Abstract
Background:
Graft choice for anterior cruciate ligament (ACL) reconstruction is of critical importance. Various grafts have been used so far, with autografts long considered the optimal solution for the treatment of ACL-deficient knees. Limited data are available on the long-term survivorship of synthetic grafts.
Purpose:
To compare the functional outcome and survivorship of ACL reconstructions performed using the LARS (ligament augmentation and reconstruction system) ligament and the ABC (active biosynthetic composite) purely polyester ligament.
Study Design:
Case series; Level of evidence, 4.
Methods:
The results of 72 patients who underwent primary arthroscopic ACL reconstruction with the LARS ligament and 31 cases with an ABC purely polyester ligament were reviewed. The mean follow-up periods for the LARS and ABC groups were 9.5 and 5.1 years, respectively. A survivorship analysis of the 2 synthetic grafts was performed using the Kaplan-Meier method with a log-rank test (Mantel-Cox, 95% CI). Lysholm, Tegner activity, Knee injury and Osteoarthritis Outcome Score (KOOS), and International Knee Documentation Committee (IKDC) scores as well as laxity measurements obtained using a KT-1000 arthrometer were recorded for all intact grafts, and a Mann-Whitney U test was used for comparison reasons.
Results:
The rupture rates for LARS and ABC grafts were 31% (95% CI, 20%-42%) and 42% (95% CI, 25%-59%), respectively. For intact grafts, the mean Lysholm score was good for both groups (90 for the LARS group and 89 for the ABC group), with the majority of patients returning to their preinjury level of activities, and the mean IKDC score was 90 for the LARS group and 86 for the ABC group.
Conclusion:
The rupture rates of both LARS and ABC grafts were both high. However, the LARS ligament provided significantly better survivorship compared with the ABC ligament at short- to midterm follow-up (95% CI).
Keywords: anterior cruciate ligament, ACL rupture rate, LARS ligament, ABC purely polyester ligament
Anterior cruciate ligament (ACL) reconstruction is the sixth most common procedure performed in orthopaedic surgery, with more than 150,000 procedures documented annually in the United States.8 Biological tissue autograft reconstruction using bone–patellar tendon–bone (BTB) or hamstrings tendons (HT) is the most common method of ACL reconstruction with the most satisfying results.24,32,58 However, the use of autografts in ACL surgery has several drawbacks. There are complications, mainly associated with the harvesting of the grafts. With BTB autografts, some patients experience impaired function and significant morbidity at the donor site, including fracture of the patella, rupture or contracture of the patellar tendon, patellar tendonitis, and secondary anterior knee pain.6,21,34 Likewise, saphenous nerve injury and hamstring weakness can occur with hamstring harvest in HT autograft ACL reconstruction.26 Another drawback of autografts is the decrease in graft strength during the long period of revascularization. This may lead to graft laxity or rupture during early rehabilitation.11,41
To avoid the drawbacks of autograft ACL reconstruction, the option of artificial ligaments has been available since the 1980s. The early results of artificial ligaments were appealing but subsequent follow-up revealed numerous problems, including higher failure rates, sterile effusions from wear particles, bone tunnel enlargement, and late infection.3,14,17,18,20,37,44,47 Synthetic grafts also had a higher cost than autologous grafts.24
Over the past 2 decades, improved surgical techniques and new material designs providing a more anatomical form of reconstruction were developed. One such synthetic graft is the active biocompatible composite (ABC) purely polyester ligament (Surgicraft Ltd), which was developed by Angus Strover in the United Kingdom and has been used since 1985.50–52 It is manufactured from a partial polyester braid over a core of polyester. During the braiding process, the core fibers are disposed into a flat zig-zag configuration, which displays a unique biphasic response to loading, protecting the implant from plastic deformation.51 The implant has radial overbraiding at both ends (loops) to aid its fixation and acts as a scaffold, promoting tissue cover and ingrowth into the implant.52 It has an ultimate tensile strength of 3130 N.35 In 1992, after an analysis of early failures of the ABC ligament performed in the Textiles Department of Manchester University, England, new instrumentation and a modified surgical technique for the implantation of the ligament were introduced.5,35,37
Another scaffold-type artificial ligament, resulting from the development of new biomaterials and more accurate surgical techniques, is the LARS (ligament augmentation and reconstruction system; Surgical Implants and Devices) ligament. The LARS ligament was developed by JP Laboureau and was first implanted in 1992.13 It consists of fibers made of polyethylene terephthalate (PET).55 Unlike earlier synthetic ligaments, LARS consists of 2 distinct segments: an intraosseous and an intra-articular segment. Its intraosseous segment is composed of longitudinal fibers bounded together by a transverse knitted structure while the intra-articular segment consists of multiple parallel longitudinal fibers twisted at 90° angles.20 The architecture of the ligament allows it to mimic the native ACL. Shearing forces are reduced by orientating the free fibers of the intra-articular part of the graft clockwise or counterclockwise for use in right and left knees, respectively.32 Additionally, the intra-articular segment of the graft acts as a scaffold inducing fibroblastic ingrowth between the fibers of the ligament due to the porosity of the material.55 Ingrowth soft tissue between the ligament fibers acts as a viscoelastic element protecting the ligament against friction at the opening of the bony canal as well as between the artificial fibers themselves.39 The LARS ligament comes in different sizes of 60, 80, 100, and 120 fibers in diameter. The ultimate tensile strength of the ligament depends on its size starting from 2500 N for the 60 fibers and raising to 3600, 4600, and 5600 N for the 80, 100, and 120 fibers, respectively.61
To identify the role of synthetic grafts for ACL reconstruction, critical analysis of the long-term outcomes of synthetic grafts needs to be done.57 The aim of this study was to comparatively evaluate the functional outcome and survivorship of ACL reconstructions performed in our clinic using either the LARS graft or the ABC graft.
Methods
The study was approved by the Scientific Council and Bioethical Committees of the Greek Air Force 251 Military Hospital and the Attikon University Hospital of the Medical School of the University of Athens–Greece. Between September 1997 and July 2009, a total of 153 patients underwent primary ACL arthroscopic reconstruction with synthetic grafts. During that time period, the majority of ACL reconstructions performed at our center were done using synthetic grafts. The LARS synthetic graft (Figure 1) was used in a period between 1997 and 2003 whereas the ABC purely polyester ligament (Figure 2) was utilized from 2003 to 2009. The transition from LARS to ABC was decided by the hospital’s scientific and ethical board committee mainly under the setting of financial reformations. At that time, both grafts were considered of similar quality, and significant cost savings were achieved by switching to the ABC graft. The inclusion criteria for this study consisted of isolated traumatic ACL ruptures, with or without meniscal lesions, in amateur or professional athletes of any age eager to return quickly into activity. Exclusion criteria included patients with multiligament tears, associated fractures of the knee or other injuries, and comorbidities that would not have allowed the accelerated rehabilitation.
