Abstract
The use of dental implants for the rehabilitation of missing teeth has broadened the treatment options for patients and clinicians equally. As a result of advances in research in implant design, materials, and techniques, the use of dental implants has increased dramatically in the past two decades and is expected to expand further in the future. Success of dental implants depends largely on the quality and quantity of the available bone in the recipient site. This however may be compromised or unavailable due to tumor, trauma, periodontal disease, etc., which in turn necessitates the need for additional bone manipulation. This review outlines the various bone manipulation techniques that are used to achieve a predictable long-term success of dental implants.
Keywords: Bone expansion, bone grafts, guided bone regeneration, maxillary sinus lift
INTRODUCTION
The loss of tooth can be psychologically traumatizing. Attempts to replace teeth have been seen even in ancient civilizations. What makes implant dentistry unique is the ability to achieve this goal, regardless of the atrophy, disease, or injury of the stomatognathic system. To satisfy the ideal goals of the implant dentistry, the hard and soft tissues need to present ideal volumes and quality. If inadequate bone exists, several surgical techniques may be used to reconstruct the deficient ridge for implant placement.[1]
The bone manipulation techniques are capable of manipulating the one's bones to alter their density to make them extremely durable and strong. These techniques mobilize vital bone with plastic bending, shaping, or condensation of tissue as a bone flap or bone-periosteal flap.[2] These result in contour or dimensional changes, while preserving bone integrity and viability. The concept is to manipulate the residual bone to create an intrabony cavity with a wider base or taller roof that heals like an extraction site, with access of mesenchymal stem cells and the normal wound healing mechanisms. The morphology of bony defect is an important consideration in the selection of a method for ridge manipulation. The fewer the number of remaining bony walls, the greater is the need for osteopromotive techniques.[1]
Current bone manipulation techniques include inlay and onlay grafting, guided bone regeneration (GBR), bone expansion, bone splitting osteotomy, and different fixation devices such as bone screws, pins, titanium mesh, different augmentation materials, and different barrier membranes.[3]
PATTERN OF BONE LOSS
The alveolar bone loss is known to occur at a rapid rate during the 1st year after tooth extraction and may continue for years. Within the 1st year of the tooth loss, there is a 25% decrease in the width of the crestal bone and a 40% decrease in the bone width occurs within the first 1–3 year after tooth extraction, resulting in a labial plate of bone that is located lingual of its original location. Preservation or recontouring of the labial appearance of the alveolar process is one of the keys to optimal implant esthetics and long-term results.[4]
AVAILABLE BONE
A multidimensional assessment of the available bone is the most important factor necessary for a sound treatment planning ensuring longevity and function of implant supported prosthesis. Determinants of available bone are:
Height
Width
Length
Angle
Crown/implant ratio.
The minimum implant length (i.e., bone height) in an ideal bone density situation for predictable success is 10 mm. Allowing a margin of 2 mm from the vital landmarks such as inferior alveolar canal is recommended. Available width is defined as the distance between the buccal and the lingual plates, measured at the crest. Each 1 mm increase in diameter increases the surface area by about 20–30%, therefore, increasing diameter effectively; decreases crestal stress. Thus, implant diameter is much more critical than its length.[1]
RATIONALE FOR BONE MANIPULATION
Dental implants are the treatment of choice for the replacement of missing teeth nowadays. However, the placement of implants in the alveolar bone remains a challenge for most of the clinicians because of the resorption of the residual ridge resulting in the insufficient bone volume in one or more dimensions. Various surgical techniques to augment the thin ridges not only increases the morbidity but also results in the increase of expenditure involved as well as the time taken. All these factors act as determinants for the acceptance of the treatment plan by the patient. Need of the hour is to review the various bone manipulation techniques developed over the years and use a suitable conservative technique.
Bone is a biologically privileged tissue in that it has the capacity to undergo regeneration as a part of repair process.[5] Adequate bone volume prerequisites the implant therapy and proper esthetic result. Inadequate alveolar bone height and width often require bone manipulation procedures performed before, at the time of, or after the implant surgery. There are various techniques that had been described for the bone manipulation [Flow Chart 1].
Flow Chart 1.
