailty confounds patient assessment and tolerance of medical therapies, and has been significantly associated with rehospitalization and mortality among HF patients at 1 year [38]. In one long-term study, Cacciatore et al. found that patients with HF and frailty syndrome had a substantially lower probability of surviving >10 years [39]. Furthermore, frailty and comorbidities often overlap in the elderly and pose significant increased risk of multiple hospitalizations, ensuing disability, becoming institutionalized, and death [40]. Consequently, the assessment of frailty has the potential to refine estimates of risk and allows treatment decisions to be tailored individually for each SNF HF patient.
Geriatric syndromes, such as cognitive impairment, delirium, falls, and urinary incontinence, are also highly prevalent among patients requiring admission to skilled nursing care. While no study confirms the prevalence and associated risks of geriatric syndromes specifically among SNF HF patients, they have been recognized as a source of substantial morbidity and worsened outcomes [41]. Cognitive impairment is particularly detrimental and prevalent. In one large study of 62,330 Medicare patients with HF age 65 or older, cognitive impairment was significantly associated with death at 30 days and 5 years [42]. A prospective cohort study of older adults hospitalized for HF found cognitive impairment to be present in 46.8 % of the study patients, but under-recognized [43]. This finding has pertinent management implications particularly for SNF HF patients considered in the rehabilitation group, where unrecognized cognitive impairment is likely to hinder treatment adherence, prognosis after discharge, and undercut improvement.
Poor Outcomes Among Heart Failure Patients in SNFs
Patients hospitalized for HF are at high risk for adverse outcomes, and those discharged to SNFs are at particularly high risk.
Mortality
A retrospective observational study of 500,322 residents in 1840 facilities including nursing homes and skilled nursing facilities found that 37.7 % of residents had HF, and the annual mortality rate among those patients exceeded 45 % [44]. An observational study of 15,459 older patients hospitalized for HF between 2005 and 2006 found that the 24.1 % of patients discharged to SNFs versus the 53.6 % discharged home had higher rates of death at both 30 days (14.4 vs 4.1 %) and 1-year (53.5 vs 29.1 %; P<0.0001). While the results of this study were partially attenuated after adjusting for in-hospital patient factors and did not exclude discharges for hospice care, SNF discharge remained associated with a 76 % increased risk of all-cause mortality compared to patients discharged to home [34••].
Few studies have looked at the associations between such high mortality risks in relation to the types of care that are administered. Hospitalized HF patients discharged to nursing home settings including SNFs and LTC are less likely to receive lifesaving renin-angiotensin system inhibitors (ACE inhibitors or ARBs), even with documentation of reduced LV function and among those who received cardiology consultations during the preceding hospitalizations [45]. While this may be related to risks of renal impairment or hypotension, one study showed that treatment with ACE inhibitors in acute HF patients among 58 SNFs was associated with a 33 % mortality reduction [46]. Additionally, despite studies showing that elderly patients with HF benefit from cardiac rehabilitation [47], few SNF cardiac patients receive such vital therapy [48]. Likewise, standard rehabilitative services like physical and occupation therapy have been shown to improve outcomes in HF patients in nursing facilities. One study demonstrated a 19 % reduction in death and higher rates of return to the community among nursing home patients with HF who received physical and occupational therapy (a 56 % subset of HF patients in a nursing home population of 11,150), [49] raising the question as to why it was not used in the others. Overall, studies indicate that HF patients in SNFs have higher mortality rates, but are less likely to receive evidence-based pharmacologic and non-pharmacologic therapies.
Readmissions
Discharging HF patients to SNFs has not been shown to reduce 30-day rehospitalizations. The overall proportion of all SNF admissions ending in rehospitalization for any cause within 30 days increased from 18.2 % in 2000 to more than 23.5 % in 2006 [11]. Heart failure was among the five reportable conditions accounting for 78 % of all 30-day rehospitalizations from SNF patients in 2004 [50] and among the 13 conditions identified as avoidable and collectively accounting for 47.3 % of all SNF hospital readmissions in 2012 [29]. Hospitalized HF Medicare patients discharged to SNFs between 2006 and 2008 had a hospital readmission rate within 30 days of 28.2 %, which was significantly higher than the readmission rate for HF patients not referred to SNFs (23.7 %; P<.001) [51]. Data involving Medicare patients aged 75 and older between 2007 and 2008 from 3254 SNF cases showed HF accounted for 31 % of the so-called avoidable hospital readmission rates [52]. Despite the fact that some hospitals rely more heavily on SNF discharges than others for hospitalized HF patients, no observable difference in 30-day risk-standardized readmission rates has been shown between hospitals that discharge 75 % of their patients to SNFs vs those that discharge none of their patients to SNFs [23].
