Abstract
Wheelchair basketball has evolved into a high-performance sport over several years, and small variations in player performance can determine the difference between winning and losing. Therefore, adequate micronutrient intake may influence this difference if performance-promoting macronutrient intake and physical fitness are equal between teams. Seventeen elite male wheelchair basketball players belonging to the Spanish National Team participated in this study. Macro- and micronutrient intake were determined using a food-weighing diary over three consecutive days during three training camps in two consecutive years. Current Dietary Reference Intake levels were used to determine the adequacy of intake of seventeen micronutrients of particular interest for athletes. After categorizing the consumed foods into fourteen food groups according to the National Nutrient Database for Standard References (USDA) these groups were used to identify the best predictors of the adequacy of intake for each micronutrient. Total energy intake correlated positively with the adequacy of all micronutrient intake levels, except for vitamins A and E. Five B vitamins and phosphorus, selenium, and iron showed 100% adequacy. All other micronutrient intake levels were found to be inadequate, e.g., vitamin E (51% adequacy) and calcium (73%). The fruit, fish and cereal food groups were found to be predictors of adequate intake of most micronutrients. Together with energy intake (p = .009, η2 = 0.49), the intake of the fruit (p = .032, η2 = 0.39) and egg (p = .036, Kendall’s W = 0.42) food groups increased significantly over time, along with improved iodine (p = .008, W = 0.61) and magnesium (p = .030, W = 0.44) adequacy levels. Because the adequacy of micronutrient intake correlates positively with energy intake (R = 0.64, p < .001), a varied diet that includes cereals, fish and fruits is especially important for players with low levels of energy intake. Supplements may be a possible solution if adequate micronutrient intake cannot be achieved through regular dietary intake alone. However, dietary analyses should be conducted on a regular basis throughout the year to improve the nutritional knowledge of the athletes and assure adequate micronutrient intake.
Introduction
In high-performance sports, differences in the factors that determine winning and losing can be small [1]. Hence, athletes should consider all factors that can help enhance their performance. In wheelchair basketball, three main factors are involved: the wheelchair, the athlete and the interactions between them [2]. As athletes undergo training programs, which are comparable to those of their able-bodied peers [3], the principles of sports nutrition should be considered to support effective training and to improve performance levels during training and competition [4, 5]. In addition to control the macronutrients energy distribution and timing of energy intake throughout the day, ensuring an adequate intake of micronutrients may also have a positive impact on performance [6].
Micronutrients, including vitamins and minerals, are required in small amounts and interact with one another to regulate physiological functions [4, 5]. For athletes, the roles of micronutrients in energy metabolism, blood and bone health and antioxidant functioning are extremely important, and the B vitamin group (e.g., thiamin, riboflavin, niacin, vitamin B6, folic acid and vitamin B12) and minerals (e.g., iodine, iron, magnesium and zinc) facilitate the conversion of macronutrients into energy and are therefore essential to athletes because of their high levels of energy expenditure [4, 5]. In athletes, red blood cell production is often increased, requiring an increased intake of iron, a component of hemoglobin, and folic acid and vitamin B12, which are also needed for the synthesis of DNA and RNA [7]. Furthermore, adequate levels of calcium, phosphorus and vitamin D ensure the maintenance of sufficient bone mineral density, helping to prevent stress fractures [7–9]. Certain antioxidants (vitamin A, C and E) and minerals (selenium and zinc) protect cells and tissues against damage from free oxygen radicals, which increase in number as a result of exercise [7]. Although athletes may have slightly higher micronutrient requirements because exercise stresses many of the metabolic pathways in which micronutrients are involved, no special recommendations have been described for these requirements [4, 5]. To date, there is no evidence of altered micronutrient requirements for wheelchair athletes, with the exception of those related to vitamin D, as osteoporosis is associated with vitamin D deficiency, which is common in athletes with spinal cord injuries (SCI) [10–12]. Therefore, we used the existing United States and Canadian Dietary Reference Intake (DRI) values to determine adequate micronutrient intake levels [13, 14].