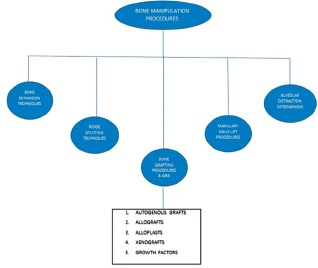
Bone manipulation procedures
SURGICAL PROCEDURES
Bone expansion technique
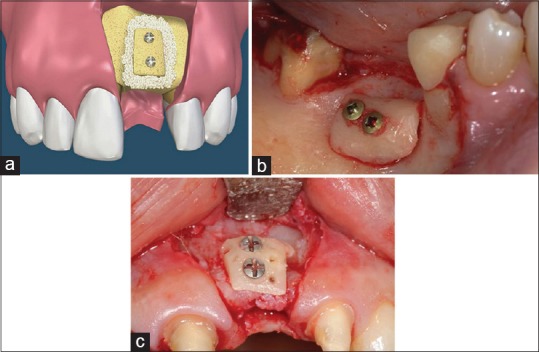
It is defined as the manipulation of the bone to form a receptor site for an implant without the removal of any bone from the patient.[6] The objective is to maintain the existing soft bone by pushing the buccal bony plates of the residual ridge laterally with minimal trauma. This technique takes the advantage of the softer bone quality found in Types III and IV maxillary bone by relocating the alveolar bone rather than losing the precious bone by drilling [Figure 1].[7]
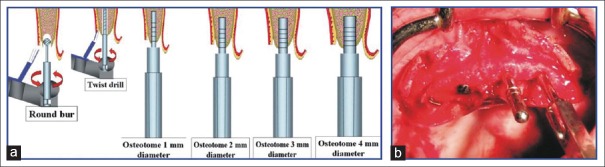
Figure 1.
(a) Schematic diagram of bone expansion technique. (b) Clinical case shows an osteotome and implants were placed using bone condensing technique
The most common anatomic area in which ridge expansion is performed is in the narrow anterior maxilla, followed by posterior maxilla and then the anterior and posterior mandible, respectively. Width of the residual alveolar crest should not be <4 mm to be able to insert the round osteotomes:
For reducing maxillary undercuts
For changing the emergence angulation
For expanding the buccal or labial bone esthetic reasons.
Bone expansion can be done by means of osteotomes.[8] Osteotomes are a special set of instruments developed to form or shape bone in preparation for the placement of dental implants. It increases the width for implant placement and allows immediate placement of implants in narrow ridges at the time of expansion. This technique also allows for greater tactile sensitivity.
In spite of so many advantages, osteotomes have certain disadvantages too. It is based on palm-held design that can be problematic to use in the posterior maxilla due to limited mouth opening. If the cortical plates of the bone are fused due to atrophy, the osteotome technique may not be effective.
Alveolar ridge splitting technique
This technique can be used to augment the atrophic maxilla and mandible before the implant placement. This method was introduced by Dr. Hilt Tatum in the 1970s and was commonly referred to as ridge splitting or bone spreading technique.[9] Gaining access to a ridge that is <3 mm wide requites splitting the buccal and palatal bone flaps with a scalpel first by separating two cortices through its cancellous bone. This technique is employed in cases where there is an insufficient width to utilize round osteotomes. This procedure provides a quicker method wherein an atrophic ridge can be predictably expanded and grafted with bone allografts, eliminating the need for a second donor site and a second stage surgery [Figure 2].
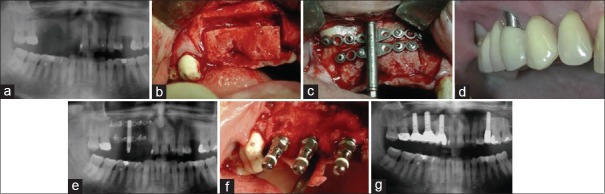
Figure 2.
(a) Schematic diagram of bone splitting technique. (b-d) Clinical procedure of bone splitting
Ideal sites demonstrate a knife-edge ridge that widens further apically, and that consists of adequate cortical thickness but with some degree of interpositional lamellar bone. The anterior region of the maxilla usually meets these demands, whereas mandibular sites usually do not. When there is adequate height of residual ridge, 8–10 mm of bone between the crest of the ridge and opposing landmark but inadequate buccolingual width, ridge splitting is an option. This technique enables problem-free widening from 2 to 5 mm.
Narrow edentulous alveolar ridges <4 mm wide can be expanded by the following means:
Single stage ridge-split procedure: In this procedure, entire edentulous bony segment is opened like an envelope to receive the implants. The pilot drills are used after the desired ridge widths have been reached and the implants inserted
Two stage ridge split technique: This is indicative when enough primary stability is not achieved. With this approach, the location of greenstick fracture is predetermined, and blood supply to the lateralized buccal segment remains intact.
The osteoperiosteal flap ridge-split procedure is performed for horizontal augmentation of narrow ridges that otherwise would not be suitable for implant placement. This technique consists of splitting the vestibular and the buccal cortical plate and further opening the space with osteotomes.[10]
This technique is advantageous as it does not require waiting period of 4–6 months for bone consolidation before the implant placement. In addition, it decreases the morbidity since it avoids a second surgical donor site for bone harvesting. However, this procedure can only increase the buccolingual bony dimension and is not applicable if there is sufficient bone height. Furthermore, implementing the technique on atrophic ridges <3 mm wide may result in unfavorable bone fractures that lead to bone resorption. Therefore, it is demonstrated that the ridge splitting technique is effective in longitudinal expansion of the alveolar ridges.