CMS considers HF to be a potentially avoidable cause of hospital readmission; it maintains that many episodes of HF exacerbations (not new onset or with hemodynamic instability) managed in a SNF can (should) be prevented with careful monitoring. Moreover, for patients experiencing frequent exacerbations despite good management (a condition signifying a very poor prognosis), palliative care or hospice is endorsed as an alternative to hospitalization [53].
Factors associated with hospital readmission among post-acute care HF patients are likely to differ from factors leading to readmission among community-dwelling HF patients. Typical destabilizing factors of outpatients include dietary indiscretion, medication non-compliance, and failure to recognize symptoms or weight gain, which should all theoretically be better controlled in a SNF environment. However, few studies have indicated what factors are then more likely to determine rehospitalization for SNF HF patients [7]. One small study found anemia among SNF patients with CHF complicated by cardiorenal syndrome to be associated with rehospitalization [54]. Other data suggests local area factors such as provider norms, practice patterns, bed availability, and use of hospice services impact SNF rehospitalizations [11]. Among 156 older HF patients from 58 SNFs with an acute HF exacerbation, rehospitalized subjects were more likely to have been living in a nursing home previously and more likely to have their symptoms evaluated at night [46]. Surprisingly, the same study showed that rehospitalized patients tended to be younger, not hypotensive, and not demented. The authors acknowledged these unanticipated results regarding age, severity of exacerbation, and cognition, and suggested that they may indicate a lack of information and understanding of the functional and hemodynamic characteristics of HF in SNFs [46]. We can further consider there may be an unawareness regarding many HF management priorities in many SNFs and/or the predominance of administrative issues which impact choices. Overall, thresholds for readmission vary greatly across facilities depending on the facility administration, staffing ratios, involvement of primary and specialty physicians, and the HF management skillset of the facility nursing staff.
Cost
In the USA, the estimated annual cost for HF is $39.2 billion [55]. The total cost of SNF care is estimated at $28.7 billion, almost half of the $59.4 billion total expenditure on post-acute care [56]. The expenditure specifically for HF care in SNFs has not been described. The cost to Medicare for all-cause SNF-related readmissions is estimated at $4.3 billion, $3.39 billion of which is spent on potentially avoidable rehospitalizations [11], including HF. Home healthcare has been found to be more cost-effective than SNFs or rehabilitation facilities [57], but more data is needed to understand the financial implications of improving HF care in SNFs.
One study of 25 nursing homes completing the Interventions to Reduce Acute Care Transfers II (INTERACT II) program found that the 17 homes that were “moderately or highly engaged” in the initiative had a 24 % reduction in hospitalizations. The authors estimated this translated to a projected Medicare savings in a 100-bed nursing home of $125,000 per year [58]. Another program evaluating the use of phone calls from hospital nurse case management to registered/licensed practical nurses in SNFs regarding weights, sodium restrictions, diuretic use, and follow-up discharge plans noted a 38.68 % reduction in hospital readmissions, a cost savings of $16,748 over a 6-month period [59]. Identifying effective strategies to reduce costs of HF care in SNFs may not only reduce the burden on our healthcare system but also may become increasingly relevant as hospitals progress to adopt bundled payment plans.
