Abstract
Introduction:
Over a period, tribal population has migrated to cities in search of livelihood. Data on various health problems of the tribes are sparse. Sugalis constitute the third largest tribe in Andhra Pradesh and have settlements in urban areas.
Objective:
To estimate the prevalence of malnutrition, diarrhea, and acute respiratory infections (ARI) among under-five children of Sugali tribe living in Chittoor district of Andhra Pradesh state in South India.
Materials and Methods:
A community-based cross-sectional study was conducted in four community blocks/mandals in 2012. A total of 500 Sugali households with under-five were identified. Demographic details, episodes of diarrhea, and ARI among under-five children and treatment/care seeking behavior were collected from mothers/care givers by interview. Nutritional status was assessed using new WHO standards.
Results:
Of the total 669 children in these 500 households, 343 (51.3%) were girls and 326 (48.7%) were boys. In the last 1 month, 21.4% (18.4-24.6) reported diarrhea and 51.6% (47.7-55.3) reported ARI. The prevalence of underweight, wasting, and stunting among under-five children was 32.7% (29.1-36.4), 18.3% (15.3-21.4), and 38.3% (34.2-41.9), respectively. Majority (70%) sought treatment for illness in modern system of medicine and only few continued with the practice of herbs and traditional medicine.
Discussion:
Despite living in urban area, the tribal children had high prevalence of malnutrition, diarrhea, and ARI, though lower compared to other tribes in India possibly due to improved access to health care services. Efforts need to be strengthened for social inclusion of tribes into mainstream.
Key words: Acute respiratory tract infection, diarrhea, malnutrition, scheduled tribe, treatment seeking behavior
INTRODUCTION
India is home to almost half the tribal population of the world.[1] The Scheduled Tribe population of the country, as per the 2011 census, was 104 million, constituting 8.6% of the total population.[2] Sugali tribe (also known as Lambadi and Banjara, and we refer them as Sugali throughout this paper) of Andhra Pradesh represents one such tribe. Historically, Sugali were nomadic pastoralists from the North/Western plains of India and have migrated to different parts of the country, and mainly settled in the Southern states of Andhra Pradesh and Telangana and are listed under scheduled tribe. In India, they are estimated to be around 5-6 million. In Andhra Pradesh, Sugalis are the third largest tribe with 3.6 lakh population.[2,3] Majority of the Indian tribes are still socially and geographically isolated with little contact with modern civilization. These groups are also vulnerable particularly in the areas of health, education, and socioeconomic aspects.[4] However, over a period of time; many of these tribes have gradually integrated into the rest of the society.
While integration is a welcome step, it presents another set of challenges. Integration results in acculturation with a mix of traditional beliefs with modern beliefs resulting in changes in practices and customs. The children are probably one of the groups that would be affected most by these changes. This is not only because they are a vulnerable group, but also because many of the beliefs which undergo a change are related to child birth and child rearing.[5] Diarrhea, acute respiratory tract infections, and malnutrition are among the most common of child morbidities. Diarrheal disease is the second leading cause of death in children under 5 years old while acute respiratory infections (ARIs) are among the leading causes of death in children under 5 years.[6] Malnutrition is the underlying cause for the increased susceptibility to infections and is indirectly responsible for many child deaths.[7,8]
Although the prevalence of acute respiratory and diarrheal diseases in under-five children in India have been adequately studied,[9,10,11,12,13,14] there is still a paucity of studies from the tribal population. The current study was planned to estimate the prevalence of malnutrition, ARI, and diarrheal diseases among under-five children of Sugali tribe, Chittoor District in Andhra Pradesh state of South India and their treatment seeking behavior.
MATERIALS AND METHODS
This study was conducted in Madanapalle revenue division of Chittoor district in Andhra Pradesh. Four mandals (administrative units in a district) with high proportion of the Sugali population were selected. All thandas (Sugali settlements are known as thandas and are usually located at one end of the village) and urban settlements inhabited by the Sugalis were included. Most of the urban settlements were a single ethnic in nature. The sample size was calculated considering the point prevalence of ARI among under-five children as 12.4%,[15] assuming an alpha error of 0.05 and relative precision of 25%, the required sample size would be 470. Since the population of this tribe was small, all households were visited and households with at least one under-five child were included in the study.
