Abstract
Background:
Indigenous populations are disproportionately affected by traumatic brain injury. These populations rely on large jurisdiction surveillance efforts to inform their prevention strategies, which may not address their needs. We examined the incidence and determinants of traumatic brain injury in an indigenous population in the Terres-Cries-de-la-Baie-James health region of the province of Quebec and compared them with the incidence and determinants in 2 neighbouring health regions and in the province overall.
Methods:
We conducted a retrospective population-based cohort study of patients in Quebec admitted to hospital with incident traumatic brain injury, stratified by health region (Terres-Cries-de-la-Baie-James, Nunavik and Nord-du-Québec), from 2000 to 2012. We used MED-ÉCHO administrative data for case-finding. A subgroup analysis of adults in the Terres-Cries-de-la-Baie-James health region was completed to assess determinants of the severity of traumatic brain injury and patient outcomes.
Results:
A total of 172 hospital admissions for incident traumatic brain injury occurred in the Terres-Cries-de-la-Baie-James region during the study period. The incidence was 92.1 per 100 000 person-years, and the adjusted incidence rate ratio was 1.84 (95% confidence interval 1.56-2.17) compared with the entire province. The incidence was higher than in the neighbouring nonindigenous population (Nord-du-Québec) but significantly lower than in the neighbouring indigenous population (Nunavik). Determinants of traumatic brain injury in the Terres-Cries-de-la-Baie-James region differed from those in the neighbouring populations and in the entire province.
Interpretation:
We found that the incidence rates and determinants of traumatic brain injury requiring hospital admission varied greatly between the three regions studied. Community-based surveillance efforts should be encouraged to inform the development of relevant prevention strategies.
The incidence of traumatic brain injury varies in populations around the globe. Rural populations tend to have a higher incidence and worse outcomes than urban populations.1,2 In Canada, the poorer health status of indigenous peoples compared with the general population has been described.3,4 Injuries are the leading cause of potential years of life lost in this indigenous population, with rates 4 times higher than in the rest of Canada.5,6 More specifically, traumatic brain injury accounts for a substantial proportion of injuries in indigenous North American populations.7-10 These populations have different risk factors related to the occurrence of trauma compared with other Canadians.11-14 Given that the determinants of traumatic brain injury and patient outcomes differ between indigenous populations, surveillance conducted on a community-specific basis can provide evidence that informs relevant prevention strategies for these communities.3,15 However, most surveillance efforts are conducted at the larger jurisdiction level. For example, in 2012, the Institut national de santé publique du Québec completed a provincial surveillance study of nonintentional traumatic brain injury requiring hospital admission and analyzed data stratified by different health regions.16 The report concluded that falls were the dominant mechanism of traumatic brain injury and that prevention strategies in the province should be informed by the evidence generated through this type of surveillance effort. However, the 2 northern health regions in Quebec that represent indigenous communities (Nunavik, and Terres-Cries-de-la-Baie-James, which serves the Cree of Eeyou Istchee) and a nonindigenous region in the same geographic area (Nord-du-Québec) were excluded from their analysis.
The primary aim of our study was to compare the incidence rates and determinants of traumatic brain injury requiring hospital admission in the Eeyou Istchee communities with those in the neighbouring indigenous (Nunavik) and nonindigenous (Nord-du-Québec) populations. A second aim of our study was to describe the severity, risk factors, functional outcomes and use of rehabilitation resources among adults with traumatic brain injury in Eeyou Istchee. The evidence generated from this analysis, which may differ from the conclusions of a recent province-wide (large jurisdiction) surveillance effort, would then be used to inform relevant prevention strategies for the Cree communities of Eeyou Istchee.
Methods
Study design, population and setting
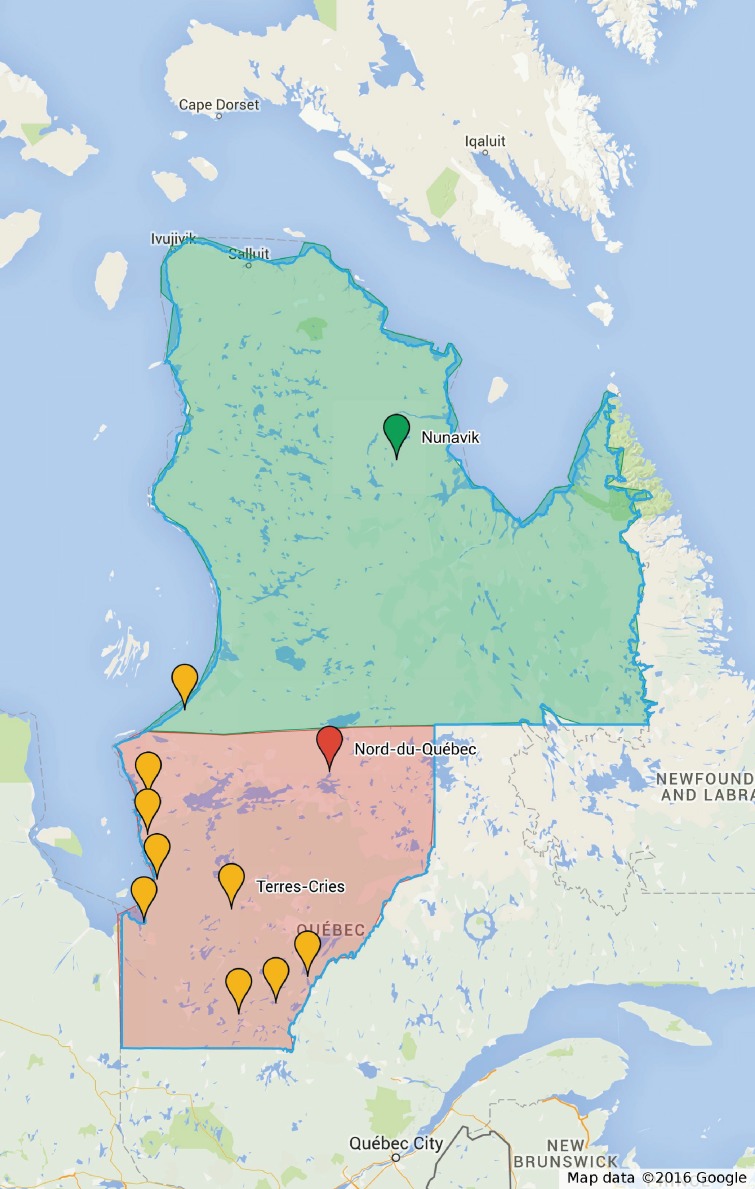
We conducted a population-based retrospective study of all hospital admissions for incident traumatic brain injury in the Terres-Cries-de-la-Baie-James health region of Quebec, which represents patients from a single indigenous population (Eeyou Istchee), from 2000 to 2012. The epidemiologic descriptions of 2 neighbouring health regions (Nunavik, serving a predominantly Inuit population, and Nord-du-Québec, serving a predominantly nonindigenous population) and the rest of the province were used as comparison populations (Figure 1).17,18
Figure 1.