Bone grafting procedures and guided bone regeneration
Autogenous bone grafts
The gold standard of bone grafting materials is autografts. Autografts are obtained from the same patient, taken from one site and placed in another site and forms the bone by the process of osteogenesis and osteoinduction. Autograft materials are obtained intraorally from edentulous areas such as maxillary tuberosity, mandibular symphysis, and mandibular ramus. Extraoral autografts are obtained from iliac crest, rib, tibia, and calvarium. The advantages of autograft bone material are that it maintains bone structures such as minerals, collagen, and viable osteoblasts and bone morphogenic proteins (BMPs). The best success rates in bone grafting have been achieved with autografts because these are essentially living tissues with their cells intact [Figure 3].
Figure 3.
(a) Schematic diagram of onlay autogenous bone graft. (b) Small graft from chin donor site. (c) Bigger graft from iliac crest
It is osteoinductive/conductive, sterile, biocompatible/nonimmunogenic, easy to manipulate, and readily available from adjacent or remote sites. The microscopic architecture is perfectly matched. The main disadvantage of autografting is that it has to be harvested from a secondary (either intra- or extra-oral) site, which usually means more complicated surgery and higher morbidity.
Allografts
An allograft is a tissue graft between individuals of the same specimen but of nonidentical genetic composition. The source is usually cadaver bone, which is available in large amounts. This bone has to undergo many different treatment sequences to render it neutral to immune reactions and avoid cross contamination of host diseases. In practice, fresh allogenic bone is rarely used because of immune response and the risk of disease transmission. Human bone material in the form of freeze-dried bone or demineralized freeze-dried bone has been used widely in implant dentistry. A wide range of grafts is available, which may be particulate, thin sheets of cortical plate, or much larger bone blocks. Allografts have been used as an alternative but have little or no osteogenicity, increased immunogenic, and resorb more rapidly than autogenous bone. Allograft bone is a useful material in patients who require bone grafting of a nonunion type but have inadequate autograft bone. It is predominantly used as a scaffold for bone repair and is resorbable.
Alloplasts
Alloplastic bone grafts are synthetic materials that have developed to replace human bone to avoid transmitted diseases such as HIV, bovine spongiform encephalitis, or hepatitis. They are biocompatible and osteoconductive materials. The most common types of alloplasts used are calcium phosphates, bioactive glasses, and biocompatible composite polymers. Moreover, the main disadvantage of alloplasts is that they are unpredictable in allowing bone formation; therefore, particles can be uncounted within the grafted site.
Furthermore, the natural biocorals are calcium carbonate materials, with similar to the natural bone hydroxyapatite structure. Advanced synthetic bioactive resorbable bone graft materials having similar chemical and mechanical properties as the host bone, can provide the means to modify existing bone topography. Hydroxyapatite is available in a variety of forms. The most commonly used nonresorbable form becomes embedded in newly formed fibrous tissue and bone, and the resulting tissue combination is a less than ideal implant bed. The use of alloplastic grafting materials on their own is not routinely recommended. Hydroxyapatite and other bone substitutes require further clinical research and should not be used on their own as grafting material until their efficacy is evidence-supported.
Xenografts
Xenografts are graft materials derived from the inorganic portion of animal bones; the most common source is bovine, the removal of the organic component is processed to remove their antigenicity, whereas the remaining inorganic components provide a natural matrix as well as an excellent source of calcium. The disadvantage of xenografts is that they are only osteoconductive, and the resorption rate of bovine cortical bone is slow.
Currently, Bio-Oss® and Bio-Gide® are widely used as dental xenograft materials. Bio-Oss® is a xenograft consisting of deproteinized, sterilized bovine bone with 75–80% porosity and a crystal size of approximately 10 μm in the form of cortical granules; it has a natural, nonantigenic porous matrix and is chemically and physically identical to the mineral phase of human bone; it has been reported to be highly osteoconductive and to show a very low resorption rate. The organic material is completely removed to leave the mineralized bone architecture, which renders it nonimmunogenic and presumably safe from the possibility of infection. A more recent study demonstrated a favorable long-term tissue response to Bio-Oss® particles with mainly woven immature bone shown at 20 months, which was replaced with lamellar bone with time. Bio-Oss® is becoming increasingly popular for the use in bone grafting in implant dentistry and is often used in combination with Bio-Gide®. Bio-Gide® is a membrane made of collagen which facilitates planned soft tissue management during augmentation. Bio-Gide® is composed of highly purified natural collagen from pigs which has a natural bilayer design and has native collagen for soft tissue compatibility and forms a barrier for undisturbed bone regeneration. Studies have shown Bio-Gide® to allow successful bone regeneration in combination with Bio-Oss® and provide a barrier function lasting several months.
