Abstract
Background
Revitalizing the necrotic subchondral bone and preserving the intact cartilage layer by retrograde drilling is the preferred option for treatment of undetached osteochondral lesions of the talus (OLT). We assessed the effectiveness of Endoscopic Core Decompression (ECD) in treatment of OLT.
Material/Methods
Seven patients with an undetached OLT of the medial talar dome underwent surgical treatment using an arthroscopically-guided transtalar drill meatus for core decompression of the lesion. Under endoscopic visualization the OLT was completely debrided while preserving the cartilage layer covering the defect. The drill tunnel and debrided OLT were filled using an injectable bone graft substitute. Various clinical scores, radiographic imaging, and MRI were evaluated after a mean follow-up of 24.1 months.
Results
The American Orthopedic Foot and Ankle Society Score significantly improved from 71.0±2.4 to 90.3±5.9, and the Foot and Ankle Disability Index improved from 71.8±11.1 to 91.7±4.8. Radiographically, we observed good bone remodelling of the medial talar dome contour within 3 months. In MRI, an alteration of the bony signal of the drill tunnel and the excised OLT remained for more than 12 months.
Conclusions
First follow-up results for the surgical technique described in this study are highly promising for treatment of undetached stable OLT grade II or transitional stage II–III according to the Pritsch classification. Even lesions larger than 150 mm2 showed good clinical scores, with full restoration of the medial talar dome contour in radiographic imaging.
MeSH Keywords: Ankle Joint; Arthroplasty, Subchondral; Arthroscopy; Bone Cysts; Osteonecrosis; Talus
Background
Avascular necrosis and osteochondral lesions can occur in diverse bones or joints [1–5]. Osteochondral lesions of the talus (OLT) are a common cause of chronic ankle pain. An OLT most often is located on the posteromedial aspect of the talus and poses a great challenge to the surgeon. Multiple surgical treatment strategies have been described, but surgical treatment dependent on the OLT stage and size remains controversial.
All operative treatment strategies aim to revitalize the necrotic subchondral bone tissue either by arthroscopic or open surgical procedures, including defect curettage, micro-fracturing, retrograde drilling, cancellous bone grafting, or osteochondral transplantation. In undetached lesions the subchondral bone area can be revitalized by retrograde drilling without damaging the intact cartilage layer covering the defect [3–5]. The surgical principles of transtalar drilling were described by Conti in 1996 [6].
In the present article we describe and evaluate the Endoscopic Core Decompression (ECD) of contained OLT. The procedure is a modified technique of transtalar drilling that may allow better removal of the necrotic tissue by using endoscopic guidance and diverse percutaneous instruments (e.g., mini-shaver). A further modification is the filling of the drill hole and the defect with an injectable, hard-setting composite calcium sulfate (CaSO4)-calcium phosphate (CaPO4) bone graft substitute (PRO-DENSE®, Wright Medical Technology™ Inc., Arlington, TN, USA).
The aim of this study was to describe the operative technique for the first time and evaluate the outcome of patients with contained OLT.
Material and Methods
Operative technique
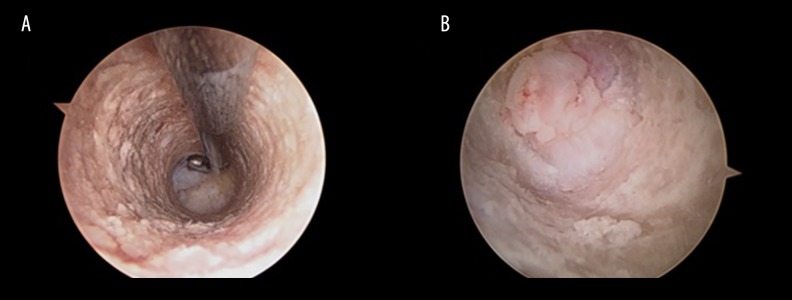
All patients were positioned supine with the ankle draped and hanging freely over the edge of the table. Arthroscopy of the ankle joint was performed in a routine fashion with a standard 4.0-mm optic. The joint was assessed by an anteromedial and an anterolateral portal. After evaluation of the OLT, a small 10–15 mm skin incision was made over the sinus tarsi. Under arthroscopic visualization the tip of a drill guide (MICRO VECTOR™ Drill Guide, Smith & Nephew, London, UK) was placed over the softened cartilage covering the OLT and a 1.6-mm K-wire was placed in the center of the OLT through the sinus tarsi. Precise placement and depth of the K-wire was confirmed fluoroscopically in 2 planes. The K-wire was then over-reamed with an 8.0-mm cannulated reamer, avoiding damage to the cartilage covering the OLT. Drill depth was again checked fluoroscopically in 2 planes. The arthroscope was then switched into the created bone tunnel in the talus. The OLT at the top of the drill tunnel with its necrotic tissue could be clearly identified and distinguished from the adjacent healthy cancellous bone (Figure 1). Under direct visualization the ECD was performed by debriding the OLT using a curette, spoon, or mini-shaver. The necrotic tissue was removed, preserving the cartilage layer covering the defect. After debridement, cartilage integrity was checked again by placing the arthroscope in the ankle joint. The debrided OLT and bone tunnel were filled with an injectable, hard-setting, synthetic osteoconductive, composite calcium sulphate (CaSO4)-calcium phosphate (CaPO4) bone graft substitute (PRO-DENSE®, Wright Medical Technology Inc., Arlington, TN). Intraarticular application of the bone graft substitute was excluded arthroscopically. The graft substitute was injected with a cannula to prevent contact with the surrounding soft tissues in the sinus tarsi due to its potential of soft tissue irritation. Final bone graft placement was checked fluoroscopically.
