Abstract
The case presented advocates for prolonged resuscitation, and aggressive rewarming in neonates with severe hypothermia (core temperature <32.0°C). The importance of rewarming has not been extensively studied in current guidelines, whereas the importance of cardiopulmonary resuscitation is well established. This abandoned, severely hypothermic (found with temperature of 27.9°C) newborn had an excellent neurological outcome at two years of age with aggressive resuscitation and rewarming techniques initiated at the time of presentation. Active core rewarming with warm saline lavages, intravenous fluids and warm air may be used at a rate of 1.8°C/h to 5.3°C/h according to most guidelines. Rewarming guidelines for asphyxiated infants undergoing therapeutic hypothermic may not be applicable to infants with accidental exposure, as in the present case. The present case of a near-term severely hypothermic infant reinforces the current recommendation of continuing resuscitative measures, irrespective of response to resuscitation, until the infant has been rewarmed.
Keywords: Hypothermia, Neonatal hypothermia, Resuscitation guidelines
Abstract
Le cas présenté plaide en faveur d’une réanimation prolongée et d’un réchauffement agressif chez les nouveau-nés présentant une grave hypothermie (température centrale de moins de 32,0 °C). Les directives à jour ne contiennent pas d’étude approfondie sur l’importance du réchauffement, mais celle de la réanimation cardiorespiratoire est bien établie. Ce nouveau-né abandonné en hypothermie grave (température de 27,9 °C lorsqu’il a été trouvé) présentait d’excellents résultats neurologiques à l’âge de deux ans, alors que des techniques de réanimation et de réchauffement agressives avaient été adoptées au moment de la présentation. On peut procéder au réchauffement actif de la température centrale à l’aide de lavages de sérum physiologique tiède, de liquides intraveineux et d’air tiède, à un rythme de 1,8 °C/h à 5,3 °C/h selon la plupart des directives. Les directives sur le réchauffement des nourrissons asphyxiés qui subissent une hypothermie thérapeutique ne s’appliquent peut-être pas aux nourrissons exposés accidentellement aux éléments, comme dans le cas présent. Ce cas d’un nourrisson presque à terme en grave hypothermie renforce la recommandation actuelle de poursuivre les mesures de réanimation, quelle que soit la réponse, jusqu’à ce que le nourrisson soit réchauffé.
Neonatal hypothermia, defined as a core temperature <36.5°C by the WHO, is a relatively common event in the first days of life. Severe neonatal hypothermia, defined as a core temperature <32°C by the WHO, is rare (1,2). Although there are numerous case reports and short-series describing neonates who have developed severe hypothermia (3–6), there have been very few in recent history.
The present report describes an infant with severe neonatal hypothermia and a prolonged resuscitation. Despite the severity of hypothermia and extended duration of resuscitation, the infant has had a good long-term neurological outcome to date.
CASE PRESENTATION
A 36-week gestational age female neonate was born outdoors in a city square on a cold (−22°C) winter evening in Toronto, Ontario. History revealed that no antenatal care was provided. The abandoned newborn was found gasping, with a heart rate (HR) of 40 beats/min and was immediately brought to the emergency department. The infant was noted to be bradycardic and hypopneic, and had a rectal temperature of 27.9°C. The baby was intubated and cardiopulmonary resuscitation was initiated promptly.
The infant’s heart rate remained between 40 beats/min and 50 beats/min 8 min after arrival, when 0.1 mg of epinephrine (1:10,000) was given via an endotracheal tube (ETT). A second dose was given 2 min later by ETT, with no response in vital signs. Despite being under an overhead warmer, her rectal temperature remained at 28°C at 20 min. Her HR remained between 30 beats/min and 50 beats/min, and her respiratory effort was intermittent. Ambient temperature in the trauma room was increased to 28°C. Warm bags of saline were placed around the infant. An umbilical venous line was placed and two additional doses of epinephrine (1:10,000) and 4.2% sodium bicarbonate (5 mL) were given, respectively, with no appreciable effect. A ‘warmed’ normal saline bolus of 20 mL was given 30 min into the resuscitation and was repeated once. A dopamine infusion (10 µg/kg/min) was started 1 h into the resuscitation.
Her core temperature remained at 28°C to 29°C for the initial 1 h 25 min. Over the next 15 min, her rectal temperature rose from 28.7°C to 32.8°C. When her temperature rose to 32°C, her HR increased to >100 beats/min and spontaneous respirations began. Effective cardiac output was then noted. Chest compressions were discontinued after 1 h 30 min of resuscitation. At this point, she remained on full ventilation. An umbilical arterial line was placed at 2 h. The first blood gas revealed the following values: pH 7.22, partial pressue of carbon dioxide (PCO2) 19 mmHg, partial pressue of oxygen (PO2) 200 mmHg, bicarbonate 8 mEq/L and a base excess of −19 mEq/L. Her serum glucose level was 0.45 mmol/L before administration of multiple doses of 10% dextrose.
