Abstract
Aim:
Self-medication is widely practiced with varying dimensions in India. This practice has many implications, especially among medical and paramedical students having some knowledge and good exposure to drugs. We conducted a two-period observational study to evaluate the change in knowledge and practice of self-medication, over 5 years of time period, among medical and paramedical students from different parts of India.
Materials and Methods:
A structured questionnaire was administered to medical (MBBS), dental (BDS), and paramedical students, who come to attend pan India annual cultural, literary, and sports event at New Delhi. The study was conducted in two phases (2007 and 2012) in different respondents of same categories (medical and paramedical) of students. Three-hundred and thirty students from 39 colleges in 2007 and 356 students from 38 colleges in 2012 participated in the study.
Results:
The prevalence of self-medication remained high in both 2007 and 2012 (74.6% and 69.4%), although no significant difference was observed between the two phases (P = 0.14%). Oral antibacterial agents, oral anti-inflammatory agents, and antipyretics were the most common group of drugs used in both phases of study. A significant increase was observed in number of students who took complete course of oral antibiotics (28.3-38.3%, P = 0.01).
Conclusion:
The prevalence of self-medication among undergraduate students remains unaltered over the span of 5 years. Nevertheless, there was a better sensitization toward appropriate antibiotic usage and the practice of responsible self-medication needs to be promoted among future healthcare providers.
Key words: Antibiotic use, cross-sectional study, medical students, paramedical students, self-care, self-medication
INTRODUCTION
World Health Organization defines self-medication as the use of medicines by individuals to treat self-recognized illnesses or symptoms.[1] It is a form of self-care and “responsible self-medication” facilitates rapid and inexpensive access to treatment, reduces the burden on health care infrastructure, thus playing an important role in a developing country like India, which has limited and uneven distribution of healthcare professionals.[2] Worldwide, over the counter drugs or “nonprescription drugs” are used in the practice of responsible self-medication, and are generally considered to be safe and effective. However, a pitfall in this practice of responsible self-medication, especially in India is that prescription drugs are also commonly dispensed without valid prescriptions.[3] Such practice poses many medical and social challenges with widespread implications.[4] Wrong self-diagnosis leading to delayed treatment, unnecessary out of pocket expenditure, adverse drug reactions due to incorrect dosage, drug-drug interactions, incorrect route of administration, and drug dependence are some of the well-recognized drawbacks of self-medication.[5]
It has been observed that medical and paramedical students are commonly involved in the practice of self-medication, without complete knowledge about the therapy they are taking.[6] Although there are many studies estimating the prevalence of self-medication worldwide, very few studies have been conducted in India to study the practice of self-medication among medical students. Most of these cross-sectional Indian studies have been conducted among MBBS students at a single institution.[7,8,9,10,11,12] Since knowledge of medical science evolves as students advance in their course, we attempted to evaluate the change in the practice of self-medication, without any active intervention, in two completely different batches of students with a time gap of 5 years through a two-period, cross-sectional, questionnaire-based study in an assembly of medical and paramedical students from different medical colleges of India.
MATERIALS AND METHODS
We carried a two-period questionnaire based cross sectional study being in 2007 and 2012. The respondents were medical students (MBBS) and dental (BDS), and paramedical students (B.Sc. Nursing, B.Sc. Optometry, and B.Sc. Medical Technology in Radiography), who came to participate in an all-India annual cultural, literary, and sports event organized at the All India Institute of Medical Sciences, New Delhi. Only up to 20 students from one college were enrolled to ensure heterogeneity of the study population. The MBBS and BDS students prior to starting their internship (not passed the final year exam) and paramedical students, who were willing to voluntarily participate, were enrolled in the study. Randomly selected consenting participants were asked to fill a three-page 23 items self-structured questionnaire. The items of the questionnaire had been previously generated, reviewed, and prevalidated by a panel of senior faculty members. It was administered to five students of each category, studying in our institution and pilot tested and suitable modifications were carried out before finalizing it for our study. The questionnaire included items to capture information about demography, prevalence, practice, and knowledge related to self-medication. The participants were given sufficient time to fill this questionnaire by striking out the most appropriate option against each item.