The State of Heart Failure Management in SNFs
For various reasons, including but not limited to lack of facility preparedness, traditional nursing home culture, staffing and administration reception to adopting new policies, and lack of systematic disease management protocols, HF management in SNFs has not yet experienced the robust quality improvements recently seen in hospitals. With the increasing number of patients discharged to SNFs, as well as their characteristic medical, social, and economic complexities, SNFs are now conspicuous with their poor outcomes. Both the Society for Post-Acute and Long-Term Care (AMDA) and the American Heart Association/Heart Failure Society of America (AHA/HFSA) joint committee released guidelines in 2015 on the management of HF in post-acute care [14•, 15], AMDA on management in post-acute and long-term care settings, and AHA/HFSA specifically in SNFs. These just-released guidelines address HF diagnosis, pharmacologic and non-pharmacologic management of acute and chronic HF, end-of-life issues, as well as HF education. The growing sense of imperative from the healthcare community to improve post-acute HF care emphasizes the need for administrators to participate in quality improvement initiatives and to give ample consideration to an integrated team approach.
There are few data on initiatives to implement HF protocols to improve outcomes. An evaluation of the baseline state of HF management in four SNFs and the effect of a staff HF educational program found that the facilities had no HF-specific SNF protocols in place initially and that the staff lacked knowledge regarding HF guidelines. After providing a HF educational program, the staff grew more knowledgeable and more confident in performing HF care, but the attrition of staff members was high [6•]. Dolansky et al. used the Kotter's Change Management principles to guide the implementation of a HF management program in SNFs. While they observed large variability in adherence to protocols stemming from inadequate availability of hospital information, increased staff workload, high staff turnover rate, failure to orient new staff to the elements of the HF program, lack of formal processes to identify HF patients, and lack of availability of specified dietary recommendations, the authors found that weekly exposure to a protocol coach and physician involvement in the program implementation improved success [60]. Another study found that a nurse case management-driven process of care to address both care transitions and SNF management utilizing improved communication and monitoring reduced readmission rates in HF patients from 30 to 11.32 % [59]. As facilities are heterogeneous in both their readiness and receptiveness to implement new models of care, it is important to understand successful ways to implement necessary change. One study looked at an approach to implementation of a novel model of HF care and found the use of a team-based approach, staff engagement, and flexibility of processes to respect the SNF's needs and culture was the most valuable and resulted in better HF care, enhanced teamwork, and improved staff job satisfaction [61].
To date, there are also significant gaps in transition of care for HF patients discharged from the SNF to either the community or other post-acute settings, which is an area garnering significant interest [9•] and opportunity for future research. Key areas of emphasis include physician assessment prior to discharge from the SNF; adequate management of comorbid conditions; transmission of complete clinical information at the discharge; adequate education to patients and caregivers; and motivation of HF patients to strictly respect dietary restrictions, medications, therapies, daily weights, and follow-up.
More Appropriate Goals of Management
The 2015 AHA/HFSA Scientific Statement regarding HF management in SNFs constitutes a major advance in therapeutic standards particularly as it conceptualizes therapy in relation to each patient's particular circumstances. Rather than delineating a fixed standard of “optimal care” for SNF residents, the statement emphasizes that SNF patient population is inherently heterogeneous and that care must correspond to individual patient's idiosyncratic goals of care. The statement exemplifies the point by defining three broad categories of patients (as described above): the long-term care, the rehabilitation, and the uncertain prognosis groups [14•]. In each group, goals of care as well as the intrinsic capacities of each patient to tolerate and respond to therapy play a determinant role in the so-called optimal care. Thus, for patients in the rehabilitation group, care is generally consistent with traditional standards of care, i.e., an aggregate of evidence-based standards of medications and procedures that are generally oriented to increased longevity and which also usually entail a significant treatment burden (i.e., multiple medications, procedures, and monitoring, with associated logistics, costs, and prioritization of CV care). In contrast, patients in the long-term group have very different goals and priorities. For these patients, symptom management, reduced falls, maximized physical and cognitive capacities, and reduced burden of care often rise as the primary priorities. Many medications (e.g., beta-blockers) that would be priorities for patients in the rehabilitation group would not be priorities in the long-term group. Similarly, the value of devices (e.g., defibrillators) and other aspects of care are fundamentally dissimilar. Patients within the uncertain prognosis group require particularly careful consideration of each aspect of treatment, with clear reasoning as to why each medication, device, and procedure is needed, and an understanding of the trade-offs between cumulative morbidity and therapeutic burden among these patients who are often destabilized by polypharmacy and interventions.