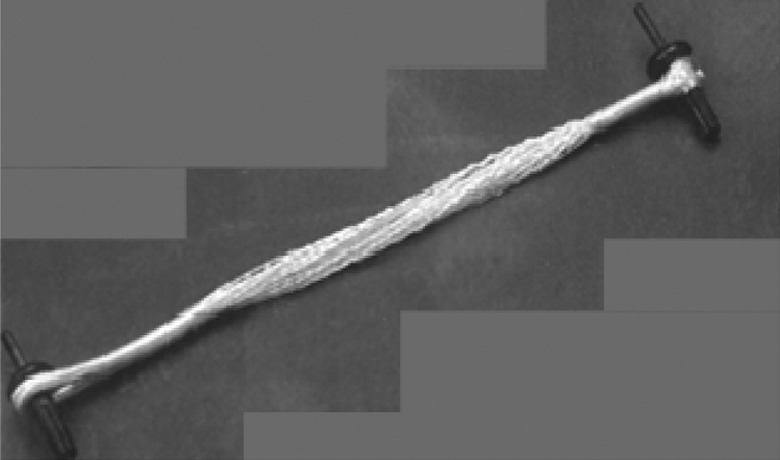
Figure 1.
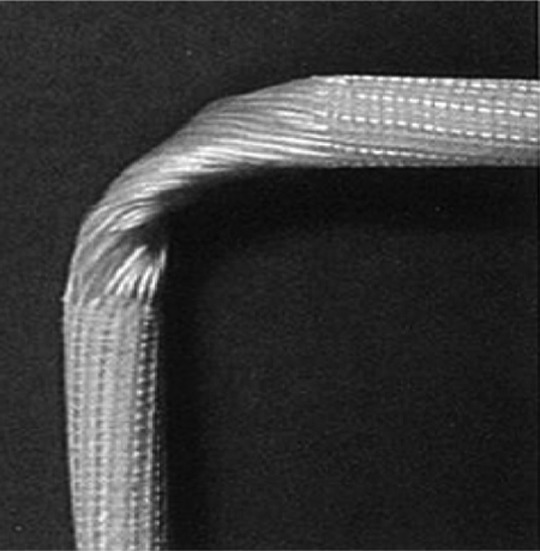
The ligament augmentation and reconstruction system (LARS) graft. The free fibers of the graft are twisted at a 90° angle.
Figure 2.
The active biosynthetic composite (ABC) purely polyester graft. The graft has a loop at either end, and a bollard fixation device is passed through each loop.
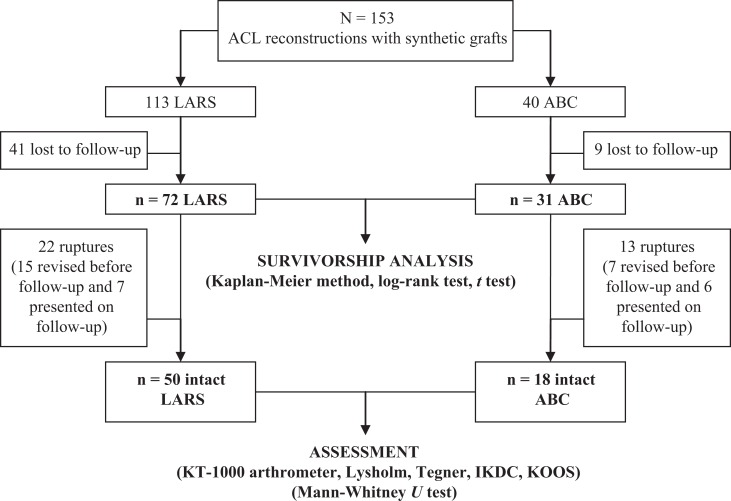
The LARS graft was used in 113 cases, whereas the ABC graft was used in 40 cases. Forty-one patients with a LARS graft (36%) and 9 patients with an ABC graft (22%) were lost to follow-up, leaving 103 patients for review: 72 patients in the LARS graft and 31 patients in the ABC graft group (Figure 3).
Figure 3.
Study design flowchart. ABC, active biosynthetic composite; ACL, anterior cruciate ligament; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; LARS, ligament augmentation and reconstruction system.
As this study was carried out at a military hospital, the majority of patients were male soldiers serving their obligatory military service. All patients with a LARS graft were males with a mean age of 26.1 years at the time of surgery (range, 18-43 years). The mean follow-up was 9.5 years (range, 6-14 years). The ABC group included 28 males (90%) and 3 females (10%) with a mean age of 28.4 years at the time of surgery (range, 19-46 years) and a mean follow-up of 5.1 years (range, 1-8 years). Fifty-one patients (71%) of the LARS group suffered meniscal tears: 31 of which were medial, 11 lateral, and 9 bilateral. In the ABC group, 23 patients (74%) had meniscal tears: 16 of which were medial, 3 lateral, and 4 bilateral. None of the meniscal tears in either group was amenable to suture repair, and therefore, in all cases a partial meniscectomy was performed (Table 1).
TABLE 1.
Patient Demographicsa
| Variable | Data |
|---|---|
| LARS group (n = 72 patients) | |
| Follow-up, y | Mean ± SD, 9.5 ± 1.81 Median (range), 9.0 (6-14) |
| Subject age, y | Mean ± SD, 26.1 ± 6.02 Median (range), 25.0 (18-43) |
| Sex | 72 males (100%), 0 females (0%) |
| Meniscal tears | 51 knees (71%): 31 medial, 11 lateral, 9 both |
| ABC group (n = 31 patients) | |
| Follow-up, y | Mean ± SD, 5.1 ± 1.78 Median (range), 5.0 (1-8) |
| Subject age, y | Mean ± SD, 28.4 ± 6.8 Median (range), 26.0 (19-46) |
| Sex | 28 males (90%), 3 females (10%) |
| Meniscal tears | 23 knees (74%): 16 medial, 3 lateral, 4 both |
aABC, active biosynthetic composite; LARS, ligament augmentation and reconstruction system.
At a mean 8.2 years postoperatively (range, 1-14 years), patients from both groups were invited for a follow-up examination to assess their postoperative outcome. For LARS patients, the follow-up period was significantly longer than that of ABC patients; however, this was unavoidable in the setting of the different time periods during which those grafts were used (LARS grafts were used in an earlier period). Patients were examined by the use of a KT-1000 arthrometer (MEDmetric Corp)12 to assess the side-to-side difference in laxity between the operated and nonoperated knee. All tests were performed by 2 doctors who were familiar with the use of this instrument. Additionally, the Lysholm score,30 Tegner activity score,53 the Knee injury and Osteoarthritis Outcome Score (KOOS),46 and the International Knee Documentation Committee (IKDC) score, including the IKDC 2000 subjective knee evaluation and examination form,22 were used to assess the postoperative outcome.