A house to house survey was conducted in each of the selected thandas. A semi-structured pretested interview schedule was used to collect information from the mother. In some cases (if mother was not available or in case of orphaned children), information was collected from the caregiver. All interviews were conducted in local language (Telugu). All data were collected by the first author (VB), who is fluent in Telugu. Demographic details of the family, episodes of ARI, and diarrhea in the last 1 month and treatment care seeking behavior for that episode were collected. Weight and height were measured for all the selected children. Weight was measured by Omron Weight Scale HN 283 after correction for zero error. The mother/caregiver was asked to remove shoes and outer clothing of the child. The child was asked to stand in the middle of the scale, feet slightly apart, and to remain still until the weight appeared on the display. Weight was recorded to the nearest 0.1 kg. For children unable to stand independently, mother/caregiver was weighed with and without the child and the difference was used as the child's weight. Height was measured using a stadiometer and recumbent length was measured using an infantometer to the nearest 0.5 cm. All measurements were taken twice and the average of two readings was used for analysis. The child was considered to have ARI if caregiver reported child having any of the symptoms viz., cough, sore throat, nasal discharge, ear discharge, or respiratory distress with or without fever in past 1 month. The child was considered to have diarrhea if the mother/caregiver reported passing of three or more loose stools in past 1 month. For children below 6 months, a recent change in the consistency of stool and water content more than fecal matter was defined as diarrhea. New WHO 2006 growth standards were used to classify the nutritional status of the child. Z scores of weight for age, height for age, and weight for height were calculated.
The study was approved by the Institute's Ethics Committee. Necessary permissions were taken from the Chittoor district administration for conducting the study. Data were entered in Microsoft excel spreadsheet and analyzed with SPSS version 17.0 (Chicago, IL, USA). Wherever applicable, proportions and mean standard deviation (SD) were calculated. Chi-square test was used a test of significance. P-value < 0.05 was considered significant.
RESULTS
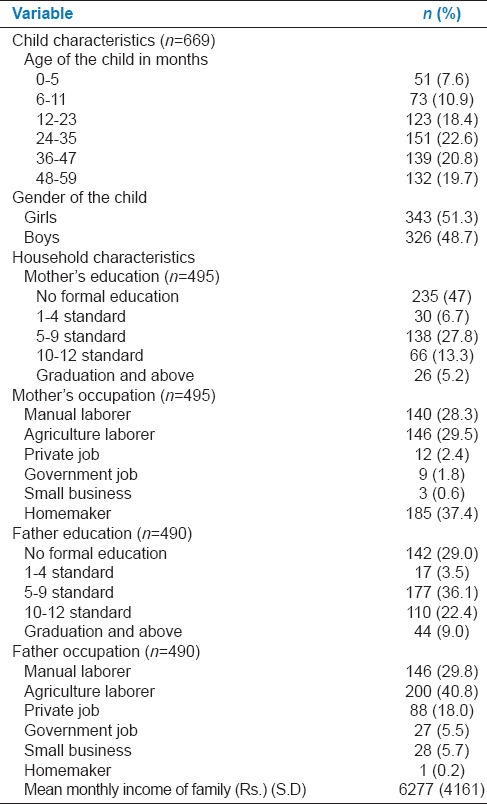
A total of 500 households were studied and all the 669 under-five children who were available from these households were included. Information on parents was available for only 495 mothers and 490 fathers (5 women were widows and five households had orphans) Table 1 presents the demographic and socioeconomic characteristics of the study sample. Out of the total 669 children, 343 (51%) were girls and 326 (49%) were boys. Three fifth (61%) of the mothers were of age <25 years and around 68% of fathers were <35 years of age (data not shown). Half of the mothers (47%) had not received any education. Only 28% mothers received education up to 9 standard. Only 5% of the mother had completed graduation. Mothers were generally involved in agriculture (30%) or were daily wage laborers (28%). Twenty-nine percentage of the fathers were illiterate, while 36% had completed 9 standard of education and only 9% completed graduation. As was seen with mothers, agriculture and manual labor were their main occupations. The average monthly household income was INR 6277 ± 4161 (US $ 98.47 ± 65.28).
