Abstract
Objective
Identify barriers and facilitators to improve prenatal fruit and vegetable (F&V) intake among WIC eligible Latinas using the Health Action Process Approach framework.
Design
Qualitative data were collected via audiotaped in-depth interviews as part of a larger study to design an intervention to increase prenatal F&V intake.
Setting
Hartford, Connecticut.
Participants
Forty-five WIC eligible Latinas completed the study. Included women were: a) ≥ 18 years old; b) in 2nd or 3rd trimester; c) having a singleton pregnancy; d) overweight or obese (i.e. pregravid BMI ≥ 25); e) not on a restricted diet; h) nonsmokers.
Phenomenon of Interest
Prenatal factors that promote and hinder F&V intake.
Analysis
Transcripts were independently read, coded, and consensus was reached about emerging themes.
Results
Ten factors influenced prenatal F&V intake: i) social support, ii) family structure, iii) F&V access, iv) F&V preferences, v) F&V knowledge, vi) F&V health outcome expectations, vii) self-efficacy, viii) intentions, ix) F&V action/coping planning strategies, and x) maternal health status.
Conclusions and Implications
Social support from family/friends emerged as the primary distal factor driving prenatal F&V intake. Interventions designed to empower pregnant Latinas to gain the access, confidence, knowledge, and strategies necessary to consume more F&Vs need to consider strengthening support to achieve the desired outcome.
INTRODUCTION
Optimal fruit and vegetable (F&V) consumption has been recognized as one of the cornerstones of a healthy diet for decades. F&Vs provide key nutrients essential to promoting and maintaining health. An abundance of evidence shows that diets rich in F&Vs reduce chronic disease risk including coronary heart disease, stroke and asthma.1–3 The recent Scientific Report of the 2015 Dietary Guidelines Advisory Committee underscores the crucial link between F&V intake and health by identifying F&Vs as the only consistent dietary components recommended for improving every health outcome evaluated by the Committee.4
Despite the undisputed health benefits, only about 10% and 15% of the U.S. population consume the recommended daily amounts of F&Vs, respectively.4 National F&V consumption trends have changed little since 2001, with vegetable consumption declining slightly and fruit intake remaining low but stable.4 Although F&V consumption trends in the U.S. are low overall, recent survey findings suggest there are racial/ethnic disparities in F&V daily intake. Minority groups, especially Latinos/Latinas, are less likely to consume the recommended daily intake of F&Vs compared to non-Latino whites. 5
Inadequate F&V consumption has unintended consequences, especially during critical life course stages, such as pregnancy. Pregnancy reflects a unique period when maternal dietary intake has implications for both the mother and the developing fetus. Suboptimal maternal dietary intake during pregnancy is associated with adverse pregnancy outcomes, including gestational diabetes and hypertension6, and poorer birth outcomes.7 Evidence suggests that improving prenatal F&V intake can promote optimal pregnancy and birth outcomes. Higher maternal F&V intake before or during pregnancy is associated with a decreased risk of miscarriage8, pre-eclampsia 9, 10, upper respiratory infections11, and protects against gestational diabetes12 in the mother. Infant birthweight improves with higher maternal F&V intake, with stronger associations seen among women living in less developed countries.13
Pregnancy is a crucial lifecycle phase that can be a powerful “teachable moment”. 14 During pregnancy, women may be more committed to adopting healthier behaviors, such as consuming more F&Vs, to minimize health risks to themselves and their unborn babies.14 Yet, achieving recommended intake levels of F&Vs, especially during pregnancy, can be challenging. Limited access, higher cost, poor quality, lack of transportation, low perceived self-efficacy, and low social support influence healthy eating behaviors, including F&V consumption, among low-income women.15, 16 Surmounting these barriers and effectively changing behavior to increase F&V intake during pregnancy requires bridging the gap between the intention to change (i.e., wanting to increase F&V intake) and the action of behavior change (i.e., improving F&V intake). The Health Action Process Approach (HAPA) is a health behavior social change model that includes mediator variables, which help to describe the gap between intentions and actual behavior.17, 18 This theory is particularly relevant to changing prenatal F&V intake behaviors, as women often intend to change dietary behaviors during pregnancy, with the intent of providing a healthy environment for their unborn child.14 However, pregnancy related changes such as cravings, morning sickness, and heartburn as well as lower motivation and exhaustion can inhibit behavior change. Situational barriers as well as resources can also influence behavior change by providing an environment that can hinder or encourage the adoption of healthy behaviors. 17, 18 For example, social support can create an enabling environment for prenatal F&V behavior change (i.e., spouse eats F&Vs together with his pregnant partner) or a hindering environment that discourages prenatal F&V behavior change (i.e., spouse/partner consumes junk food while his partner struggles to consume F&Vs). Thus, the HAPA identifies key areas in the adoption and maintenance of health behaviors (i.e., intentions, coping planning, and action planning) 17, 18, which have typically been ignored in prenatal nutrition behavior change interventions.
Previous research has documented the need for culturally appropriate prenatal F&V interventions among low-income pregnant Latinas. Low-income pregnant Latinas are at increased risk of suboptimal F&V intake, consuming median daily servings intakes of F&Vs of 1.3 and 2.0 respectively.19 Additionally, birth outcomes are poorer among some Latina subgroups such as Puerto Rican Latinas, compared to non-Latina whites 20, 21, indicating a need to address nutrition-related factors during pregnancy.
This study is one of the first to utilize the HAPA model to develop a conceptually sound behavioral change model to serve as a foundation for culturally appropriate interventions to improve prenatal F&V intake among low-income, WIC eligible Latinas. Given that the HAPA model has not been used before in prenatal nutrition, a qualitative approach can effectively identify: a) both previously documented as well as new emerging factors that facilitate F&V behavior change among this population, and b) action/coping planning strategies that can lead to the adoption and maintenance of behaviors that increase prenatal F&V intake. Identifying factors that facilitate behavior change among this population is key for developing effective interventions to improve prenatal F&V intake among low-income Latinas.