The respondents were different during both the surveys (2007 and 2012), but categories (medical and paramedical) remained the same. Self-medication was defined as the use of medicinal products (allopathic or traditional) for treatment or prevention of self-diagnosed medical disorders without a valid prescription from medical practitioner during past 1 year. This study was conducted among students who come to attend an annual cultural event organized at our institute and did not involve any intervention or elicited anything that was confidential or private in nature. It was conducted in accordance with the Declaration of Helsinki.
Data were analyzed using Statistical Package for the Social Sciences (SPSS, Chicago, IL, USA) version 15 for windows. For quantitative data, Chi-square test/Fisher's exact test and for continuous data, Student's t-test was applied, wherever applicable. Besides this, the comparison between the 2 times period in the same group was done by applying paired t-test/Wilcoxon signed-rank separately in each group, wherever necessary. The outcomes were expressed as mean ± standard deviation or in %. A P < 0.05 (2-tailed) was considered as statistically significant.
RESULTS
This study was conducted in two phases. In first phase in 2007, a total of 330 students from 39 colleges participated in the study; whereas in 2012, 356 students from 38 colleges participated in the study. Three questionnaire in 2007 and 19 in 2012 were found to be incomplete and excluded from the final analysis. Hence, a total of 327 students in 2007 and 337 students in 2012 were included in study analysis. The study population in 2012 (19.90 ± 1.28 years) was statistically significant younger than in 2007 (20.27 ± 1.67 years) [Table 1]. A statistically nonsignific0ant decrease was observed in the prevalence of self-medication which was found out to be 74.6% (244 out of 327) in 2007 and 69.4% (234 out of 337) in 2012 [Table 1]. The proportion of students who were involved in this practice was found to be highest in the 3rd year of their professional studies in both the phases [Table 2] and was not influenced by the medical profession of their parents. There seems to be no gender predominance but statistically significant differences were observed in the category of the students (medical and paramedical) in which self-medication was observed in two phases of the study (P < 0.001) [Table 3].
Table 1.
Profile of students enrolled in the study

Table 2.
Distribution of students participating in this study according to their year of medical studies
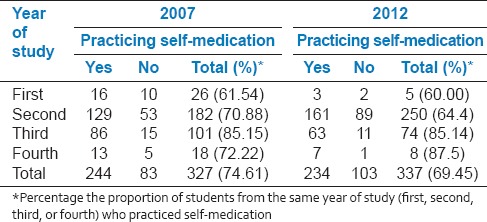
Table 3.
Students practicing self-medication
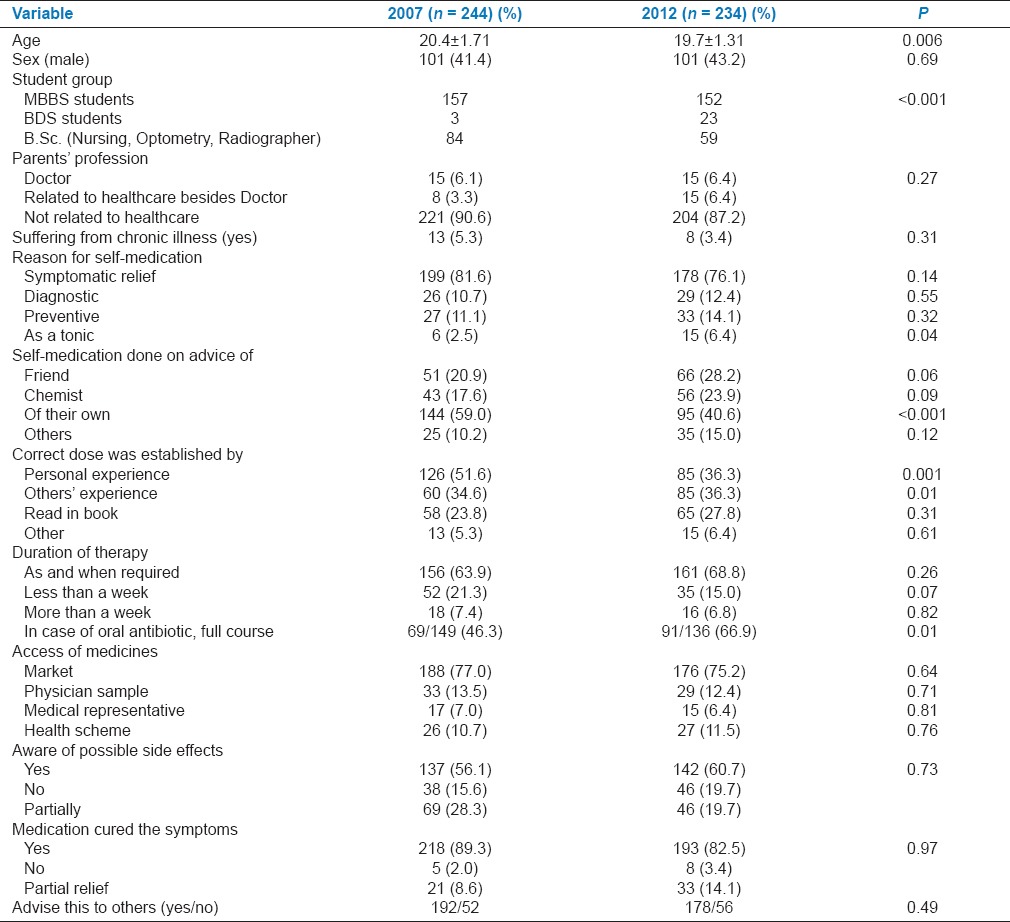
There was no statistical difference in reasons for self-medication during both phases of the study, with symptomatic relief as the foremost reason for this practice, other being for preventive, diagnostic purpose, or as a tonic for general well-being [Table 3]. It is noteworthy that in 2012, significantly lesser number of students practiced self-medication of their own than in 2007. In addition, the number of students who relied more on personal experience rather than other sources of information (including other's experience, books, etc.,) to establish the correct dose were significantly less in 2012 than in 2007 (P = 0.001). However, in both the periods, books and literature were not considered as the primary sources for establishing the correct dose of medication. Interestingly, majority of students claimed that they were aware of the possible side effects in the both phases of the study (56.1% in 2007 and 60.7% in 2012). There was no change between 2007 and 2012 with respect to the use of different system of medicines with most taking medicines from allopathic system and very few using alternative systems viz. Ayurvedic, Homeopathy, or Unani.
