Abstract
Background:
Currently, the most common therapy for periodontal diseases consists of professional scaling and root planing (SRP). However, it was found to be of limited efficacy especially in areas which are inaccessible to periodontal instrumentation. Therefore, treatment strategies using antimicrobials in conjunction with conventional therapy have evolved. Thus, the study was undertaken with an.
Aim:
To evaluate the efficacy of application of chlorhexidine gel and curcumin gel as an adjunct to SRP.
Materials and Methods:
The study was conducted on thirty chronic periodontitis patients who were divided into two groups as control and experimental groups using a split-mouth design. After SRP chlorhexidine gel was applied in control and curcumin gel in experimental groups. The plaque index, gingival index, sulcus bleeding index, probing pocket depth were recorded at baseline and subsequently after 1 month and 45 days.
Results:
The results revealed that both chlorhexidine gel and curcumin gel have an effect on mild to moderate periodontal pockets in chronic periodontitis patients, but greater reduction was observed in the experimental group than the control group.
Conclusion:
It can be concluded that both control and experimental gel can be used as an adjunct to SRP, but the curcumin gel was more effective than the chlorhexidine gel in the treatment of mild to moderate periodontal pockets with a significant reduction in the indice scores when compared to the baseline values.
Key words: Chlorhexidine gel, chronic periodontitis, curcumin gel, local drug delivery
INTRODUCTION
Periodontitis describes a group of related diseases resulting in the destruction of the tissues that support the tooth. The most common destructive disease of the periodontal attachment apparatus is initiated by oral microflora.[1]
Scaling and root planing (SRP) remains the “gold standard” treatment for periodontal diseases against which other treatments are compared. However, after nonsurgical therapy, several deep periodontal pockets may persist and in such cases, the treatment consists of surgical procedures.[2] Since the systemic antibiotics therapy has various disadvantages such as the development of resistant bacteria and also requires higher dosage to attain required gingival crevicular fluid concentration at the target site, this led to use of local drug delivery system.[3]
As an antiseptic, chlorhexidine has been used effectively for over 30 years in the treatment of periodontal disease. It shows a broad spectrum of topical antimicrobial activity, safety, effectiveness, substantivity, and lack of toxicity. However, after prolonged use it may lead to undesirable side-effect such as the pigmentation of teeth and oral tissues.[4]
Curcumin more commonly known as “Haldi” in its various forms is a very auspicious element in many religious ceremonies in Hindu families. Curcumin possesses anti-inflammatory, antioxidant, antimicrobial properties along with its hepatoprotective, immunostimulant, antiseptic, antimutagenic, and many more properties. It is for this concern that promotion of curcumin in dental terrain would prove beneficial.[5]
In this study, an attempt has been made to evaluate and compare the efficacy of gel containing curcumin and chlorhexidine as an adjunct to SRP.
Aim
To evaluate the efficacy of subgingival application of chlorhexidine gel and curcumin gel as an adjunct to SRP in the treatment of mild to moderate (4–6 mm) periodontal pockets.
MATERIALS AND METHODS
The study was carried out on thirty subjects who fulfilled the inclusion and exclusion criteria of the study. Ethical approval was obtained from the Institutional Review Board before the commencement of the study. All potential participants were explained the need and design of the study. Only those subjects who consented by written informed consent for the study were included.
Inclusion criteria
Age group of 25–50 years
Belonging to both sexes
Chronic periodontitis patients
Probing pocket depth (PPD) ≤5 mm
Gingival index (GI) (Loe and Silness 1963) score: 2.0–3.0
Plaque index (PI) (Silness and Loe 1964) score: 2.0–3.0.
Exclusion criteria
Subjects having taken antibiotics prior to or during the trial
Patients on medication likely to induce gingival enlargement
Pregnant or lactating women
Smokers
Tobacco chewers
Allergy to chlorhexidine gluconate and curcumin gel.