Guided bone regeneration
It is also known as “membrane protected bone regeneration.” The concept of GBR implies the use of cell-occlusive membranes for space provision over a vertical or horizontal defect, promoting the in-growth of osteogenic cells while preventing migration of undesired cells from the overlying soft tissue. It also effectively stabilizes the blood coagulum and thereby allows for faster healing to occur. This technique can be used before or at the same time as implant placement. Barrier membranes may be nonresorbable (e.g., expanded polytetrafluoroethylene) or resorbable.[11] Although nonresorbable has shown the most bone volume gain, they are associated with higher incidence of complications such as membrane exposure due to soft tissue dehiscence [Figure 4].
Figure 4.
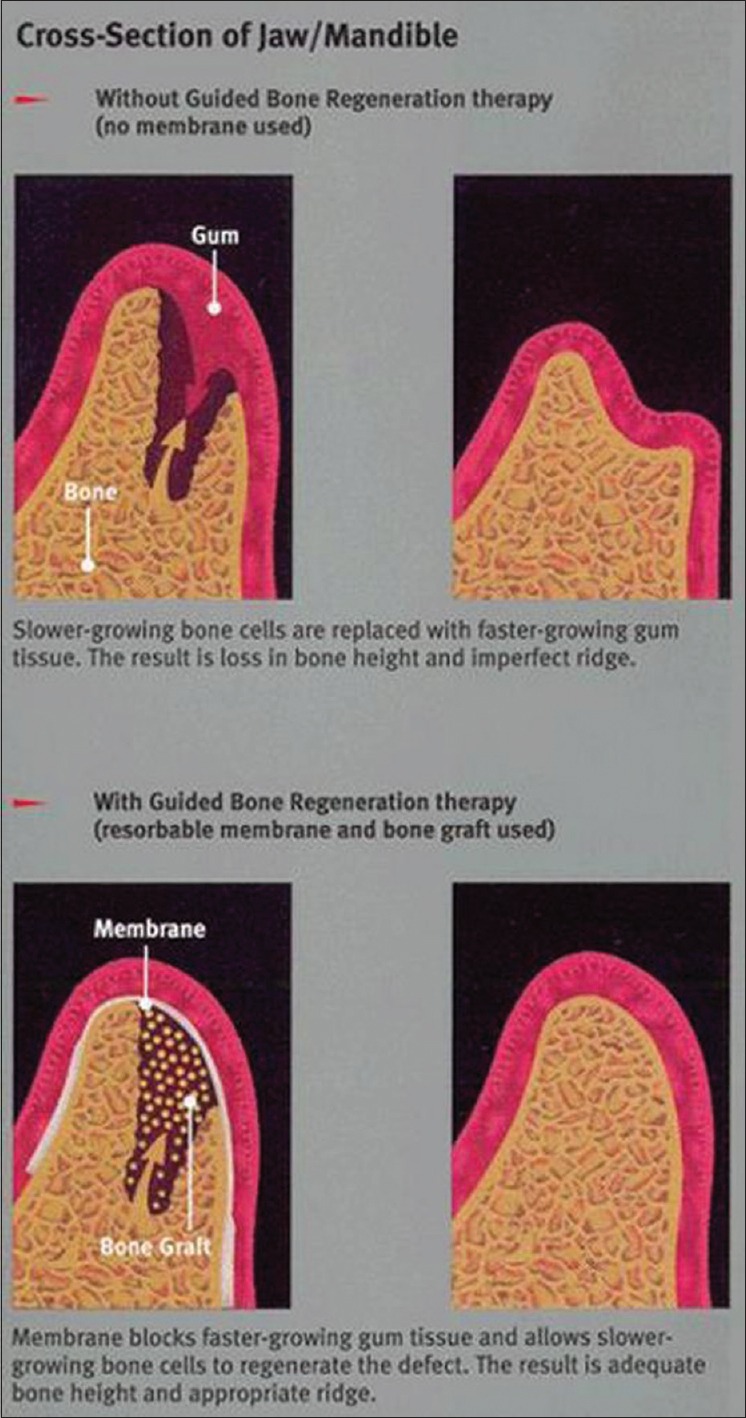
Guided bone regeneration
Growth factors
Various growth factors have widely been tested in animal models. Of these, bone BMPs require special mention as they induce osteogenic precursor cells into osteogenic cells and have shown tremendous bone growth in many animals and also human clinical studies.