Fifteen patients (21%) of the LARS group had already had revision surgery for graft failure, whereas 7 patients (10%) presented on follow-up examination with rupture of the graft. Similarly, in the ABC group, 7 patients (23%) had already had revision surgery for graft failure and 6 patients (19%) presented on follow-up examination with graft rupture. Those LARS and ABC patients with graft failures were not included in the functional outcome scores or KT-1000 arthrometer measurements. They were included, though, in the survivorship data.
Surgical Technique
An arthroscopic procedure for reconstruction of the ACL was carried out in all patients. However, there were differences in the surgical technique using a LARS graft from that using an ABC according to each manufacturer’s guidelines. The major difference was that the LARS graft (see Figure 1) was placed through a femoral tunnel located within the ACL insertion site, while the ABC ligament (see Figure 2) was placed in a groove created in the “over-the-top” position of the lateral femoral condyle. Another significant difference in the surgical technique among the 2 grafts was the method of their fixation to the bone. The LARS graft was fixed at both ends using LARS cannulated interference screws. These were titanium screws designed for easy insertion into the tunnels by virtue of the conical shape at the tip of the screw. Deep threaded shoulders and blunt outer edges maximized the fixation without damage to the ligament and ensured maximum contact between the screw and the tunnel wall to prevent tunnel widening. In the ABC method, the graft was fixed proximally and distally using a bollard fixation device (see Figure 2). This was a double polysulfone bollard. First, a unicortical drill hole was prepared in the bone using a special drill. The bollard was then placed through a loop at either end of the implant and was introduced into the drill hole. The bollard was secured by tapping home the expansion pin in the bollard, providing a strong unicortical fixation.
In the LARS method, the femoral (Figure 4) and tibial isometric points were identified by preoperative radiography, and the entire procedure was performed arthroscopically with fluoroscopic control. The femoral tunnel was created using an anteromedial portal technique. A guide pin was drilled from the isometric point across the femur and out the lateral thigh. A small incision was enlarged using graduated telescopic tubes, and the tunnel was reamed from outside-in. The tibial tunnel guide pin was placed at the center of the ACL footprint using an ACL guide set at approximately 65° to the tibial plateau in the sagittal plane. The guide pin was overreamed with the appropriate sized drill. Special attention was given while drilling the tunnels not to damage the stumps of the native ACL. The LARS ligament was then inserted through the tunnels and fixed on the femoral side with a LARS interference screw. The graft was then tensioned and ranged to ensure no impingement. Final fixation on the tibial side was performed using a LARS interference screw at 20° of flexion with a posterior drawer force being applied to the tibia. Once fixation of the ligament was completed, the redundant extremities of the ligament were cut flush with the bone. Based on manufacturer’s instructions, in patients with less than 80 kg of body weight, an 80-gauge fiber graft was used, whereas for patients heavier than 80 kg, 100-gauge fiber grafts were preferred.
Figure 4.
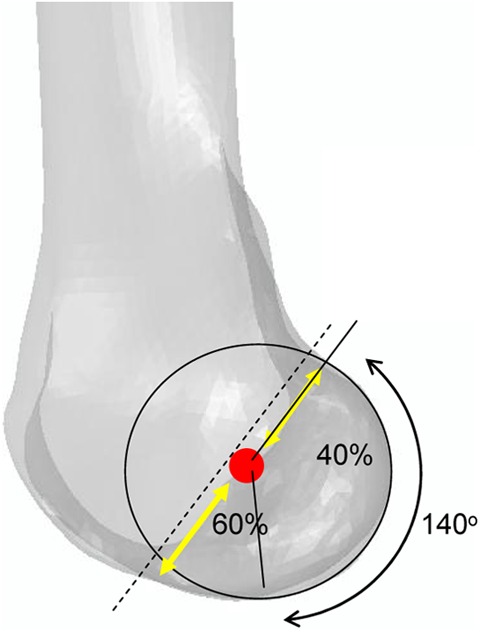
The isometric femoral point (red dot) is located in the center of an arc of approximately 140° formed by the posterior condyle. It is also located at 60% of a line drawn parallel to the Blumensaat line and passing through the most prominent point of the posterior condyle.
For the ABC ligament, the graft was implanted into the knee joint by use of special instrumentation provided by the manufacturing company. The tibial tunnel was created with the aid of a specialized guide to avoid impingement of the graft on the roof and lateral wall of the intercondylar notch. The opening of the tibial tunnel was chamfered to minimize graft abrasion. Through a lateral incision, the over-the-top position of the lateral femoral condyle was identified and cleared of soft tissue. With the knee in full extension, a blunt trocar was inserted into the knee joint through the tibial tunnel, penetrating the posterior capsule of the knee. The surgeon’s finger was placed in the over-the-top position to avoid injury to the popliteal fossa structures. A 2- to 3-mm groove was created in the over-the-top position with a single-sided rasp. The ABC ligament was then inserted into the knee joint passing through the tibial tunnel and from the over-the-top femur position and was fixed at both ends with a bollard fixation device. The tibial end of the graft was fixed first and the femoral side temporarily fixed with a K-wire passed through a special handle that held the graft. After ensuring that stability had been restored and that there was no impingement, final femoral fixation was achieved with the second bollard fixation device.
Rehabilitation Program
After surgery, all patients were enrolled in an accelerated physical therapy program broadly similar to that described by Shelbourne and Nitz.49 Emphasis was placed on restoration of full extension and of quadriceps muscle function as soon as possible after surgery. An unlocked functional knee brace was kept for safety reasons for 1 month. From the first postoperative day, patients were encouraged to walk with full extension of the knee and weightbearing according to tolerance. Extension range of motion (ROM) exercises, such as heel props and towel extensions, were performed. Flexion ROM exercises included heel slides, wall slides, and active/assistive flexion. Early leg control was accomplished with quadriceps setting, straight-leg raises, and active knee hyperextension.
By the end of the second postoperative week, the patient should have been able to demonstrate normal gait, full passive extension, 130° of flexion, and good quadriceps leg control. During this week, patients added prone hangs to their daily ROM exercises. Patients were encouraged to stand with their weight over their reconstructed knee with the quadriceps contracted, which locked the knee into full hyperextension.
Four weeks after surgery, patients were allowed unlimited activities of daily living. Muscle strengthening exercises included both closed kinetic chain (CKC) and open kinetic chain (OKC) exercises such as step downs, leg press, stationary bicycle, leg extensions, step machines, and half squats.
Participation in light sports activities was permitted by the end of the eighth week. Patients performed light agility drills and proprioceptive activity that included a running progression, lateral slides, crossovers, and single-leg hopping. Return to competitive sports was allowed as early as 4 months after surgery.