Figure 1.
Endoscopic views of (A) drill tunnel probing the OLT and (B) necrotic OLT tissue which can be clearly distinguished from healthy bone of the drill tunnel.
All patients were treated with a standardized rehabilitation schedule. Partial weight-bearing with 20 kg was allowed for 4 weeks, half of body weight in weeks 5 and 6, and total weight-bearing from week 7.
Patients and study design
Seven patients (3 male, 4 female, average age 36 (range, 18–69) years) were included in this prospective case series. All patients suffered from chronic ankle pain due to an OLT of the medial talar dome and had undergone non-operative treatment for at least 3 months without improvement of their symptoms. The diagnosis was confirmed by plain radiographs (standing a.p., true a.p., and lateral) and an MRI of the ankle joint.
The criteria for inclusion were symptomatic undetached osteochondral lesions of the medial talar dome grade II, partially detached grade III or grade V according to the Bristol classification [7,8], an OLT of at least 100 mm2, and full range of motion of the ankle and subtalar joint. Exclusion criteria were OLT grade I, fully detached grade III or grade IV, prior operative treatment of the OLT, symptomatic ankle instability, hindfoot malalignment, or signs of osteoarthritis in imaging.
Under arthroscopic visualization the diagnosis was confirmed intraoperatively and concomitant pathologies were recorded and treated. The OLT of the medial talar dome was localized by probing the cartilage covering the defect. According to the classification of Pritsch, intact overlying cartilage was graded I, softened depressible cartilage was graded II, and frayed overlying cartilage was graded III. Patients showing unstable loose cartilage grade III [8] were excluded from the study. Small cracks or fissures in the cartilage layer were treated if the lesion was stable on probing and if two-thirds of the circumferential cartilage was intact. These lesions were graded as transitional stage II–III.
Outcome and patient satisfaction were evaluated according to the American Orthopedic Foot and Ankle Society Score (AOFAS) and the Foot and Ankle Disability Index (FADI) preoperatively and after a mean follow-up of 24.1 months (range, 20–28 months). Remodeling of the OLT and bone ingrowth into the graft substitute were evaluated by means of true a.p. and lateral plain radiographs of the ankle joint, as well as an MRI 1 year after treatment.
Statistical analysis
Summary statistics of the data are expressed as mean ±SD. The Shapiro-Wilk test was used to test for normal distribution. The paired Student’s t-test was used for comparison of the normal distribution of pre- and postoperative means and the Wilcoxon signed-rank test was used for non-normal distribution. The comparisons with p-values <0.05 were considered to be significant. The software SPSS 19 (SPSS Inc. Headquarters, Chicago, Illinois, USA) was used to carry out the statistical computations.
Results
No intraoperative complications, such as an extrusion of the liquid bone graft substitute into the ankle joint or detachment of the cartilage layer, were observed. In addition to treatment of the OLT a minor anterior tibial spur was removed in 2 cases and in 5 cases partial synovectomy was necessary to aid in visualization.