Other growth factors besides BMPs that have been implicated during bone regeneration are also being investigated, including platelet-derived growth factor, transforming growth factor-β, insulin-like-growth factor-1, vascular endothelial growth factor, and fibroblast growth factor, among others.[12]
Maxillary sinus lift procedures
Currently, two main approaches to the maxillary sinus floor elevation procedure can be found in the literature. The first approach, lateral antrostomy, is the classic and the more commonly performed technique originally described by Tatum. This technique is often used as a preimplant procedure when residual alveolar ridge is inadequate to a point where initial implant stability is compromised. More recently, Summers advocated a second approach, the crestal approach, using osteotomes.[13] The crestal approach is considered to be a more conservative method for sinus floor elevation. In this technique, maxillary floor is fractured, the sinus membrane is elevated through an implant site with the use of osteotomes [Figure 5].
Figure 5.
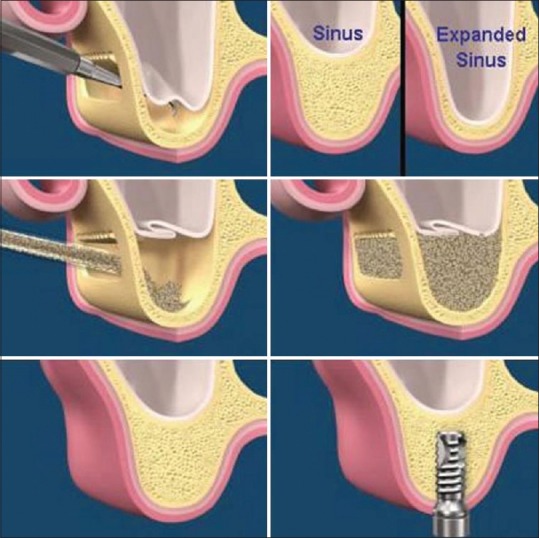
Direct sinus lift technique
The crestal technique has the advantage that it improves the density of the maxillary bone. It also has the potential for the use of less autogenous grafting material. The disadvantage of this approach is that the initial implant stability is unproven if the residual bone height is <6 mm. The chances of achieving a sufficiently high elevation with osteotome technique are limited. Other alternative techniques used nowadays in sinus lift procedures include the hydraulic pressure technique, endoscopically controlled technique called as subantroscopic laterobasal sinus floor augmentation, antral membrane balloon elevation technique, dentium advanced sinus kit technique, grind-out technique, and wall-off technique.[14]
Alveolar distraction osteogenesis
Distraction osteogenesis of the edentulous alveolar ridges may be considered an alternative to many other surgical techniques such as alloplastic graft augmentation, autogenous onlay bone grafting, and GBR. Alveolar distraction is now widely used for treating severe forms of alveolar ridge atrophy.[15] In this technique, a defect is created when two bone segments are slowly separated under tension. One week after osteotomy and distractor placement (latency period), distraction of segments is advanced at a rate of 0.5–1 mm/day until the desired separation is reached. A consolidation period of 5 days/mm of the space created should be maintained before device removal and implant placement. It allows for a vertical bone gain of 3–20 mm without the use of graft material, and additional mucosal grafting is not required as the soft tissue follows bone distraction [Figure 6].
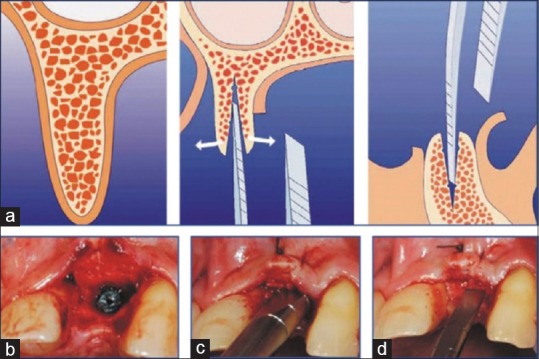
Figure 6.
Alveolar reconstruction using alveolar distraction in preparation for dental implants. (a) Right maxillary posttraumatic vertical defect. (b) Osteotomy. (c) Alveolar distractor in place. (d) Vector control using a prosthesis. (e) Panoramic radiograph after the end of the distraction. (f) Placement of dental implants. (g) Panoramic radiograph at the end of the treatment
Currently, vertical distraction osteogenesis of alveolar bone can be performed with three distraction systems:
Central application device (e.g., LEAD system)
Eccentric application of the device (e.g., TRACK distractor, Martin Gmbh, and Co., Germany)
Distraction by an implant (e.g., DIS-SYS distraction implant; Sis Inc., Klagenfurt, Austria).