Statistical Analysis
After collection and evaluation of the data, an analysis of the survivorship of the 2 synthetic grafts was performed using the Kaplan-Meier method. A log-rank test (Mantel-Cox, 95% CI) of the 2 Kaplan-Meier curves was then used to define whether there was a statistically significant difference in survivorship between these 2 types of grafts. The end-point of survival of each graft was the date of the magnetic resonance imaging examination that revealed the rupture. Subsequently, 2-sided t tests (95% CI) were performed to show how long after surgery each graft may last. Finally, a Mann-Whitney U test was used to indicate whether there was significant difference between the subjective outcome scores and the KT-1000 arthrometer measurements among the intact LARS and ABC grafts.
Results
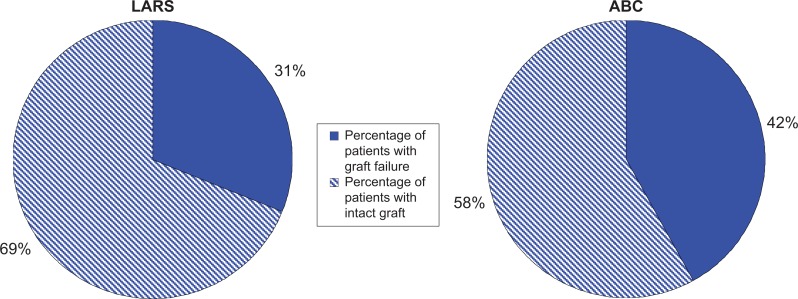
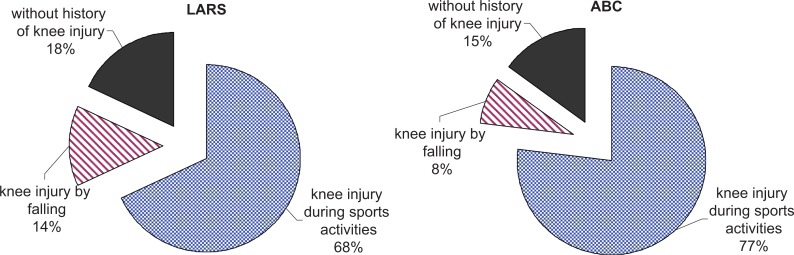
In total, 35 of 103 artificial ACL grafts (34%) were ruptured (Figure 5), including 22 of 72 LARS grafts (31%) and 13 of 31 ABC grafts (42%) (Figure 6). In the LARS group, 15 of 22 patients with graft failure had already been revised prior to our investigation while the remaining 7 patients presented on follow-up examination with a graft rupture. Likewise, in the ABC group, 7 of 13 patients with graft failure were revised at an earlier point and the remaining 6 patients presented on follow-up examination with graft rupture. Most ruptures occurred as a result of knee injury, with the majority of them taking place during sports activities (Figure 7). It is worth noting that more “less traumatic” (without history of knee injury) graft failures occurred in the LARS group. As the LARS group had a longer follow-up period, these “less traumatic” ruptures may signal graft wear.
Figure 5.
Total rupture percentages for ligament augmentation and reconstruction system (LARS) and active biosynthetic composite (ABC) grafts. Time of follow-up differs significantly. The mean follow-up for the LARS and ABC grafts was 9.5 years (range, 6-14 years) and 5.1 years (range, 1-8 years), respectively.
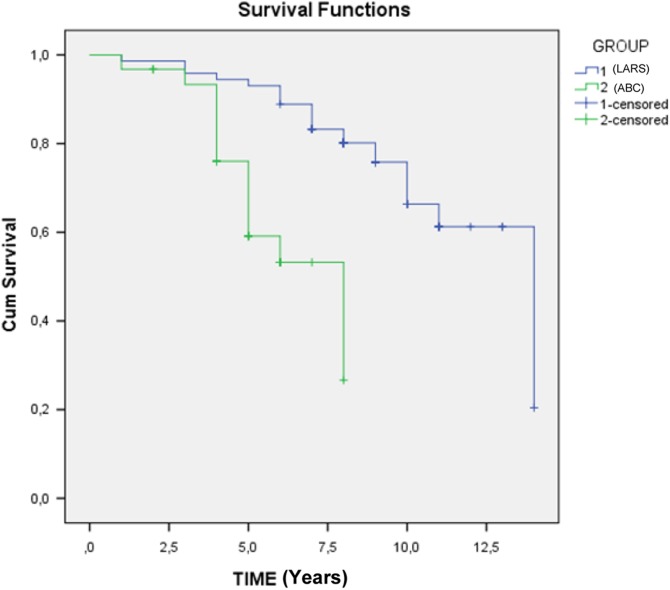
Figure 6.
Kaplan-Meier survivorship curves for all anterior cruciate ligament reconstructions using the ligament augmentation and reconstruction system (LARS) and active biosynthetic composite (ABC) grafts.
Figure 7.
Rate of knee injury among patients with failed ligament augmentation and reconstruction system (LARS; n = 22) and active biosynthetic composite (ABC; n = 13) grafts.
A log-rank test (Mantel-Cox, 95% CI) of the 2 Kaplan-Meier survivorship curves (Figure 6) showed a statistically significant difference between the 2 grafts. The chi-square statistic was 17.57 (degrees of freedom, 1). Although both grafts had high failure rates, the LARS ligament demonstrated significantly better endurance compared with the ABC graft. The mean survival was 8.8 years for the LARS reconstructions and 5 years for the ABC reconstructions.
