Abstract
Some patients with gastroesophageal reflux disease experience persistent reflux symptoms despite proton pump inhibitor therapy. These symptoms reduce their health-related quality of life. Our aims were to evaluate the relationship between proton pump inhibitor efficacy and health-related quality of life and to evaluate predictive factors affecting treatment response in Japanese patients. Using the gastroesophageal reflux disease questionnaire, 145 gastroesophageal reflux disease patients undergoing proton pump inhibitor therapy were evaluated and classified as responders or partial-responders. Their health-related quality of life was then evaluated using the 8-item Short Form Health Survey, the Pittsburgh Sleep Quality Index, and the Hospital Anxiety and Depression Scale questionnaires. Sixty-nine patients (47.6%) were partial responders. These patients had significantly lower scores than responders in 5/8 subscales and in the mental health component summary of the 8-item Short Form Health Survey. Partial responders had significantly higher Pittsburgh Sleep Quality Index and Hospital Anxiety and Depression Scale scores, including anxiety and depression scores, than those of responders. Non-erosive reflux disease and double proton pump inhibitor doses were predictive factors of partial responders. Persistent reflux symptoms, despite proton pump inhibitor therapy, caused mental health disorders, sleep disorders, and psychological distress in Japanese gastroesophageal reflux disease patients.
Keywords: gastroesophageal reflux disease, health-related quality of life, 8-item Short Form Health Survey, Pittsburgh Sleep Quality Index, Hospital Anxiety and Depression Scale
Introduction
Gastroesophageal reflux disease (GERD) is defined as “a condition that develops when the reflux of stomach contents causes troublesome symptoms and/or complications”.(1) GERD is categorized into erosive reflux disease (ERD), defined as the presence of esophageal mucosal breaks, and non-erosive reflux disease (NERD), defined as the presence of GERD symptoms without esophageal mucosal breaks. In East Asian countries, more than half of GERD patients have a mild form of ERD or NERD, as identified by endoscopic examination, unlike Western countries.(2,3) Recently the number of GERD patients in Japan has increased and the prevalence of GERD in Japan is now almost the same as that in Western countries. This increase is due to an increase in gastric acid secretion and a decrease in the Helicobacter pylori (H. pylori) infection rate, as well as to the increased attention that GERD has gained, and advances in the concept of GERD itself.(2,4) In studies in Western countries, the severity and frequency of GERD symptoms has been shown to increase physical and mental health disorders, and night-time symptoms have been reported to cause sleep disturbances in more than half of GERD patients.(5,6) Proton pump inhibitors (PPIs) strongly inhibit gastric acid secretion, and are generally the first choice of treatment for GERD.(1) Many studies have reported that PPI therapy improved physical health, mental health, and sleep disorders in GERD patients.(7–10) However, it has also been reported that some GERD patients experience persistent and troublesome symptoms despite PPI therapy and their health-related quality of life (HRQOL) and sleep are often badly affected.(11,12) Physical and mental health levels, sleep disorders, and anxiety and depression levels are often evaluated by the 8-item Short Form Health Survey (SF-8), the Pittsburgh Sleep Quality Index (PSQI), and the Hospital Anxiety and Depression Scale (HADS), respectively. There have been few studies that have used all 3 questionnaires. Moreover, response rates to PPI therapy or causative factors affecting HRQOL in GERD patients receiving PPI therapy differ by country. The aims of this observation study were to evaluate the relationship between the efficacy of PPI and HRQOL in Japanese GERD patients receiving PPI therapy, using the SF-8, PSQI, and HADS questionnaires, and to examine predictive factors affecting response to PPI therapy.
Materials and Methods
Patients
This study was performed as an observational study to assess the association between symptomatic response to PPI therapy and HRQOL in Japanese GERD patients receiving PPI therapy at Nagoya City West Medical Center and Nagoya City University between October 2012 and February 2013. During this study period, we enrolled 145 consecutive GERD outpatients at Nagoya City West Medical Center and Nagoya City University Hospital. The subjects of this study were GERD patients, older than 20 years of age, who were undergoing continuous PPI therapy and had been receiving treatment for over 2 months. GERD had been diagnosed based on the presence of the typical reflux symptoms of heartburn and/or acid regurgitation; these symptoms occurred more than twice a week prior to PPI therapy. PPI therapy consisted of 10 or 20 mg omeprazole, 15 or 30 mg lansoprazole, or 10 or 20 mg rabeprazole once a day. Prior to PPI therapy initiation, an endoscopic examination was performed in all patients to evaluate mucosal breaks according to the Los Angeles (LA) classification system, with NERD described as LA grade 0 and ERD described as LA grades A–D. For patients with more than 1 endoscopic examination, the worst severity was recorded.
Study design
In this study, all patients were asked to evaluate their HRQOL and PPI therapy response by filling out a gastroesophageal reflux disease questionnaire (GerdQ), SF-8, PSQI, and HADS questionnaires, and 1 further questionnaire consisting of 4 original questions related to life-style factors [alcohol, smoking, non-steroidal anti-inflammatory drugs (NSAID) intake, and PPI daily dosage]. All aspects of this study were approved by the Ethical Committees of both the Nagoya City West Medical Center and the Nagoya City University Graduate School of Medical Sciences. All patients agreed to take part in the study and answered all questions in each of the questionnaires.