One key aspect of care that is ironically often underemphasized for older HF patients is the benefit of exercise training. Rehabilitation-type patients certainly benefit from aerobic and strength training after enduring the erosive effects of illnesses as well as hospitalizations associated with bed rest and deconditioning. However, it is often less obvious that frail and relatively more infirmed SNF patients in the uncertain prognosis or even the long-term groups may benefit even more [62]. Exercise training regimens also need to be tailored to each patient's capacities and goals, but well-done programs can facilitate improved functional metrics that can factor decisively in recovery, quality of life, and/or other aspects of care. Even the most enfeebled patients can gain critical capacities for transfers (e.g., bed-to-chair), toileting, eating, and other aspects of self-care that are essential for overcoming disability, depression, and other debilitating aspects of illness.
Conclusion
The high risk for HF hospitalized patients extends beyond their inpatient admission into discharge. This period was nicely described previously as post-hospital syndrome [63], a time characterized by increased risk related to the physiologic and psychological stressors of hospitalization. Within this vulnerable time frame, the most frail, sick, and high-risk subset of hospitalized HF patients will increasingly be discharged without adequate care transitions to SNFs, post-acute care settings where no standardized educational HF staff programs or CHF management protocols currently exist. Yet roughly one in five HF patients will be admitted to a SNF; family and caregiver expectations for “rehabilitation” will remain high, and discharging hospitals, healthcare regulatory agencies, and the government will soon be expecting improving outcomes and measurable progress in quality metrics. Data is accumulating regarding the outcomes and targets for interventions to improve care, but more research is needed to match the interest and growing demands for progress in SNF HF care.
Acknowledgments
Dr. Forman is supported in part by NIA grant P30 AG024827 and VA Office of Rehabilitation Research and Development grant F0834-R.
Footnotes
This article is part of the Topical Collection on Cardiovascular Disease in the Elderly
Compliance with Ethics Guidelines
Conflict of Interest Nicole M. Orr, Daniel E. Forman, Giuseppe De Matteis, and Giovanni Gambassi declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Krumholz HM, Nuti S, Downing N, et al. Mortality, hospitalizations, and expenditures for the Medicare population aged 65 years or older, 1999–2013. JAMA. 2015;314(4):355–65. doi: 10.1001/jama.2015.8035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tyler DA, Feng Z, Leland NE, Gozalo P, Intrator O, Mor V. Trends in postacute care and staffing in US nursing homes, 2001–2010. J Am Med Dir Assoc. 2013;14(11):817–20. doi: 10.1016/j.jamda.2013.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US News and World Report. 2015 Aug 5; Available at http://health.usnews.com/health-news/hospital-of-tomorrow/articles/2015/08/05/half-of-nations-hospitals-fail-again-to-escape-medicares-readmission-penalties.
- 4.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–7. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vidic A, Chibnall JT, Hauptman PJ. Heart failure is a major contributor to hospital readmission penalties. J Card Fail. 2015;21:134–7. doi: 10.1016/j.cardfail.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 6•.Boxer RS, Dolansky MA, Frantz MA, Prosser R, Hitch JA, Piña IL. The Bridge Project: improving heart failure care in skilled nursing facilities. J Am Med Dir Assoc. 2012;13(1):83, e1–7. doi: 10.1016/j.jamda.2011.01.005. [A study describing some current deficiencies in HF management in SNFs and effects of staff HF education.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung M, Yeh A, Pressler S. Heart failure and skilled nursing facilities: review of the literature. J Card Fail. 2012;18(11):854–71. doi: 10.1016/j.cardfail.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Kosecoff J, Kahn KL, Rogers WH, et al. Prospective payment system and impairment at discharge. The Bquicker-and-sicker^ story revisited. JAMA. 1990;264:1980–3. [PubMed] [Google Scholar]
- 9•.Centers for Medicare and Medicaid Services [15 Aug 2015];Medicare program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities (SNFs) for FY 2016, SNF Value-Based Purchasing Program, SNF Quality Reporting Program, and Staffing Data Collection Federal Register. 08-04-15 Available at https://www.federalregister.gov/articles/2015/08/04/2015-18950/medicare-program-prospective-payment-system-and-consolidated-billing-for-skilled-nursing-facilities. [Details the legislative changes affecting SNF payment and quality reporting programs.] [PubMed]
- 10.Morley M, Bogasky S, Gage B, et al. Medicare post-acute care episodes and payment bundling. Medicare and Medicaid Research Review. 2014;4(1):E1–E12. doi: 10.5600/mmrr.004.01.b02. doi:10.5600/mmrr.004.01.b02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood) 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medicare Payment Advisory Commitee [20 Jul 2015];A Data Book: Health care spending and the Medicare program, Section 8: Post Acute Care. 2015 Jun;:114. available at http://www.medpac.gov/documents/data-book/june-2015-data-book-section-8-post-acute-care.pdf?sfvrsn=0.