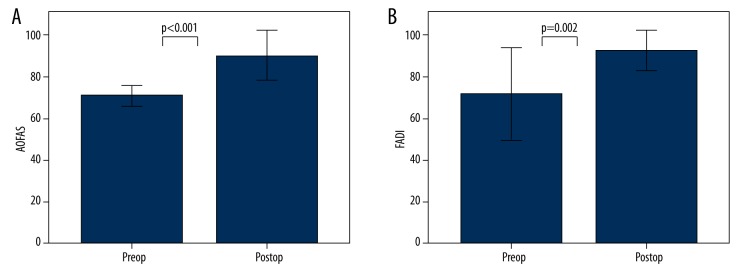
In all cases the ECD led to an improvement in the AOFAS and FADI scores (Figure 2, Table 1). The AOFAS score significantly improved from 71.0±2.4 to 90.3±5.9 (p<0.001) at the latest follow-up. The improvement in the AOFAS score was mainly due to pain reduction. The preoperative symptoms of moderate daily (6/7) or severe almost always present pain (1/7) improved after ECD to mild occasional daily pain (4/7) or no pain at all (3/7). The FADI score improved significantly from 71.8±11.1 to 91.7±4.8 (p=0.002) at follow-up.
Figure 2.
(A) American Orthopedic Foot and Ankle Society Score (AOFAS) before and after ECD and (B) Foot and Ankle Disability Index (FADI) before and after ECD.
Table 1.
Cases treated with ECD.
| No | Gender | Age at op | OLT grade (Bristol) | OLT Pritsch grade | Defect size length/width/ depth (mm) in MRI (mm2) | AOFAS pre | AOFAS post | FADI pre | FADI post | FU months |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 18 | II | II | 15×10×10 (150) | 71 | 90 | 65.4 | 93.3 | 20 |
| 2 | Female | 43 | III | II–III | 10×10×7 (100) | 68 | 85 | 63.5 | 88.4 | 26 |
| 3 | Female | 19 | II | II | 12×10×8 (120) | 68 | 87 | 53.8 | 91.3 | 27 |
| 4 | Male | 38 | V | II | 15×11×12 (165) | 71 | 97 | 80.8 | 95.2 | 23 |
| 5 | Female | 22 | II | II–III | 12×10×10 (120) | 71 | 85 | 78.8 | 84.2 | 28 |
| 6 | Female | 44 | III | II | 14×9×9 (131) | 74 | 88 | 76.0 | 90.3 | 24 |
| 7 | Male | 69 | V | II | 17×10×9 (170) | 74 | 100 | 84.6 | 99.0 | 21 |
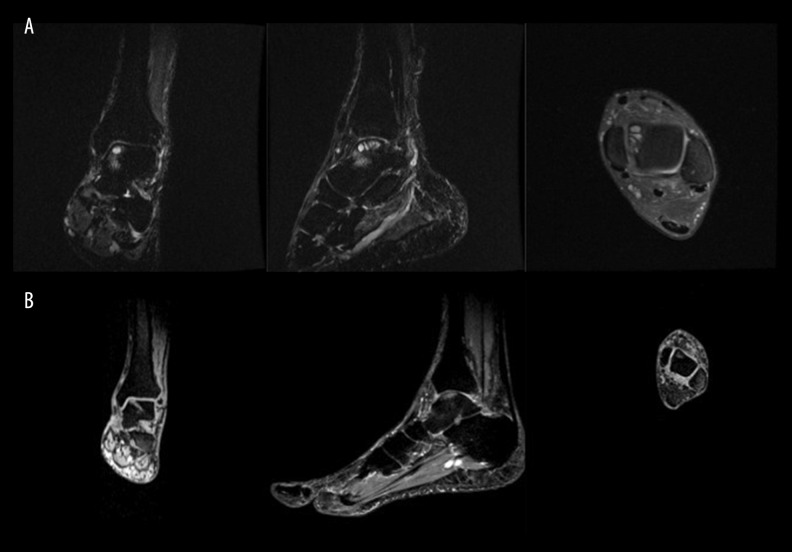
The mean OLT defect in preoperative MRI imaging measured 136.6±25.9 mm2. The radiographic controls showed good bone remodelling with invisibility of the bone graft substitute in x-ray within 8–12 weeks. The ECD led to a good restoration of the medial talar dome contour with an almost complete resection of the OLT (Figure 3). MRI imaging showed an alteration of the bony signal in the treated OLT and drill meatus for more than 12 months. Compared to preoperative imaging, the lesions no longer showed demarcation but only vague contours, indicating bony ingrowth and remodelling of the lesion. Moreover, previous bone bruising adjacent to the OLT had disappeared (Figure 4).
Figure 3.