METHODS
STUDY DESIGN
Data were analyzed from forty-five in-depth interviews collected as part of a larger study conducted to design an intervention to increase F&V intake among WIC eligible pregnant Latinas living within Hartford county, Connecticut. Three phases comprised this larger study: focus groups (phase 1), prenatal maternal survey (phase 2), and taste testings (phase 3). Women enrolled in phase 2 of the study completed a maternal prenatal baseline survey and were invited to participate in a follow-up prenatal assessment, the latter of which included the in-depth interview. The HAPA model guided the data collection and data analysis for this study, leading to the development of a conceptually sound behavior change model based on the HAPA framework. The HAPA framework is a solid model to guide this project since it helps identify what is needed to move individuals from intentions to behaviors through action coping and planning.
PARTICIPANTS AND RECRUITMENT
A convenience sample of participants who met the study’s specific inclusion criteria for phase 2 were recruited. This sampling approach was needed because the resources needed to conduct probabilistic sampling were not available for this study. However all mothers participating in the maternal survey (phase 2) were invited to participate in this qualitative study. Recruitment occurred from August 2013 thru August 2014 at the Women’s Ambulatory Health Services (WAHS) clinic at Hartford Hospital, a local hospital within Hartford which serves some of the poorest residents in the state. Women were invited to participate if they were: a) ≥ 18 years old; b) in 2nd or 3rd trimester; c) WIC eligible; d) Latina; e) with a singleton pregnancy; f) overweight or obese (i.e., pregravid body mass index ≥ 25); g) not on a restricted diet; h) nonsmokers. Of the 130 eligible women who were recruited for phase 2, 74 women completed the initial maternal prenatal assessment in English or Spanish (33 English, 41 Spanish), and 45 completed the second prenatal assessment (20 English, 25 Spanish), including the in-depth interview. The vast majority of women (93%) who did not participate in the second prenatal assessment had declined participation, while the rest were unable to be located.
The IRBs of Yale University and Hartford Hospital reviewed and approved the study. The Hispanic Health Council delegated IRB approval to both Yale University and Hartford Hospital.
PROCEDURES
Women meeting eligibility criteria were approached during their WAHS clinic or Centering Pregnancy session (i.e., group prenatal care sessions) by a trained bilingual (English/Spanish), bicultural recruiter/interviewer who explained the study in a private, confidential setting. Those that agreed to participate in the maternal baseline survey were scheduled to complete a single 24-hour recall and a quantitative survey in their language of choice, in the privacy of their home or the Hispanic Health Council, a local nonprofit community agency. All 74 participants were invited to participate in a follow-up visit consisting of a second 24-hour recall and an in-depth qualitative interview. Forty-five participants completed this follow-up visit an average of 3 weeks after completing the maternal prenatal baseline survey. All in-depth interviews were audio-taped and lasted between 12 and 63 minutes (26 minutes on average). Participants received $35 and $20 for participation in the initial and follow-up visits, respectively.
Prior to the start of the study, the bilingual/bicultural recruiters/interviewers were extensively trained by seasoned community nutritionists (AHF, ABM, and SSP) to conduct and administer all study components in both English and Spanish, including recruiting, consenting, and interviewing (i.e., the survey, 24-hour recall, and in-depth interview). To avoid potential bias, recruiters rotated recruitment days and did not recruit or interview eligible study participants that they previously knew.
INSTRUMENTS
Baseline Quantitative Survey
A quantitative survey administered at baseline collected the following maternal data: demographics, socioeconomic status; food assistance participation; food security; F&V purchasing and intake patterns; weight gain; and psychosocial constructs of F&V intake including risk perception, outcome expectancies, self-efficacy, intentions, action planning, and coping planning.
In-depth Interview
The initial in-depth interview guide was designed to assess the eight HAPA constructs of intentions, task self-efficacy, maintenance self-efficacy, recovery self-efficacy, risk perception, outcome expectancies, action planning, and coping planning. Based on feedback from a behavior change researcher with expertise in the HAPA model (JM), revisions were made to the guide resulting in: a) the combining of the three types of self-efficacy to assess general self-efficacy to prevent questions from sounding repetitious; b) having four questions that assessed action planning and coping planning constructs as well as identified actual action planning and coping planning strategies that could inform a prenatal F&V intervention; c) having two questions assessing risk perception to help identify both barriers and perceive threat of not eating F&Vs.
The in-depth interview guide underwent two rounds of pretesting: a) within a focus group setting with 5 Latina staff who provide services to low-income pregnant Latinas at the HHC and b) with 4 other Latina HHC staff members. Pretesting of the in-depth interview guide demonstrated that motivation and social support were important factors related to prenatal F&V intake within the target population, thus two questions were added to the in-depth interview to assess these two constructs. The final in-depth interview questions reflected six HAPA constructs representing intentions, self-efficacy, risk perception, outcome expectancies, action planning, and coping planning plus two additional supplement questions assessing motivation and social support (see Table).
Table.
In-depth Interview Questions Guided by Six HAPA Constructs as well as Motivation, and Social Support.
| HAPA constructs | Interview questions |
|---|---|
| Intentions | Now that you are pregnant, would you like to eat more fruits and vegetables each day? Why? |
| Self-efficacy | Now that you are pregnant, do you feel you have the ability (i.e. will be able) to eat more fruit and vegetables during pregnancy? Why? |
| Risk perception |
|
| Outcome expectancies | Now that you are pregnant, what do you think will happen if you do not eat more fruits and vegetables during pregnancy? |
| Action planning |
|
| Coping planning | Now, imagine you stopped eating fruits and vegetables during a particular month in your pregnancy… |
|
|
| Motivation | Now that you are pregnant, what strategies would help motivate you to eat more fruits and vegetables during your pregnancy? |
| Social support | Can you share with me what support you receive (from family and friends) to help you eat more fruits and vegetables during your pregnancy? |
DATA ANALYSIS
Audiotapes were transcribed and, if in Spanish, translated by a reliable and accurate transcription/translation service previously used for multiple qualitative projects. Once data collection was completed, the first 10 transcripts were independently read and coded by two of the authors (AHF and RPE) to standardize coding of salient domains, themes, and subthemes that emerged from the group as a whole. Both are experienced mixed-methods nutrition researchers with extensive prior training in conducting qualitative analyses. After meeting and reaching consensus on the domains, themes, and subthemes that emerged from the first 10 transcripts, AHF and RPE independently read and coded the remaining transcripts. During that time, AHF and RPE met through six face-to-face sessions to standardize and finalize their coding of domains, themes, and subthemes against each other for the remaining transcripts. There was agreement between AHF and RPE for the majority of the domains, themes, and subthemes, but a consensus process was used to reach convergence when there was not agreement. The code manual was finalized when saturation was achieved and consensus on all domains, themes, and subthemes between coders was reached. Saturation was considered reached when no new domains, themes, and subthemes emerged from the transcripts. Saturation was reached after approximately half of the interviews had been coded. Lastly, AHF and RPE independently identified the quotes best illustrating each theme and subtheme, and a final meeting was held to reach agreement on them and the final behavior change model representing the findings.