- 13.Centers for Medicare and Medicaid Services [1 Aug 2015];Final fiscal year 2016 payment and policy changes for Medicare Skilled Nursing Facilities 2015-07-30. Available at https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-07-30-2.html.
- 14•.Jurgens CY, Goodlin S, Dolansky M, et al. Heart failure management in skilled nursing facilities: a scientific statement from the American Heart Association and the Heart Failure Society of America. J Card Fail. 2015;21:263–99. doi: 10.1016/j.cardfail.2015.02.007. [A scientific statement issued to detail appropriate practice management strategies specifically for heart failure patients in skilled nursing facilities.] [DOI] [PubMed] [Google Scholar]
- 15.AMDA. Heart failure in the long-term care setting: clinical practice guidelines. AMDA: Society of Post-acute and Long-term care Medicine; Columbia: 2015. [Google Scholar]
- 16.Barker WH, Mullooly JP, Getchell W. Changing incidence and survival for heart failure in a well-defined older population, 1970–1974 and 1990–1994. Circulation. 2006;113:799–805. doi: 10.1161/CIRCULATIONAHA.104.492033. [DOI] [PubMed] [Google Scholar]
- 17.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306(15):1669–78. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 19.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol. 2008;52(6):428–34. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 20.Hall MJ, Levant S, DeFrances CJ. Hospitalization for Congestive Heart Failure: United States, 2000–2010. 108. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention National Center for Health Statistics NCHS Data Brief; 2012. [21 Jul 2015]. pp. 1–8. Available at http://www.cdc.gov/nchs/data/databriefs/db108. pdf. [Google Scholar]
- 21.Centers for Medicare & Medicaid Services . Medicare Hospital Quality Chartbook 2014: Performance Report on Outcome Measures. Centers for Medicare & Medicaid Services; Washington, DC: 2014. p. 22. [Google Scholar]
- 22.Gheorghiade M, Abraham WT, Albert NM, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217–26. doi: 10.1001/jama.296.18.2217. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Medicare & Medicaid Services . Medicare Hospital Quality Chartbook 2010: Performance Report on Outcomes Measures for Acute Myocardial Infarction, Heart Failure, and Pneumonia. Centers for Medicare & Medicaid Services; Washington, DC: 2010. pp. 32–4. [Google Scholar]
- 24.Brown DW, Haldeman GA, Croft JB, Giles WH, Mensah GA. Racial or ethnic differences in hospitalization for heart failure among elderly adults: Medicare, 1990 to 2000. Am Heart J. 2005;150:448e54. doi: 10.1016/j.ahj.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 25.McMurray JJ, Pfeffer MA. Heart failure. Lancet. 2005;365(9474):1877–89. doi: 10.1016/S0140-6736(05)66621-4. [DOI] [PubMed] [Google Scholar]
- 26.Heidenreich PA, Albert NM, Allen LA, et al. American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat. 2009;13(167):1–155. [PubMed] [Google Scholar]
- 28.Ahmed AA, Hays CI, Liu B, Aban IB, Sims RV, Aronow WS, et al. Predictors of in-hospital mortality among hospitalized nursing home residents: an analysis of the National Hospital Discharge Surveys 2005–2006. J Am Med Dir Assoc. 2010;11:52–8. doi: 10.1016/j.jamda.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kramer A, Lin M, Fish R, Min S. Final Report March. Vol. 10. Providigm LLC; Denver, CO: 2014. [20 Jul 2015]. Development of potentially avoidable readmission and functional outcome SNF quality measures. p. 22. Available at http://www.medpac.gov/documents/contractor-reports/mar14_snfqualitymeasures_contractor.pdf?sfvrsn=0. [Google Scholar]
- 30.Heckman G, Boscart V, McKelvie R. Management considerations in the care of elderly heart failure patients in long-term care facilities. Futur Cardiol. 2014;10(4):563–77. doi: 10.2217/fca.14.35. [DOI] [PubMed] [Google Scholar]
- 31.Butler R, Fonseka S, Barclay, et al. The health of elderly residents in long term care institutions in New Zealand. N Z Med J. 1999;12:427–9. [PubMed] [Google Scholar]
- 32. [20 Aug 2015];CMS manual system. https://www.cms.gov/Regulations-and-guidance/Guidance/Transmittals/downloads/R57BP.pdf.