Map of Quebec showing the Terres-Cries-de-la-Baie-James, Nunavik and Nord-du-Québec health regions. The Terres-Cries-de-la-Baie-James health region has 9 communities (yellow pins) that are nested mainly within the Nord-du-Québec region (shaded in red). The northernmost community of the Terres-Cries-de-la-Baie-James is nested within Nunavik (shaded in green). The map was produced with the use of Google My Maps using Google's map data. The map is being reproduced under the terms set out by Google.17
The Terres-Cries-de-la-Baie-James comprises 8 rural Cree communities and 1 remote community within the drainage basin of the James Bay in Quebec and the southern Hudson Bay (Appendix 1, available at www.cmajopen.ca/content/4/2/E249/suppl/DC1). These communities are nested within the Nord-du-Québec and Nunavik health regions (Figure 1). More specifically, the boundaries of the Terres-Cries-de-la-Baie-James health region are different from those of the Cree-controlled territories that form the traditional lands of Eeyou Istchee. The Cree Board of Health and Social Services of James Bay, a Cree-Quebec institution created through the James Bay and Northern Quebec Agreement (1975),18 is responsible for the regional health administration of the Terres-Cries-de-la-Baie-James health region within the provincial Ministry of Health and Social Services. The Cree Board of Health and Social Services of James Bay is an ethnically based governmental organization serving everyone residing or visiting within the Cree communities of Eeyou Istchee.
Data sources
For case-finding, we used MED-ÉCHO, a provincial database that records the hospital admissions of all Quebec residents covered by public health insurance. The province provides public health care coverage for more than 7.7 million people (> 93% of its residents).19 The database used the International Classification of Disease, ninth revision (ICD-9) coding scheme from 2000 to 2005; since then, it has used the Canadian version of the International Statistical Classification of Diseases and Related Health Problems (ICD-10-CA). MED-ÉCHO has been shown to be valid and reliable in ascertaining data on hospital admissions for various diagnoses.20,21 The ICD-9 and ICD-10-CA codes typically detect admissions for traumatic brain injury with a sensitivity of 45%-78% and a specificity of 97%.22
Case definitions
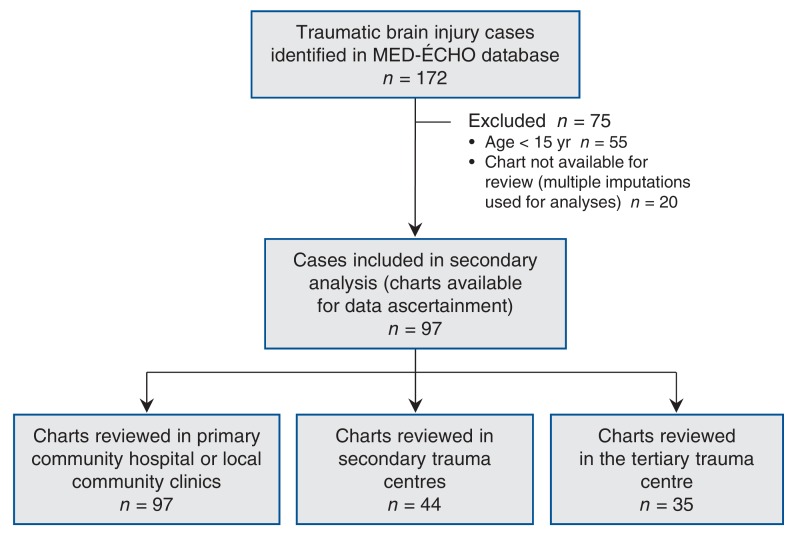
For the primary analysis, we used the same case definition for traumatic brain injury as that used by the Institut national de santé publique du Québec to allow comparison of surveillance data with the rest of the province (Appendix 2, available at www.cmajopen.ca/content/4/2/E249/suppl/DC1).16 We also included cases of intentional traumatic brain injury in this analysis because assaults are known to be a prominent mechanism of injury in indigenous communities.6 Because severity of traumatic brain injury and patient outcomes are not assessed in the same manner in pediatric and adult populations, and because these injuries predominantly affect young adults in indigenous communities, we conducted a secondary analysis involving adults (age ≥ 15 yr) in the Terres-Cries-de-la-Baie-James region.23 These patients' charts were reviewed at all of the hospitals and clinics where they were treated for the incident head injury (Figure 2 and Appendix 1).
Figure 2.
Selection of cases for the secondary analysis. For the primary analysis, the MED-ÉCHO administrative database was used for case-finding. For the secondary analysis, charts were reviewed at local community clinics. If patients were transferred numerous times between institutions (see Appendix 1, available at www.cmajopen.ca/content/4/2/E249/suppl/DC1), up to 3 different charts for a single patient were reviewed in separate institutions.
Measured variables
The variables ascertained from MED-ÉCHO included the patient's age, sex, length of hospital stay, external cause of injury (mechanism of injury), primary and secondary diagnoses in the hospital chart, and the patient's health region/current municipality of origin. The external mechanisms of injury were coded as per the ICD-9 and ICD-10-CA classifications (Appendix 2).16
Additional variables ascertained through the chart review were used to address the secondary objectives of the study. These variables included the earliest initial post-resuscitation Glasgow Coma Scale score, specific use of protective equipment (seatbelt or helmet), polytrauma status (defined as traumatic injury to a body region besides the head), comorbidity status (2 or more of diabetes mellitus, dyslipidemia, hypertension, coronary artery disease, history of stroke or psychiatric illness), use of rehabilitation services and any status of intoxication with alcohol (as reported by the chart note of the first physician assessment). We classified the severity of injury based on the earliest recorded Glasgow Coma Scale score after resuscitation: mild (score of 3-15), moderate (9-12) or severe (3-8).24 We assessed functional outcomes using the first Glasgow Outcome Scale scores at least 6 months after the injury.25 These scores were ascertained from the patients' local community charts. A score of 3 was assigned to patients with severe disability who were unable to live independently; a score of 4 was assigned to patients with residual neurologic or psychological deficits who were independent but had not returned to their pre-injury functioning; and a score of 5 was assigned to patients with minor deficits who had returned to their pre-injury functioning. No patients died (score of 1) or entered a vegetative state (score of 2) as a result of their injuries. If no Glasgow Outcome Scale score was recorded, the chart extractor assigned one by interpreting the patients' clinical evolution (based on follow-up notes in the chart) 6 months after the injury.