RESULTS
PARTICIPANT CHARACTERISTICS
Women were an average of 24.5 years old and an average of 19 weeks gestation at recruitment. Over 46% were of Puerto Rican descent and 66.6% were bilingual. Women had lived in the U.S. for an average of 14.5 years, with 38% being born in the U.S. Almost 22% worked and 51% had at least a high school education. Over 59% lived with a partner and for 24.4%, this was their first baby. Almost 78% were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), while only 69% were enrolled in the Supplemental Nutrition Assistance Program (SNAP).
DOMAINS
Ten domains were identified as direct or indirect factors influencing prenatal F&V intake: i) social support, ii) family structure, iii) F&V access, iv) F&V preferences, v) F&V knowledge, vi) F&V health outcome expectations, vii) self-efficacy, viii) intentions, ix) F&V action/coping planning strategies, and x) maternal health status.
Social support
Social support was the principal factor driving prenatal F&V intake. Social support was provided primarily by friends/family. For women, family/friends (identified as partners, mothers/fathers, grandmothers, in-laws, sisters/brothers, aunts/uncles, and children) were critical to the introduction to various F&Vs, adoption/reinforcement of F&Vs, and maintenance of F&V intake prenatally. Family/friends supplied a range of social support, including instrumental (e.g., financial), information, emotional, and psychological, empowering women to initiate or return to eating F&Vs prenatally.
“Support of the family [to start eating fruits and vegetables again], I think. If I have a good family, as I have, I think it is the best thing to do. Call my mom or call someone. “Can you help me?” …There’s some ways so, “I want to start again. Can you come and help me? Can you give me a supper to try to begin everything again?” And I know if that happened, I will have them help me. My mom, my sisters. I’m not going to say my father because he doesn’t cook. He only eats. But he’ll be on my side. He’ll tell me to eat because there’s a little person growing inside of you. So you have to do it.” (ID111, p.8)1
Providers and food assistance programs were additional support systems, predominantly providing informational and/or instrumental F&V support. Providers and WIC nutritionists were sources for nutrition education.
“And they (WIC) give you little brochures and like menus of tips of things that you can eat, they give you pamphlets and stuff…vegetables and fruits, she shows you pictures and she says that you’ve got to have like five food groups a day. And she will explain to you and show you pictures…I was just looking at the picture like – I didn’t even have a clue. And then I learned, so now I know what to do, what to eat.” (ID122, p.6)
WIC and SNAP benefits provided women with instrumental support. The monetary assistance from these programs provided women with more F&V purchasing power.
“…the programs that support me is WIC and my food stamps. Especially the WIC because it has fruits and vegetables on the check…I still buy fruits and vegetables [with food stamps] but it’s like with food stamps, I could buy something else if I want. Like the WIC helps me stay on track more because I don’t want to waste a check. I don’t want to waste the fruits and vegetables. So I want to take advantage of it. So I just get it and stuff. But I get fruits with my food stamps and stuff too.” (ID144, p.3)
Family Structure
Family structure directly influenced the type of familial support women received. Lack of family or feeling alone/lonely discouraged women from cooking and eating healthy, affecting F&V intake. In the absence of other familial support, children in the household had a pronounced impact on maternal eating patterns. Women placed the food needs and wants of their children above their own, often reducing the quality and/or quantity of their own diets to satisfy their children’s dietary preferences. Thus, having fussy children meant that women were less likely to cook vegetables to avoid having to throw out uneaten food.
“No, like I’m saying for my kids’ pregnancy. It was more like supported and you know? I’ll cook, more people will eat. It was different. Now these kids are so picky, they are so picky. The only one that will eat is like my daughter and that’s it. Yeah, sometimes I – like yesterday was a day that I was like, I’m not gonna cook. I have certain things to cook so I’m like I’m not gonna cook so they can throw it out. You know I just make sure they ate and I didn’t even bother to eat, myself…” (ID115, p.4)
F&V Access
Prenatal F&V access was affected by the physical environment, the material environment, and seasonality. The physical environment, comprised of the built environment, transportation, and work environment, posed challenges to accessing F&Vs. Neighborhoods within XX lacked local, easily accessible supermarkets, while local convenience stores within walking distance did not offer a variety of fresh F&Vs. Thus, transportation was crucial for women when accessing fresh F&Vs within XX. Women expressed frustration with local public transportation, instead relying on friends/family for rides to local supermarkets.
“Sometimes it’s difficult to get [F&V’s], because there’s no transportation. So me walking being this pregnant it’s kind of hard. So sometimes, like getting to places is difficult, because I don’t like always going to – to just corner stores. I like to go to a supermarket. But I mean, I can get there, I just got to wait for when it’s convenient for someone to take me, which is hard.” (ID122, pg. 9)
Economic access was identified as a barrier influencing women’s perception of F&V accessibility. Women felt F&Vs were expensive, which determined the type and quantity of F&Vs purchased. Food budgets depended on available income and receipt of WIC/SNAP benefits, which often allowed women more access to F&Vs at the beginning of each month. Since F&Vs tended to run out towards the end of the month, women were more likely to purchase cheaper, less expensive foods as well as fewer F&Vs throughout the month to stretch their available food benefits.
“…sometimes I find that I eat better when I first get my food stamps than I do – grocery shopping, I can buy my fruits, I can buy my vegetables. But then, when it finishes, I won't eat good again until next month because I can't buy fruits and vegetables fresh all the time.” (ID115, p.5)
However, not all women agreed and for some, economic access was not a barrier influencing prenatal F&V intake.
