Abstract
Background: Infantile colic, cry-fuss and sleep problems are transient in the initial months of life, but they contribute to maternal depression, parenting stress and family mental health problems. In this randomized clinical trial, we aimed to explore the efficacy of massage therapy compared to rocking in reducing infantile colic symptoms including duration and number of cries, sleep duration and severity of infant colic.
Methods: This was a single blind RCT study with a one-week follow-up. One hundred colicky infants aged younger than 12 weeks old were randomly assigned into massage and rocking groups. Infants in the massage group received a massage for 15-20 minutes once during a day and once at night before sleeping for a week. In the control group, mothers rocked their infants gently for 5-25 minutes when the symptoms of colic appeared. Parents recorded the details of the colic symptoms in a diary every day. A GEE approach was applied to explore the effect of the intervention.
Results: Efficiency of massage therapy was significantly higher than rocking. At the end of the study, the mean number of daily cries was 4.26±1.40 in the massage and 6.9±2.14 the rocking groups (p<0.01). The mean of the severity score was 1.39±0.19 less in the massage group (p<0.01). Moreover, the mean differences of massage and rocking groups were -0.82±0.20 hour (p<0.01) and 0.72±0.35 (p= 0.04) in the duration of cries and duration of sleep, respectively.
Conclusion: Massaging significantly improved colic symptoms during a one-week intervention for all outcomes. In addition, significant differences were found between the intervention and control groups in favor of massaging. Therefore, massage therapy is more effective than rocking for treating infant colic symptoms.
Keywords: Colic, Massage, Clinical Trial, Pediatrics
Introduction
Based on Wessel criteria, an infant who cries for at least three hours a day three days a week and for three consecutive weeks, is colicky (1). Infantile colic, cry-fuss and sleep problems are transient in the initial months of life, but they contribute to maternal depression, parenting stress and family mental health problems (2-8). In addition, the long-term effects of infantile colic on subsequent child behavior problems have been studied even as early signs of the future disease for both parents and infants (2,9-13).
Crying and irritability, as the most common symptoms of infantile colic, are the reasons of most parents’ complaints and seeking medical care in the first three months of life. The prevalence of infantile colic was reported in a wide range from 3% to 40%. Variation in estimating the prevalence comes from differences in definitions, methods and the geographic area of the study (14,15). However, infantile colic is easily recognized, and its etiology is not completely understood and is difficult to solve. Therefore, in addition to the burden of infantile colic on family and social health-care system, ambiguity of its cause(s) makes it an interesting subject for pediatric researches (7,16-18). However, lack of proven cause for infantile colic subsequently leads to a wide spectrum of therapies for treating infants who suffer from this problem (19-21).
Researches in this field are classified into pharmacological, nutritional and parental care studies. Simethicone, Dicyclomine Hydrochloride and Cimetropium bromide are usually used in pharmacological treatments; however, their efficiency has not been proven in the related texts. In addition, some side effects are mentioned in this type of therapy (22). Nutritional methods, particularly probiotics, are safe compared to pharmacological treatments. However, recent systematic reviews have not approved these treatments as a definite solution (22-26).
Massage therapy not only effects infantile colic, but also has proven benefits on maternal- infant relationship, weight gain, gastrointestinal problems and infant immune system (27-31). Our literature review revealed that the majority of studies in this context explored the relation between massage therapy and number and duration of crying. In contrast, few studies were conducted in the field of reducing the severity of infantile colic and improving infant sleep time (1,16,32).
We conducted this randomized clinical trial to explore the effect of massage therapy as a type of parental care therapy on reducing infantile colic symptoms. We compared the efficiency of massaging with rocking the infants in reducing the frequency, duration and severity of infantile cries. In addition, improvements in infants’ sleep time were examined between the two groups.
Methods
This was a randomized clinical trial to explore the effect of massaging on pacifying infantile colic symptoms with a one-week follow-up. Symptoms included duration and number of cries, severity of infant colic and duration of sleep. This study was registered in the Iranian Registry of Clinical Trials (IRCT), with a registration number of IRCT201106054317N5.