The chart review was conducted by one reviewer (O.L.), who had more than 5 years of experience as a neurosurgery resident and had training in epidemiology and biostatistics. A validation of the chart abstraction for a subset of patients (35/97 [36%]) was completed by using the traumatic brain injury registry of the level 1 trauma centre that serves the Terres-Cries-de-la-Baie-James region exclusively for head injuries. The registry includes information on the age, sex, initial Glasgow Coma Scale score and Glasgow Outcome Scale score based on a consensus agreement between various health professionals treating the patients. The kappa statistic for interrater agreement was measured for each variable ascertained in the chart review.
Statistical analysis
The denominator for the traumatic brain injury incidence calculation was determined through census data provided by the Statistical Institute of Quebec and the Ministry of Health and Social Services.16,26,27 The incidence rates were standardized to the 1991 Quebec population structure, as was done in the province-wide surveillance project.16 We calculated adjusted incidence rate ratios using negative binomial models (because the variance and mean of counts were not equal) between the study population and the 3 referent populations, while controlling for age, sex and year of injury.
We assessed the association between different mechanisms of traumatic brain injury and the 3 geographic zones of the Terres-Cries-de-la-Baie-James region (coastal, inland and remote), which are described below. For this analysis, we used 2 Poisson regression models with a robust variance estimator to estimate risk ratios (RRs). The methodology behind this approach has been previously described.28 We also assessed the association between mechanisms of injury and health region using a multinomial regression model.
For the secondary objectives, we used 6 regression models to assess the association of risk factors with the occurrence or outcome of traumatic brain injury. These associations were established before the start of the study to determine whether injury severity, outcome and use of rehabilitation services were associated with modifiable risk factors in the Terres-Cries-de-la-Baie-James communities. Model assumptions were verified in each instance (linear regression model assumptions and the proportional odds assumption for cumulative odds regression models). Known confounders of the associations under investigation were adjusted for in the models. The Akaike Information Criterion was used to assess model fit. Covariates were removed from models when model fit was improved and when the estimate of the main association under investigation remained unchanged. Age categories were used in this analysis because model fit was better than when continuous covariates were used. All-terrain vehicle collisions and snowmobile collisions were grouped as off-road vehicle collisions for the same reason. The age categories that we used were in keeping with those used by the recent provincial surveillance project on traumatic brain injury.16
The Terres-Cries-de-la-Baie-James communities were stratified based on their geographic location as coastal, inland (rural and semi-remote) or remote. We did this because the communities in each category have similar built environments (coastal communities are on the James Bay coast and have distant access to the provincial network of roadways; inland communities are substantially closer to the provincial network of roadways and are not on the James Bay coast; and the remote community's roadways are not connected to provincial roadways) (Figure 1 and Appendix 1).
R version 3.0.3 for Mac OS X (R Foundation for Statistical Computing) and Stata version 12.0 for Mac OS X (StataCorp) statistical software were used for all data analyses.
Missing data
For the primary analysis, data on mechanism of injury were missing only for the province as a whole and only in a small proportion of cases (6.6%). Although the missing data mechanism was unknown, we believe that missing data were related to the age of individuals. The average age of patients with missing data was 64.8 years, as compared with 44.6 years for patients without missing data. The imputation model for this analysis included age, sex and year of injury.
For the secondary analysis, the missing data mechanism was not clear. Missing data were the result of charts not being accessible for review. There were no significant differences in variables that were measured in all patients when stratified by patients with complete data and by those with missing data. Archivists at the various hospitals where the chart review was conducted were unable to elaborate on why some charts were not accessible. The imputation model for this analysis included age, year of injury, geographic zone of injury and mechanism of injury, since the missing data had a subtle but nonsignificant association to these variables.
For both analyses, we applied a multiple imputation technique with chained equations using 20 data sets and 10 iterations per data set. These results were compared with those from the complete-case analyses. Given the above, data were assumed to be missing at random after using imputation models that at least partially accounted for the missing data mechanism.29 All regression models used pooled estimates of the imputed data sets.
Sensitivity analysis
Because the study was conducted in rural and remote populations, there was the possibility that more hospital admissions for milder injuries occurred in those regions than in urban centres, where hospital beds are proportionately more limited for a larger population. Thus, we completed a sensitivity analysis by measuring the proportion of admissions that were for mild, moderate and severe traumatic brain injury in the urban health region of Montréal and compared them with the proportion of such injuries in the Terres-Cries-de-la-Baie-James health region. A provincial policy mandates that every patient in the Montréal region who resides within the catchment area of the level 1 trauma centre and has a diagnosis of moderate or severe traumatic brain injury be admitted to this specialized centre.30 We identified such patients from information in the traumatic brain injury database used in the chart review validation and in the MED-ÉCHO database. A χ2 test for independence (significance level < 0.05) was used to establish whether patients admitted to hospital with traumatic brain injury from the Terres-Cries-de-la-Baie-James region had injuries similar in severity to those of patients from Montréal.
Ethics approval
The Institutional Research Ethics Board of McGill University approved the study design. The study conformed to the Tri-Council Policy Statement on Ethical Conduct for Research Involving Humans, in particular research involving First Nations, Inuit and Métis peoples.31 Each hospital where a chart review was completed had authorization from their director of professional services. The Public Health Department of the Cree Board of Health and Social Services of James Bay partnered with the study, which was approved by the Public Health Management Committee. The study findings were widely shared with community members, stakeholders and organizations through various media.