“I have more than enough access. If I don't have access home, I have access on my mom's, I have access as my sister's – everywhere and anywhere I go. I have an uncle who works at a fruit market so if I don't have access to buy them, he brings a lot of fruits home so there's times where my mom calls me and it's like okay, there's fruits here…” (ID101, p.7)
Lastly, seasonal variations limited access to favorite F&Vs, discouraging women from accessing and subsequently eating F&Vs at times.
“…. Like the watermelon? There aren’t any because the weather is still too slow. I’m waiting for the big watermelon. That would be one of the things that would prevent me from [eating], not being able to find them.” (ID139, p.3)
F&V Preferences
Taste/smell, freshness, and appearance of F&Vs as well as cultural preferences for specific F&Vs were influential in determining F&V preferences. Taste/smell impacted consumption, with unpleasant tastes/distinct smells discouraging F&V intake. In turn, taste/smell was reflected in cravings, fruit preferences, and junk food/fried food preferences. The juicy, fresh taste/smell of fruits overshadowed taste for vegetables, while junk food/fried foods were preferable to any F&Vs taste. Women were aware that their prenatal F&V intake transmitted flavors in utero, affecting infant taste/smell and the subsequent F&V preferences of the offspring.
“…when they reach a certain, certain type, certain weeks or certain trimester…the baby can taste what you’re eating, or they can smell what you’re cooking. So if I’m constantly eating that, then there’s a chance that my baby is gonna want nuggets and fries all the time instead of fruits and veggies and, and stuff like that.” (ID124, p.13)
Fresh F&Vs meant uncanned, safe produce. Spoiled F&Vs were avoided and F&Vs were washed to reduce pesticides and contamination from handling. F&Vs that looked “weird” or unappetizing were not consumed.
“Like I think if they’re fresh not rotten like most stores sell, they usually have rotten stuff or even on TV how they say that the gardeners put some type of peroxide for to kill the little animals. Sometimes, I’m scared to eat vegetables, and that’s the reason why. Is it safe to eat this? Is it not safe to eat it?” (ID134, p.9)
Cultural preferences limited women’s desire to eat unfamiliar F&Vs from different cultures.
“I mean people are picky… Like they're so used to eating things from their culture that they won't go outside the box...” (ID155, p.14)
F&V Knowledge
Women demonstrated informational knowledge about the health benefits for a mom and/or her unborn baby. F&Vs were generally regarded as healthy/nutritious, with some women understanding basic biological benefits of particular F&Vs:
“Orange provides the body with vitamin C. Carrot, I think vitamin A, for the eyes.” (ID149, p.1)
Instrumental knowledge, including hands-on learning about F&V cooking/recipes and using technology, was primarily provided by supportive friends/family. The knowledge learned served to empower the women and encourage them to cook on their own.
“Well, I’m more confident now that since my boyfriend is the recipe guy, he’s telling me that he’s giving me ideas to do it myself and not him all the time.” (ID134, p.7)
F&V Health Outcome Expectancies
Women described anticipated health outcomes for themselves, their unborn baby, and both together based on increasing or reducing F&V intake. Increasing prenatal intake of F&Vs was believed to improve maternal health by: i) controlling gestational weight gain, gestational diabetes, satiety, and being nutritious, ii) preventing pregnancy complications, iii) improving energy levels, and iv) preventing obesity/chronic disease. For women, F&Vs enhanced satiety and discouraged overeating, subsequently helping control gestational weight gain and prevent pregnancy complications. Women felt weak, sluggish, and less energized when reducing or stopping F&V consumption. Women identified maternal F&V intake as vital to preventing chronic diseases including diabetes, high cholesterol, and obesity.
“…it's gonna get to a point where I'm not gonna be a healthy person anymore. I'm gonna walk around always who knows, with asthma, diabetes, high cholesterol…and I'll be like oh my God, what did I do to myself? Because I did it to myself, nobody else did it to myself. So yeah, I do sit here and be like if I don't eat healthy and I'm constantly eating this junk food, what's gonna happen to me? I know in the long run, all that junk food affects you somehow.” (ID101, p.8)
Women felt poor prenatal F&V intake caused suboptimal fetal growth and brain development, subsequently leading to birth defects, poorer immune system (i.e. lower defenses), and smaller infants at birth. Most women also understood that F&Vs provided nutrients to both mother and fetus, thus linking maternal and fetal health outcomes during pregnancy.
If you’re not eating [fruits and vegetables], the baby won’t be healthy.” (ID121, p.1)
Self-Efficacy
Self-efficacy, the belief in one’s ability to complete a task or reach a goal (i.e., eat more F&Vs) improved when women: i) were already consuming and enjoying F&Vs; ii) felt they could improve health outcomes for themselves and their infant; and iii) were able to make the choice to eat F&Vs.
“I have never been one month without eating fruits, I don’t think I could. If one day I have not eaten any fruits or vegetables I feel the need to eat it, so I think that after a month my body would feel strange. I would have to return to the habit of eating fruits.” (ID116, p.3)
Intentions
According to Schwarzer et al., “intentions comprise a person’s motivation towards a goal or target behavior in terms of direction and intensity”.22 Internal/external motivation was shown to influence prenatal F&V intake. Some women felt that changing F&V eating behaviors had to be generated internally within themselves; outside sources couldn’t influence their intentions to increase F&V intake as strongly as internal motivation.
“If I'm motivated, I'm motivated because of myself, because that's what I want, not motivated by someone else or anything else. I won't, I won't eat it [F&Vs]. I won't even try it.” (ID101, p.2)
Others required external motivation from family/friends/coworkers to help them try to change F&V intake behavior.
“Here at home we eat fruit. My husband likes fruit very much and he motivates me to eat fruit. My children also like fruit very much.” (ID130, p.2)
F&V Action/Coping Planning Strategies
Fourteen action planning/coping planning behavioral strategies emerged as methods women felt helped them to improve prenatal F&V intake: i) goal setting; ii) self-monitoring; iii) experimenting with new F&Vs; iv) changing the home environment; v) family shared meals/home cooking; vi) changing food purchasing/preparation patterns; vii) self-remind/self-motivation; viii) forcing self; ix) role-modeling; x) decreasing junk food to increase F&V intake; xi) cooking/recipes; xii) masking F&V flavors/F&V blends; xiii) healthy snacking/healthy meals; and xiv) making F&Vs more convenient to eat.