At 2 h, the infant’s rectal temperature was 34.1°C, with an HR of 144 beats/min and a blood pressure of 58/34 mmHg. She had a respiratory rate of 57 breaths/min and was breathing above the set ventilator rate, in 50% oxygen. The neurological examination revealed an active infant who moved all four limbs spontaneously and whose suck, gag and rooting reflexes were present. Her pupils were equal and reactive to light. Tone and power were normal and symmetrical, while primitive reflexes were present.
A blood culture was drawn and she was started on ampicillin and gentamicin. The infants weight was 2.116 kg. Repeat arterial blood gas at 3 h 20 min revealed a pH 7.33, PCO2 20 mmHg, PO2 223 mmHg, bicarbonate 11 mEq/L and a base excess −13 mEq/L. The infant received two additional doses of sodium bicarbonate.
A chest x-ray was normal. A complete blood count revealed a leukocyte count of 16.9/mm3 with no left shift, a hemoglobin level of 202 g/L and a platelet count of 186,000/µL. She developed a mild coagulopathy with thrombocytopenia and a prolonged international normalized ratio (INR). Her lowest platelet count was 65,000/µL and peak INR was 2.48. These all normalized spontaneously by three days of age. The dopamine infusion was discontinued by 12 h of age. Urine output was first noted at 24 h. Creatinine level at 24 h was 103 µmol/L and 57 µmol/L at four days.
The infant’s neurological examination remained normal following resuscitation. Magnetic resonance imaging (MRI) of the head performed on day 4 was normal. Visual evoked potentials were abnormal bilaterally on day 3 of age, and were absent five days later.
Follow-up MRI performed at seven months revealed mild enlargement of the lateral and third ventricles, with normal parenchyma while hearing and vision testing were normal. At 24 months of age, language and problem solving skills were assessed using validated screening tools (Reel-2, Ages & Stages Questionnaire) and were within normal limits.
DISCUSSION
Hypothermia, as defined by the WHO, is a body temperature below the normal range (36.5°C to 37.5°C) and is subclassified into three grades: mild (36.0°C to 36.5°C), moderate (32.0°C to 35.9°C) and severe (<32.0°C) (1,2). Neonates are at a particularly high risk for hypothermia given their limited ability to retain heat, with an increased surface area to weight ratio, limited fat stores and inability to shiver (4). A low birth weight neonate has decreased thermal insulation due to less subcutaneous and brown fat (7). Metabolism of brown fat is the source of heat production, and blood flow through brown fat becomes warm, which transfers heat throughout the body via the circulation (7). Hypothermia from exposure is associated with significant morbidity and mortality in neonates. A mortality rate of 5% to 18% has been reported in cases of severe hypothermia (8).
This neonate presented with multisystem effects of severe hypothermia including apnea and bradycardia (1). This persisted for an extended length of time despite full resuscitative efforts including intubation, chest compressions, multiple doses of epinephrine and bicarbonate, as well as dopamine. In infants with severe hypothermia, bradycardia as a result of hypothermia may interfere with the normal response to resuscitation, particularly when prolonged (1). It is important that persistent bradycardia is not interpreted as a failure of the infant to respond to the resuscitative efforts (9). It was only with the increase in core temperature to >32°C that spontaneous respirations, followed by an increase in HR, occurred.
The increase in core temperature of this neonate through external rewarming was 3.2°C/h. In other reported cases, the rate ranged from 1.8°C/h to 5.3°C/h (8,10). In severe hypothermia, active core rewarming with warm saline lavages, intravenous fluids and warm air may be used (8,10). These lavages could include irrigation of body cavities, such as gastric, colonic, bladder or thoracic, with heated saline. Rapid rewarming during resuscitation is a traditionally accepted method (8–11). There have been multiple reports of severely hypothermic infants with normal MRI findings with excellent outcomes following aggressive resuscitation and rewarming (3–6,12). This infant made a full recovery, even at 24 months of age.
The American Heart Association has made clear the importance of cardiopulmonary resuscitation (CPR) in hypothermia; however, the importance of rewarming during CPR has not been extensively studied in these guidelines (13). Current recommendations for ‘warming’ are focused on the preterm or very low birth weight (<1500 g) infant (13). Rewarming guidelines for asphyxiated infants undergoing therapeutic hypothermia is generally 0.5°C/h at most centres (14), although this rate may not be directly applicable to infants with accidental exposure. Because temperature monitoring is an important step, the present case shows how crucial rewarming of the neonate can be, especially during continued CPR.
Although guidelines regarding the relationship between prolonged CPR and temperature control are vague, the present case demonstrates its importance. CPR should continue even if there appears to be no response to resuscitation, which is exemplified in this case. Outcomes, however, are most likely dependent on the underlying etiology of the hypothermia (15). As of 2010, there are no reliable predictors of outcome to guide when to terminate resuscitative efforts in children. Clinical variables associated with survival include duration of CPR, number of doses of epinephrine, age, witnessed versus unwitnessed cardiac arrest, and the first and subsequent rhythm. Intact survival has been documented after unusually prolonged in-hospital resuscitation (15).
We report a case of a near-term infant with severe hypothermia, who despite a prolonged resuscitation, experienced an excellent outcome at two years of age. The present case reinforces the current recommendation of continuing resuscitative measures –irrespective of response to resuscitation – until a patient is rewarmed.