(A) Preoperative a.p. standing x-ray showing OLT stage V of the medial talar dome. Postoperative a.p. x-ray showing (B) bone graft filling of drill tunnel and OLT at day 1 after ECD, (C) partial resorption of bone graft substitute 8 weeks after ECD, and (D) complete resorption of bone graft substitute with bony ingrowth into the OLT and remodelling of medial talar dome 7 months after ECD.
Figure 4.
(A) Preoperative MRI (STIR) showing an osteochondral lesion with bone edema and cysts of the medial talar dome (OLT stage V, Bristol classification) in frontal, sagittal, and axial views. (B) MRI of the same patient 10 months after ECD, demonstrating absence of former bone edema and bony ingrowth with remodelling of drill tunnel and former OLT.
Discussion
Advanced Core Decompression is a technique for treatment of avascular necrosis of the femoral head, which is characterized by removal of the affected tissue and filling of the defect zone and drill tunnel with an injectable bone graft to achieve bone remodelling and biomechanical stability [9]. The aim of the ECD described in the current study is to transfer this technique from the hip to the ankle joint for treatment of osteochondral defects. Due to the different anatomy of the ankle joint, it was necessary to modify the technique. For optimal access to the defect zone we use arthroscopic visualization and guidance throughout the procedure. Arthroscopically, the OLT can be easily located by probing the softened cartilage layer covering the defect, and with the aid of a drill guide, retrograde drilling can be accomplished with high precision. Visualization in the drill meatus offers maximum control over the debriding instrument, preventing damage to the cartilage layer, and helps to accomplish complete removal of the necrotic bone area. After debridement, the created talar defect is filled with an injectable, hard-setting bone graft substitute.
In our cohort, radiographic follow-up imaging revealed remodelling of the bone graft substitute within 12 weeks and showed a good restoration of the medial talar dome contour. Vague contours of the drill meatus and the former OLT remained for more than 12 months in the MRI images. Corresponding to the promising radiographic results, all patients treated with the ECD showed significant pain relief reflected in an improvement in the AOFAS and FADI scores.
To date, there is no established treatment strategy for OLT [10–13]. The ECD competes with other techniques of bone marrow stimulation. Lesion diameter, depth, and patient age have been found to be prognostic factors in bone marrow stimulation techniques [14–16]. Abrasive treatment and bone marrow stimulation in OLT larger than 100 mm2 often lead to persistent pain and the need for follow-up surgery with restoration of the medial talar dome contour by osteochondral transplantation or cancellous bone grafting. The lesion size best suited for treatment with arthroscopic bone marrow stimulation has not been defined [17]. However, Chuckpaiwong et al. determined a critical defect size of 15 mm and found poor results after bone marrow stimulation exceeding this size [16]. Choi et al. also evaluated the effect of lesion size on clinical outcome in 117 patients and found the lowest clinical failure rate to be associated with a defect area of <100 mm2, whereas defects >150 mm2 showed only poor results [15].
An OLT is most likely to consist of an ellipsoid; therefore, 3D geometry and depth or volume of the lesion should also be taken into consideration. Angthong et al. postulate that defect depth is another prognostic factor determining clinical outcome. In their study, in which they treated 50 patients by debridement, drilling and/or micro-fracturing, they observed unsatisfactory results in lesions with a depth of more than 7.8 mm [14].
It must be noted that the mean OLT defect size in our cohort treated with the ECD procedure was 136.6±25.9 mm2. The cohort included 3 cases with defects exceeding the critical size of 150 mm2 (150, 165, and 170 mm2). Moreover, all the treated lesions exceeded the critical depth of 7.8 mm, having an average defect depth of 9.3±1.6 mm. We have not seen any influence of patient age on clinical outcome.
The first results of the ECD have been encouraging. In our hands, the technique combines a minimally invasive approach with radical debridement of the necrotic subchondral bone area. In contained lesions the procedure showed excellent results even in OLT larger than 150 mm2 or more than 7.8 mm in depth.
We believe that clinical outcome depends not only on lesion size and depth but also on the amount of necrotic OLT tissue removed, especially in larger lesions. Due to the osteoconductive characteristics of the bone graft substitute used for ECD, full excision of the necrotic OLT tissue is mandatory to achieve good bone remodelling. For bony ingrowth, the graft substitute has to be surrounded by healthy bone. With the ECD a minimally invasive technique is available even for the treatment of larger OLT exceeding the critical defect size, which limits classical bone marrow stimulation techniques. Nevertheless, these promising results have to be confirmed in a larger patient cohort.