Results
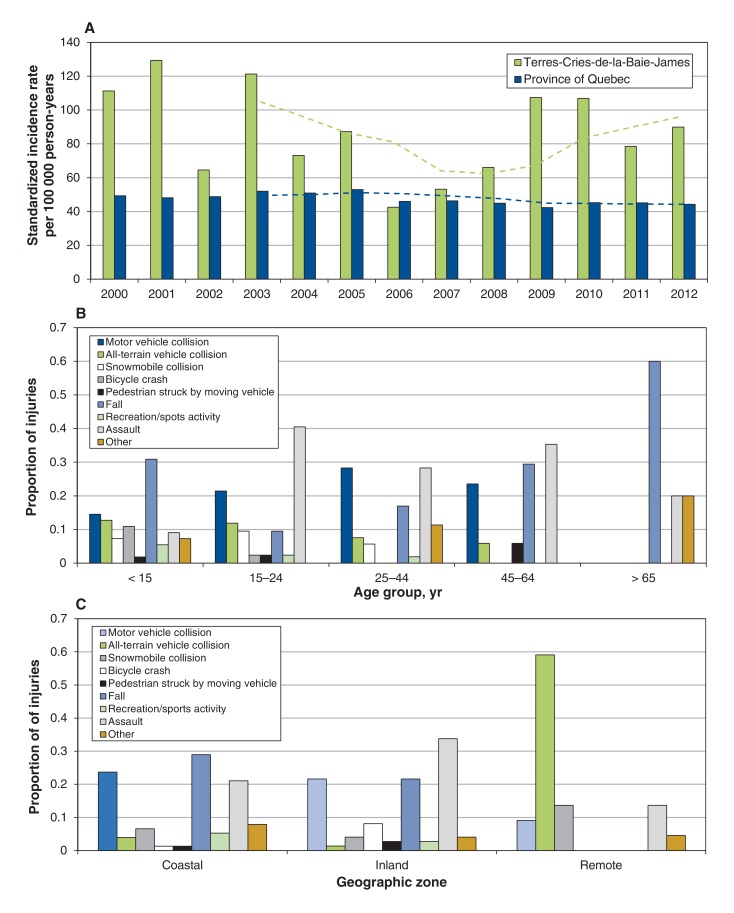
A total of 172 hospital admissions for incident traumatic brain injury occurred in the Terres-Cries-de-la-Baie-James region from 2000 to 2012, for a crude incidence rate of 92.1 per 100 000 person-years (Table 1). Mechanisms of injury were mainly related to assaults, followed by falls, motor vehicle collisions and off-road vehicle collisions. For most years, the standardized incidence rates in the Terres-Cries-de-la-Baie-James region were higher than the provincial average (Figure 3A). The remote community in the Terres-Cries-de-la-Baie-James region had the highest crude incidence rate, followed by the coastal and inland communities (Table 1). The distribution of mechanisms of injury varied by age group, with falls being the most common mechanism in the youngest and oldest groups (Figure 3B). After adjustment for relevant confounders, Nunavik had the highest incidence rate ratio, followed by the Terres-Cries-de-la-Baie-James and Nord-du-Québec regions (Table 1).
Table 1: Summary statistics and incidence rates of hospital admissions for traumatic brain injury in the Terres-Cries-de-la-Baie-James health region and referent populations in the province of Quebec, 2000-2012.
| Analysis by health region and entire province | ||||
|---|---|---|---|---|
| Variable | Terres-Cries-de-la-Baie-James | Nunavik | Nord-du-Québec | Province of Quebec |
| No. of hospital admissions for traumatic brain injury | 172 | 469 | 154 | 50 362 |
| Age, yr | ||||
| Mean ± SD | 24.63 ± 18.03 | 23.42 ± 16.28 | 35.82 ± 24.44 | 45.93 ± 29.20 |
| Range | 0-80 | 0-86 | 0-98 | 0-106 |
| Sex, no. (%) of patients | ||||
| Male | 113 (65.7) | 255 (54.4) | 100 (64.9) | 32 041 (63.6) |
| Female | 59 (34.3) | 214 (45.6) | 54 (35.1) | 18 321 (36.4) |
| Mechanism of injury, no. (%) of patients | ||||
| Assault | 44 (25.6) | 76 (16.2) | 8 (5.2) | 1 866 (3.7) |
| Fall | 38 (22.1) | 72 (15.4) | 57 (37.0) | 24 086 (47.8) |
| Motor vehicle collision | 36 (20.9) | 41 (8.7) | 31 (20.1) | 9 129 (18.1) |
| All-terrain vehicle collision | 17 (9.9) | 173 (36.9) | 15 (9.7) | 1 243 (2.5) |
| Snowmobile collision | 11 (6.4) | 17 (3.6) | 2 (1.3) | 150 (0.3) |
| Bicycle crash | 7 (4.1) | 9 (1.9) | 8 (5.2) | 2 851 (5.7) |
| Pedestrian struck by moving vehicle | 3 (1.7) | 24 (5.1) | 4 (2.6) | 2 365 (4.7) |
| Motorcycle collision | 0 (0) | 12 (2.6) | 0 (0) | 841 (1.7) |
| Recreation/sports activity | 6 (3.5) | 2 (0.4) | 1 (0.6) | 326 (0.6) |
| Other | 10 (5.8) | 43 (9.2) | 28 (18.2) | 4 202 (8.3) |
| Missing data* | - | - | - | 3 303 (6.6) |
| Total no. of population person-years | 186 581 | 142 059 | 198 786 | 100 545 876 |
| Crude incidence per 100 000 person-years [not standardized] | 92.1 | 330.2 | 77.5 | 50.1 |
| Adjusted IRR† (95% CI) | 1.84 (1.56-2.17) | 6.82 (606-7.65) | 1.65 (1.30-1.83) | 1.00 (Referent) |
| Analysis by geographic zone of the Terres-Cries-de-la-Baies-James region | ||||
| Crude incidence per 100 000 person-years | 72.0 | 95.5 | 200.0 | |
| Adjusted IRR† (95% CI) | 1.00 (Referent) | 1.32 (0.96-1.82) | 2.73 (1.64-4.27) | |
Note: CI = confidence interval, IRR = incidence rate ratio.
*Missing data were present only for province-wide data on mechanisms of injury and only represented a small proportion (6.6%).
†Calculated using a negative binomial regression model. Adjusted for age, sex and year of injury.
Figure 3.
Annual incidence of hospital admissions for traumatic brain injury, and descriptive statistics on mechanisms of injury, in the Terres-Cries-de-la-Baie-James region compared with the entire province of Quebec. (A) Incidence rates per 100 000 person-years standardized to the 1991 provincial population. A 4-year moving average of the incidence rates is also shown. (B) Mechanisms of injury by age group. (C) Mechanisms of injury by geographic zone.