The sample size was calculated using the random sampling method with a significant level of 0.05, power of 0.8 and considering the results of similar studies (1.4 and 2 as standard deviation of duration of cries in the intervention and control groups and one hour as a significant difference between the mean of cry duration in the two groups) (33). The minimum sample size of 47 was needed for each group. To control the loss to follow up, 50 samples were considered in each group.
Study Design
The trial was conducted in Amirkabir Hospital of Arak, in the central part of Iran. A pediatrician examined infants who were brought into the pediatric clinic from August 23, 2010 to January 20, 2011. The examination was conducted based on Wessel’s criteria. The aims of the study were explained to the parents and the volunteer families signed the written consent. Infants who were younger than 12 weeks old, with full-term birth, without any known diseases, with no medical treatments for colic and no allergy to lactose were admissible to take part in this study. In addition, infants with smoker mothers during pregnancy or those whose mothers had severe anxiety background were not included. Furthermore, we excluded infants who underwent traditional and medical treatments during the study, or those whose mothers failed to perform the intervention correctly. Due to the nature of the intervention, among the infants who passed the above criteria, those who had no skin problems or limitations on receiving massage were recruited.
The participants were randomly assigned into the intervention and control groups based on referral day. Pediatrician and hospital staffs were kept blind to the allocation. Unfortunately, it was not possible to consider blinding method for mothers. An expert taught the mothers of infants in the intervention group to massage their babies correctly. Then, they were asked to massage infants for 15-20 minutes once during a day and once at night before sleeping during a one-week period. In the control group, mothers rocked their infants gently for 5-25 minutes when the symptoms of colic appeared. All participants recorded the duration (minutes), severity (Visual Analog Scale) and count of colic cries of the babies during the day for one week in an information diary. In addition, similar diaries were completed for one and two days before the start of the intervention as the baseline information for each participant.
A committee including ten specialists in midwifery, obstetrics and gynecology, pediatrics and neurophysiology verified the validity of the information diary. Moreover, to increase the validity of registration, two members of the research team who were kept blind to the allocation, guided families during the study in both groups.
Ethical Considerations
The participants freely participated in this clinical trial and could withdraw from the study at any time they wished. The Ethics Committee of the Shahid Beheshti University of Medical Sciences approved the study. Written informed consent was obtained from each participant.
Statistical Analysis
All data management and statistical analyses were conducted using Stata statistical software, Version 11 (Stata Inc., College Station, TX, USA). Pearson’s Chi-squared test was used for categorical variables and independent t-test for continuous variables to examine the differences in the levels of cofounder and demographic variables. In addition, the generalized estimating equations (GEE) approach was used to explore the effect of the interventions in the presence of other variables.
Results
All fifty infants in both groups completed the trial because they had no adverse effect related to the trial, and no one refused to cooperate during the study. Baseline characteristics, demographic variables and the results of comparison tests are shown in Table 1. According to this table, no significant difference existed between the massage group and the rocking group in demographic variables at the significance level of 0.05. The majority of the mothers breastfed their infants, 92% and 90% in the massage and rocking groups, respectively. Type of delivery was equally distributed in both groups (p= 0.23) and no significant difference was found between the percentage of caesarean section (CS) and normal vaginal delivery (NVD) in the two groups (p=0.23).
Table 1 . Comparing Baseline Characteristics of the Infants between the Two Groups .