Among the 19 group of medications asked in the questionnaire, oral antibacterial agents (antibiotics), oral anti-inflammatory agents, and antipyretics were the common groups of drugs being used for self-medication in both 2007 and 2012 [Figure 1]. Importantly, significant increase was observed from 2007 to 2012 (46.3-66.9%, P = 0.001) in the number of students who took complete course of oral antibiotics, rather than leaving the therapy incomplete after symptomatic relief [Table 3]. In both the time periods, almost three-fourth of students accessed the drugs for self-medication directly from chemist shops in the market. Majority of the students also reported symptomatic relief with use of the medicine and would also advise the use of these medicines to others.
Figure 1.
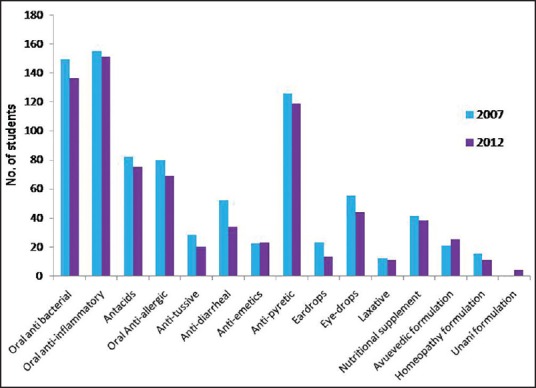
Drugs used for self-medication
DISCUSSION
In this study, the prevalence rate of self-medication among medical and paramedical students remain high in both the phases and was found to be 74.6% in 2007 and 69.4% in 2012, indicating a small but statistically nonsignificant change in trend over the 2 time points. This was probably due to increased awareness and better drug regulations (such as ban on certain fixed dose combinations, ban on misleading TV commercials of drugs, etc.,) during this time span. The overall prevalence rates of this practice, found in both the phases, were in accordance with the other studies on the prevalence of self-medication (57.1-92.0%) among medical students in India.[8,9,10,11,12] However, previous Indian studies included only MBBS students from only one center at one point of time. It is noteworthy that in our study, both medical and paramedical students from all over India were included to capture a comprehensive picture of this practice. In a study conducted in Medical School in the United Kingdom among medical students, it was reported that 39.2% feel that it is appropriate for doctors to self-prescribe.[13] Similarly, in studies done in USA, 22% of medical students reported using informal care[14] and 52% of resident doctors were engaged in the practice of self-medication.[15] In Norway, 54% of the physicians in their fourth and ninth postgraduate years had reported the use of self-prescription in case of illness.[16] A comprehensive study conducted among medical, pharmacy, and health science students of single medical college in Ethiopia found the prevalence of this practice to be 38.5%.[17] Similarly, prevalence among medical students was reported to be 55% from Egypt,[18] 76.6% in Iran,[19] and 44.8% in Bahrain.[20] Hence, it can be inferred that all over the world self-medication is practiced by medical students, in varying degree. However, the frequency varies from Western world to India, which could be due to easy availability of prescription drugs from pharmacies in India.[3] There is also another larger dimension of prescription drugs being abused by students for self-medication. A study by Benotsch et al. found out the lifetime misuse of an over-the-counter medication to be 13.0-18.6% among young adults (age 18-25 years) and this misuse is significantly linked to increased use of illicit substances for abuse purposes.[21] Recently, a study established that self-medication is the chief reason for misuse of prescription medication among physicians.[22]