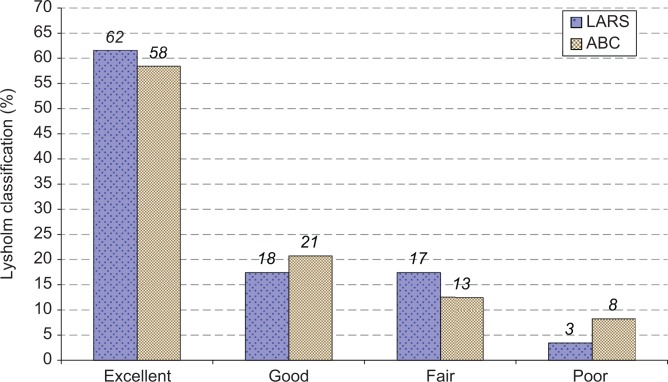
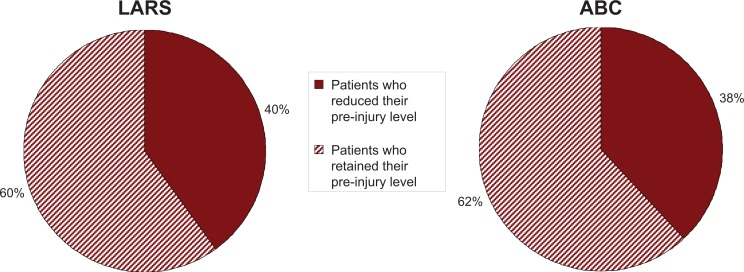
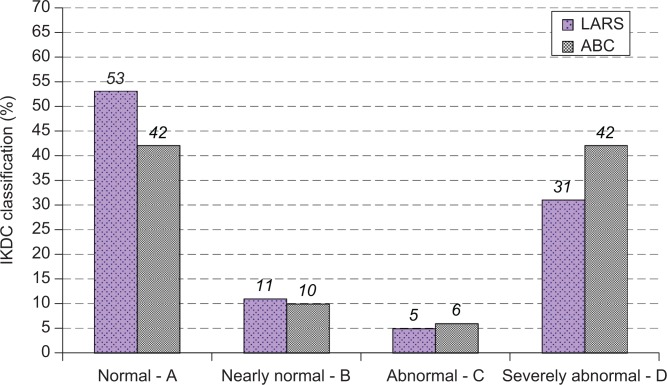
At a mean follow-up of 9.5 years (range, 6-14 years), patients with an intact LARS graft (n = 50) demonstrated a mean difference of anterior tibial displacement of 2 mm between the operated and the healthy knee at 134 N of force and 2.9 mm with manual maximum displacement testing. For those patients of the LARS group with an intact graft, the mean Lysholm score was 90 (out of 100) (Figure 8), the mean IKDC 2000 subjective score was 90 (out of 100), and the mean KOOS score was satisfying for all the parameters examined (Tables 2 and 3). The mean Tegner activity level score prior to injury was 7, while on follow-up after surgery it was 6 (Table 2), with 60% of patients retaining their preinjury level of activity (Figure 9). For patients with high Tegner activity level prior to surgery (eg, 7-10), 57% retained the same activity level postoperatively until follow-up examination. However, according to the IKDC evaluation score, when all LARS graft patients (n = 72) were included (both patients with intact and failed LARS grafts), 53% of the operated knees were qualified as normal, 11% as nearly normal, 5% as abnormal, and 31% as severely abnormal (Figure 10).
Figure 8.
Classification for patients with intact ligament augmentation and reconstruction system (LARS) and active biosynthetic composite (ABC) grafts according to Lysholm score.
TABLE 2.
Mean Postoperative Outcome Scores for Patients With Intact LARS and ABC Graftsa
| Outcome Measure | Mean ± SD | Median (Range) |
|---|---|---|
| LARS group | ||
| Lysholm test | 90 ± 11.94 | 95 (50-100) |
| IKDC 2000 subjective outcome score | 90 ± 14.85 | 95 (44-100) |
| Tegner activity score | ||
| Before injury | 7 ± 1.30 | 7 (2-10) |
| At follow-up | 6 ± 1.95 | 7 (1-9) |
| ABC group | ||
| Lysholm test | 89 ± 15.15 | 95 (45-100) |
| IKDC 2000 subjective outcome score | 86 ± 17.81 | 96 (44-100) |
| Tegner activity score | ||
| Before injury | 7 ± 2.26 | 7 (1-9) |
| At follow-up | 6 ± 2.30 | 7 (1-9) |
aABC, active biosynthetic composite; IKDC, Internationl Knee Documentation Committee; LARS, ligament augmentation and reconstruction system.
TABLE 3.
Postoperative KOOS Results of Patients With Intact LARS and ABC Graftsa
| KOOS Subscale | Mean ± SD | Median (Range) |
|---|---|---|
| LARS group | ||
| Pain | 96 ± 6.90 | 100 (69-100) |
| Symptoms | 91 ± 8.57 | 93 (57-100) |
| ADL | 98 ± 4.69 | 100 (79-100) |
| Sport/Rec | 92 ± 14.72 | 100 (35-100) |
| QoL | 81 ± 21.93 | 88 (19-100) |
| Stiffness | 98 ± 4.80 | 100 (88-100) |
| ABC group | ||
| Pain | 95 ± 8.23 | 100 (72-100) |
| Symptoms | 86 ± 13.60 | 91 (46-100) |
| ADL | 98 ± 4.23 | 100 (84-100) |
| Sport/Rec | 87 ± 21.31 | 100 (30-100) |
| QoL | 82 ± 21.86 | 94 (25-100) |
| Stiffness | 94 ± 11.05 | 100 (63-100) |
aABC, active biosynthetic composite; ADL, activities of daily living; KOOS, Knee injury and Osteoarthritis Outcome Score; LARS, ligament augmentation and reconstruction system; QoL, quality of life; Sport/Rec, sports and recreation.
Figure 9.
Percentage of patients with intact ligament augmentation and reconstruction system (LARS) and active biosynthetic composite (ABC) grafts who retained their preinjury level of activities.
Figure 10.
Postoperative classification of knee joints according to Internationl Knee Documentation Committee (IKDC) evaluation for all anterior cruciate ligament reconstructions using ligament augmentation and reconstruction system (LARS) and active biosynthetic composite (ABC) grafts. All patients from both groups, those with intact and those with failed grafts, are included.
At a mean follow-up of 5.1 years, patients with intact ABC grafts (n = 18) demonstrated a mean difference of anterior tibial displacement of 2.5 mm between the operated and healthy knee at 134 N of applied force and 3.1 mm with manual maximum displacement testing. For those patients with an intact ABC graft, the postoperative mean Lysholm score was 89 (Figure 8), the mean IKDC 2000 subjective score was 86, and the mean KOOS score was satisfying for all the parameters examined (Tables 2 and 3). The mean Tegner activity level score was 7 prior to injury, whereas it was estimated to be 6 on follow-up after surgery (Table 2), with 63% of the patients retaining their preinjury level of activity (Figure 9). For patients with high Tegner activity level prior to surgery (eg, 7-10), 50% retained the same activity level postoperatively until follow-up examination. The IKDC evaluation score when all patients of the ABC (n = 31) were included (those with intact and those with failed ABC grafts) qualified 42% of the operated knees as normal, 10% as nearly normal, 6% as abnormal, and 42% as severely abnormal (Figure 10).
A Mann-Whitney U test comparing the subjective outcome scores and KT-1000 measurements between the intact LARS and ABC grafts showed that there was no statistically significant difference among them (P > .05 for each category) (Table 4).
TABLE 4.
Mann-Whitney U Test Results for Subjective Outcome Scores and KT-1000 Measurements Among Intact LARS Grafts (n = 50) and ABC Grafts (n = 18)a
| Measure | Mann-Whitney U Test | P Value |
|---|---|---|
| KOOS subscale | ||
| Pain | 367 | .188 |
| Symptoms | 365 | .230 |
| ADL | 448 | .962 |
| Sport/Rec | 496 | .458 |
| QoL | 400 | .475 |
| Stiffness | 410 | .440 |
| Lysholm | 413 | .597 |
| Subjective IKDC 2000 | 436 | .837 |
| Tegner activity score | ||
| Before injury | 424 | .685 |
| At follow-up | 437 | .840 |
| Difference in scores | 432 | .767 |
| KT-1000 arthrometer side-to-side difference | ||
| At 134 N | 433 | .219 |
| Manual maximum displacement | 433 | .223 |
aABC, active biosynthetic composite; ADL, activities of daily living; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; LARS, ligament augmentation and reconstruction system; QoL, quality of life; Sport/Rec, sports and recreation.