| Variables | Massage Gup | Rocking Group | p |
| Infant age (week) | 4.32±3.24† | 4.80±3.55 | 0.481 |
| Infant weight (g) | 4121.2±986.03 | 4142.8±1028.23 | 0.91 |
| Birth weight (g) | 3229.2±509.89 | 3383±3143.28 | 0.27 |
| Mother age (year) | 26.9±3.87 | 27±4.50 | 0.91 |
|
Sex Girl Boy |
21 (42%)‡ 29 (58%) |
27(54%) 23(46%) |
0.23 |
|
Nutrition Breastfeeding Other |
46 (92%) 4 (8%) |
45 (90%) 5 (10%) |
0.73 |
|
Delivery type NVD CS |
24 (48%) 26 (52%) |
30 (60%) 20 (40%) |
0.23 |
| Number of cries one day before | 6.12±1.75 | 6.92±2.91 | 0.08 |
| Number of cries two days before | 5.74±1.66 | 6.52±2.70 | 0.09 |
| Duration of cries one day before (hour) | 4.96±1.37 | 3±1.31 | <0.001 |
| Duration of cries two days before (hour) | 4.58±1.36 | 2.86±1.31 | <0.001 |
| Duration from the start of the colic symptoms (day) | 8.3±6.82 | 11.22±11.41 | 0.12 |
| Duration of sleep per day (hour) | 9.22±1.76 | 12.24±2.98 | <0.001 |
| Infant colic severity | 0.001 | ||
|
Moderate Medium Sever |
0 (0%) 34 (68%) 16 (32%) |
11 (22%) 22 (44%) 17 (34%) |
† mean±SD, ‡ number (percent)
Among symptoms of colic, number of cries had a statistically equal baseline means in the two groups (p=0.08). The mean of cry duration was 4.96 hours in the massage and 3 hours in the rocking groups (p<0.05) one day before the intervention. Furthermore, significant differences were found between the baselines of sleep duration (9.29 hours in the massage and 12.24 hours in the rock groups), and infant colic severity between the two groups (p<0.05). All these differences were in favor of the rocking group, which could affect the results. Therefore, Table 1 indicates that the baseline values of the time of cry, duration of sleep and severity of infantile colic should be considered in the modeling process.
Table 2 summarizes the results of GEE model, which was applied to explore the effect of interventions on improving colic symptoms. The baseline values of outcomes did not match the randomization process. Therefore, we entered these values to adjust the coefficients of the intervention group. Baseline values for all outcomes were significant (p<0.01) except duration of sleep (p=0.38), and ignoring them could affected the results. On the other hand, the interaction between time and group variable was significant in all models (p<0.01).
Table 2 . Results of Applying GEE Model to Explore the Effect of the Interventions on Infantile Colic Symptoms in the Presence of Other Variables .
| Variable | Duration of Sleep | Duration of Cries | Number of Cries | Infant Colic Severity | ||||
| Mean(SD) | p | Mean (SD) | p | Mean (SD) | p | Mean (SD) | p | |
| Time | 1.01±0.08 | <0.01 | -0.95±0.05 | <0.01 | -0.20±0.02 | <0.01 | -0.77±0.06 | <0.01 |
| Group (Massage) | -2.14±0.44 | <0.01 | 1.34±0.30 | <0.01 | 0.29±0.07 | <0.01 | 0.94±0.21 | <0.01 |
| Interaction | -0.51±0.05 | <0.01 | 0.46±0.03 | <0.01 | 0.09±0.01 | <0.01 | 0.34±0.04 | <0.01 |
| Baseline | 0.06±0.07 | 0.38 | 0.40±0.08 | <0.01 | 0.04±0.01 | <0.01 | 0.69±0.11 | <0.01 |
| Constant | 11.67±0.89 | <0.01 | 1.06±0.31 | <0.01 | 1.69±0.09 | <0.01 | 2.89±0.28 | <0.01 |
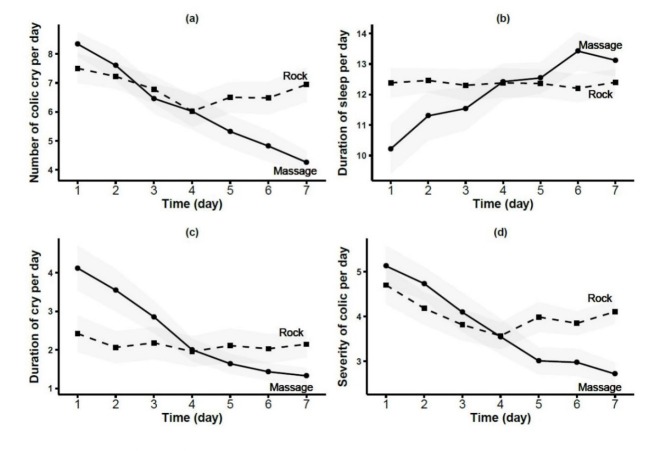
Although the coefficients of group variable were in favor of rocking intervention, the significant interaction terms indicated that coefficients should not be interpreted directly. Graphical illustrations of the trends of colic symptoms with 95% confidence intervals are depicted in Figure 1. Exploring the trends of outcomes in each group expresses the decreasing slope for the number, duration and severity of cries. In addition, one could observe an increasing slope for the duration of sleep in both groups.