Evaluation of the response to PPI therapy using the GerdQ questionnaire
The GerdQ is a 6-item questionnaire that has been recently developed to help identify patients with GERD. Using the results of this questionnaire, we classified 145 patients as either those in whom GERD was well-controlled with PPI therapy (responders) or those in whom it was not well-controlled with PPI therapy (partial responders). Responders were defined as patients who reported 0–1 days of persistent reflux symptoms in any of the 4 questions concerning heartburn, regurgitation, sleep disturbances, and additional medications in the GerdQ. On the other hand, partial responders were defined as patients that reported 2–3 days of persistent reflux symptoms in at least 1 of the 4 questions concerning heartburn, regurgitation, sleep disturbances, and additional medications in the GerdQ.(13)
Evaluation of physical and mental health using the SF-8 questionnaire
The SF-8 is an 8-item, self-rating, questionnaire which assesses HRQOL. The scores for the 8 domains [general health (GH), physical functioning (PH), role-physical (RP), bodily pain (BP), vitality (VT), social functioning (SF), mental health (MH), and role-emotional (RE)] and 2 summaries [physical component summary (PCS) and mental component summary, (MCS)] were derived from this questionnaire.(14) The “Manual of the SF-8 Japanese Version” was used in this study. The mean score for the Japanese general population is 50 points for each domain and summary. A score of <50 was considered to indicate impaired HRQOL, and higher scores indicated a good level of functioning and well-being in comparison with the Japanese general population.(15) We evaluated the SF-8 scores between responders and partial responders.
Evaluation of sleep disorders using the PSQI questionnaire
The PSQI is a 19-item, self-rating, questionnaire which assesses sleep quality and disturbances over a 1-month time interval. Nineteen individual items generate 7 “component” scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication, and daytime function. The subscales yield a score from 0 to 3 and are summed to yield a total score ranging from 0 to 21. The more sleep disturbances suffered by a patient, the higher the PSQI score. The validated Japanese version was used in this study and a PSQI score of >5.5 was considered to indicate impaired sleep.(16,17) We evaluated the PSQI scores between responders and partial responders.
Evaluation of anxiety disorders and depression using the HADS questionnaire
The HADS is a 14-item, self-rating, questionnaire which assesses psychological distress. It is designed to measure anxiety and depression, and its 2 subscales contain 7 items each. Respondents indicate the frequency of any symptom on a 4-point Likert-type scale. The anxiety subscale (HADS-A) and depression subscale (HADS-D) scores were calculated as the sum of their respective 7-item scores (ranging from 0 to 21) and the total score was the sum of the 14 items (ranging from 0 to 42). When a patient suffered more serious anxiety or depressive symptoms, the HADS-A or HADS-D scores reached 7 or higher.(18) Moreover, we classified the total HADS scores as follows: <7 points, “mild”; 7–11 points, “moderate”; >11 points, “severe”. We evaluated the HADS scores between responders and partial responders.
Evaluation of background factors in responders and partial responders
Age, gender, body mass index (BMI), alcohol intake, smoking, H. pylori infection, NSAID intake, concomitant gastrointestinal medication other than PPI, esophagitis grade by LA classification, and PPI daily dose were evaluated in responders and partial responders by univariate analysis as background factors associated with the response to PPI therapy. Moreover, we performed a multivariate analysis to predict partial response to PPI therapy using the factors that had a p value <0.2 in univariate analysis.
Statistical analysis
Statistical analysis was performed using the Ekuseru-Toukei 2015 platform (Social Survey Research Information Co., Ltd., Tokyo, Japan). Values are expressed as mean ± SD or frequency (%). Student’s t test was used to compare individual SF-8 component scores, PSQI scores, HADS component scores, and background factors in PPI responders and partial responders. The Fisher’s exact test was used for the analysis of HADS Anxiety and Depressive state, LA classification, and PPI daily dose. A logistic regression analysis was used to determine predictive factors for partial response to PPI in GERD patients, which were expressed as an odds ratio (OR) and 95% confidence interval (CI). A 2-sided p value of less than 0.05 was considered statistically significant.
Results
Patient clinical characteristics
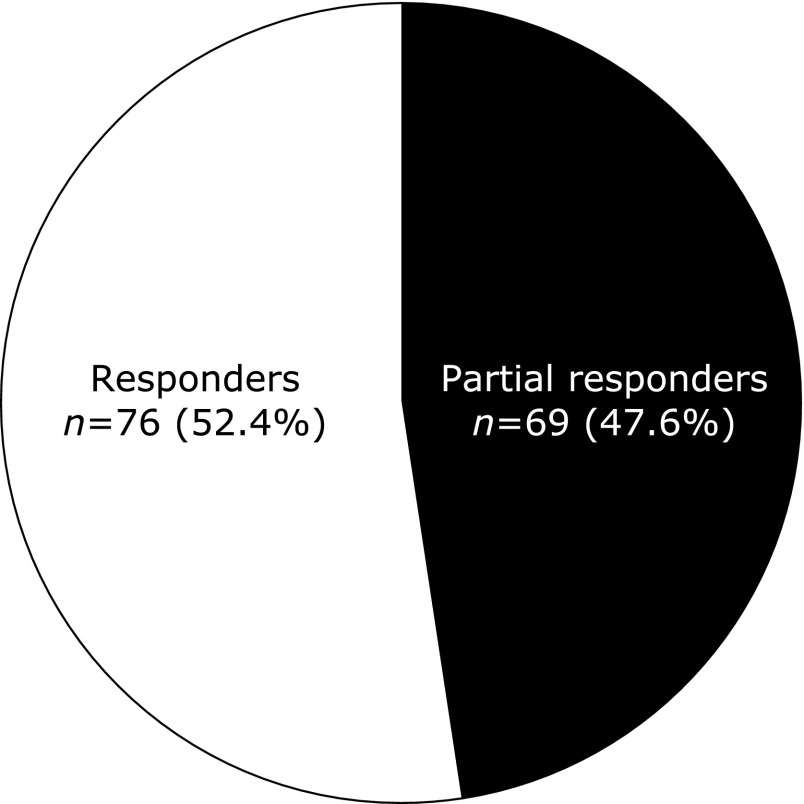
The study population consisted of 145 GERD patients (mean age, 65.3 years; female, 49.0%; median GERD disease duration, 18 months; mean BMI, 22.9). A summary of the patient characteristics is shown in Table 1. PPI therapy response rate as determined by the GerdQ questionnaire. Seventy-six (52.4%) and 69 (47.6%) patients were identified as responders and partial responders to PPI therapy, respectively (Fig. 1).