In our study, this practice of self-medication was not influenced by gender or profession of parents. This is in contrast to previously reported studies from India, which reported higher female predilection for self-prescription among medical students.[8,9,10] In addition, a study from the USA concluded that females are at increased risk of prescription drug misuse, due to greater amount of strain in daily lives as compared to their male counterparts.[23] However, another Indian study had also reported higher self-medication practice among male participants.[24] There was a statistically significant difference between the different category of students who participated in this study and who practiced self-medication between 2007 and 2012. This was possibly owing to a sampling error with more number of BDS students and less of B.Sc. (Nursing) being administered the questionnaire in 2012 as compared to 2007. This difference disappeared when self-medication practice was analyzed only for MBBS students between 2007 and 2012. However, in both the phases, the proportion of students practicing self-medication was maximum during the 3rd year of their studies probably because the pharmacology curriculum is completed during the 3rd year of study.
Majority of students in both the phases (76.1% in 2012 vs. 81.6% in 2007) took the medications for symptomatic relief and stopped them as soon as symptoms are relieved. However, less number of students took the medicines and decided the correct dosage of their own and relied more on the advice or experience of friends, chemists or others in 2012 as compared to 2007. This is possible because, in the second phase, more number of participants were still in their 2nd year compared to the first phase (i.e., 250/337 in 2012 vs. 182/327 in 2007). Importantly, in both the phases of the study, around half of students were either not aware or partially aware of the adverse effects of the drugs they used for self-medication. This demonstrates the callousness on part of students toward their own health and also raises serious concerns regarding the quality of medical care which they are supposed to provide in future to patients.
Oral anti-inflammatory, oral antibiotics, and oral antipyretics are the major classes of drugs being used for self-medication in both phases of this study. This finding is consistent with previous studies from other parts of the world;[17,18,19] however, earlier studies from India have mentioned antipyretics as the most commonly used drug group for self-medication.[9,10] Majority of the students in both the phases (63.9% in 2007 and 68.8% in 2012) took medicines as long as the symptoms persisted and stopped them after having symptomatic cure. However, an important change was observed in the practice of taking antibiotics between two phases of the study. Although there was no significant difference in the proportion of students who took antibiotics in both the phases (58.1% in 2012 vs. 61.1% in 2007), a significant increase in the number of students who took the full course of antibiotics irrespective of symptomatic cure in was observed in 2012. The proportion of students who took oral antibiotics in this study is quite high as compared to previously reported studies from India (i.e., 31.1-39.3%)[8,9,10] and abroad (i.e., 30.0-58.8%).[18,25,26] The media coverage of emergence of New Delhi Metallo beta-lactamase-1 enzyme bearing bacteria, which are resistant to most of the known antibiotics; and its relation to India might have created awareness among medical students regarding proper use of antibiotics.[4] In both the phases of this study, most of the students who self-prescribed got symptomatic relief and further emphasized that they will recommend this practice to others, which itself is a worrying trend. Such practice will be further compounded by the fact that in India, antibiotics are prescribed without appropriate indications and patients often do not complete the full course of the drugs.[27,28] However, on the brighter side, a shift toward rational self-prescribing was evident from the antibiotic taking patterns of the students in the second phase of the study.