The multinomial regression revealed that assaults were more strongly associated with traumatic brain injury hospital admission occurring in the Terres-Cries-de-la-Baies-James and Nunavik regions than in Nord-du-Québec and the rest of the province. All-terrain vehicle collisions were significantly more often associated with traumatic brain injury hospital admission in Nunavik than in the other health regions. The Terres-Cries-de-la-Baie-James and Nord-du-Québec regions had similar relative probability ratios for these collisions, which were higher than for the entire province (Table 2 and Appendix 3 available at www.cmajopen.ca/content/4/2/E249/suppl/DC1). Snowmobile collisions were most strongly associated with traumatic brain injury in the Terres-Cries-de-la-Baie-James and Nunavik regions compared with the entire province. Also, off-road vehicle collisions were more common in the remote community than in the inland and coastal communities (Figure 3C and Appendix 4, available at www.cmajopen.ca/content/4/2/E249/suppl/DC1).
Table 2: Association between mechanism of injury leading to traumatic brain injury hospital admission and health regions (multinomial regression)*.
| Region; mechanism of injury |
Relative probability ratio (95% CI) |
|---|---|
| Nord-du-Québec | |
| Assault | 1.20 (0.55-2.62) |
| All-terrain vehicle collision | 3.50 (1.88-6.52) |
| Snowmobile collision | 3.76 (0.89-15.89) |
| Nunavik | |
| Assault | 11.01 (7.40-16.40) |
| All-terrain vehicle collision | 38.06 (24.93-51.79) |
| Snowmobile collision | 31.39 (17.07-57.72) |
| Terres-Cries-de-la-Baie-James | |
| Assault | 8.70 (5.28-14.33) |
| All-terrain vehicle collision | 5.01 (2.66-9.42) |
| Snowmobile collision | 27.11 (12.98-56.59) |
Note: CI = confidence interval.
*The referent population is the entire province of Quebec, and the referent mechanism of injury is falls. Multiple imputations were used for missing data on mechanisms of injury. Only significant differences in the relative probability ratios are shown. The model was adjusted for age and sex. A complete-case analysis regression output, which shows similar results, is shown in Appendix 3 (available at www.cmajopen.ca/content/4/X/E249/suppl/DC1).
There were 117 incident traumatic brain injury hospital admissions involving individuals 15 years of age or more in the Terres-Cries-de-la-Baie-James health region between 2000 and 2012. Table 3 summarizes the findings for this subgroup. Table 4 summarizes the important associations that were measured through various regression models. Patients in the remote community had more severe injuries than those in the other communities in the Terres-Cries-de-la-Baie-James region. Individuals who used protective equipment tended to have less severe injuries and had a better outcome, as assessed by the Glasgow Outcome Scale score. Patients involved in motor vehicle collisions had a higher probability of receiving rehabilitation than those with a mechanism of fall or assault (Appendices 5 and 6, available at www.cmajopen.ca/content/4/2/E249/suppl/DC1). The results from complete-case analyses were similar (Appendix 7, available at www.cmajopen.ca/content/4/2/E249/suppl/DC1).
Table 3: Summary statistics for subgroup analysis of adults (≥ 15 yr) in the Terres-Cries-de-la-Baie-James region admitted to hospital with traumatic brain injury.
| Variable | No. (%) of patients* n = 117 |
|---|---|
| Initial post-resuscitation Glasgow Coma Scale score | n = 97 |
| Mean ± SD | 13.7 ± 2.3 |
| Range | 3-15 |
| Injury severity (Glasow Coma Scale range) | n = 97 |
| Mild (13-15) | 81 (83.5) |
| Moderate (9-12) | 7 (7.2) |
| Severe (3-8) | 9 (9.3) |
| Polytrauma | n = 97 |
| Yes | 43 (44.3) |
| No | 54 (55.7) |
| Rehabilitation | n = 97 |
| In-patient | 12 (12.4) |
| Out-patient (in community) | 22 (22.7) |
| Discharge orientation | n = 97 |
| Home | 83 (85.6) |
| Rehabilitation (in-patient) | 12 (12.4) |
| Deceased | 0 (0) |
| Long-term care | 0 (0.0) |
| Other hospital centre | 2 (2.1) |
| Glasgow Outcome Scale score | n = 97 |
| 1 | 0 (0) |
| 2 | 0 (0) |
| 3 | 14 (14.4) |
| 4 | 52 (53.6) |
| 5 | 31 (32.0) |
| No. of outcome scores assigned by data extractor from interpretation of chart | 45 (46.4) |
| Protective equipment used‡ | n = 41 |
| Yes | 11 (26.8) |
| No | 30 (73.2) |
| Intoxication with alcohol | n = 97 |
| Yes | 43 (44.3) |
| No | 54 (55.7) |
| Missing data† | 20 (17.1) |
*Unless stated otherwise.
†A total of 20 cases had missing data for the Glasgow Coma Scale score, Glasgow Outcome Scale score, polytrauma status, use of rehabilitation services and intoxication status. Multiple imputation using chained equations was used for these missing data, and all regression analyses used the pooled data from the imputations.
‡Specific to motor vehicle, off-road vehicle and bicycle crashes.
Table 4: Summary of regression models used in secondary analysis to assess associations between risk factors for traumatic brain injury and injury severity, functional outcome and use of rehabilitation services*.
| Outcome; contrast (regression type) | Association measure (95% CI) | Interpretation |
|---|---|---|
| Injury severity | ||
| Remote v. inland geographic zone (linear) |
Beta -2.31 (-4.14 to -0.47) | Living in a remote community was associated with higher injury severity (initial GCS score) |
| Protective equipment use (linear) |
Beta 1.19 (-0.30 to 2.69) | Although effect size was not statistically significant, it suggests that use of protective equipment was associated with lower injury severity (initial GCS score) |
| Functional outcome | ||
| Protective equipment use (proportional odds) |
OR 4.79 (1.12 to 20.48) | Use of protective equipment was associated with better functional outcomes (6-mo GOS score) |
| Initial GCS score (proportional odds) |
OR 1.80 (1.35 to 2.39) | Higher initial GCS score was associated with better functional outcomes (6-mo GOS score) |
| Use of rehabilitation services | ||
| Initial GCS score (Poisson with robust variance) |
RR 0.82 (0.70 to 0.95) | Lower initial GCS score was associated with greater use of rehabilitation services |
| Motor-vehicle collision v. fall (Poisson with robust variance) |
RR 2.91 (1.04 to 8.17) | Being involved in a motor vehicle collision was associated with greater use of rehabilitation services |
Note: CI = confidence interval, GCS = Glasgow Coma Scale, GOS = Glasgow Outcome Scale, OR = odds ratio, RR = risk ratio.