Masking undesired F&V flavors emerged as the primary strategy used. Women understood the importance of consuming F&Vs, thus they had experimented with methods such as blending F&Vs in smoothies or “hiding” vegetables in different foods. Family/friends were relied on to implement these methods, especially with undesired F&Vs.
“…like if you don’t like tomatoes, you can blend it and add something else with it to make you – you know even if you could drink it, but you need to eat the fruits and vegetables. So I don’t know, maybe a blender is a good strategy? Or sneak it in your food, I don’t know…That helped me eat a lot more vegetables, because I kind of don’t like a lot of vegetables.” (ID122, p.2)
Maternal Health Status
Some women modified their F&V intake during pregnancy to reduce their risk of pregnancy complications. Those who experienced pregnancy complications, including gaining excessive weight during pregnancy or gestational diabetes/prenatal stress, modified their F&V intake during pregnancy to improve their health status. For example, women diagnosed with gestational diabetes later during pregnancy limited fruit intake to avoid blood sugar fluctuations.
“If it wasn’t for that [having gestational diabetes], I will eat more. I, I feel like that’s kind of stopping me from eating them. Ever since I found out that I was diabetic, I kinda stopped eating more the fruits. Not the veggies, but more the fruits.” (ID102, p.5–6)
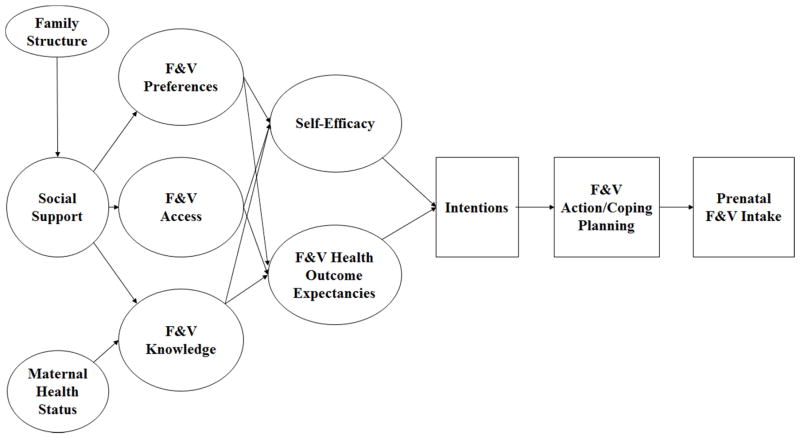
F&V CONCEPTUAL MODEL
The conceptual model that emerged from the in-depth qualitative analysis adapts and expands on the HAPA model to include distal factors deemed important to improve F&V intake among pregnant WIC eligible Latinas. First, self-efficacy, intentions, F&V health outcome expectancies, and action/coping planning strategies link to reflect the two stages of the HAPA model, the motivational and volitional phases. In the motivational phase of the HAPA model, F&V health outcomes expectancies (i.e., the health outcomes women expect for themselves and their babies if they don’t eat F&Vs during pregnancy) help a woman to weigh the pros and cons of consuming more F&Vs during pregnancy.17 According to the HAPA model, women contemplate their outcome expectancies and then consider whether they have the ability (or perceived self-efficacy) to take action (e.g., adherence to eating F&Vs during pregnancy even with cravings for junk food). 17 Both perceived self-efficacy and F&V health outcomes expectancies help a pregnant woman form an intention to adopt the behavior of increasing prenatal F&V intake. In the volitional phase, the intention to change F&V intake becomes transformed into action plans (which tell when, where, and how to increase F&V intake) and coping plans (i.e., planning how to cope with potential barriers that might hinder one from consuming more F&V during pregnancy). 17
Adapting and expanding on the HAPA model, F&V preferences, access, and knowledge each directly influence a woman’s perceived self-efficacy and F&V health outcome expectancies. Women that don’t like the taste of certain F&Vs are less likely to believe they have the ability to eat those F&Vs (reflecting poorer perceived self-efficacy) and don’t expect to eat more of those F&Vs during pregnancy (reflecting negative health outcome expectancies). Increasing F&V access as well as knowledge can increase a woman’s belief in her ability to eat more F&Vs during pregnancy and improve her expectation that she will eat more F&Vs during pregnancy.
This model posits that the distal factor of social support directly influences F&V preferences, access, and knowledge, subsequently influencing self-efficacy and F&V health outcomes expectancies, causing intentions to form, action and coping planning to develop, and generating action to improve prenatal F&V intake among Latinas. Two pre-existing factors, family structure and maternal health status, influence social support and F&V knowledge respectively.
DISCUSSION
This study strongly indicates the need to strengthen social support among pregnant WIC eligible Latinas to empower them to gain the access, confidence, knowledge, and strategies they need to consume more F&V. Study findings showed that, overall, social support was the primary distal factor driving prenatal F&V behavior change. Family/friends were the primary source, providing emotional, psychological, instrumental and informational F&V support. These findings are consistent with studies showing that familial social support encourages healthier eating among pregnant Latinas.23–25 High spousal social support improved vegetable intake among pregnant Latinas 24, and encouraged optimal health behaviors, including a healthy diet, among low-income pregnant/postpartum Latinas.23 Similarly, pregnant adolescent Latinas were found to have good eating habits if they had a family support system that provided care, attention, and buffered them from life stressors.25 While the presence of one or more sources of familial support encouraged more prenatal F&V intake, prenatal F&V intake faltered when support was absent. Thornton et al. also found that women adopted healthier eating habits if their husbands’ provided instrumental support, such as eating together, while lack of support inhibited them from eating healthier.23 In this study, the absence of familial support signified a lack of a cohesive family structure. In the absence of familial support, women felt isolated, lonely, and subsequently disinterested in cooking or eating healthy. Studies have documented similar findings that lack of family support, specifically from females, inhibited Latinas from receiving prenatal/postpartum food-related advice, participating in food-related activities, and subsequently feeling isolated.23 Thus, a solid support system, led by a cohesive family structure, is an important element for promoting and improving prenatal F&V intake among Latinas. In the absence of a solid family structure and familial support, available support systems must be strengthened to provide a supportive environment for improving prenatal F&V intake among Latinas.