Fig. 1 .
Comparing the Trends of Outcomes across Groups during the Trial with 95% Confidence Intervals in Gray (a): Number of Colic Cries per Day; (b): Duration of Sleep Per Day; (c): Duration of Cry Per Day; (d): Severity of Colic Per Day
Finally, Table 3 compares the changes in the outcomes means during the study. We compared the mean differences between the first and the last days in each group. The obtained results revealed that all symptoms improved significantly in the massage group (p<0.001) during the intervention, while only the severity of colic improved in the rocking group (p=0.02).
Table 3 . Comparing the Means of Infantile Colic Symptoms between the First and Last Days of the Trial in the Massage Group and Rocking Group .
| Massaging | Rocking | ||||
| Outcome | Mean difference† | p | Mean difference | p | |
| Duration of cries | 2.80±0.31 | <0.001 | 0.27±0.30 | 0.36 | |
| Duration of sleep | -2.9±0.49 | <0.001 | -0.02±0.33 | 0.95 | |
| Number of cries | 4.08±0.29 | <0.001 | 0.56±0.20 | 0.16 | |
| Infant colic severity | 2.41±0.26 | <0.001 | 0.59±0.26 | 0.02 |
† (Mean of the First Day –Mean of the Last Day) ±SD
Discussion
We compared the effect of massage therapy and rocking on improving infantile colic symptoms. Although regression coefficients indicated that rocking was more effective, the more accurate explorations demonstrated the efficiency of massaging compared to rocking. In addition, improvement in all colic symptoms was significant in the massage group during the study.
Our study revealed that the number of colic cries in the massage group was reduced from 8.34/day to 4.26/day at the end of the study. Alvandi et al. conducted a similar study and found that massage therapy could reduce the number of colic cries from 8 to 6 cries per day (34). Olafsdottir et al. used chiropractic spinal manipulation to decrease the number of colic cries from 5.1 at the first day of the study to 3.1 at the end of the study (35). They also demonstrated that placebo could improve the colic cries in colicky infants.
The majority of the studies on infantile colic explored the effect of massage therapy on the rate and duration of colic cries. In this study, we showed that the average of crying severity was reduced from 5.13 to 2.71 during a one-week intervention. This study also showed that massage therapy helps infants to have a better sleep. The Average of sleep duration increased about 2.9 hours per day for infants who received a one-week massage.
Reviewing the available literature about the suggested treatments for infantile colic showed that none of these treatments were considered as the definite solution for this problem. Hall et al. evaluated 19 studies and 2 literature reviews on infantile colic treatments (five studies on pharmacological treatments, 10 on nutritional intervention and 4 on behavioral therapies). They concluded that pharmacological interventions are not effective or appropriate for infantile colic. They also stated that studies on behavioral interventions for infantile colic are limited and do not provide adequate evidence for using these treatments. They mentioned scientific evidences that support the use of some nutritional interventions for infantile colic (22). A systematic review by Sung et al. showed that there is still insufficient evidence to support probiotic use for managing colic (24). Comparing these studies confirms the importance of conducting more research to find a safe and efficient treatment for infantile colic.
