Abstract
At our institution, we have noted that end-stage renal disease patients choosing a home dialysis modality after education often initiate renal replacement therapy with in-center hemodialysis (HD) instead. We interviewed 24 such patients (23 choosing peritoneal dialysis [PD], one choosing home HD) to determine reasons for this mismatch. The most common reasons cited for not starting home dialysis were: lack of confidence/concerns about complications, lack of space or home-related issues, a feeling of insufficient education, and perceived medical or social contraindications. We propose several potential strategies to help patients start with their preferred modality.
Keywords: Home dialysis, dialysis modality selection, pre-dialysis education
Pre-dialysis education presents different modes of renal replacement therapy, allowing patients to choose the modality that best fits their lifestyle. Ideally, the information presented should be comprehensive enough that patients are fully informed, but not overwhelmed. A potential measure of the success of pre-dialysis education is whether patients start with their chosen modality. In our center, we have found that slightly more than half of patients choosing a home modality ultimately started with in-center hemodialysis (HD) (1). This study examined reasons for this discrepancy.
Methods
English-speaking University of Rochester patients 18 years or older who attended pre-dialysis education between June 2004 and April 2014 and started with in-center HD despite choosing a home modality were approached for this study. Included patients gave verbal consent and were informed of the study's voluntary nature. All aspects of the project were submitted to, reviewed by, and approved by the University of Rochester institutional review board.
Patients were referred to pre-dialysis education at the discretion of their nephrologist. The education consisted of 1 visit with a nephrology nurse versed in all aspects of renal replacement therapy. Initially, we offered in-center HD, continuous ambulatory peritoneal dialysis (CAPD) and continuous cycling peritoneal dialysis (CCPD). Home HD (HHD) was added as an option in 2011. The nurse recorded the patient's modality selection, and the patient could follow up with the educator as needed.
We interviewed patients using a series of open-ended questions exploring patient, education, family, disease, and physician-related reasons why they did not start with a home dialysis modality despite saying they would do so after the education session.
Analysis of patient characteristics was done using STATA, version 13 (StataCorp LP, College Station, TX, USA), with a p value of less than 0.05 considered significant. Interview notes were reviewed for recurrent themes including medical/social issues, influence of physician/peers, issues related to the home, and concerns about complications.
Results
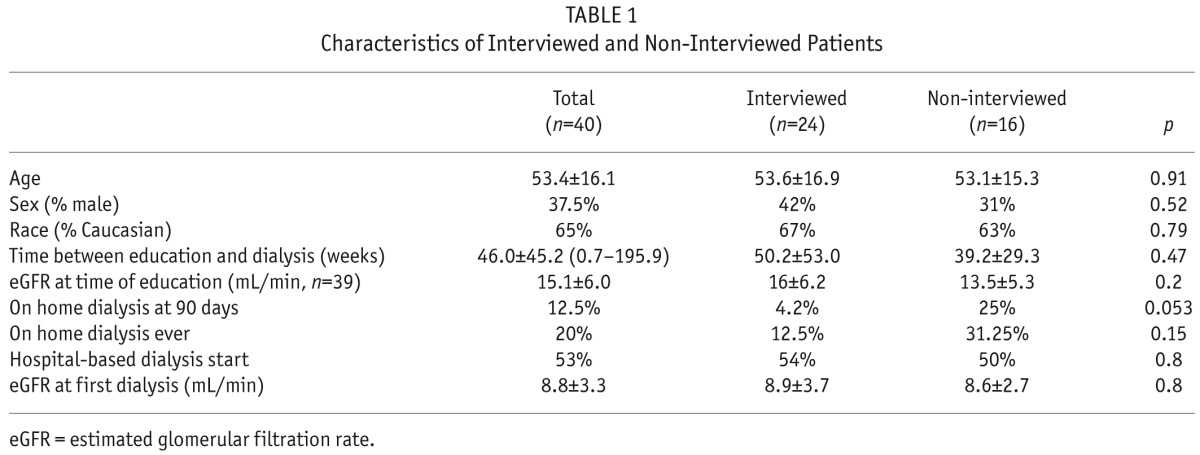
Twenty-four out of 40 patients agreed to be interviewed: 16 patients in the dialysis unit, and 8 by telephone. Interviews were conducted 350 ± 107 weeks after the education session. There were no differences between interviewed and non-interviewed patients (Table 1).
TABLE 1.
Characteristics of Interviewed and Non-Interviewed Patients
One patient selected HHD and 23 chose PD. Over half (54%) had an urgent, hospital-based dialysis start and almost a third of patients started HD with a permanent access in place. Three patients did not recall receiving education at all (despite documentation that they did). Ten of the remaining 21 patients had someone with them for the education session. One patient could not recall anything specific.
The following themes emerged as reasons why patients did not start home dialysis (typically PD). Select patient quotations which exemplify the theme are presented.
-
Lack of confidence/concerns about complications (38% of patients)
I saw blood squirting into someone's face [at hemodialysis] and I can't deal with that at home.I decided right away it [home dialysis] was too complicated. -
Lack of space or home-related issues (33%).