Table 1.
Demographic and socioeconomic characteristics of the study population
The prevalence of underweight, wasting, and stunting among under-five children was 32.7%, 18.3%, and 38.3%, respectively. Of the total, 9.3%, 6.0%, and 13.5% of children were severely underweight, wasted, and stunted, respectively [Table 2]. The prevalence of underweight was similar among boys and girls (P = 0.38). There was statistically significant difference by age group in the prevalence of underweight (P = 0.007), wasting (P < 0.001), and stunting (P < 0.001).
Table 2.
Prevalence (95% CI) of underweight, wasting, stunting, ARI, and diarrhea by sex and age among under-five study children (n = 669)
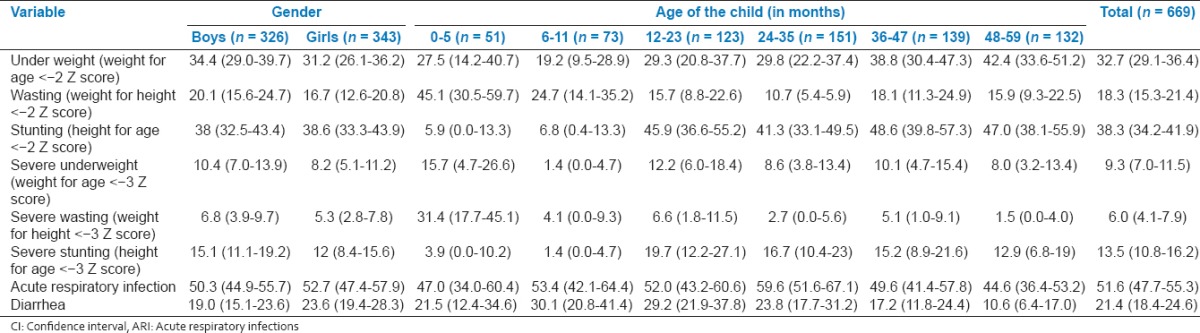
More than half of the children had at least one episode of ARI (51.6%) during last 1 month. The prevalence of ARI was similar in boys and girls (P > 0.14). There were no significant differences in prevalence of ARI by age group (P > 0.08), though highest prevalence was reported in 24-35 months of age group [Table 2]. Nearly, one fifth (21.4%) of the children have had at least one episode of diarrhea during the last 1 month. The prevalence of diarrhea was found to be significantly different by age (P < 0.03) with children aged 5-11 months (30%) followed by 12-23 months (29%), reporting higher prevalence of diarrhea.
The data on treatment seeking behavior show that approximately three fourths of the children with illness sought some sort of treatment either in modern or in traditional medicine [Table 3]. There was no statistically significant gender differences in terms of the place of treatment sought. Around two thirds of children with diarrhea (67%) and 69% with ARIs were taken to a modern health facility for treatment. 10.7% children with diarrhea and 1.3% with ARI were taken to traditional healers. Majority of the children had received home remedies (50.2%) along with medicines during the episode of diarrhea. The most common home remedy for diarrhea was feeding buttermilk to the child. The mean interval in seeking treatment was 1.31 (SD, 0.83) and 2.13 (SD, 1.01) days, respectively, for diarrhea and ARIs. The delay in seeking care was due to nonperception of seriousness, access issues, and lack of resources (time and money).
Table 3.