Table 1.
A summary of patient characteristics
| Charasteristics | Value |
|---|---|
| Age (years; n = 145) | 65.3 ± 13.7 |
| Duration of GERD (months; n = 145) | 18 (6, 37) |
| Gender (n = 145) | |
| Male | 74 (51) |
| Female | 71 (49) |
| BMI (n = 145) | 22.9 ± 3.2 |
| Alcohol intake (n = 145) | 49 (34) |
| Smoking (n = 145) | 14 (10) |
| NSAID intake (n = 145) | 24 (17) |
| Los Angeles classification (n = 145) | |
| NERD | 63 (43) |
| Grade 0 | 63 |
| ERD | 82 (57) |
| Grade A | 37 |
| Grade B | 28 |
| Grade C | 12 |
| Grade D | 5 |
| PPI daily dose (n = 145) | |
| Half dose | 26 (18) |
| Regular dose | 107 (74) |
| Double dose | 12 (8) |
Values are presented as the mean ± standard deviation or frequency (%); Duration of GERD is presented in order of the median, lower quartile, and upper quartile; GERD, gastroesophageal reflux disease; BMI, body mass index; NSAID, non-steroidal anti-inflammatory drugs; NERD, non-erosive reflux disease; ERD, erosive reflux disease; PPI, proton pump inhibitor.
Fig. 1.
Response rate to proton pump inhibitors (PPIs). Seventy-six patients (52.4%) were identified as responders and 69 patients (47.6%) were identified as partial responders to PPI therapy.
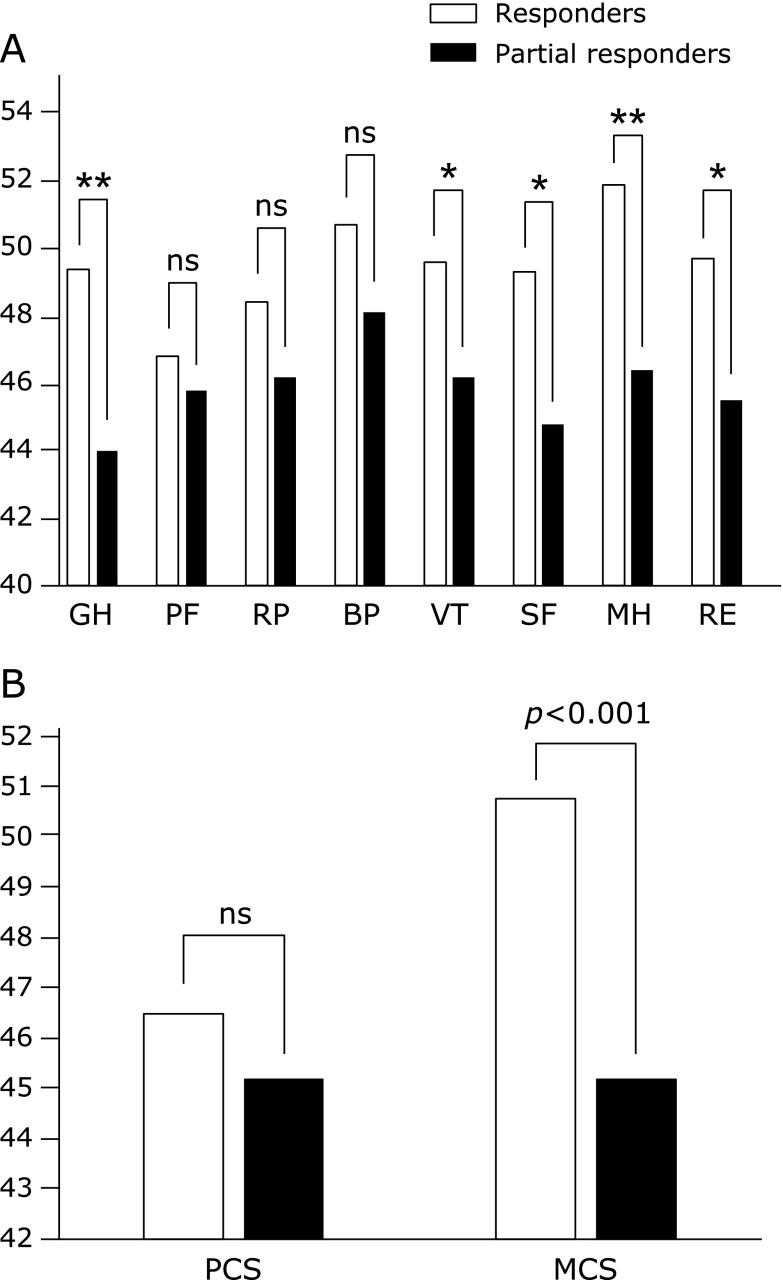
Comparison of the SF-8 score between responders and partial responders
The mean scores for the 8 domains of the SF-8 are shown in Fig. 2A. The mean scores for the GH, PF, RP, BP, VT, SF, MH, and RE domains in responders were 49.437, 46.842, 48.373, 50.749, 49.637, 49.257, 51.897, and 49.723, respectively. The mean scores for the GH, PH, RP, BP, VT, SF, MH, and RE domains in partial responders were 43.961, 45.822, 46.191, 48.090, 46.225, 44.806, 46.415, and 45.480, respectively. The GH, VT, SF, MH, and RE scores were significantly lower in partial responders than in responders (p<0.001, p<0.01, p<0.01, p<0.001, and p<0.01, respectively). The mean PCS and MCS scores are shown in Fig. 2B. In responders, the mean PCS and MCS scores were 46.480 and 50.824, respectively. In partial responders, the mean PCS and MCS scores were 45.181 and 45.162, respectively. The MCS score in partial responders was significantly lower than that in responders (p<0.001). There was no significant difference in PCS score between responders and partial responders.