*Depending on the model selection results, the following covariates were included in the models: age, sex, initial GCS score, 6-mo GOS score, comorbid conditions, geographic zone, use of rehabilitation services, use of protective equipment, polytrauma status, year of injury and alcohol intoxication status. Appendix 7 (available at www.cmajopen.ca/content/4/2/E249/suppl/DC1) shows the full regression model outputs for each of these multiple imputation regression models, along with complete-case regression model outputs for comparison.
The interrater agreement between the chart review and the traumatic brain injury database had a kappa value of greater than 0.9 for all variables except the Glasgow Outcome Scale scores. For the latter, the kappa value was 0.86 (bootstrapped 95% CI 0.67-1.00), which included 18 charts in which the Glasgow Outcome Scale score was not recorded (the chart abstractor assigned the score based on clinical notes).
The proportions of patients admitted to hospital with mild, moderate and severe traumatic brain injury in the Terres-Cries-de-la-Baie-James and Montréal regions were similar (p = 0.8). The comparison of hospital admission rates between the rural setting and the rest of the province appeared justified (Appendix 8, available at www.cmajopen.ca/content/4/2/E249/suppl/DC1).
Interpretation
Our study showed that the incidence of hospital admission for traumatic brain injury in the province of Quebec differed from the incidence in the rural indigenous (Terres-Cries-de-la-Baie-James and Nunavik) and rural nonindigenous (Nord-du-Québec) communities that we studied. The rates were higher in the rural communities, and the mechanisms of injury differed significantly from those in the entire province. The detailed analysis of adults living in the Terres-Cries-de-la-Baie-James region provided a better understanding of traumatic brain injury prevention strategies that would be useful to this community, in addition to identifying inequalities in access to health care resources. Furthermore, the determinants of traumatic brain injury in the Terres-Cries-de-la-Baie-James communities differed substantially from those described in a province-wide surveillance initiative.16 Thus, relying on large-jurisdiction surveillance efforts to describe the determinants of traumatic brain injury in indigenous communities can be misleading.
The heterogeneity of traumatic brain injury epidemiology between populations has been reported in various jurisdictions. This heterogeneity has been attributed to varying case definitions, data sources and risk factors related to these injuries.32-35 For example, the provinces of Ontario and Quebec completed surveillance studies on traumatic brain injury hospital admissions using similar ICD coding methodology.16,36 Their rates tended to decrease over a decade and to be no higher than 83.4 cases per 100 000 person-years. In contrast, the rates in the Terres-Cries-de-la-Baie-James communities were consistently higher than the provincial rate and did not decrease over time (Figure 3A).9,16,36 Because our surveillance methodology was nearly identical to the Ontario and Quebec surveillance studies, the main variation is likely due to differing risk factors in these populations. Furthermore, these 2 provincial surveillance studies each concluded that preventing falls is a priority for reducing traumatic brain injury burden across their populations. Although this recommendation may still be useful for the Terres-Cries-de-la-Baie-James population, it overlooks other important mechanisms of injury that could be the object of prevention strategies, such as assaults. Our analysis showed that assaults were more common in the indigenous communities than in the nonindigenous communities studied. Similarly, studies in the province of Alberta and in New Zealand found that the main causes of trauma among indigenous and nonindigenous populations varied, with assault being more common in the indigenous populations.6,13 In contrast, a study involving traumatic brain injury rehabilitation patients in Saskatchewan found no such association.8 Thus, the determinants of traumatic brain injury between indigenous communities are heterogeneous. Community-based surveillance is needed to properly identify these determinants. Moreover, although they were not the focus of our study, socioeconomic factors may have contributed to the differences we noted in the 2 indigenous populations.37
The detailed analysis of traumatic brain injury among adults in the Terres-Cries-de-la-Baie-James region was critical in understanding many determinants of injury severity and outcomes. First, living in the region's remote community was associated with the highest hospital admission rate and the most severe injuries. Previous research has shown that individuals living in rural environments are more prone to transport-related accidents, which was substantiated by our findings.38 Although mechanism of injury was controlled for, residual confounding of this association likely existed. The distance travelled and time spent on off-road vehicles in this remote community is likely higher because residents have no access to provincial roadways as they do in the coastal and inland communities. However, the remote community of the Terres-Cries-de-la-Baie-James region, set in the same remote environment as Nunavik, had lower rates of traumatic brain injury hospital admission. As noted above, there are probably other unmeasured cultural and social factors that play a role in the occurrence of traumatic brain injury in this population that go beyond the geographic environment.
Second, we found that use of protective equipment predicted a lower severity of injury and improved functional outcomes among the Terres-Cries-de-la-Baie-James adults, which is supported by findings from previous studies.39-41
Third, in our study, alcohol intoxication at the time of injury did not seem to be an important factor in terms of functional outcome (Table D of Appendix 7). Still, the precision of this estimate was poor, and firm conclusions cannot be drawn. Previous studies have shown that as many as 50% of traumatic brain injuries occur in the context of alcohol intoxication,42 which is not substantially different from the rate we reported of 44.3%. Still, alcohol use has been shown to be an important risk factor for traumatic brain injury recurrences, which ultimately lead to poorer functional outcomes.43 As such, addressing alcohol abuse remains important in our study population as it does in other populations, and further investigation on this topic is warranted.
Fourth, our analysis showed that milder injuries and younger age were associated with lesser use of rehabilitation services, which is to be expected. However, patients injured in motor vehicle collisions had a greater probability of receiving rehabilitation than those whose traumatic brain injury was due to an assault or fall. Identifying such an inequality in access to rehabilitation was possible with our community-based approach to surveillance. The latter is particularly important, because rehabilitation services, across the spectrum of traumatic brain injury severity, have been shown to improve patients' functional outcomes.44 These inequalities should be addressed with policies that encourage providers and the health care system to offer rehabilitation resources based on need.
Limitations
Our study has several limitations. Case-finding relied on ICD codes. Such codes have been known to be less sensitive for identifying cases of mild traumatic brain injury.45 Our analysis excluded fatal cases that occurred outside of hospital, which leads to more underestimation of incidence rates. Furthermore, we omitted hospital admissions with ICD-9 code 959.01 ("head injury, unspecified") so that our results would be comparable to those from a province-wide surveillance initiative.16
Our population had Glasgow Outcomes Scale scores from 3 to 5. Of the 97 patients with complete data, 45 (46%) did not have a recorded Glasgow Outcome Scale score. In these cases, the chart extractor interpreted clinical follow-up notes to establish the score. However, this method of assigning a score has not been validated. A score of 3 may be easy to differentiate from higher scores, but there may have been misclassification between scores of 4 and 5 because of subtleties that cannot be ascertained from a chart. If this misclassification were nondifferential, the magnitude of our association measures might be biased toward the null.