- 33.Dolansky M, Xu F, Zullo M, et al. Post-acute care services received by older adults following a cardiac event: a population-based analysis. J Cardiovasc Nurs. 2010;25:342–9. doi: 10.1097/JCN.0b013e3181c9fbca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34••.Allen LA, Hernandez AF, Peterson ED, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [The first large prospective study characterizing patients discharged to SNF and non-SNF locations after acute hospitalization for HF and associating discharge status with outcome.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harkness K, Heckman GA, McKelvie RS. The older patient with heart failure: high risk for frailty and cognitive impairment. Expert Rev Cardiovasc Ther. 2012;10(6):779–95. doi: 10.1586/erc.12.49. [DOI] [PubMed] [Google Scholar]
- 36.Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56:2171–9. doi: 10.1111/j.1532-5415.2008.02023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fried LP, Walston JD, Ferrucci L. Frailty. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, High KP, Asthana S, editors. Hazzard's geriatric medicine and gerontology. 6th ed. McGraw-Hill; New York: 2009. pp. 631–46. [Google Scholar]
- 38.Lupón J, González B, Santaeugenia S, et al. Prognostic implication of frailty and depressive symptoms in an outpatient population with heart failure. Rev Esp Cardiol. 2008;61:835–42. [PubMed] [Google Scholar]
- 39.Cacciatore F, Abete P, Mazzella F, et al. Frailty predicts long-term mortality in elderly subjects with chronic heart failure. Eur J Clin Investig. 2005;35:723–30. doi: 10.1111/j.1365-2362.2005.01572.x. [DOI] [PubMed] [Google Scholar]
- 40.Murad K, Kitzman DW. Frailty and multiple comorbidities in the elderly patient with heart failure: implications for management. Heart Fail Rev. 2012;17(4–5):581–8. doi: 10.1007/s10741-011-9258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dodson JA, Chaudry SI. Geriatric conditions in heart failure. Curr Cardiovasc Risk Rep. 2012;6(5):404–10. doi: 10.1007/s12170-012-0259-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chaudhry SI, Wang Y, Gill TM, Krumholz HM. Geriatric conditions and subsequent mortality in older patients with heart failure. J Am Coll Cardiol. 2010;55:309–16. doi: 10.1016/j.jacc.2009.07.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dodson JA, Truong TT, Towle VR, Kerins G, Chaudhry SI. Cognitive impairment in older adults with heart failure: prevalence, documentation, and impact on outcomes. Am J Med. 2013;126(2):120–6. doi: 10.1016/j.amjmed.2012.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hutt E, Elder SJ, Fish R, Min SJ. Regional variation in mortality and subsequent hospitalization of nursing residents with heart failure. J Am Med Dir Assoc. 2011;12:595–601. doi: 10.1016/j.jamda.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 45.Aronow WS, Rich MW, Goodlin SJ, et al. In-hospital cardiology consultation and evidence-based care for nursing home residents with heart failure. J Am Med Dir Assoc. 2012;13(5):448–52. doi: 10.1016/j.jamda.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hutt E, Frederickson E, Ecord M, Kramer AM. Associations among processes and outcomes of care for Medicare nursing home residents with acute heart failure. J Am Med Dir Assoc. 2003;4(4):195–9. doi: 10.1097/01.JAM.0000073964.19754.C0. [DOI] [PubMed] [Google Scholar]