Fig. 2.
(A) 8-item Short Form Health Survey (SF-8) subscale score. GH, general health; PF, physical function; RP, role-physical; BP, bodily pain; VT, vitality; SF, social function; MH, mental health; RE, role-emotional. The GH, VT, SF, MH, and RE scores of the partial responders were significantly lower than those of the responders. *p<0.01, **p<0.001. (B) SF-8 summary score. The mental component summary (MCS) score in partial responders was significantly lower than that in responders. There was no significant difference in physical component summary (PCS) score between responders and partial responders.
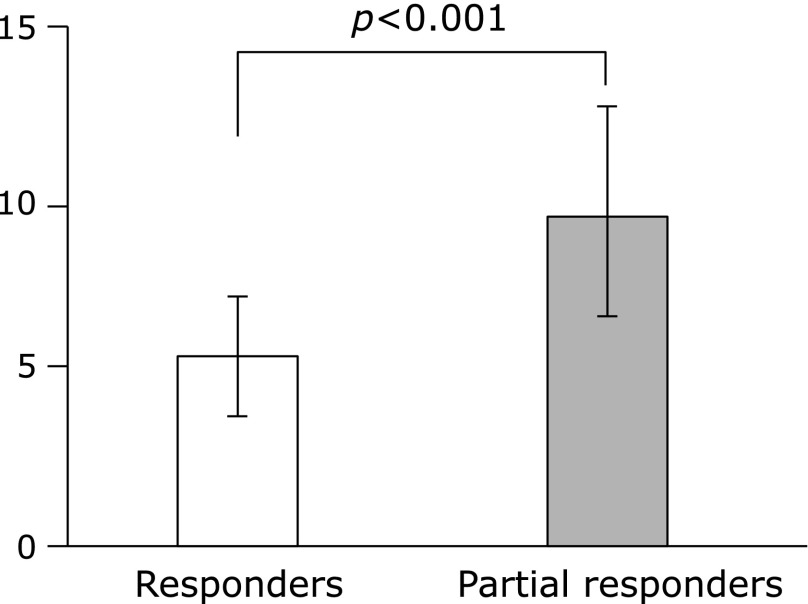
Comparison of the PSQI scores between responders and partial responders
The mean PSQI scores are shown in Fig. 3. In responders and partial responders, the mean PSQI score was 5.1 and 9.4, respectively. The PSQI score in partial responders was significantly higher than that in responders (p<0.001).
Fig. 3.
Comparison of the Pittsburgh Sleep Quality Index (PSQI) scores. The PSQI score was significantly higher in partial responders than in responders.