One of the main problems in alveolar distraction is the accurate control of the direction. When the transport segment is relatively long (more than about 2 cm), it may be difficult to achieve controlled osteogenesis using only one distraction device. There is the possibility of tilting in the longitudinal axis of the distraction. In such cases, one solution is to use two distractors for each transport segment. Used singly, intraosseous distractors effectively control the movement of the transport segment in only one-dimension, which is the axis of distraction. The use of two distractors, one at each end of the segment, resolves this problem by ensuring that the segment stays parallel to the alveolar ridge.[16]
Other alternatives
Use of zygomatic implants
Zygomatic implants are a suitable alternative for the treatment of severe posterior maxillary atrophy. Three different surgical techniques exist for placing zygomatic implants: The sinus window technique (classic), the sinus slot technique, and the procedure for extrasinus zygomatic implants. The classic sinus window technique consists of exposing the frontolateral face of the zygomatic bone and creating a 10–3 5-mm window in the sinus to visualize the implant trajectory. The sinus slot technique improves visualization of the implant positioning, reduces sinus complications and postoperative symptoms, and allows a more buccal positioning of the implant head, thus facilitating prosthetic restoration. A new technique is currently being developed that involves placing extrasinus zygomatic implants by fixing them to the lateral sinus wall and the zygomatic bone. The authors observed higher primary stability than with the classic technique since the implant is fixed to a larger amount of cortical bone [Figure 7].[17]
Figure 7.
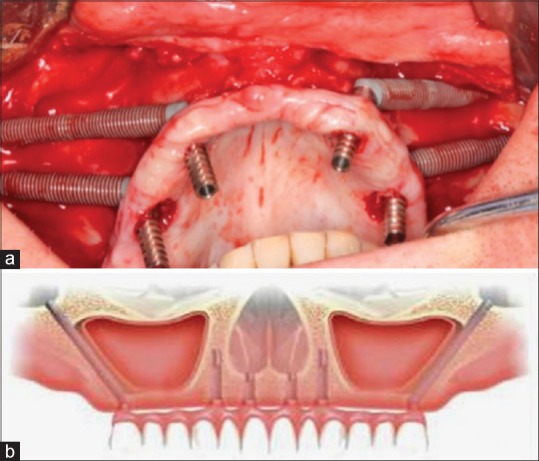
(a) Insertion with a low-speed motor of the zygomatic implant. The head of the implant is seen at the top of the zygoma. (b) Schematic diagram of zygomatic implants and additional four anterior implants in anterior maxilla
Use of tilted implants
The technique of tilting implants in the residual crestal bone of patients with maxillary atrophy allows placement of longer implants, thus increasing implant–bone contact area and implant primary stability; anchorage into the dense bone adjacent to the anterior sinus wall also contributes to increased stability. Posterior tilting of distal implants increases the distance between anterior and posterior implants, thus reducing the need for distal cantilevers; biomechanically, the distalization of the implant platform reduces the moments of force and improves the load distribution. Furthermore, tilted implants may suppress the need for bone grafting procedures in some cases, thus reducing biologic and economic costs and leading to higher patient acceptance.[18]
Use of basal implants
Basal implantology also known as bicortical implantology or cortical implantology is a modern implantology system which utilizes the basal cortical portion of the jaw bones for retention of the dental implants which are uniquely designed to be accommodated in the basal cortical bone areas. The basal bone provides excellent quality cortical bone for retention of these unique and highly advanced implants. The two types basal osseointegrated and basal cortical screw (BCS) basal implants are specifically designed to utilize strong cortical bone of the jaw. Screwable basal implants (BCS brand) have been developed with up to 12 mm thread diameter can be inserted into immediate extraction socket.[19]
Use of subperiosteal implants
The subperiosteal implant was conceived out of the need to improve the retention and stability of full dentures in severely atrophied ridges. Today, its use is still limited to the severely atrophied ridge of either the mandible or the maxilla. However, the implant is used less commonly in the maxilla because it has a lower success rate there; in addition, qualities of the maxilla allow for more retentive and stable prostheses. Lower success rates in the maxilla can be attributed to the poorer quality of bone. Subperiosteal implants are more successful in the basal bone – rich mandible than in the maxilla, which is primarily cancellous bone.[20]
DISCUSSION
Alveolar ridge modification is a prerequisite for both the implant and/or fixed prosthesis. It improves both the gingival and the bone architecture for esthetic and functional purposes. Peri-implant plastic surgery focuses on harmonizing peri-implant structures by means of hard tissue and soft tissue engineering. It includes bone structure enhancement, soft tissue enhancement, precision implant placement, and quality of prosthetic restoration.