The majority of the statistical methods including regression models for analyzing longitudinal data consider the data from all measurements under the study in the modeling process simultaneously. In the presence of an interaction, these models should not be used without considering the interaction term. On the other hand, interpretation of coefficients in regression models with the interaction term are not usually clear (36,37). In this study, we fitted a marginal model using the GEE method and found a significant interaction between the treatment groups and time (Fig. 1). We did not interpret the coefficients due to the presence of this interaction. The major advantage of statistical regression models is their ability to adjust the results when randomization is not able to match confounders or baseline values.
This study had two limitations. First, mothers performed the massage therapy at home, so we could not be sure of the similarity and correctness of the massaging methods. To overcome this problem we examined the manner mothers massaged the infants three times. In addition, the parents were in direct contact with an advisor for their questions during the intervention. We believe this consideration makes the results of this study more trustworthy than other similar studies. Second, the interaction term was significant., and statistical references suggested expanding duration of the study in this case (38). Therefore, conducting further studies to explore the effect of massage therapy on infantile colic symptoms in a wider period of intervention is highly recommended.
A number of studies have been conducted about the influence of different kinds of oils on infantile colic like lavender oil (39,40). Massaging could be more comfortable by oil. Therefore, we suggest conducting a study to assess the use of the lavender oil in massage therapy as a new intervention for infantile colic.
Conclusion
In this study, colic symptoms were relieved in colicky infants who received a massage over a one-week intervention. On the other hand, rocking just affected the colic severity based on comparing the outcomes mean at the first and last days of the intervention. Therefore, massage therapy could be more effective than rocking for treating infant colic symptoms.
Acknowledgements
We extend our sincere appreciation to the Committee of Scientific Research at Shahid Beheshti University of Medical Sciences. We also extend our unlimited gratitude to Dr. Parsa Yousefi (M.D) for his help and guidance during this study. We thank Amirkabir Hospital of Arak for providing us with the space and equipment. Finally, we thank the parents and infants who participated in this study.
Cite this article as: Sheidaei A, Abadi A, Zayeri F, Nahidi F, Gazerani N, Mansouri A. The effectiveness of massage therapy in the treatment of infan-tile colic symptoms: A randomized controlled trial. Med J Islam Repub Iran 2016 (9 April). Vol. 30:351.
References
- 1.Wessel MA, Cobb JC, Jackson EB, Harris GS, Detwiler AC. Paroxysmal fussing in infancy, sometimes called" colic". Pediatrics. 1954;14(5):421–35. [PubMed] [Google Scholar]
- 2.Smart J, Hiscock H. Early infant crying and sleeping problems: A pilot study of impact on parental wellbeing and parentendorsed strategies for management. Journal of paediatrics and child health. 2007;43(4):284–90. doi: 10.1111/j.1440-1754.2007.01060.x. [DOI] [PubMed] [Google Scholar]
- 3.Radesky JS, Zuckerman B, Silverstein M, Rivara FP, Barr M, Taylor JA. et al. Inconsolable infant crying and maternal postpartum depressive symptoms. Pediatrics. 2013;131(6):e1857–e64. doi: 10.1542/peds.2012-3316. [DOI] [PubMed] [Google Scholar]
- 4. Sung V, Hiscock H, Tang ML, Mensah FK, Nation ML, Satzke C, et al. Treating infant colic with the probiotic Lactobacillus reuteri: double blind, placebo controlled randomised trial. BMJ: British Medical Journal 2014;348. [DOI] [PMC free article] [PubMed]