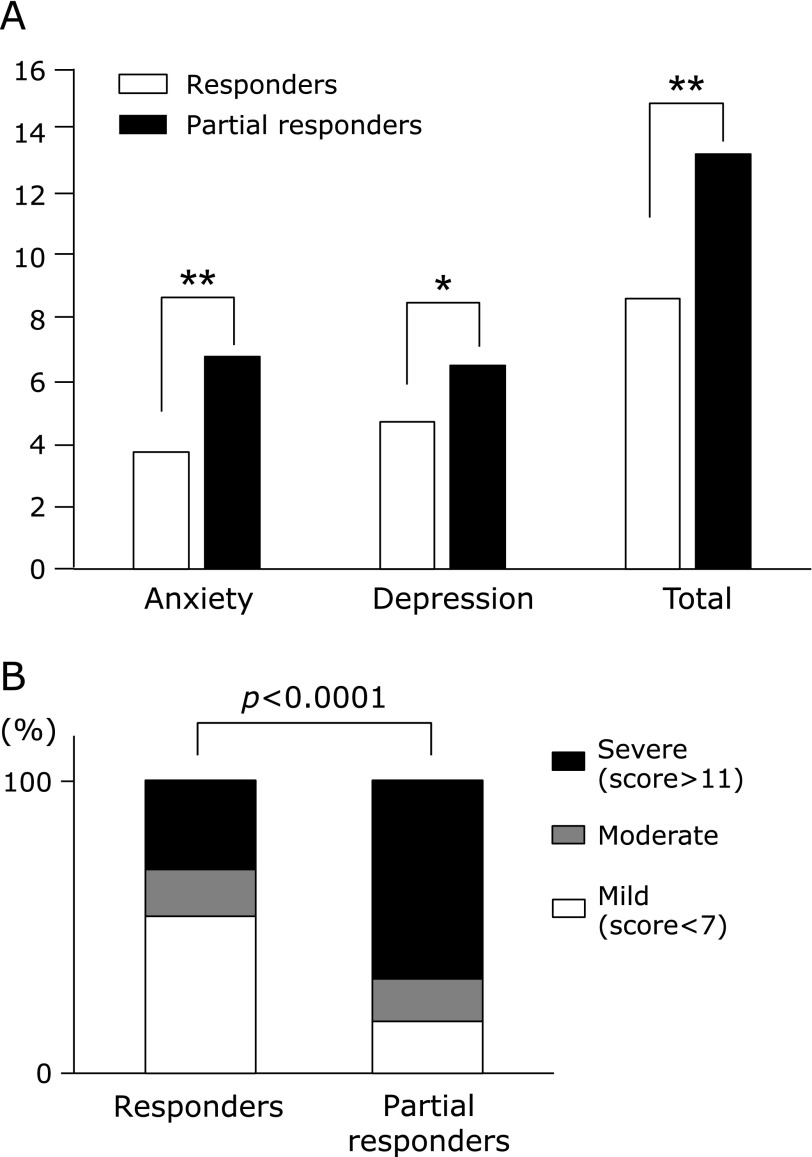
Comparison of the HADS scores between responders and partial responders
The mean HADS-A and HADS-D scores, and the total HADS score are shown in Fig. 4A. In responders, the mean HADS-A, mean HADS-D, and total HADS scores were 3.826, 4.826, and 8.776 respectively. In partial responders, those scores were 6.857, 6.663, and 13.468, respectively. The HADS-A, HADS-D, and total HADS scores of the partial responders were significantly higher than those of the responders (p<0.001, p<0.01, and p<0.001, respectively). The ratios of “severe”, “moderate”, and “mild” were 31.3, 13.4, and 55.2%, respectively, in responders, and 69.4, 12.9, and 17.7%, respectively, in partial responders (Fig. 4B). There was significant difference in the anxiety or depression level ratio between responders and partial responders (p<0.0001). The “severe” and “mild” ratios in partial responders were significantly higher and lower, respectively, than those in responders (p<0.0001 for both).
Fig. 4.
(A) Comparison of Hospital Anxiety and Depression Scale (HADS) scores. The mean HADS-A, HADS-D, and total HADS scores in partial responders were significantly higher than those in responders. *p<0.01, **p<0.001. (B) Comparison of HADS-A and HADS-D states. There was a significant difference in the ratio of anxiety or depression levels between responders and partial responders. The “severe” ratio of partial responders was significantly higher than that of responders and the “mild” ratio of partial responders were significantly lower than that of responders.
Comparison of the background factors between responders and partial responders
The background factor results for responders and partial responders are shown in Table 2. LA classification and PPI daily dose were significant factors associated with PPI response (p<0.01, p<0.01, respectively). Age, gender, GERD disease duration, BMI, alcohol intake, smoking, and NSAID intake were not significantly associated with PPI response. Sixty-three patients (43.4%) were classified as having NERD. The proportion of partial responders with NERD was significantly higher than the proportion of responders (p<0.01). The proportion of responders classified as LA-C was significantly higher than the proportion of partial responders (p<0.05). Moreover, the proportion of responders receiving the regular PPI dose was significantly higher than that of partial responders (p<0.01), whereas the proportion of partial responders receiving the double PPI dose was significantly higher than that of responders (p<0.05). A multivariate analysis demonstrated that NERD (OR, 3.30; 95% CI, 1.61–6.74; p<0.01) and the double PPI daily dose (OR, 7.29; 95% CI, 1.46–36.46; p<0.05) were significantly associated with partial response to PPI therapy (Table 3).
Table 2.
The background factor results for responders and partial responders
| Factors | Responders (n = 76) | Partial responders (n = 69) | p value |
|---|---|---|---|
| Age (years) | 67.1 ± 13.1 | 63.4 ± 13.1 | 0.099 |
| Duration of GERD (months) | 21 (8, 36) | 14 (6, 44) | 0.941 |
| Gender | 0.504 | ||
| Male (n = 74) | 40 (53) | 34 (49) | |
| Female (n = 71) | 36 (47) | 35 (51) | |
| BMI | 22.9 ± 3.2 | 23.0 ± 3.2 | 0.78 |
| Alcohol intake | 25 (33) | 24 (35) | 0.728 |
| Smoking | 8 (11) | 6 (9) | 0.783 |
| NSAID intake | 16 (21) | 8 (12) | 0.179 |
| Los Angeles classification | 0.007** | ||
| NERD (n = 63) | |||
| Grade 0 | 23 (30) | 40 (58) | 0.001** |
| ERD (n = 82) | |||
| Grade A | 24 (32) | 13 (19) | 0.089 |
| Grade B | 16 (21) | 12 (17) | 0.675 |
| Grade C | 10 (13) | 2 (3) | 0.033* |
| Grade D | 3 (4) | 2 (3) | 0.999 |
| PPI daily dose | 0.006** | ||
| Half dose | 10 (13) | 16 (23) | 0.133 |
| Regular dose | 64 (84) | 43 (62) | 0.007** |
| Double dose | 2 (3) | 10 (15) | 0.014* |
Values are presented as either the mean ± standard deviation or frequency (%); Duration of GERD (months; n = 145) is presented in order of the median, lower quartile, and upper quartile; GERD, gastroesophageal reflux disease; BMI, body mass index; NSAID, non-steroidal anti-inflammatory drugs; NERD, non-erosive reflux disease; ERD, erosive reflux disease; PPI, proton pump inhibitor. *p<0.05, **p<0.01.