A deform ridge may result from teeth extractions, severe periodontal disease, abscess formations, etc., the deformity that exits in the ridge is directly related to the volume of the root structure and associated bone that is missing or has been destroyed.[21] When managing the edentulous maxilla, the clinician is often faced with a large pneumatized maxillary sinus and a very thin alveolar ridge in the anterior maxilla. Alveolar bone resorption can be accelerated with denture use, resulting in loss of vertical height and very thin bone separating the crest of the ridge from the large sinus and the floor of the nose. These patients could be treated in a conventional fashion with augmentation of the sinuses only. When this is done, the patient can be restored with implant-supported dentures or a fixed-detachable prosthesis, but the lost vertical dimension must be replaced with acrylic. To improve the implant-to-tooth ratio, vertical augmentation is desired. If near ideal ridge height is obtained, the dentist and patient have several restorative options.
The severely atrophic mandible is also challenging to restore. Placement of implants in the severely atrophic mandible can result in fracture, thus reconstruction with bone grafting is usually indicated. With larger bone stock, implants can sometimes be placed posterior to the mental foramina, allowing for restorative options other than placement of implants in the anterior mandible only.
Bone grafts are widely used in the reconstruction of osseous defects in the oral and maxillofacial region. Autogenous bone grafts are generally obtained from the ilium, the rib, and the calvarium. These grafts can be easily obtained from these donor sites, but each site has associated morbidity. The maxilla and mandible are alternative sources of membranous bone and are thought to undergo less resorption than endochondral bone.
A variety of local bone grafts, such as mandibular symphysis, mandibular body, mandibular ramus, and coronoid process, have been used in the oral and maxillofacial reconstruction. Intraoral bone donor sites are excellent alternatives for the augmentation of edentulous alveolar defects before implantation.
GBR is a safe and effective technique for obtaining bone formation and placing dental implants in cases in which it would otherwise not be possible, even if an ideal membrane for treatment is not yet established. The technique of GBR, with nonresorbable membranes, is a very predictable technique and with excellent results, provided that you comply with the universally accepted surgical procedure, the surgeon should have extensive experience in handling, especially surgical soft tissue to cover the nonresorbable membrane, which is the key to success.[22]
The bony expansion using osteotomes is a reliable and relatively noninvasive way of widening narrow ridges. The expansion of atrophic ridges by the osteotome technique does not require harvesting of bone, reduces operating time and postoperative morbidity, shortens rehabilitation time, and eliminates the risk of exposure of the membrane or bone graft that could lead to infection. In the same manner, ridge splitting technique is used to expand the edentulous ridge for implantation or insertion of interpositional bone graft. This technique is only suitable for enhancing ridge width. There must be adequate available bone height for implant placement, and no vertical bone defect should be present.[23]
Alveolar distraction is a technique in constant evolution. A review of the literature within the past 14 years reveal that there are clear indications for its use, with outcomes similar to and sometimes even more predictable than traditional bone grafting techniques in preparation for implant placement. Although complications exist with alveolar distraction, it seems that most are minor and easy to manage. Appropriate patient selection and a better understanding of the technique are paramount in successful bone regeneration with alveolar distraction osteogenesis.
Therefore, the success of the bone manipulation procedures relies on maintaining the integrity of the labial wail, which occurs as long as the periosteum remains intact. Since 80% of the blood supply is from the periosteum, we feel the high degree of the success in expanding very thin ridges is due to our ability to manipulate the thin cortical bone without disrupting the periosteal attachment to this bone.
CONCLUSION
On the basis of available data, it is difficult or impossible to determine that one surgical procedure offers a better outcome than another, as far as predictability of the augmentation and survival/success rates of implants placed in the augmented sites are concerned. Every surgical procedure presents advantages and disadvantages, which must be carefully evaluated before surgery. Moreover, it is not yet known if some surgical procedures that are widely used in clinical practice, such as sinus grafting procedures in the case of limited/moderate sinus pneumatization or reconstruction of atrophic edentulous mandibles with onlay autogenous bone grafts, are really useful for improving the long-term survival of implants.