Other than graft failure, there were no complications noted in either group (eg, infection, thrombophlebitis, etc).
Discussion
The ideal graft choice for ACL reconstruction has been debated by the orthopaedic community for over 30 years. The majority of synthetic ACL grafts used in the past have exhibited poor long-term physiologic and functional outcomes.32 Permanent synthetic ACL grafts were found to be prone to creep, fatigue, and mechanical failure,9 and on the other hand, tissue ingrowth scaffolds and ligament augmentation devices appeared unable to provide adequate mechanical support while avoiding stress-shielding of the host tissue.32 Because of the previous high failure rates of synthetic ligaments, most surgeons utilize autograft or allograft for ACL reconstruction.1,25,28,32 However, the desire to have a readily available, sterile, synthetic graft that avoids donor site morbidity remains appealing. The LARS and ABC synthetic ligaments have been designed to avoid some of the graft abrasion problems found in previous synthetic grafts, but little data are available on their long-term outcomes.42,45 Our study had the advantage of long-term follow-up of 2 synthetic grafts and is the first study to our knowledge comparing these 2 grafts.
The rupture rate of 31% for the LARS ligament found in this series is higher in comparison with other studies, suggesting the LARS ligament as a suitable option for primary ACL reconstruction, with good clinical results comparable to that of autografts.15,16,19,27,29,39,42,60 However, the duration of follow-up was relatively short in all these studies, with the longest achieving 5 years, which differs significantly with the mean follow-up of 9.5 years (range, 6-14 years) in our study. The need for long-term results for the LARS ligament is also highlighted by systematic review studies, which nevertheless demonstrated good results with its use but always under the prism of short- to medium-term follow-up.31,38,40 Indeed, 1 of these systematic review studies concluded that although the short-term results for the LARS ligament appear good and are not significantly different from that of autografts, there is real concern that late failure may occur based on the results of long-term studies of other PET grafts.38
In response to previous concerns dictated by systematic review studies, recently published longer term follow-up studies of the LARS ligament have advocated in favor of satisfying results, comparable to that of autografts.10,43 Specifically, Cerulli et al10 presented a survival rate of 100% at 9 years follow-up and Parchi et al43 a rupture rate of about 4% at a mean follow-up of 8 years. There are important differences between these 2 studies and ours, however, which might be the cause for the different results we obtained. The patients in the study by Cerulli et al10 were significantly older (mean age, 46 years) compared with our active military population (mean age, 26.1 years). Similarly, in the study by Parchi et al,43 all the operations were performed on patients older than 30 years. Additionally, in both studies the exact preoperative and postoperative activity level of the patients was not clarified since the Tegner activity level was not reported. It is known, however, that patients with higher activity level may have an increased rate of ACL graft rupture.4,56 It is also known that younger patients tend to have higher activity levels both before and after surgery48 and are at increased risk for graft rupture.56 Since traumatic failure of the graft is often considered the primary cause of failure,7,33,59 the risk of reinjury increases when patients return to high-demand activities.4,56 While synthetic ACL grafts might have a role in older, lower demand patients, we found an unacceptably high failure rate in younger, active patients. We caution against the use of the LARS ligament in this population.
The results of our study for the LARS ligament are in agreement with the long-term follow-up study by Tiefenboeck et al.54 In their series of 18 patients, they found a 50% failure rate with a minimum follow-up of 10 years. We found similar failure rates in our larger group of patients.
As for the ABC artificial ligament, there are surprisingly few studies reporting on results, and no long-term outcome studies are available. The ABC ligament has been used during 2 distinct time periods. After it was introduced in 1985 until 1991, the ABC ligament was implanted via an open arthrotomy.36 The ligament was inserted into the knee joint through the tibial tunnel and was brought over the top of the lateral femoral condyle. After appropriate tensioning, the ligament was fixated at both ends with monocortical polysulfone flanged bollards. In 1990, a detailed mode analysis of early failures, undertaken in the Textiles Department at Manchester University, showed clear evidence of fatigue and mechanical failure occurring at the intra-articular tibial tunnel exit.35 This led to the development and introduction of new instrumentation and a modified surgical technique to avoid graft abrasion and impingement. From 1992 onward, a specially designed tibial jig was used to avoid roof impingement, and a back radius cutter was used to chamfer the tibial tunnel opening to reduce abrasion.
In our study, the ABC ligament was implanted using the new instrumentation and the revised surgical technique introduced in 1992. Jadeja et al23 evaluated the results of ACL reconstruction using the ABC ligament and compared the results before and after the newer instrumentation was developed. They noted a significant improvement in survivorship with the change in instrumentation. The newer technique had a low initial failure rate (0% in the first 3 years), but that increased to 27.9% at 5-year follow-up.
Petrou et al45 reported on a series of ABC ligaments placed using the newer instruments via an arthrotomy and an accelerated rehabilitation program. They found a survival rate of 100% at follow-up of 4 to 7 years. Our results were markedly different, with a 42% failure rate at a mean follow-up of 5.1 years. We cannot readily explain the significant differences between our study and that by Petrou et al,45 but our results are similar to those of Jadeja et al.23
Our study is the first, to our knowledge, to compare the results of the LARS and ABC synthetic ligaments. We found the survivorship to be significantly better for the LARS ligament. Possible reasons for this could be: the greater ultimate strength of the LARS ligament, the unique architecture of the LARS ligament, or the difference in recommended surgical technique. It should also be noted that patients with intact ligaments had good outcome scores regardless of which synthetic ligament was implanted. However, based on our results, we do not recommend the use of either the LARS or ABC synthetic ligaments as suitable grafts for primary ACL reconstructions. Further research is required to develop a synthetic ACL ligament that can withstand the high demands of a young, athletic patient.
This series has a number of limitations that can be summarized as follows: First, it is a retrospective study including 2 groups that were operated in different time periods during which each graft was the standard of care, concerning synthetic ACL grafts, in our hospital. The retrospective nature of the study may have caused inherent difficulties in data collection, such as the exact cause of synthetic graft rupture, whereas different time periods chronically may correspond to different levels of surgical experience acquired between the 2 groups, since all the operations were performed by the same surgical team. Additionally, the cohorts were exclusively or predominantly male, which also adds bias to the representative status of the findings since a high incidence of ACL injuries is also recorded in women.2 The preponderance of male patients in our series, which is observed in both the LARS and ABC groups, is due to the fact that this study was carried out at a military hospital, thus a large number of patients relate to male soldiers serving their obligatory military service. Another limitation was that synthetic ACL rupture timing was calculated at the time of a positive magnetic resonance imaging examination, leaving uncertainty about the exact survival endurance of the grafts, which should be considered to be less than calculated. Also, differences in the technique used for the implantation of each graft could be a reason for the variation in survivorship between them. Finally, a considerable percentage of patients were lost to follow-up, which might mask an even higher failure rate of the grafts.