Studies conducted with non-Latina pregnant populations suggest that social support plays an important role in establishing an environment that promotes or inhibits the adoption of healthier prenatal eating behaviors. Qualitative studies conducted among pregnant African American populations infer that family and friends can create a challenging environment for those women who want to improve their prenatal eating behaviors.26, 27 Pregnant African American women in these studies felt discouraged by social pressure to eat “for two” and by having little control over food cooked at home, thus feeling as though they had to rely on themselves to make appropriate prenatal food choices or change prenatal eating behaviors. 26, 27 Other studies conducted with predominately Caucasian or Asian pregnant women suggest that family, friends and the community contribute to a supportive prenatal environment that promotes healthy prenatal food choices and encourages behavior change. 28, 29
With that in mind, social support can influence other key factors affecting prenatal FV intake. First, social support can influence F&V access, knowledge, and preferences. First, improving F&V access increases the availability of F&Vs for consumption, but requires tackling physical and monetary barriers. With only 37% of convenience stores in Hartford accepting WIC checks and stocking an average of only 4.2 fruits and 6.1 vegetables, local F&V access is limited. 30 Study findings indeed suggest that social support, provided through family/friends as well as through food assistance programs, improves F&V access by helping women surmount the physical and monetary barriers, subsequently increasing their belief in their ability to improve their prenatal F&V intake as well as change the F&V health outcomes expectancies they have for themselves.
Social support can also improve knowledge, which in turn can lead to improved self-efficacy and planning strategies to encourage behavior change. Keiffer et al. 31 showed that a community health worker-led intervention to increase knowledge and skills about healthy eating, exercise, and managing stress improved dietary practices, including increasing vegetable consumption, among pregnant Latinas. Study findings suggest that knowledge can affect prenatal F&V intake behavior in two ways. First, F&V knowledge can improve self-efficacy directly, by improving women’s belief in their ability to eat more F&Vs and adopt effective action/coping planning behavioral strategies. Secondly, improving F&V knowledge can change F&V health outcome expectancies women have for themselves and their baby, subsequently promoting more effective action/coping planning behavioral strategies.
Finally, social support can directly influence F&V preferences. Study findings show that family/friends are key sources for instrumental (i.e., cooking; bringing fresh F&Vs) and informational F&V support (i.e., providing recipes, teaching cooking skills; educate on choosing fresh F&Vs). Since prenatal F&V intake was found to be strongly influenced by taste/smell, appearance, freshness, and cultural preferences, which is consistent with the literature on F&V sensory factors,32 any positive social support that helps mothers enhance the sensory properties of their F&V (i.e., taste/smell, appearance, and freshness) may lead to improved prenatal F&V intake. In a small pilot study among pregnant adolescents, Symon and Wriden demonstrated that support and instrumental education offered through group cooking classes influenced the acceptability and home dietary habits of the participating teens.33
An established support system that provides a strong, encouraging environment can promote optimal F&V intake behavior change by indirectly promoting self-efficacy, especially perceived self-efficacy. Perceived self-efficacy, an underlying HAPA construct, is the belief an individual has in her/his ability to perform a specific action.17 Perceived self-efficacy works together with positive health outcome expectancies to help form the intention to adopt a desired behavior.17 Positive health outcome expectancies and positive perceived self-efficacy lead to the adoption of F&V intentions. Essentially, women who recognized the positive impact improving prenatal F&V intake had on their health and their unborn baby’s health, felt they had more ability to eat more F&Vs during pregnancy, and the intention of changing prenatal F&V intake occurs.
According to the HAPA, once an intention is formed, the process of performing the desired behavior requires identifying action and coping planning behaviors and strategies to aid in changing behavior.17 Fourteen action/coping planning strategies that women used or felt they could adopt to increase prenatal F&V intake were identified. Strategies, such as masking the taste of F&Vs, can make F&Vs more palatable and increase maternal prenatal F&V intake.
In this study, F&V knowledge was influenced by maternal health status. Studies show that significant life events, such as a poor health diagnosis, encourages one to seek knowledge to help change behavior to address a health issue.34 Women experiencing pregnancy complications or excessive gestational weight in this study were more likely to seek out and receive prenatal nutrition education to empower them to modify their behavior to better stabilize their health status during pregnancy. Others tried to reduce the risk of pregnancy complications by modifying their prenatal F&V intake, but may have benefited from additional F&V knowledge to help change behavior if it had been provided.
This study had several strengths. The sample size of forty-five in-depth interviews led to saturation of themes and confirmation that all themes had been extensively covered in the discussion among the two coders. The use of HAPA as the foundation for the in-depth interview questions is novel, especially among pregnant Latinas. Findings support HAPA as a solid conceptual framework to use for identifying promising strategies to improve F&V intake among Latinas.
This study had some limitations. Within the conceptual model, risk perception, a HAPA construct, could not be included since there was no evidence of perception of risk for consuming F&V in this study. This study also did not gather data on maintenance and recovery self-efficacy, allowing us to include only perceived self-efficacy within the motivational phase of the conceptual model. Other studies have also adapted the HAPA model to suit the specific behavior and population under investigation. 35, 36 Overall, however study findings do indicate that the adapted HAPA model does help explain F&V intake in the target population and can serve as a basis for developing sound interventions. Another study limitation is that causal inferences cannot be drawn from qualitative studies. However the goal of this study, which was met, was to inform the development of an intervention package that can be subsequently tested in the target population through a randomized trial design.