Conclusions
The major advantage of our operative technique is the minimally invasive approach, endoscopically-guided radical excision of the necrotic subchondral bone tissue, and simple defect filling with a stable osteoconductive bone graft substitute aiming for restoration of the talar dome contour.
The ECD procedure could therefore be an alternative treatment option, not only for debridement and bone marrow stimulation, but also for an OATS procedure or cancellous bone grafting in larger OLT stages II, III, or V according to the Bristol classification [8].
Acknowledgements
One of the authors is a consultant at Wright Medical Technology™, Inc. Arlington, TN, USA.
Footnotes
Source of support: Departmental sources
References
- 1.Li R, Guo G, Chen B, et al. Arthroscopically-assisted reduction and fixation of an old osteochondral fracture of the lateral femoral condyle. Med Sci Monit. 2012;18(12):CS117–20. doi: 10.12659/MSM.883637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGoldrick NP, McGoldrick FJ. Avascular Necrosis of the metacarpal head: A case of Dietrich’s disease and review of the literature. Am J Case Rep. 2015;16:12–15. doi: 10.12659/AJCR.892389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Draper SD, Fallat LM. Autogenous bone grafting for the treatment of talar dome lesions. J Foot Ankle Surg. 2000;39(1):15–23. doi: 10.1016/s1067-2516(00)80059-9. [DOI] [PubMed] [Google Scholar]
- 4.Hangody L, Kish G, Modis L, et al. Mosaicplasty for the treatment of osteochondritis dissecans of the talus: two to seven year results in 36 patients. Foot Ankle Int. 2001;22(7):552–58. doi: 10.1177/107110070102200704. [DOI] [PubMed] [Google Scholar]
- 5.Zengerink M, Szerb I, Hangody L, et al. Current concepts: treatment of osteochondral ankle defects. Foot Ankle Clin. 2006;11(2):331–59. vi. doi: 10.1016/j.fcl.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Conti SF, Taranow WS. Transtalar retrograde drilling of medial osteochondral lesions of the talar dome. Operat Tech Orthop. 1996;6:226–30. [Google Scholar]
- 7.Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: A revised classification. Foot Ankle Int. 1999;20(12):789–93. doi: 10.1177/107110079902001206. [DOI] [PubMed] [Google Scholar]
- 8.Pritsch M, Horoshovski H, Farine I. Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1986;68(6):862–65. [PubMed] [Google Scholar]
- 9.Landgraeber S, Theysohn JM, Classen T, et al. Advanced core decompression, a new treatment option of avascular necrosis of the femoral head – a first follow-up. J Tissue Eng Regen Med. 2013;7(11):893–900. doi: 10.1002/term.1481. [DOI] [PubMed] [Google Scholar]
- 10.Giannini S, Vannini F. Operative treatment of osteochondral lesions of the talar dome: current concepts review. Foot Ankle Int. 2004;25(3):168–75. doi: 10.1177/107110070402500311. [DOI] [PubMed] [Google Scholar]
- 11.Loveday D, Clifton R, Robinson A. Interventions for treating osteochondral defects of the talus in adults. Cochrane Database Syst Rev. 2010;(8):CD008104. doi: 10.1002/14651858.CD008104.pub2. [DOI] [PubMed] [Google Scholar]
- 12.van Bergen CJ, de Leeuw PA, van Dijk CN. Treatment of osteochondral defects of the talus. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8 Suppl):398–408. doi: 10.1016/j.rco.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Zwingmann J, Sudkamp NP, Schmal H, Niemeyer P. Surgical treatment of osteochondritis dissecans of the talus: a systematic review. Arch Orthop Trauma Surg. 2012;132(9):1241–50. doi: 10.1007/s00402-012-1544-1. [DOI] [PubMed] [Google Scholar]
- 14.Angthong C, Yoshimura I, Kanazawa K, et al. Critical three-dimensional factors affecting outcome in osteochondral lesion of the talus. Knee Surg Sports Traumatol Arthroscopy. 2013;21(6):1418–26. doi: 10.1007/s00167-013-2364-8. [DOI] [PubMed] [Google Scholar]
- 15.Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: Is there a critical defect size for poor outcome? Am J Sports Med. 2009;37(10):1974–80. doi: 10.1177/0363546509335765. [DOI] [PubMed] [Google Scholar]
- 16.Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008;24(1):106–12. doi: 10.1016/j.arthro.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 17.Murawski CD, Kennedy JG. Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 2013;95(11):1045–54. doi: 10.2106/JBJS.L.00773. [DOI] [PubMed] [Google Scholar]