Conclusion
Conclusively, both LARS and ABC grafts exhibited a high rupture rate of 31% and 42%, respectively. However, the LARS graft had significantly better survival compared with the ABC ligament at short- to midterm follow-up. At the present time, synthetic ACL grafts should be avoided in younger, active patients.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Andersson D, Samuelsson K, Karlsson J. Evidence-based medicine series systematic review: treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. J Arthrosc Relat Surg. 2009;25:653–685. [DOI] [PubMed] [Google Scholar]
- 2. Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694–701. [DOI] [PubMed] [Google Scholar]
- 3. Arnauw G, Verdonk R, Harth A, et al. Prosthetic versus tendon allograft replacement of ACL-deficient knees. Acta Orthop Belg. 1991;57(suppl II):67–74. [PubMed] [Google Scholar]
- 4. Barrett AM, Craft JA, Replogle WH, Hydrick JM, Barrett GR. Anterior cruciate ligament graft failure: a comparison of graft type based on age and Tegner activity level. Am J Sports Med. 2011;39:2194–2198. [DOI] [PubMed] [Google Scholar]
- 5. Barry M, Kong KC, Thomas R, Mowbray MAS. Instrumentation to avoid impingement lesions in anterior cruciate ligament reconstruction. Knee. 1996;3:191–197. [Google Scholar]
- 6. Bonamo JJ, Krinick RM, Sporn AA. Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction. A report of two cases. J Bone Joint Surg Am. 1984;66-A:1294–1297. [PubMed] [Google Scholar]
- 7. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40:1985–1992. [DOI] [PubMed] [Google Scholar]
- 8. Busam ML, Fulkerson JP, Gaskill TR, Moorman CT, 3rd, Noyes FR, Galloway MT. Technical aspects of anterior cruciate ligament reconstruction for the general orthopaedic surgeon. Instr Course Lect. 2011;60:485–497. [PubMed] [Google Scholar]
- 9. Cao Y, Vacanti J, Ma X, et al. Generation of neo-tendon using synthetic polymers seeded with tenocytes. Transplant Proc. 1994;26:3390–3392. [PubMed] [Google Scholar]
- 10. Cerulli G, Antinolfi P, Bruè S, et al. Clinical experience using biomaterials in the knee. GIOT. 2011;37:159–166. [Google Scholar]
- 11. Clancy WG, Jr, Narechania RG, Rosenberg TD, et al. Anterior and posterior cruciate ligament reconstruction in rhesus monkeys. J Bone Joint Surg Am. 1981;63-A:1270–1284. [PubMed] [Google Scholar]
- 12. Daniel DM, Stone ML, Sachs R, Malcolm L. Instrumented measurement of anterior knee laxity in patients with acute ACL disruption. Am J Sports Med. 1985;13:401–407. [DOI] [PubMed] [Google Scholar]
- 13. Dericks G. Ligament advanced reinforcement system anterior cruciate ligament reconstruction. Oper Tech Sports Med. 1995;3:187–205. [Google Scholar]
- 14. Engström B, Wredmark T, Westblad P. Patellar tendon or Leeds-Keio graft in the surgical treatment of anterior cruciate ligament ruptures. Intermediate results. Clin Orthop Relat Res. 1993;295:190–197. [PubMed] [Google Scholar]
- 15. Fan Q, Fan J. Comparison between four-strand semitendinosus tendon autograft and ligament advanced reinforcement system for anterior cruciate ligament reconstruction by arthroscopy [in Chinese]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008;22:676–679. [PubMed] [Google Scholar]
- 16. Gao K, Chen S, Wang L, et al. Anterior cruciate ligament reconstruction with LARS artificial ligament: a multicenter study with 3- to 5-year follow-up. Arthroscopy. 2010;26:515–523. [DOI] [PubMed] [Google Scholar]
- 17. Gillquist J, Odensten M. Reconstruction of old anterior cruciate ligament tears with a Dacron prosthesis. A prospective study. Am J Sports Med. 1993;21:358–366. [DOI] [PubMed] [Google Scholar]
- 18. Guidoin MF, Marois Y, Bejui J, Poddevin N, King MW, Guidoin R. Analysis of retrieved polymer fiber based replacements for the ACL. Biomaterials. 2000;21:2461–2474. [DOI] [PubMed] [Google Scholar]
- 19. Guo L, Chen H, He R, et al. Short-term effectiveness of anterior cruciate ligament reconstruction with LARS artificial ligament [in Chinese]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2011;25:921–924. [PubMed] [Google Scholar]
- 20. Huang JM, Wang Q, Shen F, Wang ZM, Kang YF. Cruciate ligament reconstruction using LARS artificial ligament under arthroscopy: 81 cases report. Chin Med J (Engl). 2010;123:160–164. [PubMed] [Google Scholar]
- 21. Hughston JC. Complications of anterior cruciate ligament surgery. Orthop Clin North Am. 1985;16:237–240. [PubMed] [Google Scholar]
- 22. International Knee Documentation Committee. Knee ligament injury and reconstruction evaluation In: Aichroth PM, Cannon WD, Jr, eds. Knee Surgery: Current Practice. New York, NY: Raven; 1992:759–760. [Google Scholar]
- 23. Jadeja H, Yeoh D, Lai M, Mowbray M. Patterns of failure with time of an artificial scaffold class ligament used for reconstruction of the human anterior cruciate ligament. Knee. 2007;14:439–442. [DOI] [PubMed] [Google Scholar]
- 24. Johnson D. Why synthetic grafts failed In: Prodromos CC, ed. The Anterior Cruciate Ligament. Reconstruction and Basic Science. Philadelphia, PA: Saunders; 2008:88–90. [Google Scholar]
- 25. Johnson RJ, Beynnon BD, Nichols CE, Renstrom PA. The treatment of injuries of the anterior cruciate ligament. J Bone Joint Surg Am. 1992;74-A:140–151. [PubMed] [Google Scholar]
- 26. Koski JA, Ibarra C, Rodeo SA. Tissue-engineered ligament: cells, matrix, and growth factors. Orthop Clin North Am. 2000;31:437–452. [DOI] [PubMed] [Google Scholar]
- 27. Lavoie P, Fletcher J, Duval N. Patients satisfaction needs as related to knee stability and objective findings after ACL reconstruction using the LARS artificial ligament. Knee. 2000;7:157–163. [DOI] [PubMed] [Google Scholar]
- 28. Legnani C, Ventura A, Terzaghi C, Borgo E, Albisetti W. Anterior cruciate ligament reconstruction with synthetic grafts. A review of literature. Int Orthop. 2010;34:465–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu Z, Zhang X, Jiang Y, Zeng BF. Four-strand hamstring tendon autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Int Orthop. 2010;34:45–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. [DOI] [PubMed] [Google Scholar]