Both the American College of Sports Medicine and the International Society of Sports Nutrition recommend a well-balanced diet to meet vitamin and mineral requirements [4, 5]. Nevertheless, athletes with restricted energy intake are at an increased risk of inadequate nutrient intake [4, 5]. Until now, very few studies have examined the energy intake patterns of male wheelchair athletes, and all of these studies have reported low energy intake levels within this group relative to the intake levels of able-bodied athletes [15–17]. Only one study, on male Canadian wheelchair athletes, has shown inadequacies in the micronutrient intake [16], and because inadequate micronutrient intake can weaken one’s immune system, increasing the risks of illness, the intake of nutrient-dense foods, that can improve the adequacy of micronutrients, could improve the health of these athletes.
Therefore, the aims of this study were to (1) evaluate micronutrient intake by elite wheelchair basketball players based on the latest Food and Nutrition Board (FNB) guidelines, (2) analyze which food groups are crucial for the adequacy of micronutrient intake, and (3) examine whether nutritional advice provided one month and again one year after the initial recommendations can improve diet quality.
Methods
Participants and study design
Seventeen male wheelchair basketball players on the Spanish National Team participated in this study, which was conducted in Madrid (Spain) at the Higher Sport Council during three training camps held in the precompetitive season in two consecutive years. To compare the adequacy of micronutrient intake at the group level, data for all players participating in the camps in May (Training Camp 1 (T1), 14 players) and June of the first year (Training Camp 2 (T2), 12 players) and in June of the second year (Training Camp 3 (T3), 11 players) were used (Fig 1). Disabilities ranged from amputations to spina bifida and spinal cord injuries. The effectiveness of the nutritional advice given was determined in consultation with the eight players who participated in all the camps.
Fig 1. Timeline of all training camps (T1, T2 and T3).
The Ethics Committee of the Technical University of Madrid (Spain) approved the study, which was conducted according to the Helsinki Declaration for research on humans [18]. Before participating, players provided their written consent.
Anthropometrics
Height was measured using a stadiometer (DKSH Switzerland Ltd, Switzerland) to the nearest 0.1 cm in a standing position if possible, and for athletes who were unable to stand, the formula recommended by Canda [19] was applied to estimate height based on arm span and seated height. Body weight was determined using a calibrated scale (Kern, Twister Medical, Spain) to the nearest 0.1 kg with athletes wearing minimal clothing.
Diet composition
Diet compositions were estimated using a food-weighing diary (1 g accuracy; Mettler-Toledo S.A.E, Barcelona, Spain) over three consecutive days during each camp. Experienced researchers weighed and recorded each food component at breakfast, lunch and dinner. The players orally reported the types and quantities of snacks consumed outside of the main meal times and the time of day they were consumed. Likewise, supplement intake for each player was determined, and players provided leaflets, labels or packaging information. To analyze micronutrient intake from food alone, the intake due to supplements was determined separately. During each camp, the players ate together at the Centre of Higher Sport Council, selecting their food from a buffet offering a wide variety of food options. Occasionally some players chose to eat at home or outside the hotel area and orally reported the types and quantities of food they have consumed. The software program DIAL version 2 (Alce Ingeniera, Madrid, Spain) was used to determine the nutrient composition of the meals. The recipes of each meal were discussed with the kitchen staff to identify the separate food components so that they could be assigned to food groups, and recipes not already included in the food composition database were added. The weights of the food components were then entered into DIAL to analyze diet composition and categorize the components into fourteen food groups (S1 Table).