Methodology
Clinical examination
The required sample for the study was obtained from the outpatient Department of Periodontics. After recording of case history, clinical examination was carried out in a dental chair. The intraoral periapical radiographs of the region selected for the study were made. After fulfilling inclusion and exclusion criteria patients with localized or generalized chronic periodontitis cases were selected for the present study. Clinical parameters such as PI, GI, sulcus bleeding index, and pocket depth measurement were evaluated at baseline (0 day), 30th day and 45th day.
Study groups
The selected thirty samples were randomly divided into two groups using split mouth design namely Group I as control and Group II as experimental group. Left side was assigned for the control group (Group I) and right side for the experimental group (Group II).
Group I (control group): Thirty sites on the left side were treated by SRP followed by chlorhexidine gel placement in the periodontal pocket
Group II (experimental group): Thirty sites on the right side were treated by SRP followed by curcumin gel placement in the periodontal pocket.
Preparation of test materials
Chlorhexidine gel
In Group I (control group) 0.2% chlorhexidine gel (Cervitec Gel, Ivoclar Vivadent, Liechtenstein) was used.
The composition of chlorhexidine gel: 900 ppm F - and 0.2% chlorhexidine digluconate.
Ingredients: Aqua, hydroxyethyl cellulose, Laureth-23, chlorhexidine digluconate, sodium fluoride, aroma, sodium saccharin.
Curcumin gel
In Group II (experimental group) 2% curcumin gel, the experimental local drug delivery system (formulated by KLES College of Pharmacy, Belgaum, Karnataka, India) used in the study.
Curcumin powder: The curcumin powder (98% curcumin) used in the study. The details of 98% curcumin are as follows: Batch No.: C111860, AR No.: KL11I5373.
Preparation of 2% curcumin gel: Using pure curcumin powder 2% curcumin gel was prepared in KLES College of Pharmacy, Belgaum, Karnataka, India.
Procedure of periodontal therapy
Clinical examination was carried out and the baseline values prior to the procedure were recorded by a single calibrated examiner and values were recorded on a standardized form containing the demographic data of the patient [Figure 1]. Scaling was performed by piezoelectric ultrasonic SRP was performed by area specific Gracey Curettes®. After thorough SRP, PPD was re-determined followed by the local drug delivery in both control and experimental sites. In Group I, the area was completely dried using oil free air syringe, and then the site was isolated with cotton rolls to prevent contamination from saliva. The local drug delivery system consisting of 0.2% chlorhexidine gel was placed in the periodontal pockets by applicator tips or syringe with a needle attached to it [Figure 2a]. The pocket opening was covered by Coe-Pak to retain the material in the pocket, as well as to prevent the ingress of oral fluids.
Figure 1.

Photograph showing determination of pocket depth at baseline
Figure 2.
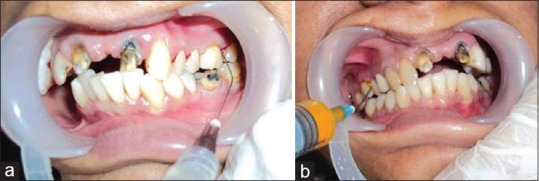
(a and b) Photograph showing local drug delivery in control site using 0.2% chlorhexidine gel and delivery in experimental site using 2% curcumin gel
Similarly, in Group II, the experimental site local drug delivery system consisting of 2% curcumin gel was placed in the periodontal pockets through a syringe with a needle attached to it [Figure 2b]. The pocket opening was covered by Coe-Pak to retain the material in the pocket, as well as to prevent the ingress of oral fluids.
The control and the experimental sites were again checked for the probing depth at 30th and 45th day [Figures 3a, b and 4a, b] respectively during follow-up.
Figure 3.
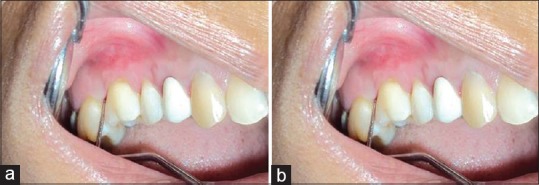
(a and b) Photograph showing determination of probing pocket depth on 30th day in control site and experimental site
Figure 4.