Limitations of the study
Although this is the first Indian study which provides a comprehensive picture of self-medication practice among future healthcare providers (medical and paramedical students) from across the country (39 colleges in 2007 and 38 colleges in 2012), there are certain limitations. First, although a recall period of 1 year was chosen to include the impact of cyclic and chronic ailments, there is a possibility of recall bias, especially for the frequency of self-medication within past 1 year at the time of participation in the study which may lead to wrong assumptions. Second, the categories of participants (medical and paramedical) despite being the same, the actual participants were different during both phases of the study. This was done purposefully to evaluate the behavior of same category of different students at separate time points. Third, most of the participants represented colleges from the North, West, and East Regions of the country because participation from the southern colleges in the annual cultural event organized at our institute in North India is traditionally low.
CONCLUSION
The practice of irresponsible self-medication by medical students can have serious implications as they are the future healthcare providers. The students are impressionable at this stage of their career, and they carry forward those practices which they acquire during this period. Our finding of students preferring to complete the full course of antibiotics in 2012 in contrast to 2007 is testimony that awareness of rational antibiotic use can positively influence their practices. A separate module on pros and cons of self-medication and drug-induced injury should also be included in the undergraduate medical curriculum. After completion of medical school, the significance of ‘responsible self-medication’ should be conveyed to physicians by organizing seminars, continuing medical education, and webinars. Along with this, support by the government in curbing the easy availability of medications across the pharmacies in the country can also reduce self-medication practices substantially.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr Guresh Kumar, Department of Biostatistics, All India Institute of Medical Sciences, New Delhi, for assistance in the analysis of study data.
REFERENCES
- 1.The Role of the Pharmacist in Self-Care and Self-Medication. Essential Medicines and Health Products Information Portal. World Health Organization Resource. 1998. [Last accessed on 2016 Jan 15]. Available from: http://apps.who.int/medicinedocs/en/d/Jwhozip32e/3.2.html .
- 2.Pallikadavath S, Singh A, Ogollah R, Dean T, Stones W. Human resource inequalities at the base of India's public health care system. Health Place. 2013;23:26–32. doi: 10.1016/j.healthplace.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Walia JK. Over the Counter Sale of Drugs – How to Curb this Practice? India Medical Times. 2012. [Last accessed on 2015 Sep 19]. Available from: http://www.indiamedicaltimes.com/2012/11/13/over-the-counter-sale-of-drugshow-to-curb-this-practice/
- 4.Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: A molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10:597–602. doi: 10.1016/S1473-3099(10)70143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruiz ME. Risks of self-medication practices. Curr Drug Saf. 2010;5:315–23. doi: 10.2174/157488610792245966. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery AJ, Bradley C, Rochfort A, Panagopoulou E. A review of self-medication in physicians and medical students. Occup Med (Lond) 2011;61:490–7. doi: 10.1093/occmed/kqr098. [DOI] [PubMed] [Google Scholar]
- 7.Talevi A. The new patient and responsible self-medication practices: A critical review. Curr Drug Saf. 2010;5:342–53. doi: 10.2174/157488610792245984. [DOI] [PubMed] [Google Scholar]
- 8.Banerjee I, Bhadury T. Self-medication practice among undergraduate medical students in a tertiary care medical college, West Bengal. J Postgrad Med. 2012;58:127–31. doi: 10.4103/0022-3859.97175. [DOI] [PubMed] [Google Scholar]