Adequacy of micronutrient intake
Ten vitamins (vitamin A, thiamin, riboflavin, niacin, vitamin B6, folic acid and vitamin B12 vitamin C, vitamin D and vitamin E) and seven minerals (calcium, iodine, iron, magnesium, phosphorus, selenium and zinc) of special relevance to athletes were examined [4, 5]. Individual intake was determined using the probability approach recommended by the American Dietetic Association [20, 21]. Furthermore, to determine intake adequacy at the group level, the Estimated Average Requirements (EAR)-cutpoint method with the latest DRI values from the FNB was applied [20–22]. According to the definition of the DRI, a probability of micronutrient intake of 50% corresponds with the EAR, and a probability of 100% corresponds with the Recommended Dietary Allowance (RDA) [21]. The Tolerable Upper Intake Level (UL) was set as the highest safe limit [14]. If the calculated probability of adequate intake for a micronutrient was stable at 100%, the amount in grams was used as the intake level instead of the probability. This was the case for niacin, riboflavin, vitamin B6, vitamin B12, iron, phosphorus and selenium. In our study, the sum of all micronutrients with a probability of at least 50% (adequacySUM) was calculated as the overall adequacy score to determine longitudinal improvement levels.
Nutritional advice
After each of the three nutritional evaluations (T1, T2, T3), individual written reports and personal interviews were conducted to optimize diet composition and micronutrient intake (i.e., daily amounts, food group variation, pre- and post-exercise snacks). All evaluations were held under the same conditions and during the same time of the year. Individual feedback was provided after each evaluation.
Resting energy expenditures were estimated according to Abel et al. [23], and energy expenditures were calculated using written activity protocols and values provided by Collins et al. [24] for athletes with SCI and by Abel et al. [23] and Bernardi et al. [25] for amputees.
Statistics
Normal distributions were tested for using the Shapiro-Wilk test and the Kolmogorov-Smirnov test. Pearson and Spearman correlations were computed for parametric and non-parametric data, respectively, to determine the linear relation between energy and micronutrient intake. Stepwise multiple linear regressions were conducted for each micronutrient intake as a dependent variable, and food groups were used as independent variables so that we could determine the relationship between micronutrient intake and dietary variation. Differences in micronutrient intake between all three evaluations were tested via analyses of variance (ANOVA) with repeated measurements for parametric data or via Friedman tests for non-parametric data. For post hoc tests we used paired Student’s t-tests for parametric data and Wilcoxon tests for non-parametric data, using Bonferroni corrections with partial eta-squared (η2) and Kendall’s W to represent the effect size, respectively. Parametric data are given as the mean ± standard deviation values and non-parametric as median [minimum; maximum] values. Significance was accepted at p < .05, and all tests were performed using SPSS version 22 (IBM Corp., Armonk, NY, USA).
Results
Participants
Characteristics for each player (5 amputees and 12 athletes with spina bifida or SCI, age 30 [22;41] years) are shown in Table 1.
Table 1. Player characteristics and diet composition shown as the mean values over the number of diaries.
| Player | Number of diaries | Height (cm) | Weight (kg) | BMI (kg/m2) | SCI or amputee |
|---|---|---|---|---|---|
| 1 | 1 | 189 | 84.0 | 23.5 | Amputee |
| 2 | 3 | 181 | 102.8 | 31.4 | Amputee |
| 3 | 2 | 187 | 88.5 | 25.3 | Amputee |
| 4 | 3 | 186 | 76.8 | 22.2 | Amputee |
| 5 | 2 | 183 | 75.3 | 22.5 | Amputee |
| 6 | 3 | 182 | 88.2 | 26.6 | SCI |
| 7 | 2 | 178 | 76.8 | 24.2 | SCI |
| 8 | 3 | 170 | 73.9 | 25.6 | SCI |
| 9 | 2 | 171 | 61.9 | 21.2 | SCI |
| 10 | 1 | 190 | 82.3 | 22.8 | SCI |
| 11 | 3 | 175 | 75.3 | 24.6 | SCI |
| 12 | 3 | 184 | 69.9 | 20.6 | SCI |
| 13 | 3 | 170 | 46.7 | 16.1 | SCI |
| 14 | 1 | 186 | 74.1 | 21.4 | SCI |
| 15 | 1 | 176 | 69.0 | 22.3 | SCI |
| 16 | 1 | 173 | 65.0 | 21.7 | SCI |
| 17 | 3 | 183 | 70.6 | 21.1 | SCI |
| 182 [170;190] | 75.5±13.5 | 23.3±3.7 |
BMI, body mass index; SCI, spinal cord injury
Diet composition
Overall, 37 food diaries were examined. Mean energy intake was 2,673±485 kcal/d (1,597 to 3,651 kcal/d) and 36.8±10.5 kcal/kg (24.6 to 63.5 kcal/kg). Macronutrient intake relative to body mass was 3.9 [1.8;8.1] g/kg for carbohydrates and 1.7±0.6 g/kg for protein, excluding supplements. The percentage of energy derived from fat was 33.7±5.5%.