- 31. Machotka Z, Scarborough I, Duncan W, Kumar S, Perraton L. Anterior cruciate ligament repair with LARS (ligament advanced reinforcement system): a systematic review. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mascarenhas R, MacDonald PB. Anterior cruciate ligament reconstruction: a look at prosthetics—past, present and possible future. McGill J Med. 2008;11:29–37. [PMC free article] [PubMed] [Google Scholar]
- 33. Mayr R, Rosenberger R, Agraharam D, Smekal V, El Attal R. Revision anterior cruciate ligament reconstruction: an update. Arch Orthop Trauma Surg. 2012;132:1299–1313. [DOI] [PubMed] [Google Scholar]
- 34. McCarroll JR. Fracture of the patella during a golf swing following reconstruction of the anterior cruciate ligament: a case report. Am J Sports Med. 1983;11:26–27. [DOI] [PubMed] [Google Scholar]
- 35. McLeod ARM. The Development of the ABC Prosthetic Ligament System Following Mode of Failure Analysis [dissertation]. Manchester, UK: University of Manchester Institute of Science and Technology; 1995. [Google Scholar]
- 36. Mody BS, Howard L, Harding ML, Parmar HV, Learmonth DJ. The ABC carbon and polyester prosthetic ligament for ACL deficient knees. Early results in 31 cases. J Bone Joint Surg Br. 1993;75:818–821. [DOI] [PubMed] [Google Scholar]
- 37. Mowbray M. Reconstruction of the anterior cruciate ligament of the knee using an artificial ligament. Surg Tech Orthop Traumatol. 2001;B10:55–540. [Google Scholar]
- 38. Mulford JS, Chen D. Anterior cruciate ligament reconstruction: a systematic review of polyethylene terephthalate grafts. ANZ J Surg. 2011;81:785–789. [DOI] [PubMed] [Google Scholar]
- 39. Nau T, Lavoie P, Duval N. A new generation of artificial ligaments in reconstruction of the anterior cruciate ligament. Two-year follow-up of randomised trial. J Bone Joint Surg Br. 2002;84:356–360. [DOI] [PubMed] [Google Scholar]
- 40. Newman SD, Atkinson HD, Willis-Owen CA. Anterior cruciate ligament reconstruction with the ligament augmentation and reconstruction system: a systematic review. Int Orthop. 2013;37:321–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ng GY, Oakes BW, Deacon OW, McLean ID, Lampard D. Biomechanics of patellar tendon autograft for reconstruction of the anterior cruciate ligament in the goat: three-year study. J Orthop Res. 1995;13:602–608. [DOI] [PubMed] [Google Scholar]
- 42. Pan X, Wen H, Wang L, Ge T. Bone-patellar tendon-bone autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Eur J Orthop Surg Traumatol. 2013;23:819–823. [DOI] [PubMed] [Google Scholar]
- 43. Parchi PD, Gianluca C, Dolfi L, et al. Anterior cruciate ligament reconstruction with LARS™ artificial ligament results at a mean follow-up of eight years. Int Orthop. 2013;37:1567–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Paulos LE, Rosenberg TD, Grewe SR, Tearse DS, Beck CL. The GORE-TEX anterior cruciate ligament prosthesis: a long-term follow-up. Am J Sports Med. 1992;20:245–252. [DOI] [PubMed] [Google Scholar]
- 45. Petrou G, Chardouvelis C, Kouzoupis A, et al. Reconstruction of the anterior cruciate ligament using the polyester ABC ligament scaffold: a minimum follow-up of four years. J Bone Joint Surg Br. 2006;88-B:893–899. [DOI] [PubMed] [Google Scholar]
- 46. Roos EM, Roos HP, Lohmander L, Ekdahl C, Beynnon BD. Knee injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 47. Seemann MD, Steadman JR. Tibial osteolysis associated with Gore-Tex grafts. Am J Knee Surg. 1993;6:31–38. [Google Scholar]
- 48. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. [DOI] [PubMed] [Google Scholar]
- 49. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292–299. [DOI] [PubMed] [Google Scholar]
- 50. Schindler OS. Surgery for anterior cruciate ligament deficiency: a historical perspective. Knee Surg Sports Traumatol Arthrosc. 2012;20:5–47. [DOI] [PubMed] [Google Scholar]
- 51. Strover AE. The ABC ligament for chronic anterior cruciate ligament insufficiency In: Aichroth PM, Cannon WD, Jr, Patel DV, eds. Knee Surgery: Current Practice. London, England: Martin Dunitz; 1992:281–297. [Google Scholar]
- 52. Strover AE, Mowbray MAS, Shafighian B, O’ Brien T. Tissue ingrowth into a prosthetic knee ligament: the role of surgical technique. J Japan Orthop Assoc. 1988;62:588–598. [Google Scholar]
- 53. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 54. Tiefenboeck TM, Thurmaier E, Tiefenboeck MM, et al. Clinical and functional outcome after anterior cruciate ligament reconstruction using the LARS system at a minimum follow-up of 10 years. Knee. 2015;22:565–568. [DOI] [PubMed] [Google Scholar]
- 55. Trieb K, Blahovec H, Brand G, Sabeti M, Dominkus M, Kotz R. In vivo and in vitro cellular ingrowth into a new generation of artificial ligaments. Eur Surg Res. 2004;36:148–151. [DOI] [PubMed] [Google Scholar]
- 56. Webster KE, Feller JA, Leigh NB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641–647. [DOI] [PubMed] [Google Scholar]
- 57. Weitzel PP, Richmond JC, Altman GH, Calabro T, Kaplan DL. Future direction of the treatment of ACL ruptures. Orthop Clin North Am. 2002;33:653–661. [DOI] [PubMed] [Google Scholar]
- 58. Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler H. Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy. 2011;27:653–665. [DOI] [PubMed] [Google Scholar]
- 59. Wright RW, Huston LJ, Spindler KP, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38:1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ye JX, Shen GS, Zhou HB, et al. Arthroscopic reconstruction of the anterior cruciate ligament with the LARS artificial ligament: thirty-six to fifty-two months follow-up study. Eur Rev Med Pharmacol Sci. 2013;17:1438–1446. [PubMed] [Google Scholar]
- 61. Yu SB, Dong QR, Wang YB, Zuo ZN, Li DG, Histological characteristics and ultrastructure of polyethylene terephthalate LARS ligament following the reconstruction of anterior cruciate ligament in rabbits. Zhongguo Zuzhi Gongcheng Yanjiu Linchuang Kangfu. 2008;12:7061–7066. [Google Scholar]