- 5. Petzoldt J, Wittchen HU, Wittich J, Einsle F, Höfler M, Martini J. Maternal anxiety disorders predict excessive infant crying: a prospective longitudinal study. Archives of disease in childhood 2014: archdischild-2013-305562. [DOI] [PubMed]
- 6.Kurth E, Spichiger E, Cignacco E, Kennedy HP, Glanzmann R, Schmid M. et al. Predictors of crying problems in the early postpartum period. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2010;39(3):250–62. doi: 10.1111/j.1552-6909.2010.01141.x. [DOI] [PubMed] [Google Scholar]
- 7.Kurth E, Kennedy HP, Spichiger E, Hösli I, Zemp Stutz E. Crying babies, tired mothers: what do we know? A systematic review. Midwifery. 2011;27(2):187–94. doi: 10.1016/j.midw.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 8.Kaley F, Reid V, Flynn E. The psychology of infant colic: A review of current research. Infant Mental Health Journal. 2011;32(5):526–41. doi: 10.1002/imhj.20308. [DOI] [PubMed] [Google Scholar]
- 9.Brown M, Heine RG, Jordan B. Health and wellbeing in schoolage children following persistent crying in infancy. Journal of paediatrics and child health. 2009;45(5):254–62. doi: 10.1111/j.1440-1754.2009.01487.x. [DOI] [PubMed] [Google Scholar]
- 10.Gelfand AA. Childhood migraine is associated with a history of infantile colic. Journal of Pediatrics. 2013;163(3):922–6. doi: 10.1016/j.jpeds.2013.06.048. [DOI] [PubMed] [Google Scholar]
- 11.Gelfand AA, Goadsby PJ, Allen IE. The relationship between migraine and infant colic: A systematic review and meta-analysis. Cephalalgia. 2015 Jan;35(1):63–72. doi: 10.1177/0333102414534326. [DOI] [PubMed] [Google Scholar]
- 12.Gelfand AA, Thomas KC, Goadsby PJ. Before the headache Infant colic as an early life expression of migraine. Neurology. 2012;79(13):1392–6. doi: 10.1212/WNL.0b013e31826c1b7b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romanello S, Spiri D, Marcuzzi E, Zanin A, Boizeau P, Riviere S. et al. Association between childhood migraine and history of infantile colic. JAMA. 2013;309(15):1607–12. doi: 10.1001/jama.2013.747. [DOI] [PubMed] [Google Scholar]
- 14.Wake M, Morton-Allen E, Poulakis Z, Hiscock H, Gallagher S, Oberklaid F. Prevalence, stability, and outcomes of cry-fuss and sleep problems in the first 2 years of life: prospective community-based study. Pediatrics. 2006;117(3):836–42. doi: 10.1542/peds.2005-0775. [DOI] [PubMed] [Google Scholar]
- 15.Talachian E, Bidari A, Rezaie MH. Incidence and risk factors for infantile colic in Iranian infants. World journal of gastroenterology: WJG. 2008;14(29):4662. doi: 10.3748/wjg.14.4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savino F. Focus on infantile colic. Acta Pædiatrica. 2007;96(9):1259–64. doi: 10.1111/j.1651-2227.2007.00428.x. [DOI] [PubMed] [Google Scholar]
- 17. Boychuk R. Infant Colic. University of Hawaii Case Based Pediatrics For Medical Students and Residents. University of Hawaii John A. Burns School of Medicine April 2003:Chapter IX.1.
- 18.Rimer R, Hiscock H. National survey of Australian paediatricians' approach to infant crying. Journal of paediatrics and child health. 2014;50(3):202–7. doi: 10.1111/jpc.12452. [DOI] [PubMed] [Google Scholar]
- 19.Savino F, Tarasco V. New treatments for infant colic. Current opinion in pediatrics. 2010;22(6):791–7. doi: 10.1097/MOP.0b013e32833fac24. [DOI] [PubMed] [Google Scholar]
- 20.Management of infantile colic. BMJ (Clinical research ed) 2013;347:f4102. doi: 10.1136/bmj.f4102. [DOI] [PubMed] [Google Scholar]
- 21.Dobson D, Lucassen P, Miller JJ, Vlieger AM, Prescott P, Lewith G. Manipulative therapies for infantile colic. Cochrane Database Syst Rev. 2012 Dec;12 doi: 10.1002/14651858.CD004796.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hall B, Chesters J, Robinson A. Infantile colic: a systematic review of medical and conventional therapies. Journal of paediatrics and child health. 2012;48(2):128–37. doi: 10.1111/j.1440-1754.2011.02061.x. [DOI] [PubMed] [Google Scholar]