In conclusion, this study is novel in its approach to utilize the HAPA model to: a) qualitatively identify barriers and facilitators to prenatal F&V intake and b) inform a conceptual behavior change model to improve prenatal F&V intake behavior among WIC eligible pregnant Latinas. Study findings suggest that changing prenatal F&V intake is a complex, multifactorial process and that the HAPA model alone is not enough, although it does help understand how to improve prenatal F&V intake among Latinas. The adapted HAPA model indeed provides a working framework that serves as the foundation for an intervention designed to encourage F&V behavior change among pregnant WIC eligible Latinas. By enhancing perceived self-efficacy (e.g., I have the ability to eat more F&Vs during pregnancy even when there is junk food available) and F&V health outcomes expectations (e.g., I know that myself and my baby may not be healthy if I don’t eat F&V during pregnancy), intentions develop (e.g., I intend to begin making changes to eat more F&Vs during pregnancy), which then translate into action planning strategies (e.g., I know when to eat F&Vs, I know where to eat F&Vs, I know how to eat F&Vs) and coping planning strategies (e.g., If I don’t have F&Vs to eat in the house, I will go out and buy them right away) to help pregnant WIC eligible Latinas act to improve prenatal F&V intake. Yet, distal factors that influence maternal perceived self-efficacy and F&V health outcome expectancies must also be considered as potential intervention points. Therefore, this model will provide the framework for an intervention that enhances social support, promotes F&V access, modifies F&V preferences, and improves F&V knowledge, to empower pregnant WIC eligible Latinas, through improved self-efficacy and F&V health outcome expectancies, to change prenatal F&V intake.
IMPLICATIONS FOR RESEARCH AND PRACTICE
Pregnancy is a “teachable moment” ; a life event when women become highly motivated to change risky behavior.14 Study findings demonstrate that changing prenatal F&V behavior is a dynamic process influenced by several factors. Understanding these factors and the links among them can lead to designing culturally appropriate prenatal dietary interventions that will effectively promote F&V intake. Since improved F&V intake has undeniable benefits for the mother and her unborn baby, identifying effective methods to change prenatal F&V intake behavior is ideal and can have a lasting impact on the health of WIC eligible pregnant Latinas and their unborn infants. This study strongly indicates the need to strengthen social support in such prenatal F&V interventions. Health care professionals working with pregnant WIC eligible Latinas are a valuable support source as well as resource for these women. Providers must take into account the fact that not only improved knowledge but also improved access and meeting the community’s F&V preferences are key for increasing the motivation and self-efficacy towards consumption of F&V in the target population. By addressing factors influencing prenatal F&V intake, providers can help pregnant WIC eligible Latinas through the process of changing F&V behavior.
Supplementary Material
Figure.
Adapted and expanded HAPA behavior change model depicting the web of factors influencing prenatal F&V intake among WIC eligible Latinas. Distal factors of social support, F&V preferences, knowledge, access influence HAPA motivational phase constructs of perceived self-efficacy and F&V health outcome expectations. As the primary distal factor, social support includes informational and instrumental support from friends, family and providers as well as material support from food assistance and other social programs. Perceived self-efficacy and F&V health outcome expectations both influence the formation/adoption of intentions to improve F&V intake. Once intentions are adopted, action planning and coping planning strategies are initiated, leading to action of changing prenatal F&V intake behavior.
Acknowledgments
The authors would like to deeply thank the staff and health care providers from the WAHS clinic at Hartford Hospital as well as the staff from the Center for Community Nutrition at the Hispanic Health Council for their unwavering support and assistance in implementing this study. Special thanks is extended to Dr. Angela Bermudez-Millan for her assistance with several aspects of study implementation. This study was funded by a grant from the National Institutes of Health/National Institute for Nursing Research to Amber Hromi-Fiedler (Grant number: 1R21NR013970).
Footnotes
The participant’s study ID number and the page number where the quote appears in the transcript are included for each quote.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007;21:717–728. doi: 10.1038/sj.jhh.1002212. [DOI] [PubMed] [Google Scholar]
- 2.He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet. 2006;367:320–326. doi: 10.1016/S0140-6736(06)68069-0. [DOI] [PubMed] [Google Scholar]
- 3.Seyedrezazadeh E, Moghaddam MP, Ansarin K, Vafa MR, Sharma S, Kolahdooz F. Fruit and vegetable intake and risk of wheezing and asthma: a systematic review and meta-analysis. Nutr Rev. 2014;72:411–428. doi: 10.1111/nure.12121. [DOI] [PubMed] [Google Scholar]
- 4.Dietary Guidelines Advisory Committee. [Accessed on: May 11, 2015];Scientific report of the 2015 Dietary Guidelines Advisory Committee. 2015 Available at: http://www.health.gov/dietaryguidelines/2015-scientific-report/
- 5.Healthy Americas Institute. [Accessed on: November 4, 2015];Healthy Americas Survey. 2014 Available at: http://www.healthyamericasinstitute.org/healthy-americas-2014.html.