Micronutrient intake
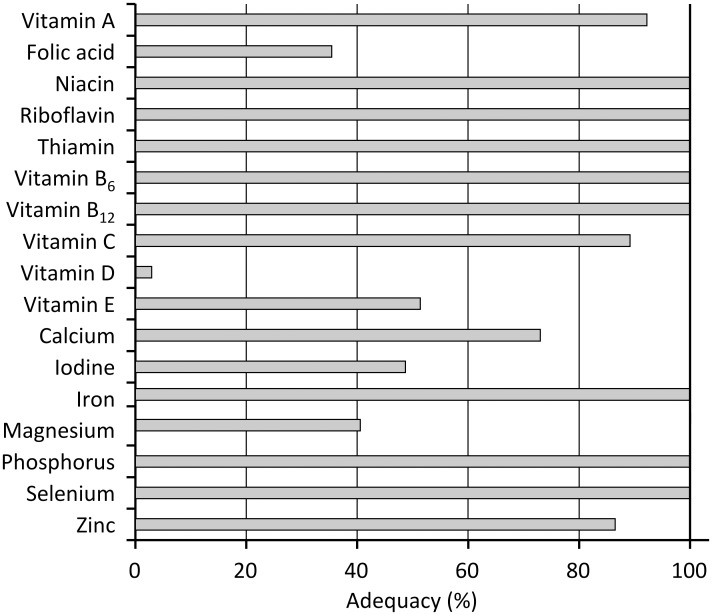
The estimated adequate intake probabilities at the group level are shown in Fig 2. The levels shown exceed the RDA for niacin, riboflavin, vitamin B6 and vitamin B12 and for various minerals (iron, phosphorus, and selenium) for all the players. No player exceeded the UL for any micronutrient. AdequacySUM was found to be 13.2±2.0, with no player achieving adequate intake levels for all 17 micronutrients but with 35% taking in adequate levels for 16 micronutrients.
Fig 2. Probability of adequate micronutrient intake.
One player used supplements on all three occasions, achieving adequate calcium and vitamin D levels for Training Camp T1 and adequate intake levels for all micronutrients and calcium for Training Camp T2. Two players used mineral supplements on one occasion, achieving levels of calcium above adequacy.
The correlation of total energy intake with adequacySUM and micronutrient intake adequacy is shown in Table 2.
Table 2. Correlation between total energy intake and the probability of adequate micronutrient intake.
| Correlation coefficient | p-Value | |
|---|---|---|
| AdequacySUM | 0.64 | <0.001 |
| Vitamins | ||
| Vitamin A | 0.29 | 0.087 |
| Folic acid | 0.50 | 0.002 |
| Niacin (mg)a | 0.59 | <0.001 |
| Riboflavin (mg)a | 0.63 | <0.001 |
| Thiamin | 0.44 | 0.006 |
| Vitamin B6 (mg)a | 0.59 | <0.001 |
| Vitamin B12 (μg)a | 0.53 | <0.001 |
| Vitamin C | 0.33 | 0.044 |
| Vitamin D | 0.54 | <0.001 |
| Vitamin E | 0.29 | 0.082 |
| Minerals | ||
| Calcium | 0.44 | 0.006 |
| Iodine | 0.64 | <0.001 |
| Iron (mg)a | 0.53 | <0.001 |
| Magnesium | 0.55 | <0.001 |
| Phosphorus (mg)a | 0.65 | <0.001 |
| Selenium (μg)a | 0.41 | 0.013 |
| Zinc | 0.59 | <0.001 |
a The probability of adequate intake is constant at 100%
Players with higher adequacySUM levels consumed more fruit, dairy, fat, oil, and cereals (Table 3).