Treatment seeking behavior for the recent episode of diarrhea and acute respiratory infections among study population
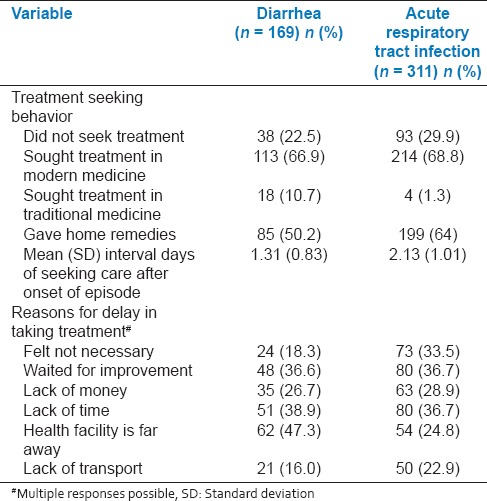
Around 43.1% of mothers and caregivers knew that children with diarrhea should receive extra fluids (data not shown). Around 37% continued to feed their children in the same manner as before the onset of the diarrheal episode. One third of the respondents said that they reduced the amount of food and fluids during the last episode of diarrhea. A similar number of mothers and caregivers avoided giving certain foods during the episode of diarrhea, spicy food being the most common. In case of ARI, 71% of the mothers did not change the diet of the child during the last episode of ARI. Giving turmeric-laced milk and chewing ragi malt were common practices during the episodes of ARIs (data not shown).
DISCUSSION
The present study was undertaken to estimate the prevalence of common childhood morbidities among under-five children of Sugali tribe from Andhra Pradesh. The prevalence of malnutrition, diarrhea, and ARIs were high among these children.
The prevalence of underweight, wasting, and stunting in the present study was similar to that estimated by UNICEF Rapid Survey on Children, 2013-2014 (underweight 29.4%, wasting 15.1%, and stunting 38.7%).[16] The prevalence of underweight among the children in the present study was comparable to rural Andhra Pradesh (39%).[14] When compared with the other tribal populations of India, the burden of underweight, among Sugali tribal children was found to be lower compared to those reported from other tribal populations of Madhya Pradesh (61.6%),[15] Odisha (58%),[9] West Bengal (80.9%),[10] Maharashtra (64%),[11] and similar to those reported from urban slums of Punjab (29.5%),[12] West Bengal (41.6%),[13] and rural Haryana (25.3%).[17] However, in contrast to underweight, stunting was lower compared to urban slums of Punjab (74%)[12] and Delhi (53%),[18] but similar to a rural Haryana (46.2%).[17] The prevalence of wasting was similar to urban slums of Delhi (23%)[18] and rural Andhra Pradesh (22%).[14]
The prevalence rates of diarrhea in the present study was similar (24.8%) to a study done in urban slum of Puducherry among under-five children.[19] The prevalence of diarrhea as well as ARI were four times higher than the estimate for Chittoor district as reported in District level household and facility survey (DLHS)-III[20] and three times higher than that reported done in tribal area of Maharashtra (5.8%).[21] The present results were lower compared to urban slum of West Bengal (31.7%)[22] and rural areas of Kashmir 25.2% (2 weeks).[23] Around half (43.1%) of the mothers and caregivers knew that children with diarrhea should receive extra fluids. Similar findings were reported in DLHS-III (41.0%).[20] In contrast, a study done in Wardha district, Maharashtra documented that around two thirds (60%) of the mothers practiced oral rehydration therapy. Nearly, one third continued to give the usual amount of food during a diarrheal episode.[24] The prevalence of diarrhea in the present study was higher than that reported by other studies in tribal areas,[11,15,25] but lower than rural and urban slums.
The prevalence of ARI was nearly similar to a study done in Puducherry (59.1%),[26] but highest among various studies conducted in tribal areas[15,25] and urban slums of Guwahati (26.2%).[27] Nearly, two thirds of the children suffering from ARI were taken for treatment, usually after 2 days, if the condition of the child was not improving. This proportion was similar to that reported by DLHS-III (79.2%).
The findings of the health situation being better than other tribal areas, but poorer than in urban slums or rural areas might reflect the changing socioeconomic situation and habits of the tribal population. Relatively lower prevalence of malnutrition can be attributed to the relatively better economic position of the Sugalis compared to the other tribes of Andhra Pradesh. Sugalis are relatively better off in terms of living conditions, educational attainment, extent of land holdings and other sources of earnings, and could access the government services and schemes, which have contributed in the process of economic development of the community. Successes of the various inclusive and developmental processes by the government as well as nongovernmental organizations in the lives of Sugali have been documented.[28]
The study has its limitations as well. The number of episodes of ARI and diarrhea were self-reported for last 1 month and there could be a possibility of recall bias. The information on diarrhea and ARI was collected in the months of June and July. As both are seasonal diseases, this does not reflect the annual load of morbidity. Various practices and processes, especially that focus on the development and integration of a tribal population can be better assessed through qualitative techniques; however, this was beyond the scope of the present study. For children who could stand independently “tare” weighing was done. This could have introduced some degree of measurement error leading to underestimation of malnutrition.