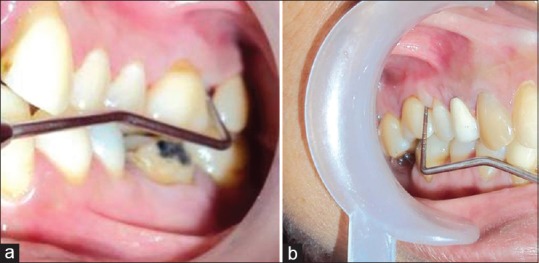
(a and b) Photograph showing determination of probing pocket depth on 45th day in control site and experimental site
Statistical analysis
All data were entered into a standardized format and analyzed to assess the efficacy of chlorhexidine gel (Group I) and curcumin gel (Group II) at 30 days and 45 days using the SPSS 16.0 version IBM SPSS Statistics 16, SPSS South Asia, Bangalore, India). Mean of standard deviation (SD) of parameters such as pocket depth, GI, PI, and sulcus bleeding index was computed and then the comparison between the study groups done using unpaired t-test. Within-group comparison was made using paired t-test. Test of significance was set at P < 0.05.
RESULTS
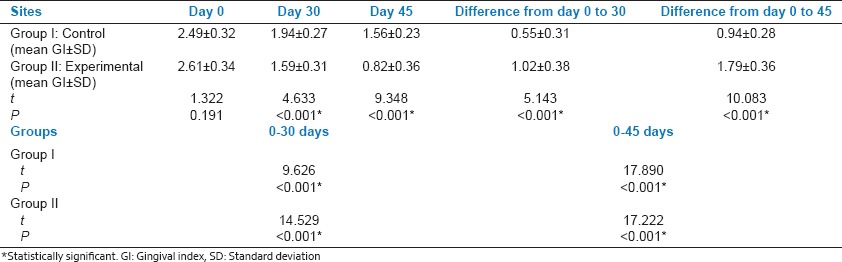
The mean ± SD for GI from day 0 to 30 was 0.55 ± 0.31 and 0.94 ± 0.28 from day 0 to 45 for control group and mean ± SD for GI from day 0 to 30 was 1.02 ± 0.38 and 1.79 ± 0.36 from day 0 to 45 for the experimental group. Mean GI was significantly lower in experimental group when compared with control group, with unpaired t-test P < 0.001. On intragroup comparison with paired t-test, t value was 9.626 from day 0 to 30 and 17.890 from day 0 to 45 for the control group and 14.529 from day 0 to 30 and 17.222 from day 0 to 45 for the experimental group with P < 0.001 [Table 1].
Table 1.
Gingival index mean values and intra-group comparison of gingival index in Group I and Group II from 0 to 45 days
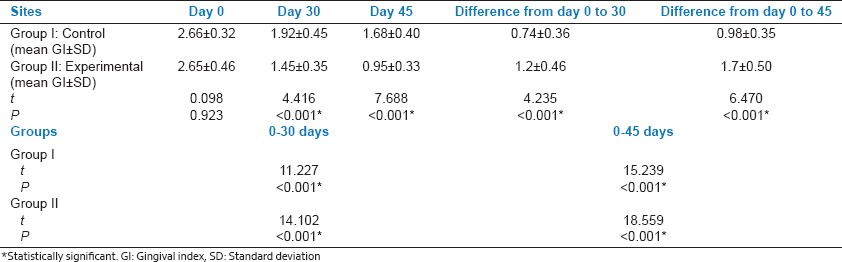
The mean ± SD for PI from day 0 to 30 was 0.74 ± 0.36 and 0.98 ± 0.35 from day 0 to 45 for control group and mean ± SD for PI from day 0 to 30 was 1.2 ± 0.46 and 1.7 ± 0.50 from day 0 to 45 for experimental group. Mean PI was significantly lower in experimental group when compared with control group, with unpaired t-test P < 0.001. On intragroup comparison with paired t-test, t value was 11.227 from day 0 to 30 and 15.239 from day 0 to 45 for the control group and 14.102 from day 0 to 30 and 18.559 from day 0 to 45 for the experimental group with P < 0.001 [Table 2].