- 6.King JC. Maternal obesity, metabolism, and pregnancy outcomes. Annu Rev Nutr. 2006;26:271–291. doi: 10.1146/annurev.nutr.24.012003.132249. [DOI] [PubMed] [Google Scholar]
- 7.Martin CL, Sotres-Alvarez D, Siega-Riz AM. Maternal Dietary Patterns during the Second Trimester Are Associated with Preterm Birth. J Nutr. 2015;145:1857–1864. doi: 10.3945/jn.115.212019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maconochie N, Doyle P, Prior S, Simmons R. Risk factors for first trimester miscarriage--results from a UK-population-based case-control study. BJOG. 2007;114:170–186. doi: 10.1111/j.1471-0528.2006.01193.x. [DOI] [PubMed] [Google Scholar]
- 9.Endeshaw M, Abebe F, Bedimo M, Asart A. Diet and Pre-eclampsia: A Prospective Multicentre Case-Control Study in Ethiopia. Midwifery. 2015;31:617–624. doi: 10.1016/j.midw.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Longo-Mbenza B, Kadima-Tshimanga B, Buassa-bu-Tsumbu B, M'Buyamba K., Jr Diets rich in vegetables and physical activity are associated with a decreased risk of pregnancy induced hypertension among rural women from Kimpese, DR Congo. Niger J Med. 2008;17:45–49. [PubMed] [Google Scholar]
- 11.Li L, Werler MM. Fruit and vegetable intake and risk of upper respiratory tract infection in pregnant women. Public Health Nutr. 2010;13:276–282. doi: 10.1017/S1368980009990590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bao W, Bowers K, Tobias DK, et al. Prepregnancy low-carbohydrate dietary pattern and risk of gestational diabetes mellitus: a prospective cohort study. Am J Clin Nutr. 2014;99:1378–1384. doi: 10.3945/ajcn.113.082966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy MM, Stettler N, Smith KM, Reiss R. Associations of consumption of fruits and vegetables during pregnancy with infant birth weight or small for gestational age births: a systematic review of the literature. Int J Womens Health. 2014;6:899–912. doi: 10.2147/IJWH.S67130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phelan S. Pregnancy: a "teachable moment" for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202:135, e131–138. doi: 10.1016/j.ajog.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang MW, Nitzke S, Guilford E, Adair CH, Hazard DL. Motivators and barriers to healthful eating and physical activity among low-income overweight and obese mothers. J Am Diet Assoc. 2008;108:1023–1028. doi: 10.1016/j.jada.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Haynes-Maslow L, Parsons SE, Wheeler SB, Leone LA. A qualitative study of perceived barriers to fruit and vegetable consumption among low-income populations, North Carolina, 2011. Prev Chronic Dis. 2013;10:E34. doi: 10.5888/pcd10.120206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology. 2008;57:1–29. [Google Scholar]
- 18.Schwarzer R. How to overcome health compromising behaviors. European Psychologist. 2008;13:141–151. [Google Scholar]
- 19.Hromi-Fiedler A, Bermudez-Millan A, Segura-Perez S, Perez-Escamilla R. Nutrient and food intakes differ among Latina subgroups during pregnancy. Public Health Nutr. 2012;15:341–351. doi: 10.1017/S136898001100108X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fuentes-Afflick E, Lurie P. Low birth weight and Latino ethnicity. Examining the epidemiologic paradox. Arch Pediatr Adolesc Med. 1997;151:665–674. doi: 10.1001/archpedi.1997.02170440027005. [DOI] [PubMed] [Google Scholar]
- 21.Fuentes-Afflick E, Hessol NA, Perez-Stable EJ. Testing the epidemiologic paradox of low birth weight in Latinos. Arch Pediatr Adolesc Med. 1999;153:147–153. doi: 10.1001/archpedi.153.2.147. [DOI] [PubMed] [Google Scholar]
- 22.Schwarzer R, Sniehotta FF, Lippke S, et al. [Accessed on: February 16, 2016];On the assessment and analysis of variables in the Health Action Process Approach: Conducting an investigation. 2003 Available at: http://userpage.fu-berlin.de/gesund/hapa_web.pdf.
- 23.Thornton PL, Kieffer EC, Salabarria-Pena Y, et al. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: the role of social support. Matern Child Health J. 2006;10:95–104. doi: 10.1007/s10995-005-0025-3. [DOI] [PubMed] [Google Scholar]
- 24.Shah MK, Kieffer EC, Choi H, Schumann C, Heisler M. Mediators and Moderators of the Effectiveness of a Community Health Worker Intervention That Improved Dietary Outcomes in Pregnant Latino Women. Health Educ Behav. 2015 doi: 10.1177/1090198114568307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gutierrez YM. Cultural factors affecting diet and pregnancy outcome of Mexican American adolescents. J Adolesc Health. 1999;25:227–237. doi: 10.1016/s1054-139x(99)00016-6. [DOI] [PubMed] [Google Scholar]
- 26.Groth SW, Morrison-Beedy D. Low-income, pregnant, African American women's views on physical activity and diet. J Midwifery Womens Health. 2013;58:195–202. doi: 10.1111/j.1542-2011.2012.00203.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reyes NR, Klotz AA, Herring SJ. A qualitative study of motivators and barriers to healthy eating in pregnancy for low-income, overweight, African-American mothers. J Acad Nutr Diet. 2013;113:1175–1181. doi: 10.1016/j.jand.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higginbottom GM, Vallianatos H, Forgeron J, Gibbons D, Mamede F, Barolia R. Food choices and practices during pregnancy of immigrant women with high-risk pregnancies in Canada: a pilot study. BMC Pregnancy Childbirth. 2014;14:370. doi: 10.1186/s12884-014-0370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hui AL, Sevenhuysen G, Harvey D, Salamon E. Food choice decision-making by women with gestational diabetes. Can J Diabetes. 2014;38:26–31. doi: 10.1016/j.jcjd.2013.08.263. [DOI] [PubMed] [Google Scholar]
- 30.Martin KS, Havens E, Boyle KE, et al. If you stock it, will they buy it? Healthy food availability and customer purchasing behaviour within corner stores in Hartford, CT, USA. Public Health Nutr. 2012;15:1973–1978. doi: 10.1017/S1368980011003387. [DOI] [PubMed] [Google Scholar]
- 31.Kieffer EC, Welmerink DB, Sinco BR, et al. Dietary outcomes in a Spanish-language randomized controlled diabetes prevention trial with pregnant Latinas. Am J Public Health. 2014;104:526–533. doi: 10.2105/AJPH.2012.301122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pollard J, Kirk SF, Cade JE. Factors affecting food choice in relation to fruit and vegetable intake: a review. Nutr Res Rev. 2002;15:373–387. doi: 10.1079/NRR200244. [DOI] [PubMed] [Google Scholar]
- 33.Symon AG, Wrieden WL. A qualitative study of pregnant teenagers' perceptions of the acceptability of a nutritional education intervention. Midwifery. 2003;19:140–147. doi: 10.1016/s0266-6138(03)00004-4. [DOI] [PubMed] [Google Scholar]
- 34.Peacock AS, Bogossian FE, Wilkinson SA, Gibbons KS, Kim C, McIntyre HD. A Randomised Controlled Trial to Delay or Prevent Type 2 Diabetes after Gestational Diabetes: Walking for Exercise and Nutrition to Prevent Diabetes for You. Int J Endocrinol. 2015;2015:423717. doi: 10.1155/2015/423717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luszczynska A. Change in breast self-examination behavior: effects of intervention on enhancing self-efficacy. Int J Behav Med. 2004;11:95–103. doi: 10.1207/s15327558ijbm1102_5. [DOI] [PubMed] [Google Scholar]
- 36.Renner B, Kwon S, Yang BH, et al. Social-cognitive predictors of dietary behaviors in South Korean men and women. Int J Behav Med. 2008;15:4–13. doi: 10.1007/BF03003068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.