CONCLUSION AND RECOMMENDATIONS
The children of Sugali tribe of Andhra Pradesh had prevalence of malnutrition higher than urban areas, but lower than rural. However, the prevalence of malnutrition, diarrhea, and ARI among children of Sugali tribe of Andhra Pradesh was less compared to other tribes in India possibly due to improved access to various services including healthcare through programs for social inclusion. A further evaluation of the problem of the tribes needs to be done, using a mixed methods approach to understand issues related to not only health, but also social development and integration.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ministry of Home Affairs Government of India. Census of India: Provisional Population Tables. 2011. [Last cited on 2013 Apr 15]. Available from: http://www.censusindia.gov.in/pca/Searchdata.aspx .
- 2.Ministry of Home Affairs Government of India. Census of India: Provisional Population Tables. 2001. [Last cited on 2013 Apr 15]. Available from: http://www.censusindia.gov.in/Data_Products/Library/Provisional_Population_Total_link/webed.html .
- 3.Ministry of Tribal Affairs Government of India. Statistical Profile of Scheduled Tribes in India. Demographic Status of Scheduled Tribe Population and Its Distribution. 2013. [Last cited on 2015 Apr 15]. Available from: http://www.tribal.nic.in/WriteReadData/CMS/Documents/2014101705192952220 .
- 4.Ministry of Health and Family Welfare Government of India. National Family Health Survey. 1998-99. [Last cited on 2015 Jun 15]. Available from: http://www.rchiips.org/NFHS/pub_nfhs-2.shtml .
- 5.Ministry of Tribal Affairs Government of India. Annual Report. 2013-14. [Last cited on 2013 Oct 27]. Available from: http://www.tribal.nic.in/WriteReadData/CMS/Documents/201305090204592676637Annualreport.pdf .
- 6.World Health Organization. Acute Respiratory Infections. [Last cited on 2013 Jul 10]. Available from: http://www.who.int/vaccine_research/diseases/ari/en/
- 7.World Health Organization. Diarrhoeal Disease. [Last cited on 2013 Jul 10]. Available from: http://www.who.int/mediacentre/factsheets/fs330/en/
- 8.Rodríguez L, Cervantes E, Ortiz R. Malnutrition and gastrointestinal and respiratory infections in children: A public health problem. Int J Environ Res Public Health. 2011;8:1174–205. doi: 10.3390/ijerph8041174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meshram II, Balakrishna N, Arlappa N, Rao KM, Laxmaiah A, Brahmam GN. Prevalence of under nutrition, its determinants, and seasonal-variation-among tribal preschool children of Odisha state, India. Asia Pac J Public Health. 2012;11:125–32. doi: 10.1177/1010539512441492. [DOI] [PubMed] [Google Scholar]
- 10.Ray SK, Biswas AB, Kumar S. A study of dietary pattern, household food security and nutritional profile of under-five children of a community of West Bengal. J Indian Med Assoc. 2000;98:517. [PubMed] [Google Scholar]
- 11.Meshram II, Arlappa N, Balakrishna N, Laxmaiah A, Mallikarjun Rao K, Gal Reddy Ch, et al. Prevalence and determinants of undernutrition and its trends among pre-school tribal children of Maharashtra State, India. J Trop Pediatr. 2012;58:125–32. doi: 10.1093/tropej/fmr035. [DOI] [PubMed] [Google Scholar]
- 12.Sengupta P, Philip N, Benjamin AI. Epidemiological correlates of under-nutrition in under-5 years children in an urban slum of Ludhiana. Health Popul Perspect Issues. 2010;33:1–9. [Google Scholar]
- 13.Shit S, Taraphdar P, Mukhopadhyay DK, Sinhababu A, Biswas AB. Assessment of nutritional status by composite index for anthropometric failure: A study among slum children in Bankura, West Bengal. Indian J Public Health. 2012;56:305–7. doi: 10.4103/0019-557X.106421. [DOI] [PubMed] [Google Scholar]
- 14.Meshram II, Laxmaiah A, Gal Reddy CH, Ravindranath M, Venkaiah K, Brahmam GN. Prevalence of under-nutrition and its correlates among under 3 year-old children in rural areas of Andhra Pradesh, India. Ann Hum Biol. 2011;38:93–101. doi: 10.3109/03014460.2010.498387. [DOI] [PubMed] [Google Scholar]
- 15.Rao VG, Yadav R, Dolla CK, Kumar S, Bhondeley MK, Ukey M. Undernutrition & childhood morbidities among tribal preschool children. Indian J Med Res. 2005;122:43–7. [PubMed] [Google Scholar]
- 16.Ministry of Women and Child Development Government of India. Rapid Survey on Children. 2013-14. [Last cited on 2015 Sep 27]. Available from: http://www.wcd.nic.in/issnip/National_Fact%20sheet_RSOC%20_02-07-2015.pdf .