I learned about space needs, and my husband can't lift that much.I learned about all the water involved [in draining PD solutions] and I have a septic system and don't want extra water going through.[My home is] just not sanitary.I would be afraid about my dogs biting the tubes.Space would be tight. -
A feeling of insufficient education (30%).
I did not absorb all the information because it was all very overwhelming.I heard different stuff about rules while on peritoneal dialysis, I didn't know if I could go on [amusement park] rides and in pools. -
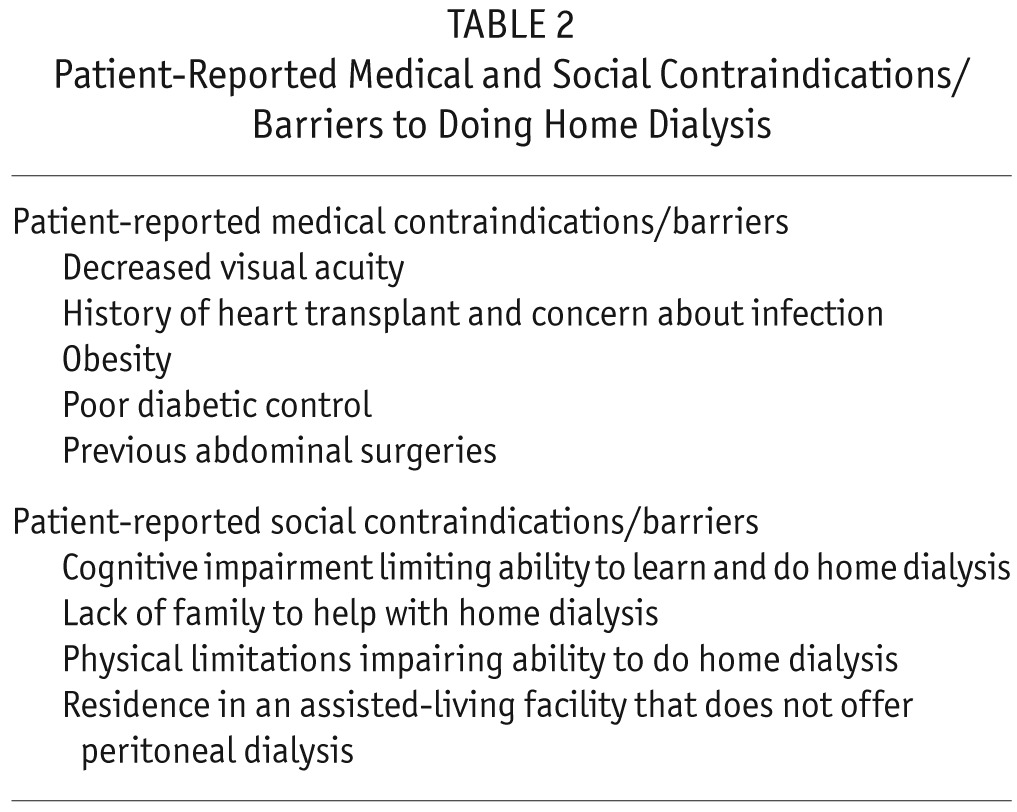
Influence of either the nephrologist (26%), often due to perceived medical or social contraindications (Table 2), or other patients (21%).
I spoke with a lot of patients at hemodialysis who got a lot of infections [on PD] and decided against it.[My doctor] told me it wouldn't be possible because I live at [an assisted-living facility] and because of my glucose.It was just not possible because of my macular degeneration.I had too many abdominal surgeries.[My nephrologist] recommended hemodialysis because my mind is gone.
TABLE 2.
Patient-Reported Medical and Social Contraindications/Barriers to Doing Home Dialysis
Eleven patients had 1 dominant factor which precluded home dialysis, whereas the remaining 13 had a combination of reasons.
Discussion
Many patients in our center who choose home dialysis still start with in-center HD. By identifying some of the reasons why, we can propose improvements to our pre-dialysis education sessions and develop a framework of important points to be covered.
A large number of patients found the education overwhelming and/or contradictory. Many patients came alone, and we feel another listener would be helpful to assimilate all the information and should be encouraged—particularly considering the known cognitive deficits of advanced chronic kidney disease (CKD) (2). To avoid contradictions, all parties involved should provide similar information and be frank about areas of uncertainty. We propose that providers attend their center's pre-dialysis education to familiarize themselves with the information presented.
Many patients were discouraged from using PD by their nephrologist due to medical and social contraindications. Some of the medical “contraindications” may be surmountable barriers, such as diabetes (3), previous abdominal surgeries (4), visual impairment (5), and obesity (6). Social issues may render the patient unable to do PD alone; however, caregivers may be willing to assist. When available, assisted PD may address many of the social barriers and serve as a vehicle of continued education (7).
We encourage providers to “think outside the box,” should a patient with medical or social concerns choose a home modality, and consider whether the condition is truly a contraindication or rather a barrier which may be overcome with more support, education, and training. We estimate that approximately half of our patients were dissuaded from using PD due to a medical or social barrier that may have been overcome with advanced planning.