- 23.Anabrees J, Indrio F, Paes B, AlFaleh K. Probiotics for infantile colic: a systematic review. BMC pediatrics. 2013;13(1):186. doi: 10.1186/1471-2431-13-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sung V, Collett S, de Gooyer T, Hiscock H, Tang M, Wake M. Probiotics to prevent or treat excessive infant crying: systematic review and meta-analysis. JAMA pediatrics. 2013;167(12):1150–7. doi: 10.1001/jamapediatrics.2013.2572. [DOI] [PubMed] [Google Scholar]
- 25.Perry R, Hunt K, Ernst E. Nutritional supplements and other complementary medicines for infantile colic: a systematic review. Pediatrics. 2011 Apr;127(4):720–33. doi: 10.1542/peds.2010-2098. [DOI] [PubMed] [Google Scholar]
- 26.Iacovou M, Ralston RA, Muir J, Walker KZ, Truby H. Dietary management of infantile colic: a systematic review. Maternal and child health journal. 2012;16(6):1319–31. doi: 10.1007/s10995-011-0842-5. [DOI] [PubMed] [Google Scholar]
- 27.Neu M, Pan Z, Workman R, Marcheggiani-Howard C, Furuta G, Laudenslager ML. Benefits of massage therapy for infants with symptoms of gastroesophageal reflux disease. Biol Res Nurs. 2014 Oct;16(4):387–97. doi: 10.1177/1099800413516187. [DOI] [PubMed] [Google Scholar]
- 28.Ang JY, Lua JL, Mathur A, Thomas R, Asmar BI, Savasan S. et al. A randomized placebo-controlled trial of massage therapy on the immune system of preterm infants. Pediatrics. 2012 Dec;130(6):e1549–58. doi: 10.1542/peds.2012-0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diego MA, Field T, Hernandez-Reif M. Preterm infant weight gain is increased by massage therapy and exercise via different underlying mechanisms. Early human development. 2014;90(3):137–40. doi: 10.1016/j.earlhumdev.2014.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Procianoy RS, Mendes EW, Silveira RC. Massage therapy improves neurodevelopment outcome at two years corrected age for very low birth weight infants. Early human development. 2010;86(1):7–11. doi: 10.1016/j.earlhumdev.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 31.Kulkarni A, Kaushik JS, Gupta P, Sharma H, Agrawal R. Massage and touch therapy in neonates: the current evidence. Indian pediatrics. 2010;47(9):771–6. [PubMed] [Google Scholar]
- 32. Kliegman R, Behrman RE, Jenson HB, Stanton BF. Nelson textbook of pediatrics: Elsevier/Saunders; 2012.
- 33.Huhtala V, Lehtonen L, Heinonen R, Korvenranta H. Infant massage compared with crib vibrator in the treatment of colicky infants. Pediatrics. 2000;105(6):e84. doi: 10.1542/peds.105.6.e84. [DOI] [PubMed] [Google Scholar]
- 34. Sh A, Taj Ansari F. Effect of theraputic touch on colicky pain in infants who admitted in pediatrics privet offices in Tehran: MS thesis in nursing; 1996.
- 35.Olafsdottir E, Forshei S, Fluge G, Markestad T. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Archives of disease in childhood. 2001;84(2):138–41. doi: 10.1136/adc.84.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis: John Wiley & Sons; 2012.
- 37. Diggle P, Heagerty P, Liang KY, Zeger S. Analysis of longitudinal data: Oxford University Press; 2002.
- 38. Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied linear statistical models 2005.
- 39.Alexandrovich I, Rakovitskaya O, Kolmo E, Sidorova T, Shushunov S. The effect of fennel (Foeniculum vulgare) seed oil emulsion in infantile colic: a randomized, placebo-controlled study. Alternative therapies in health and medicine. 2003;9(4):58–61. [PubMed] [Google Scholar]
- 40.Çetinkaya B, Başbakkal Z. The effectiveness of aromatherapy massage using lavender oil as a treatment for infantile colic. International Journal of Nursing Practice. 2012;18(2):164–9. doi: 10.1111/j.1440-172X.2012.02015.x. [DOI] [PubMed] [Google Scholar]