Table 3.
Factors predicting partial response to proton pump inhibitor therapy in patients of gastroesophageal reflux disease
| Factors | Partial response to PPI | p value | |
|---|---|---|---|
| OR | 95% CI | ||
| Age (per 1 year) | 0.98 | 0.95–1.00 | 0.062 |
| NSAID intake | 0.61 | 0.098–3.76 | 0.593 |
| Los Angeles classification | |||
| NERD | 3.3 | 1.61–6.74 | 0.001** |
| PPI daily dose | |||
| Double dose | 7.29 | 1.46–36.46 | 0.016* |
PPI, proton pump inhibitor; OR, odds ratio; CI, confidence interval; NSAID, non-steroidal anti-inflammatory drugs; NERD, non-erosive reflux disease. *p<0.05, **p<0.01.
Discussion
This study evaluated the relationship between the efficacy of PPI therapy and HRQOL (physical health, mental health, sleep levels, anxiety levels, and depression levels) in Japanese GERD patients receiving PPI therapy and examined predictive factors affecting the response to PPI therapy. We found that approximately 47% of GERD patients receiving PPI therapy were partial responders and that these patients had significantly more mental health, sleep, anxiety, and depression disorders in comparison to responders. Moreover, responders did not display any mental health disorders and GERD patients generally suffer from some physical disorder, regardless of the response to PPI therapy. Furthermore, the grade of the endoscopic findings and the PPI daily dose were significant factors that affected the response to PPI therapy, and NERD and the double PPI daily dose were predictive factors of partial response to PPI therapy.
According to Jones et al.,(13) a GERD patient receiving PPI therapy is defined as a partial responder when 2–3 days of persistent reflux symptoms are reported in at least 1 of 4 questions concerning heartburn, regurgitation, sleep disturbance, and additional medication in the GerdQ. In our study of GERD patients receiving PPI therapy for more than 8 weeks, the proportion of partial responders, identified using the GerdQ, was approximately 47%. In a systematic review, El-Serag et al.(19) reported that persistent and troublesome GERD symptoms remained in 17–32% of primary care patients receiving PPI therapy and 45% (30–60%) of participants reported persistent GERD symptoms in observational primary care and community-based studies. In our study of Japanese GERD patients, the proportion of partial responders was slightly higher than that of these previous studies. One of the reasons for the high proportion of partial responders in our study could be due to the fact that our patients were enrolled at a core hospital and a university hospital, in which refractory GERD patients are often introduced secondarily from primary clinics. In these patients, the effect of PPI therapy may have decreased over time, as they would have often contracted GERD, the median duration of which was 18 months, and often been treated with PPI.
Our SF-8 data showed that partial responders had scores of <49 points for all SF-8 domains, PCS, and MSC, whereas responders had scores of <49 points for only 1 SF-8 domain and PCS. These results indicated that partial responders had significantly more mental health disorders than responders. A systematic review reported that the physical health and mental health scores of non-responders to PPI therapy were, on average, 8–16% and 2–12% lower, respectively, than those of responders.(11) Contrary to these previous reports, there was no significant difference in physical health disorders between responders and partial responders in our study. However, the PCS scores of the responders and partial responders were both <47 points, which showed that GERD patients suffer from some type of physical disorder regardless of response to PPI therapy, compared with the general Japanese population. Hongo et al.(9) reported that, 8 weeks after the initiation of rabepurazole treatment, SF-8 scores had improved in their study. However, our study revealed that nearly half of GERD patients are still partial responders in spite of PPI therapy, and persistent reflux symptoms are strongly associated with a mental health disorder.
We demonstrated that the mean PSQI score of 9.4 in partial responders indicated a serious degree of sleep disorders; this score was significantly greater than that in responders. On the other hand, the mean PSQI score in responders was <5.5, which indicated that responders did not suffer from more sleep disorders than the general Japanese population. This result revealed that persistent reflux symptoms are also strongly associated with sleep disorders. Fujiwara et al.(12) reported the occurrence of sleep disorders in 52.2% of Japanese GERD patients before PPI treatment. This study also reported that daily treatment with rabeprazole for 8 weeks decreased sleep disorders. However, Hiramoto et al.(20) reported that once-daily treatment with esomeprazole for 2 weeks decreased GERD symptoms, but did not decrease sleep disorders. Whether the sleep disorders of partial responders can be improved by PPI therapy alone is a subject for future analysis.
Our data showed that the HADS-A and HADS-D scores of responders and partial responders were both <7, which indicated that they did not suffer from serious symptoms of anxiety or depression. However, the total HADS score of partial responders was >11, which indicated that they displayed severe psychiatric symptoms. In addition, partial responders suffered from a significantly greater degree of anxiety and depression disorders than responders. Moreover, the proportion of partial responders with severe psychiatric symptoms was significantly higher than that of responders, while the proportion of responders with mild psychiatric symptoms was significantly lower than that of responders. Consistent with our results, a population-based study in Norwegian GERD patients reported that anxiety and depression were strongly associated with reflux symptoms.(21) However, contrary to our results, a study by Boltin et al.(22) observed that failure to respond to PPI therapy was not associated with anxiety or depression. In addition, a study in Korean patients observed that response to PPI therapy was not associated with anxiety or depression.(23) These conflicting results may be due to differences in the method used to measure response to PPI therapy. Our study revealed that persistent reflux is also strongly associated with anxiety and depression levels.