We standardized our incidence rates to the 1991 Quebec population structure to produce comparable estimates between our study and a previous province-wide surveillance project.16 The population structure of the Terres-Cries-de-la-Baie-James region differs substantially from the rest of the province; therefore, caution should be used in interpreting these rates on their own. However, the negative binomial regression that compared rates across populations did not rely on standardization to any specific population structure.
Missing data for the primary and secondary analyses were assumed to be missing at random because we adjusted for the missing data mechanism to the best of our knowledge. However, the possibility that data were missing not at random, which may be a source of bias in our results, should still be considered. In addition, residual confounding is likely to be an issue given that we were not able to account for all potential socioeconomic factors associated with traumatic brain injury that may vary between the populations studied.
Finally, generalizing our findings to other indigenous communities should be done with caution. Nonetheless, our study shows that community-based surveillance is needed to identify the heterogeneity in the incidence and determinants of traumatic brain injury that exists in different populations.
Conclusion
We found that the incidence rates and determinants of traumatic brain injury requiring hospital admission varied greatly between the three regions studied. Large-jurisdiction surveillance efforts may fail to properly describe the determinants of traumatic brain injury in indigenous and in rural nonindigenous communities. Community-based surveillance efforts should be encouraged in these communities so that evidence that informs relevant prevention strategies is available to them. This surveillance approach would set the stage for further research on the cultural and socioeconomic determinants of traumatic brain injury, which is critical for tailoring prevention strategies to individual communities.
Supplemental information
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/4/2/E249/suppl/DC1
Supplementary Material
Acknowledgements
The authors thank Pierre Lejeune from the Cree Board of Health and Social Services of James Bay for helping with data retrieval from the MED-ÉCHO database. In addition, the authors are grateful for all the time and effort that the archivists at each hospital contributed to retrieving charts used in the study.
Footnotes
Funding: Oliver Lasry was funded by the Canadian Institutes of Health Research (CIHR) through a Canada Graduate Scholarship. He also received funding by the Régie de l'assurance maladie du Québec/Ministère de la Santé et des Services sociaux du Québec through their Année Complémentaire program for residents enrolled in the Royal College of Physicians and Surgeons of Canada's Clinician-Investigator Program. In addition, Oliver Lasry received funding from the Cree Board of Health and Social Services of James Bay and McGill University's Faculty of Medicine to travel to the Cree communities and to complete the data ascertainment component of the study. Rebecca Fuhrer was funded by the CIHR Canada Research Chair in Psychosocial Epidemiology.
References
- 1.Hyder AA, Wunderlich CA, Puvanachandra P, et al. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation. 2007;22:341–53. [PubMed] [Google Scholar]
- 2.Zhao YD, Wang W. Neurosurgical trauma in People's Republic of China. World J Surg. 2001;25:1202–4. doi: 10.1007/s00268-001-0082-8. [DOI] [PubMed] [Google Scholar]
- 3.MacMillan HL, MacMillan AB, Offord DR, et al. Aboriginal health. CMAJ. 1996;155:1569–78. [PMC free article] [PubMed] [Google Scholar]
- 4.Greenwood ML, de Leeuw SN. Social determinants of health and the future well-being of Aboriginal children in Canada. Paediatr Child Health. 2012;17:381–4. [PMC free article] [PubMed] [Google Scholar]
- 5.Ottawa: Canadian Institute for Health Information. Improving the health of Canadians 2004. 2004. [accessed 2015 May 16]. Available https://secure.cihi.ca/estore/productSeries.htm?pc=PCC180.
- 6.Karmali S, Laupland K, Harrop AR, et al. Epidemiology of severe trauma among status Aboriginal Canadians: a population-based study. CMAJ. 2005;172:1007–11. doi: 10.1503/cmaj.1040432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rutland-Brown W, Wallace LJ, Faul M, et al. Traumatic brain injury hospitalizations among American Indians/Alaska Natives. J Head Trauma Rehabil. 2005;20:205–14. doi: 10.1097/00001199-200505000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Blackmer J, Marshall SC. A comparison of traumatic brain injury in the Saskatchewan native North American and non-native North American populations. Brain Inj. 1999;13:627–35. doi: 10.1080/026990599121359. [DOI] [PubMed] [Google Scholar]
- 9.Langlois JA, Kegler SR, Butler JA, et al. Traumatic brain injury-related hospital discharges. Results from a 14-state surveillance system, 1997. MMWR Surveill Summ. 2003;52:1–20. [PubMed] [Google Scholar]
- 10.Coronado VG, Xu L, Basavaraju SV, et al. Surveillance for traumatic brain injury-related deaths - United States, 1997-2007. MMWR Surveill Summ. 2011;60:1–32. [PubMed] [Google Scholar]
- 11.Desapriya E, Han G, Jivani K, et al. Vancouver: BC Injury Research and Prevention Unit. Motor vehicle crashes and occupant restraint use among Aboriginal populations in BC. 2008. [accessed 2015 May 14]. Available data.injuryresearch.bc.ca/admin/DocUpload/3_20090612_121856Aboriginal%20Restraint%20Use%20Report_Apr.22%20Edi%20a.pdf.
- 12.Desapriya E, Fujiwara T, Verma P, et al. Comparison of on-reserve road versus off-reserve road motor vehicle crashes in Saskatchewan, Canada: a case control study. Asia Pac J Public Health. 2011;23:1005–20. doi: 10.1177/1010539510361787. [DOI] [PubMed] [Google Scholar]
- 13.Feigin VL, Theadom A, Barker-Collo S, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 2013;12:53–64. doi: 10.1016/S1474-4422(12)70262-4. [DOI] [PubMed] [Google Scholar]
- 14.Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil. 2005;20:229–38. doi: 10.1097/00001199-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Auer AM, Andersson R. Canadian Aboriginal communities: a framework for injury surveillance. Health Promot Int. 2001;16:169–77. doi: 10.1093/heapro/16.2.169. [DOI] [PubMed] [Google Scholar]
- 16.Gagné M, Robitaille Y, Légaré G, et al. Québec: Institut national de santé publique du Québec. Évolution des hospitalisations attribuables aux traumatismes craniocérébraux d'origine non intentionnelle au Québec. 2012. [accessed 2015 May 13]. Available www.inspq.qc.ca/pdf/publications/1473_EvolHospitaAttribuTCCNonIntentQc.pdf.