Nephrologist bias may also be an issue. A patient who does not feel supported will likely not pursue home dialysis. A lack of familiarity, and therefore comfort, with home dialysis (particularly PD) may explain some physicians' lack of enthusiasm for home modalities (8). This is a difficult obstacle to overcome and may need to be addressed at the training program/society level. The American Society of Nephrology's Home Dialysis Benchmarks Workgroup provides some guidance in this area (9). We encourage providers experienced with home modalities to mentor colleagues who are less comfortable.
Negative peer influence, usually by failed PD patients during in-center HD, also impacted modality selection. We suggest that educators provide the opportunity for patients to speak with successful home dialysis patients as they work through their decision.
Home-related issues were also prevalent. We recommend that educators candidly discuss these concerns up front to avoid surprises later. If known early, many of these problems may be amenable to troubleshooting.
We found that patients urgently started on HD frequently remained in center. There may be several reasons for this including peer influence at dialysis, fear that dialysis complications would occur at home, and simple inertia—patients develop a routine doing in-center HD and do not wish to change. Urgent start PD (USPD) may help mitigate this problem by avoiding in-center HD altogether (particularly using a central venous catheter). Small studies suggest that USPD is associated with less bacteremia than a catheter-based HD start (10), although with a higher risk of leaks than non-urgent PD (11).
Can patients truly make an informed choice? Winterbottom et al. found that even with a “plethora of information,” many patients still had a simplistic view of treatment options, and that in end-stage renal disease (ESRD), a complex and chronic disease, decision making occurs over a long period of time, allowing biases to develop (12). These biases may hinder patients' ability to make a fully informed choice. Upon reviewing our interview data, we estimate that over half of our patients did not truly make an informed choice, and expecting this after a single educational visit may be unrealistic. We suggest that pre-dialysis education be an ongoing commitment rather than a single session.
Our study is limited by a small sample size and recall bias related to the long time period between patients' education sessions and the interviews. In addition, we did not consider patient concerns or changes in modality selection voiced after the initial education session.
We determined some of the reasons why patients may not start with a home dialysis modality despite its selection after pre-dialysis education. Using this, we propose several potential strategies to help patients make a more informed decision and to facilitate their starting with their desired modality.
Disclosures
The authors have no financial conflicts of interest to declare.
Acknowledgments
Part of this work was presented in abstract form at the Annual Dialysis Conference, 2015, New Orleans, LA, USA.
REFERENCES
- 1. Liebman SE, Bushinsky DA, Dolan JG, Veazie P. Differences between dialysis modality selection and initiation. Am J Kidney Dis 2012; 59(4):550–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nulsen RS, Yaqoob MM, Mahon A, Stoby-Fields M, Kelly M, Varagunam M. Prevalence of cognitive impairment in patients attending pre-dialysis clinic. J Renal Care 2008; 34(3):121–6. [DOI] [PubMed] [Google Scholar]
- 3. Dalai P, Misra M. Improving the care of diabetic patients on peritoneal dialysis. Contrib Nephrol 2012; 178:271–7. [DOI] [PubMed] [Google Scholar]
- 4. Crabtree JH, Burchette RJ. Effect of prior abdominal surgery, peritonitis, and adhesions on catheter function and long-term outcome on peritoneal dialysis. Am Surgeon 2009; 75(2):140–7. [DOI] [PubMed] [Google Scholar]
- 5. Wright L. Training a patient with visual impairment on continuous ambulatory peritoneal dialysis. Nephol Nurs J 2005; 32(6):675–7. [PubMed] [Google Scholar]
- 6. Mendelssohn DC, Mujais SK, Soroka SD, Brouillette J, Takano T, Barre PE, et al. A prospective evaluation of renal replacement therapy modality eligibility. Nephrol Dial Transplant 2009; 24(2):555–61. [DOI] [PubMed] [Google Scholar]
- 7. Oliver MJ, Quinn RR, Richardson EP, Kiss AJ, Lamping DL, Manns BJ. Home care assistance and the utilization of peritoneal dialysis. Kidney Int 2007; 71(7):673–8. [DOI] [PubMed] [Google Scholar]
- 8. Berns JS. A survey-based evaluation of self-perceived competency after nephrology fellowship training. Clin J Am Soc Nephrol 2010; 5(3):490–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. American Society of Nephrology Home Dialysis Benchmarks Workgroup. https://www.asn-online.org/education/training/tpd/PD_and_HHD_benchmarks.pdf Accessed July 14, 2015.
- 10. Koch M, Kohnle M, Trapp R, Haastert B, Rump LC, Aker S. Comparable outcome of acute unplanned peritoneal dialysis and haemodialysis. Nephrol Dial Transplant 2012; 27(1):375–80. [DOI] [PubMed] [Google Scholar]
- 11. Ghaffari A. Urgent-start peritoneal dialysis: a quality improvement report. Am J Kidney Dis 2012; 59(3):400–8. [DOI] [PubMed] [Google Scholar]
- 12. Winterbottom A, Bekker H, Conner M, Mooney M. Choosing dialysis modality: decision making in a chronic illness context. Health Expect 2014; 17(5):710–23. [DOI] [PMC free article] [PubMed] [Google Scholar]