The predictable outcome of these procedures depends on several biologic principles that must be followed. Diagnosis, treatment planning, careful execution of the surgical treatment, postoperative follow-up, and appropriate implant loading are all important factors in achieving success.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Misch CE. Contemporary Implant Dentistry. 2nd ed. Mosby; 1993. [Google Scholar]
- 2.Cullum D. Advances in bone manipulation: Part 2. Osteomobilization for horizontal and vertical implant site development. SORMS. 2010;18.5:1–44. [Google Scholar]
- 3.Simion M, Baldoni M, Zaffe D. Jawbone enlargement using immediate implant placement associated with a split-crest technique and guided tissue regeneration. Int J Periodontics Restorative Dent. 1992;12:462–73. [PubMed] [Google Scholar]
- 4.Goyal S, Iyer S. Bone manipulation techniques. Int J Clin Implant Dent. 2009;1:22–31. [Google Scholar]
- 5.Basa S, Varol A, Turker N. Alternative bone expansion technique for immediate placement of implants in the edentulous posterior mandibular ridge: A clinical report. Int J Oral Maxillofac Implants. 2004;19:554–8. [PubMed] [Google Scholar]
- 6.Borgner RA, Kirkos LT, Gougaloff R, Cullen MT, Delk PL. Computerized tomography scan interpretation of a bone expansion technique. J Oral Implantol. 1999;25:102–8. doi: 10.1563/1548-1336(1999)025<0102:CTSIOA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Siddiqui AA, Sosovicka M. Lateral bone condensing and expansion for placement of endosseous dental implants: A new technique. J Oral Implantol. 2006;32:87–94. doi: 10.1563/786.1. [DOI] [PubMed] [Google Scholar]
- 8.Hahn J. Clinical uses of osteotomes. J Oral Implantol. 1999;25:23–9. doi: 10.1563/1548-1336(1999)025<0023:CUOO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Demetriades N, Park JI, Laskarides C. Alternative bone expansion technique for implant placement in atrophic edentulous maxilla and mandible. J Oral Implantol. 2011;37:463–71. doi: 10.1563/AAID-JOI-D-10-00028. [DOI] [PubMed] [Google Scholar]
- 10.Jensen OT, Bell W, Cottam J. Osteoperiosteal flaps and local osteotomies for alveolar reconstruction. Oral Maxillofac Surg Clin North Am. 2010;22:331–46, vi. doi: 10.1016/j.coms.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez R, Hartmann N, Weingart D. Current concepts of bone regeneration in implant dentistry. J Surg. 2015;10:283–5. [Google Scholar]
- 12.Dimitriou R, Tsiridis E, Giannoudis PV. Current concepts of molecular aspects of bone healing. Injury. 2005;36:1392–404. doi: 10.1016/j.injury.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Woo I, Le BT. Maxillary sinus floor elevation: Review of anatomy and two techniques. Implant Dent. 2004;13:28–32. doi: 10.1097/01.id.0000116369.66716.12. [DOI] [PubMed] [Google Scholar]
- 14.Ali SA, Karthigeyan S, Deivanai M, Kumar A. Implant rehabilitation for atrophic maxilla: A review. J Indian Prosthodont Soc. 2014;14:196–207. doi: 10.1007/s13191-014-0360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaggl A, Schultes G, Karcher H. Vertical alveolar ridge distraction with prosthetic treatment. A clinical investigation. Int J Oral Maxillofac Implants. 2000;15:701–10. [PubMed] [Google Scholar]
- 16.Yalcin S, Ordulu M, Emes Y, Gur H, Aktas I, Caniklioglu C. Alveolar distraction osteogenesis before placement of dental implants. Implant Dent. 2006;15:48–52. doi: 10.1097/01.id.0000202422.36990.6d. [DOI] [PubMed] [Google Scholar]
- 17.Candel-Martí E, Carrillo-García C, Peñarrocha-Oltra D, Peñarrocha-Diago M. Rehabilitation of atrophic posterior maxilla with zygomatic implants: Review. J Oral Implantol. 2012;38:653–7. doi: 10.1563/AAID-JOI-D-10-00126. [DOI] [PubMed] [Google Scholar]
- 18.Oltra DP, Marti EC. Rehabilitation of posterior maxilla with tilted implants: A review of literature. J Oral Implantol. 2013;2:39–43. doi: 10.1563/AAID-JOI-D-11-00068. [DOI] [PubMed] [Google Scholar]
- 19.Yadav RS, Sangur R, Mahajan T. An alternative to conventional dental implants: Basal implants. Rama Univ J Dent Sci. 2015;2:22–8. [Google Scholar]
- 20.Demirdjan E. The complete maxillary subperiosteal implant: An overview of its evolution. J Oral Implantol. 1998;24:196–7. doi: 10.1563/1548-1336(1998)24<196:TCMSIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Prasad DK, Mehta D. Osseointegrated support prosthesis – Surgical techniques for hard and soft tissue grafting. J Dent Implants. 2014;4:72–7. [Google Scholar]
- 22.El Haddad E, Lauritano D, Candotto V, Carinci F. Guided bone regeneration is a reliable technique in implant dentistry: An overview and a case report. OA Dentistry. 2014;2:5. [Google Scholar]
- 23.Khoshhal M. Mandibular ridge splitting and gradual bone expansion technique for immediate placement of implant in posterior thin region. Avic J Dent Res. 2013;5:e19463. [Google Scholar]