Figure 1).
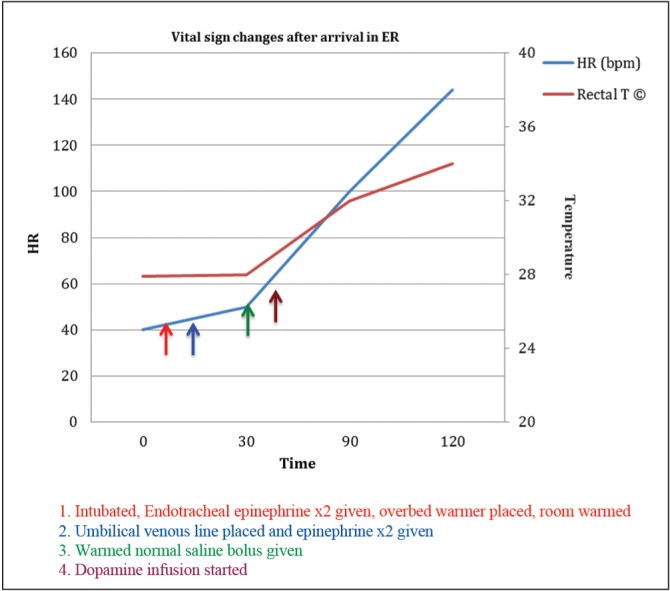
Time plot of key vital signs and interventions
REFERENCES
- 1.Danzl DF, Pozos RS. Accidental hypothermia. N Engl J Med. 1994;331:1756–60. doi: 10.1056/NEJM199412293312607. [DOI] [PubMed] [Google Scholar]
- 2.Mullany L. Neonatal hypothermia in low-resource settings. Semin Perinatol. 2010;34:426–33. doi: 10.1053/j.semperi.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson DA, Anderson N. Successful resuscitation of a severely hypothermic neonate. Ann Emerg Med. 1994;23:1390–3. doi: 10.1016/s0196-0644(94)70369-8. [DOI] [PubMed] [Google Scholar]
- 4.Bernstein SR, Heimler R, Sasidharan P. Normal 17-month outcome of a severely hypothermic term neonate. Clin Pediatr. 1998;37:191–6. doi: 10.1177/000992289803700306. [DOI] [PubMed] [Google Scholar]
- 5.Sofer S, Benkovich E. Severe infantile hypothermia: Short- and long-term outcome. Intens Care Med. 2000;26:88–92. doi: 10.1007/s001340050017. [DOI] [PubMed] [Google Scholar]
- 6.Healy J, Ryan CA. Normal developmental outcome following exposure and hypothermia in a new-born infant. Ir Med J. 1998;91:216–7. [PubMed] [Google Scholar]
- 7.Kleigman R, Marcdante K, editors. Nelson Essentials of Pediatrics. 7th edn. Philadelphia: Elsevier Saunders; 2015. Fetal and neonatal medicine; p. 2013. [Google Scholar]
- 8.Kaplan M, Eidelman AI. Improved prognosis in severely hypothermia newborn infants treated by rapid rewarming. J Pediatr. 1984;105:470–4. doi: 10.1016/s0022-3476(84)80031-1. [DOI] [PubMed] [Google Scholar]
- 9.Manzar S. Role of hypothermia in asphyxia. Pediatrics. 1999;104:1169. doi: 10.1542/peds.104.5.1169. [DOI] [PubMed] [Google Scholar]
- 10.Tafari N, Gentz J. Aspects on rewarming newborn infants with severe accidental hypothermia. Acta Paediatr Scand. 1974;63:595–600. doi: 10.1111/j.1651-2227.1974.tb04853.x. [DOI] [PubMed] [Google Scholar]
- 11.Daga SR, Gajendragadkar A, Chutke P, Kamat H. Rapid rewarming of severely hypothermic newborns during initial stabilization. Acta Paediatr. 1994;83:263–4. doi: 10.1111/j.1651-2227.1994.tb18090.x. (Lett) [DOI] [PubMed] [Google Scholar]
- 12.Shculman H, Laufer L, Berginer J, et al. CT findings in neonatal hypothermia. Pediatr Radiol. 1998;28:414–7. doi: 10.1007/s002470050373. [DOI] [PubMed] [Google Scholar]
- 13.Kattwinkel J, Perlman JM, Aziz K, et al. Part 15: Neonatal resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(Suppl 3):S909–S919. doi: 10.1161/CIRCULATIONAHA.110.971119. [DOI] [PubMed] [Google Scholar]
- 14.Peliowski-Davidovich A, Canadian Paediatric Society, Fetus and Newborn Committee Hypothermia for newborns with hypoxic ischemic encephalopathy. Paediatr Child Health. 2012;17:41–3. doi: 10.1093/pch/17.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kleinman ME, Chameides L, Schexnayder SM, et al. Pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126:e1361. doi: 10.1542/peds.2010-2972D. [DOI] [PubMed] [Google Scholar]