Table 2.
Plaque index mean values and intra-group comparison of plaque index in Group I and Group II from 0 to 45 days
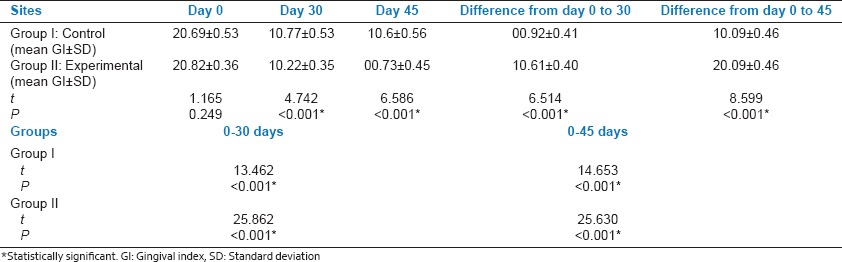
The mean ± SD for Sulcular Bleeding Index (SBI) from day 0 to 30 was 0.92 ± 0.41 and 1.09 ± 0.46 from day 0 to 45 for control group and mean ± SD for SBI from day 0 to 30 was 1.61 ± 0.40 and 2.09 ± 0.46 from day 0 to 45 for experimental group. Mean SBI was significantly lower in experimental group when compared with control group, with unpaired t-test P < 0.001. On intragroup comparison with paired t-test, t value was 13.462 from day 0 to 30 and 14.653 from day 0 to 45 for control group and 25.862 from day 0 to 30 and 25.630 from day 0 to 45 for experimental group with P < 0.001 [Table 3].
Table 3.
Sulcus bleeding index mean values and intra-group comparison of sulcus bleeding index in Group I and Group II from 0 to 45 days
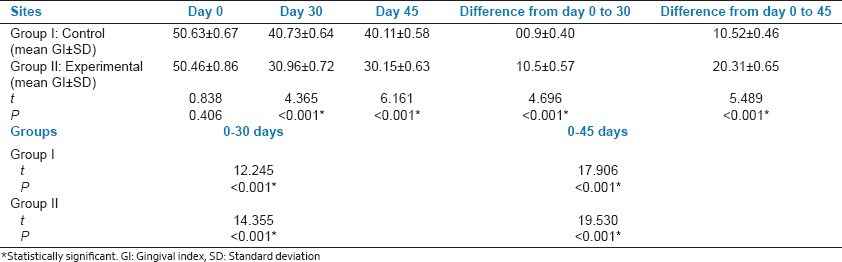
The mean ± SD for PPD from day 0 to 30 was 0.9 ± 0.40 and 1.52 ± 0.46 from day 0 to 45 for control group and mean ± SD for PPD from day 0 to 30 was 1.5 ± 0.57 and 2.31 ± 0.65 from day 0 to 45 for experimental group. Mean PPD was significantly lower in experimental group when compared with control group, with unpaired t-test P < 0.001. On intragroup comparison with paired t-test, t value was 12.245 from day 0 to 30 and 17.906 from day 0 to 45 for control group and 14.355 from day 0 to 30 and 19.530 from day 0 to 45 for experimental group with P < 0.001 [Table 4].
Table 4.
Probing pocket depth mean values and intra-group comparison of probing pocket depth in Group I and Group II from 0 to 45 days
DISCUSSION
Local delivery of antimicrobial agents has been investigated for overcoming the limitations of conventional SRP therapy. Recently, the use of sustained release formulations to deliver antimicrobial agents to the site of infection in periodontal pockets has become successful therapy.[5]
Chlorhexidine has long been known as an effective anti-inflammatory, antimicrobial agent, antiseptic agent, and shown many other beneficial properties. Recently, Indian traditional ayurvedic medicine like curcumin (polyphenol-rich natural product) has shown strong anti-inflammatory and antioxidant properties.[6] To overcome the shortcomings of chlorhexidine and also to evaluate the efficacy of ayurvedic herbal medicine like curcumin in periodontal treatment present study was designed and carried out in a systematic way.