- 9.Kumar N, Kanchan T, Unnikrishnan B, Rekha T, Mithra P, Kulkarni V, et al. Perceptions and practices of self-medication among medical students in coastal South India. PLoS One. 2013;8:e72247. doi: 10.1371/journal.pone.0072247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badiger S, Kundapur R, Jain A, Kumar A, Pattanshetty S, Thakolkaran N, et al. Self-medication patterns among medical students in South India. Australas Med J. 2012;5:217–20. doi: 10.4066/AMJ.2012.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patil SB, S H V, B V P, Santoshkumar J, Binjawadgi AS, Kanaki AR. Self-medication practice and perceptions among undergraduate medical students: A cross-sectional study. J Clin Diagn Res. 2014;8:HC20–3. doi: 10.7860/JCDR/2014/10579.5313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biswas SS, Adikari A, Ray M, Kundu P. A KAP study on graduate nursing students of a tertiary health care teaching hospital in rural West Bengal, India. Nepal Med Coll J. 2013;15:14–7. [PubMed] [Google Scholar]
- 13.Hooper C, Meakin R, Jones M. Where students go when they are ill: How medical students access health care. Med Educ. 2005;39:588–93. doi: 10.1111/j.1365-2929.2005.02175.x. [DOI] [PubMed] [Google Scholar]
- 14.Roberts LW, Hardee JT, Franchini G, Stidley CA, Siegler M. Medical students as patients: A pilot study of their health care needs, practices, and concerns. Acad Med. 1996;71:1225–32. doi: 10.1097/00001888-199611000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Christie JD, Rosen IM, Bellini LM, Inglesby TV, Lindsay J, Alper A, et al. Prescription drug use and self-prescription among resident physicians. JAMA. 1998;280:1253–5. doi: 10.1001/jama.280.14.1253. [DOI] [PubMed] [Google Scholar]
- 16.Hem E, Stokke G, Tyssen R, Grønvold NT, Vaglum P, Ekeberg Ø. Self-prescribing among young Norwegian doctors: A nine-year follow-up study of a nationwide sample. BMC Med. 2005;3:16. doi: 10.1186/1741-7015-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abay SM, Amelo W. Assessment of self-medication practices among medical, pharmacy, and health science students in Gondar University, Ethiopia. J Young Pharm. 2010;2:306–10. doi: 10.4103/0975-1483.66798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El Ezz NF, Ez-Elarab HS. Knowledge, attitude and practice of medical students towards self medication at Ain Shams University, Egypt. J Prev Med Hyg. 2011;52:196–200. [PubMed] [Google Scholar]
- 19.Sarahroodi S, Maleki-Jamshid A, Sawalha AF, Mikaili P, Safaeian L. Pattern of self-medication with analgesics among Iranian University students in central Iran. J Family Community Med. 2012;19:125–9. doi: 10.4103/2230-8229.98302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Princ Pract. 2006;15:270–5. doi: 10.1159/000092989. [DOI] [PubMed] [Google Scholar]
- 21.Benotsch EG, Koester S, Martin AM, Cejka A, Luckman D, Jeffers AJ. Intentional misuse of over-the-counter medications, mental health, and polysubstance use in young adults. J Community Health. 2014;39:688–95. doi: 10.1007/s10900-013-9811-9. [DOI] [PubMed] [Google Scholar]
- 22.Merlo LJ, Singhakant S, Cummings SM, Cottler LB. Reasons for misuse of prescription medication among physicians undergoing monitoring by a physician health program. J Addict Med. 2013;7:349–53. doi: 10.1097/ADM.0b013e31829da074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ford JA, Reckdenwald A, Marquardt B. Prescription drug misuse and gender. Subst Use Misuse. 2014;49:842–51. doi: 10.3109/10826084.2014.880723. [DOI] [PubMed] [Google Scholar]
- 24.Selvaraj K, Kumar SG, Ramalingam A. Prevalence of self-medication practices and its associated factors in Urban Puducherry, India. Perspect Clin Res. 2014;5:32–6. doi: 10.4103/2229-3485.124569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pan H, Cui B, Zhang D, Farrar J, Law F, Ba-Thein W. Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among university students in Southern China. PLoS One. 2012;7:e41314. doi: 10.1371/journal.pone.0041314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Donkor ES, Tetteh-Quarcoo PB, Nartey P, Agyeman IO. Self-medication practices with antibiotics among tertiary level students in Accra, Ghana: A cross-sectional study. Int J Environ Res Public Health. 2012;9:3519–29. doi: 10.3390/ijerph9103519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khan FA, Singh VK, Sharma S, Singh P. A prospective study on the antimicrobial usage in the medicine department of a tertiary care teaching hospital. J Clin Diagn Res. 2013;7:1343–6. doi: 10.7860/JCDR/2013/6265.3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharma M, Eriksson B, Marrone G, Dhaneria S, Lundborg CS. Antibiotic prescribing in two private sector hospitals; one teaching and one non-teaching: A cross-sectional study in Ujjain, India. BMC Infect Dis. 2012;12:155. doi: 10.1186/1471-2334-12-155. [DOI] [PMC free article] [PubMed] [Google Scholar]