In our study, the background variables affecting the response to PPI therapy were LA classification and PPI daily dose, but not gender, BMI, alcohol intake, smoking, or NSAID intake, as determined by univariate analysis. The proportion of partial responders receiving a double PPI daily dose was significantly higher than that of responders. On the other hand, the proportion of responders with LA grade C classification or receiving a regular PPI daily dose was significantly higher than that of the partial responders. Moreover, we revealed, by multivariate analysis, that NERD and a double PPI daily dose were significant factors predicting partial response to PPI therapy. We believe that partial responders took higher doses of PPI in an effort to improve persistent and troublesome reflux symptoms, whereas responders were satisfied with the decrease in GERD symptoms they achieved with the regular daily dose of PPI. In other words, it is very difficult to improve GERD symptoms completely with only PPI therapy. Several recent studies have suggested that female sex, lower BMI, NERD, esophageal hypersensitivity, non-acid reflux, and psychological factors were associated with poor response to PPI treatment in GERD patients.(23–26) In East Asian countries, NERD was identified as a risk factor for sleep disorders, and the daily activity of NERD patients was affected more than that of ERD patients, consistent with our results.(3,4,12,25)
The present study has some limitations. First, the number of study subjects was small, and we did not include healthy controls. Moreover, 3 different kinds of PPI treatment were used. At present, we are accumulating data on GERD patients with persistent symptoms to further explore factors affecting HRQOL. We want to examine whether the control of persistent reflux symptoms using other treatments can improve mental health, sleep, anxiety, and depression disorders.(27–29)
In conclusion, nearly half of Japanese GERD patients receiving PPI therapy were partial responders, and their persistent and troublesome reflux symptoms caused mental health and sleep disorders, and psychological distress despite PPI therapy. In addition, responders did not suffer from mental health disorders, and all GERD patients had some form of physical disorder regardless of response to PPI therapy. Moreover, LA classification and PPI daily dose were identified as significant factors affecting the response to PPI, and NERD and the double PPI daily dose were predictive factors of partial response to PPI therapy.
Abbreviations
- BMI
body mass index
- BP
bodily pain
- ERD
erosive reflux disease
- GERD
gastroesophageal reflux disease
- GerdQ
gastroesophageal reflux disease questionnaire
- GH
general health
- HADS
Hospital Anxiety and Depression Scale
- HADS-A
Hospital Anxiety and Depression Scale-anxiety
- HADS-D
Hospital Anxiety and Depression Scale-depression
- HRQOL
health-related quality of life
- LA
Los Angeles
- MCS
mental component summary
- MH
mental health
- NERD
non-erosive reflux disease
- NSAID
non-steroidal anti-inflammatory drugs
- PCS
physical component summary
- PH
physical functioning
- PPI
proton pump inhibitor
- PSQI
Pittsburgh Sleep Quality Index
- RE
role-emotional
- RP
role-physical
- SF
social functioning
- SF-8
8-item Short Form Health Survey
- VT
vitality
Conflict of Interest
No potential conflicts of interest were disclosed.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 2.Hongo M, Shoji T. Epidemiology of reflux disease and CLE in East Asia. J Gastroenterol. 2003;38:25–30. [PubMed] [Google Scholar]
- 3.Kim JY, Kim N, Seo PJ, et al. Association of sleep dysfunction and emotional status with gastroesophageal reflux disease in Korea. J Neurogastroenterol Motil. 2013;19:344–354. doi: 10.5056/jnm.2013.19.3.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujiwara Y, Arakawa T. Epidemiology and clinical characteristics of GERD in the Japanese population. J Gastroenterol. 2009;44:518–534. doi: 10.1007/s00535-009-0047-5. [DOI] [PubMed] [Google Scholar]
- 5.Wahlqvist P, Karlsson M, Johnson D, Carlsson J, Bolge SC, Wallander MA. Relationship between symptom load of gastro-oesophageal reflux disease and health-related quality of life, work productivity, resource utilization and concomitant diseases: survey of a US cohort. Aliment Pharmacol Ther. 2008;27:960–970. doi: 10.1111/j.1365-2036.2008.03671.x. [DOI] [PubMed] [Google Scholar]
- 6.Mody R, Bolge SC, Kannan H, Fass R. Effects of gastroesophageal reflux disease on sleep and outcomes. Clin Gastroenterol Hepatol. 2009;7:953–959. doi: 10.1016/j.cgh.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Johnson DA, Orr WC, Crawley JA, et al. Effect of esomeprazole on nighttime heartburn and sleep quality in patients with GERD: a randomized, placebo-controlled trial. Am J Gastroenterol. 2005;100:1914–1922. doi: 10.1111/j.1572-0241.2005.00285.x. [DOI] [PubMed] [Google Scholar]
- 8.Fujiwara Y, Kohata Y, Kaji M, et al. Sleep dysfunction in Japanese patients with gastroesophageal reflux disease: prevalence, risk factors, and efficacy of rabeprazole. Digestion. 2010;81:135–141. doi: 10.1159/000253849. [DOI] [PubMed] [Google Scholar]