The GI score showed significant reduction for both the treatment groups. Previous studies by Rams TE et al.[7] and Rodrigues et al.[8] also shown reduction in gingival inflammation with chlorhexidine gel which was similarly observed in our study.
Reduction in gingival inflammation was observed in our study. A significant reduction was seen 30th day and 45th day as compared to chlorhexidine group which was similar to the previous studies carried out by Behal R et al.[9] and Gopinath V et al.[10] who used 2% curcumin gel as a local drug delivery system. Thus, the greater significant reduction of GI score in the experimental sites (curcumin) in our study could be due to the anti-inflammatory, antibacterial, antioxidant properties of curcumin.
Reduction in plaque was better in curcumin group as compared to chlorhexidine group at all the follow-up periods and which were similarly observed with previous studies by Kuru et al.,[11] Lawande et al.[12] and Khan and Antony.[13] The greater significant reduction of PI score in the experimental sites (curcumin) in our study could be due to the anti-plaque property of curcumin.[12] The total curcuminoids content showed better antibacterial as well as antifungal activity against important bacteria Escherichia coli, Enterobacter aerogenes, and Pseudomonas aeruginosa and two fungi Aspergillus niger and Candida albicans as compared to volatile oil extracted from curcumin.
Reduction in sulcus bleeding index score was better in curcumin group as compared to chlorhexidine group at all the follow-up periods from immediate to 45 days and which were similarly observed with previous studies by Birang R et al.,[14] Mali AM et al.[15] The reduction in bleeding index score at the experimental site (curcumin) may be due to its anti-inflammatory action.
Reduction in PPD score was better in curcumin group as compared to chlorhexidine group at all the follow-up periods from immediate to 45 days and which were similarly observed with previous studies by Kondreddy et al.[16,17] The greater significant reduction of PPD score in the experimental sites (curcumin) in our study could be due to the antimicrobial action of curcumin.
Less literature is available on curcumin gel as a local drug delivery system in the treatment of chronic periodontitis. To the best of our knowledge, curcumin gel used as a local drug delivery system is based on its bioadhesive and other various properties such as anti-inflammatory, antiseptic, antibacterial, antimutagenic, anticarcinogenic, hepatoprotective, healing properties, it is also well accepted by all the subjects of our study without any side effects.
Curcuma longa's anti-inflammatory properties may be attributed to its ability to inhibit both biosyntheses of inflammatory prostaglandins from arachidonic acid and neutrophil function during inflammatory states.
Limitations of the present study were lesser sample size, short-term follow-up and microbiological evaluation was not done as it was taken as a pilot study. To use the curcumin gel as a local drug delivery system, further long-term studies with a larger sample size are required to analyze its clinical and microbiological efficacy in comparison to other available marketed local drug delivery products in the treatment of chronic periodontitis.
CONCLUSION
It can be concluded that both chlorhexidine gel and curcumin gel can be used as an adjunct to SRP, but the curcumin gel has shown to be more effective than the chlorhexidine gel in the treatment of mild to moderate periodontal pockets.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Oosterwaal PJ, Mikx FH, van’t Hof MA, Renggli HH. Comparison of the antimicrobial effect of the application of chlorhexidine gel, amine fluoride gel and stannous fluoride gel in debrided periodontal pockets. J Clin Periodontol. 1991;18:245–51. doi: 10.1111/j.1600-051x.1991.tb00422.x. [DOI] [PubMed] [Google Scholar]