- 17.Google My Maps. [accessed 2016 Jan. 14]. Available https://www.google.ca/maps/d/
- 18.Nemaska (QC): Grand Council of the Crees. The James Bay and northern Quebec agreement (JBNQA). 1975. [accessed 2015 May 12]. Available www.gcc.ca/pdf/LEG000000006.pdf.
- 19.Quebec: Régie de l'assurance maladie du Québec. The Régie. 2014. [accessed 2016 Jan. 12]. Available www.ramq.gouv.qc.ca/en/regie/Pages/mission.aspx.
- 20.Monfared AA, Lelorier J. Accuracy and validity of using medical claims data to identify episodes of hospitalizations in patients with COPD. Pharmacoepidemiol Drug Saf. 2006;15:19–29. doi: 10.1002/pds.1131. [DOI] [PubMed] [Google Scholar]
- 21.Lareau-Trudel E, Fortin E, Gauthier M, et al. Epidemiological surveillance of amyotrophic lateral sclerosis in Saguenay region. Can J Neurol Sci. 2013;40:705–9. doi: 10.1017/s0317167100014955. [DOI] [PubMed] [Google Scholar]
- 22.St Germaine-Smith C, Metcalfe A, Pringsheim T, et al. Recommendation for optimal ICD codes to study neurologic conditions: a systematic Review. Neurology. 2012;79:1049–55. doi: 10.1212/WNL.0b013e3182684707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thornhill S, Teasdale GM, Murray GD, et al. Disability in young people and adults after head injury: prospective cohort study. BMJ. 2000;320:1631–5. doi: 10.1136/bmj.320.7250.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 25.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 26.Québec: Institut de la statistique du Québec. Population et structure par âge et sexe. 2015. [accessed 2015 May 13]. Available www.stat.gouv.qc.ca/statistiques/population-demographie/structure/index.html.
- 27.Québec: Santé et Services sociaux. Projections et estimations de la population par territoire sociosanitaire. 2015. [accessed 2015 May 23]. Available www.informa.msss.gouv.qc.ca/Listes.aspx?Name=y9M4IcKgjFYapz02jKwkUg==&Key=hhKpcdsNkJS+eg2gWNwm7A==&OrderByClause=8jnVPckjxX8dPG+Ajs/DlA==&idDimension=PGShVhdHJuA=
- 28.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 29.Baraldi AN, Enders CK. An introduction to modern missing data analyses. J Sch Psychol. 2010;48:5–37. doi: 10.1016/j.jsp.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 30.Orientations ministérielles pour le traumatisme craniocérébral léger. Québec: Santé et Services sociaux. 2005. [accessed 2016 Jan. 4]. Available www.repar.veille.qc.ca/info-tcc/IMG/pdf/orientations_traumatisme.pdf.
- 31.Ottawa: Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, Social Sciences and Humanities Research Council of Canada. Tri-council policy statement: ethical conduct for research involving humans. 2010. [accessed 2015 June 2]. Available www.pre.ethics.gc.ca/pdf/eng/tcps2/TCPS_2_FINAL_Web.pdf.
- 32.Roozenbeek B, Maas AIR, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9:231–6. doi: 10.1038/nrneurol.2013.22. [DOI] [PubMed] [Google Scholar]
- 33.Maas AI, Harrison-Felix CL, Menon D, et al. Standardizing data collection in traumatic brain injury. J Neurotrauma. 2011;28:177–87. doi: 10.1089/neu.2010.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Koskinen S, Alaranta H. Traumatic brain injury in Finland 1991-2005: a nationwide register of hospitalized and fatal TBI. Brain Inj. 2008;22:205–14. doi: 10.1080/02699050801938975. [DOI] [PubMed] [Google Scholar]
- 35.Shivaji T, Lee A, Dougall N, et al. The epidemiology of hospital treated traumatic brain injury in Scotland. BMC Neurol. 2014;14:2. doi: 10.1186/1471-2377-14-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colantonio A, Croxford R, Farooq S, et al. Trends in hospitalization associated with traumatic brain injury in a publicly insured population, 1992-2002. J Trauma. 2009;66:179–83. doi: 10.1097/TA.0b013e3181715d66. [DOI] [PubMed] [Google Scholar]
- 37.Gabella B, Hoffman RE, Marine WW, et al. Urban and rural traumatic brain injuries in Colorado. Ann Epidemiol. 1997;7:207–12. doi: 10.1016/s1047-2797(96)00150-0. [DOI] [PubMed] [Google Scholar]
- 38.Laflamme L, Burrows S, Hasselberg M. Geneva: World Health Organization. Socioeconomic differences in injury risks. A review of findings and a discussion of potential countermeasures. 2009. [accessed 2015 Apr. 14]. Available www.euro.who.int/en/health-topics/disease-prevention/violence-and-injuries/publications/pre-2009/socioeconomic-differences-in-injury-risks.-a-review-of-findings-and-a-discussion-of-potential-countermeasures.
- 39.Bowman SM, Aitken ME, Helmkamp JC, et al. Impact of helmets on injuries to riders of all-terrain vehicles. Inj Prev. 2009;15:3–7. doi: 10.1136/ip.2008.019372. [DOI] [PubMed] [Google Scholar]
- 40.Thompson DC, Rivara F, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev. 2000:CD001855. doi: 10.1002/14651858.CD001855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thurman DJ, Alverson C, Dunn KA, et al. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14:602–15. doi: 10.1097/00001199-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Rimel RW, Giordani B, Barth JT, et al. Disability caused by minor head injury. Neurosurgery. 1981;9:221–8. [PubMed] [Google Scholar]
- 43.Winqvist S, Luukinen H, Jokelainen J, et al. Recurrent traumatic brain injury is predicted by the index injury occurring under the influence of alcohol. Brain Inj. 2008;22:780–5. doi: 10.1080/02699050802339397. [DOI] [PubMed] [Google Scholar]
- 44.Cope DN. The effectiveness of traumatic brain injury rehabilitation: a review. Brain Inj. 1995;9:649–70. doi: 10.3109/02699059509008224. [DOI] [PubMed] [Google Scholar]
- 45.Carroll LJ, Cassidy JD, Holm L, et al. Methodological issues and research recommendations for mild traumatic brain injury: the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;(Suppl):113–25. doi: 10.1080/16501960410023877. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.