- 47.Balady GJ, Williams MA, Ades PA, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee. Circulation. 2007;115:2675–82. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 48.Dolansky MA, Zullo MD, Hassanein S, Schaefer JT, Murray P, Boxer R. Cardiac rehabilitation in skilled nursing facilities: a missed opportunity. Heart Lung. 2012;41:115e24. doi: 10.1016/j.hrtlng.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murray PK, Singer M, Dawson NV, et al. Outcomes of rehabilitation services for nursing home residents. Arch Phys Med Rehabil. 2003;84(8):1129–36. doi: 10.1016/s0003-9993(03)00149-7. [DOI] [PubMed] [Google Scholar]
- 50.Donelan-McCall N, Eilersen T, Fish R. Small patient population and low frequency event effects on the stability of SNF quality measures. Medicare Payment Advisory Commission; Washington (D.C.): 2006. [Google Scholar]
- 51.Chen J, Ross JS, Carlson MD, et al. Skilled nursing facility referral and hospital readmission rates after heart failure or myocardial infarction. Am J Med. 2012;125:100, e1–9. doi: 10.1016/j.amjmed.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ouslander JG, Diaz S, Hain D, Tappen R. Frequency and diagnoses associated with 7- and 30-day readmission of skilled nursing facility patients to a nonteaching community hospital. J Am Med Dir Assoc. 2011;12(3):195–203. doi: 10.1016/j.jamda.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 53.Ingber M, Feng Z, Khatutsky G. Evaluation of the initiative to reduce avoidable hospitalizations among nursing facility residents summary of evaluation as of December 2014. [10 Aug 2015];RTI International. 2015 May; Available at http://innovation.cms.gov/Files/reports/irahnfr-secondevalrpt.pdf.
- 54.Tamhane U, Voytas J, Aboufakher R, Maddens M. Do hemoglobin and creatinine clearance affect hospital readmission rates from a skilled nursing facility heart failure rehabilitation unit? J Am Med Dir Assoc. 2008;9:194–8. doi: 10.1016/j.jamda.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 55.Braunschweig F, Cowie M, Auricchio A. What are the costs of heart failure? Europace. 2011;13(Suppl 2):ii13–7. doi: 10.1093/europace/eur081. [DOI] [PubMed] [Google Scholar]
- 56.Medicare Payment Advisory Committee . Report to the Congress: Medicare Payment Policy. Skilled Nursing Facilities; Washington, DC: Mar, 2014. [13 Aug 2015]. Chapter 8 Available at: http://www.medpac.gov/documents/reports/mar14_ch08.pdf?sfvrsn=0. [Google Scholar]
- 57.Chen Q, Kane RL, Finch MD. The cost effectiveness of post-acute care for elderly Medicare beneficiaries. Inquiry. 2000;37:359–75. [PubMed] [Google Scholar]
- 58.Ouslander J, Lamb G, Tappen R, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc. 2011;59(4):745–53. doi: 10.1111/j.1532-5415.2011.03333.x. [DOI] [PubMed] [Google Scholar]
- 59.Jacobs B. Reducing heart failure hospital readmissions from skilled nursing facilities. Prof Case Manag. 2011;16:18e24. doi: 10.1097/NCM.0b013e3181f3f684. [DOI] [PubMed] [Google Scholar]
- 60.Dolansky MA, Hitch JA, Pina IL, Boxer RS. Improving heart failure disease management in skilled nursing facilities: lessons learned. Clin Nurs Res. 2013;22:432–47. doi: 10.1177/1054773813485088. [DOI] [PubMed] [Google Scholar]
- 61.Nazir A, Dennis M, Unroe K. Lessons from the implementation of a heart failure quality improvement initiative in a skilled nursing facility. J Gerontol Nurs. 2015;41:2633. doi: 10.3928/00989134-20141216-01. [DOI] [PubMed] [Google Scholar]
- 62.Conner D, Barnes C, Harrison-Felix C, Reznickova N. Rehabilitation outcomes in a population of nonagenarians and younger seniors with hip fracture, heart failure, or cerebral vascular accident. Arch Phys Med Rehabil. 2010;91:1505–10. doi: 10.1016/j.apmr.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 63.Krumholz HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–2. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]