- 9.Hongo M, Miwa H, Kusano M, ; J-FAST Group Effect of rabeprazole treatment on health-related quality of life and symptoms in patients with reflux esophagitis: a prospective multicenter observational study in Japan. J Gastroenterol. 2011;46:297–304. doi: 10.1007/s00535-010-0342-1. [DOI] [PubMed] [Google Scholar]
- 10.Mizuno H, Matsuhashi N, Sakaguchi M, et al. Recent effectiveness of proton pump inhibitors for severe reflux esophagitis: the first multicenter prospective study in Japan. J Clin Biochem Nutr. 2015;57:233–238. doi: 10.3164/jcbn.14-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becher A, El-Serag H. Systematic review: the association between symptomatic response to proton pump inhibitors and health-related quality of life in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;34:618–627. doi: 10.1111/j.1365-2036.2011.04774.x. [DOI] [PubMed] [Google Scholar]
- 12.Fujiwara Y, Kohata Y, Kaji M, et al. Sleep dysfunction in Japanese patients with gastroesophageal reflux disease: prevalence, risk factors, and efficacy of rabeprazole. Digestion. 2010;81:135–141. doi: 10.1159/000253849. [DOI] [PubMed] [Google Scholar]
- 13.Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30:1030–1038. doi: 10.1111/j.1365-2036.2009.04142.x. [DOI] [PubMed] [Google Scholar]
- 14.Turner-Bowker DM, Bayliss MS, Ware JE, Jr, Kosinski M. Usefulness of the SF-8 Health Survey for comparing the impact of migraine and other conditions. Qual Life Res. 2003;12:1003–1012. doi: 10.1023/a:1026179517081. [DOI] [PubMed] [Google Scholar]
- 15.Fukuhara S, Suzukamo Y.Manual of the SF-8 Japanese Version Institute for Health Outcomes & Process Evaluation Research; Kyoto, 2004 (in Japanese) [Google Scholar]
- 16.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 17.Doi Y, Minowa M, Okawa M, et al. Development of the Japanese version of the Pittsburgh Sleep Quality Index. Jpn J Psychiater Treat. 1998;13:755–763. (in Japanese) [Google Scholar]
- 18.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 19.El-Serag H, Becher A, Jones R. Systematic review: persistent reflux symptoms on proton pump inhibitor therapy in primary care and community studies. Aliment Pharmacol Ther. 2010;32:720–737. doi: 10.1111/j.1365-2036.2010.04406.x. [DOI] [PubMed] [Google Scholar]
- 20.Hiramoto K, Fujiwara Y, Ochi M, et al. Effects of esomeprazole on sleep in patients with gastroesophageal reflux disease as assessed on actigraphy. Intern Med. 2015;54:559–565. doi: 10.2169/internalmedicine.54.3718. [DOI] [PubMed] [Google Scholar]
- 21.Jansson C, Nordenstedt H, Wallander MA, et al. Severe gastro-oesophageal reflux symptoms in relation to anxiety, depression and coping in a population-based study. Aliment Pharmacol Ther. 2007;26:683–691. doi: 10.1111/j.1365-2036.2007.03411.x. [DOI] [PubMed] [Google Scholar]
- 22.Boltin D, Boaz M, Aizic S, et al. Psychological distress is not associated with treatment failure in patients with gastroesophageal reflux disease. J Psychosom Res. 2013;75:462–466. doi: 10.1016/j.jpsychores.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Heading RC, Mönnikes H, Tholen A, Schmitt H. Prediction of response to PPI therapy and factors influencing treatment outcome in patients with GORD: a prospective pragmatic trial using pantoprazole. BMC Gastroenterol. 2011;11:52. doi: 10.1186/1471-230X-11-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dickman R, Boaz M, Aizic S, Beniashvili Z, Fass R, Niv Y. Comparison of clinical characteristics of patients with gastroesophageal reflux disease who failed proton pump inhibitor therapy versus those who fully responded. J Neurogastroenterol Motil. 2011;17:387–394. doi: 10.5056/jnm.2011.17.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim SE, Kim N, Oh S, et al. Predictive factors of response to proton pump inhibitors in Korean patients with gastroesophageal reflux disease. J Neurogastroenterol Motil. 2015;21:69–77. doi: 10.5056/jnm14078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessing BF, Bredenoord AJ, Saleh CM, Smout AJ. Effects of anxiety and depression in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2015;13:1089–1095. doi: 10.1016/j.cgh.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 27.Kinoshita Y, Ashida K, Miwa H, Hongo M. The impact of lifestyle modification on the health-related quality of life of patients with reflux esophagitis receiving treatment with a proton pump inhibitor. Am J Gastroenterol. 2009;104:1106–1111. doi: 10.1038/ajg.2009.77. [DOI] [PubMed] [Google Scholar]
- 28.Tominaga K, Kato M, Takeda H, et al. A randomized, placebo-controlled, double-blind clinical trial of rikkunshito for patients with non-erosive reflux disease refractory to proton-pump inhibitor: the G-PRIDE study. J Gastroenterol. 2014;49:1392–1405. doi: 10.1007/s00535-013-0896-9. [DOI] [PubMed] [Google Scholar]
- 29.Tsuda Y, Fukui H, Sujishi T, et al. Is administrating branched-chain amino acid-enriched nutrition achieved symptom-free in malnourished cirrhotic patients? J Clin Biochem Nutr. 2014;54:51–54. doi: 10.3164/jcbn.13-64. [DOI] [PMC free article] [PubMed] [Google Scholar]