- 17.Gupta A, Kalaivani M, Gupta SK, Rai SK, Nongkynrih B. Burden of under nutrition, composite index of anthropometric failure (CIAF) and perception of caregivers about under nutrition among under five children in rural India. Indian J Nutr Diet. 2015;52:140–52. [Google Scholar]
- 18.Saxena N, Nayar D, Kapil U. Prevalence of underweight, stunting and wasting. Indian Pediatr. 1997;34:627–31. [PubMed] [Google Scholar]
- 19.Upadhyay RP, Chinnakali P, Bhilwar M, Krishnan B, Kulkarni V, Gupta A, et al. Prevalence of malnutrition, acute respiratory infections and diarrhoea in children aged 1-5 years in urban slums of Puducherry, South India. Int J Contemp Pediatr. 2015;2:37–41. [Google Scholar]
- 20.District Level Household & Facility Survey, India. 2007-2008. [Last cited on 2013 Jun 15]. Available from: http://www.rchiips.org/prch-3.html .
- 21.Giri VC, Dhage VR, Zodpey SP, Ughade SN, Biranjan JR. Prevalence and pattern of childhood morbidity in a tribal area of Maharashtra. Indian J Public Health. 2008;52:207–9. [PubMed] [Google Scholar]
- 22.Banerjee B, Hazra S, Bandyopadhyay D. Diarrhea management among under fives. Indian Pediatr. 2004;41:255–60. [PubMed] [Google Scholar]
- 23.Ahmed SF, Farheen A, Muzaffar A, Mattoo GM. Prevalence of diarrhoeal disease, its seasonal and age variation in under- fives in Kashmir, India. Int J Health Sci (Qassim) 2008;2:126–33. [PMC free article] [PubMed] [Google Scholar]
- 24.Datta V, John R, Singh VP, Chaturvedi P. Maternal knowledge, attitude and practices towards diarrhea and oral rehydration therapy in rural Maharashtra. Indian J Pediatr. 2001;68:1035–7. doi: 10.1007/BF02722350. [DOI] [PubMed] [Google Scholar]
- 25.Patnaik SK. Diarrhoeal diseases in children - A survey in east Godavari District of Andhra Pradesh. J Commun Dis. 1990;22:43–6. [PubMed] [Google Scholar]
- 26.Kumar SG, Majumdar A, Kumar V, Naik BN, Selvaraj K, Balajee K. Prevalence of acute respiratory infection among under-five children in urban and rural areas of Puducherry, India. J Nat Sci Biol Med. 2015;6:3–6. doi: 10.4103/0976-9668.149069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Islam F, Sarma R, Debroy A, Kar S, Pal R. Profiling acute respiratory tract infections in children from Assam, India. J Glob Infect Dis. 2013;5:8–14. doi: 10.4103/0974-777X.107167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eswarappa K. Inclusion of Sugali community in the development process: A case study form South India. Int J Sociol Anthropol. 2012;4:204–17. [Google Scholar]