- 2.Unsal E, Akkaya M, Walsh TF. Influence of a single application of subgingival chlorhexidine gel or tetracycline paste on the clinical parameters of adult periodontitis patients. J Clin Periodontol. 1994;21:351–5. doi: 10.1111/j.1600-051x.1994.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 3.Amitha R, Thomas B, Sathish M. Comparative evaluation of sub-gingival application of chlorhexidine varnish and chlorhexidine gel as an adjunct to full mouth scaling and root planing in the treatment of moderate to deep periodontal pockets - A clinical study. J Indian Dent Assoc. 2011;5:369–72. [Google Scholar]
- 4.Perinetti G, Paolantonio M, Cordella C, D’Ercole S, Serra E, Piccolomini R. Clinical and microbiological effects of subgingival administration of two active gels on persistent pockets of chronic periodontitis patients. J Clin Periodontol. 2004;31:273–81. doi: 10.1111/j.1600-051x.2004.00481.x. [DOI] [PubMed] [Google Scholar]
- 5.Pragati S, Ashok S, Kuldeep S. Recent advances in periodontal drug delivery systems. Int J Drug Deliv. 2009;1:1–14. [Google Scholar]
- 6.Basnet P, Skalko-Basnet N. Curcumin: An anti-inflammatory molecule from a curry spice on the path to cancer treatment. Molecules. 2011;16:4567–98. doi: 10.3390/molecules16064567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol 2000. 1996;10:139–59. doi: 10.1111/j.1600-0757.1996.tb00072.x. [DOI] [PubMed] [Google Scholar]
- 8.Rodrigues IF, Machion L, Casati MZ, Nociti FH, Jr, de Toledo S, Sallum AW, et al. Clinical evaluation of the use of locally delivered chlorhexidine in periodontal maintenance therapy. J Periodontol. 2007;78:624–8. doi: 10.1902/jop.2007.060317. [DOI] [PubMed] [Google Scholar]
- 9.Behal R, Mali AM, Gilda SS, Paradkar AR. Evaluation of local drug-delivery system containing 2% whole turmeric gel used as an adjunct to scaling and root planing in chronic periodontitis: A clinical and microbiological study. J Indian Soc Periodontol. 2011;15:35–8. doi: 10.4103/0972-124X.82264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gopinath V, Ramakrishnan T, Emmadi P, Ambalavanan N, Mammen B, Vijayalakshmi Effect of a controlled release device containing minocycline microspheres on the treatment of chronic periodontitis: A comparative study. J Indian Soc Periodontol. 2009;13:79–84. doi: 10.4103/0972-124X.55844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuru L, Kuru B, Noyan U, Kukrer A, Acar T, Yilmaz S. Effects of adjunctive local or systemic metronidazole with non-surgical periodontal therapy on periodontal clinical parameters and gingival crevicular fluid biomarkers. Nobel Med. 2012;8:89–94. [Google Scholar]
- 12.Lawande SA. Therapeutic applications of turmeric (Curcuma longa) in dentistry: A promising future. J Pharm Biomed Sci. 2013;27:586–91. [Google Scholar]
- 13.Khan R, Antony VV. Efficacy of chlorhexidine varnish on Streptococcus mutans in plaque. Orthod Cyber J. 2010:1–10. [Google Scholar]
- 14.Birang R, Yaghini J, Adibrad M, Kiany S, Mohammadi Z, Birang E. The effects of diode laser (980 nm Wavelength) and chlorhexidine gel in the treatment of chronic periodontitis. J Lasers Med Sci. 2011;2:131–8. [Google Scholar]
- 15.Mali AM, Behal R, Gilda SS. Comparative evaluation of 0.1% turmeric mouthwash with 0.2% chlorhexidine gluconate in prevention of plaque and gingivitis: A clinical and microbiological study. J Indian Soc Periodontol. 2012;16:386–91. doi: 10.4103/0972-124X.100917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kondreddy K, Ambalavanan N, Ramakrishna T, Kumar RS. Effectiveness of a controlled release chlorhexidine chip (PerioCol™ -CG) as an adjunctive to scaling and root planing when compared to scaling and root planing alone in the treatment of chronic periodontitis: A comparative study. J Indian Soc Periodontol. 2012;16:553–7. doi: 10.4103/0972-124X.106909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verma A, Sanghi S, Grover D, Aggarwal S, Gupta R, Pandit N. Effect of insertion of xanthan-based chlorhexidine gel in the maintenance phase following the treatment of chronic periodontitis. J Indian Soc Periodontol. 2012;16:381–5. doi: 10.4103/0972-124X.100916. [DOI] [PMC free article] [PubMed] [Google Scholar]