Table 3. Beta coefficients of stepwise multiple linear regressions with the probability of adequate micronutrient intake as a dependent variable and energy intake levels from different food groups as independent variables.
| R2 | Cereals | Legumes | Vegetables | Fruits | Dairy | Meats | Fish | Eggs | Sugars and sweets | Fats and oils | Beverages | Prepared meals | Appetizers | Sauces | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AdequacySUM | 0.72 | 0.27 | 0.58 | 0.22 | 0.42 | ||||||||||
| Vitamins | |||||||||||||||
| Vitamin A | 0.25 | 0.36 | -0.30 | ||||||||||||
| Folic acid | 0.71 | 0.30 | 0.66 | 0.40 | 0.33 | -0.25 | |||||||||
| Niacin (mg)a | 0.87 | 0.24 | 0.29 | 0.21 | 0.66 | 0.38 | 0.21 | ||||||||
| Riboflavin (mg)a | 0.54 | 0.43 | 0.49 | 0.38 | |||||||||||
| Thiamin | 0.26 | 0.51 | |||||||||||||
| Vitamin B6 (mg)a | 0.49 | 0.35 | 0.30 | 0.44 | |||||||||||
| Vitamin B12 (μg)a | 0.85 | 0.30 | 0.55 | 0.64 | 0.26 | 0.26 | |||||||||
| Vitamin C | 0.50 | 0.30 | -0.38 | -0.41 | |||||||||||
| Vitamin D | 0.24 | 0.49 | |||||||||||||
| Vitamin E | 0.62 | 0.50 | 0.51 | -0.27 | |||||||||||
| Minerals | |||||||||||||||
| Calcium | 0.40 | 0.63 | |||||||||||||
| Iodine | 0.61 | 0.36 | 0.41 | 0.46 | -0.27 | ||||||||||
| Iron (mg)a | 0.55 | 0.39 | 0.35 | 0.48 | 0.40 | ||||||||||
| Magnesium | 0.67 | 0.51 | 0.42 | 0.27 | |||||||||||
| Phosphorus (mg)a | 0.75 | 0.38 | 0.34 | 0.29 | 0.41 | 0.30 | |||||||||
| Selenium (μg)a | 0.66 | 0.37 | -0.21 | 0.60 | |||||||||||
| Zinc | 0.21 | 0.46 |
a The probability of adequate intake was constant at 100%
Effects of nutritional advice
Anthropometric data and diet compositions for the eight players who took part in all three evaluations are shown in Table 4. Although body weight and BMI levels changed significantly over time, post hoc tests showed no significance. Total energy intake increased significantly during the evaluation at T3 relative to values recorded for T1 (p = .017) and T2 (p = .046). Similar results were found for fruit (p = .032, η2 = 0.39) and egg intake levels (p = .036, Kendall’s W = 0.42), although significant post hoc test results were not found.
Table 4. Anthropometric data and diet compositions for the eight players who took part in all three evaluations.
| Parameter | Training Camp T1 | Training Camp T2 | Training Camp T3 | p-Value | η2 |
|---|---|---|---|---|---|
| Age (years) | 29.9±6.5 | 30.0±6.5 | 31.0±6.5 | --- | |
| Height (cm) | 178.9±6.3 | 178.9±6.3 | --- | ||
| Body weight (kg) | 75.0±16.2 | 74.3±15.6 | 77.3±16.5 | 0.029 | 0.40 |
| BMI (kg/m2) | 23.4±4.7 | 23.1±4.5 | 24.1±4.7 | 0.032 | 0.39 |
| Total energy intake (kcal/d) | 2441±341b | 2446±588a | 2968±453a,b | 0.009 | 0.49 |
| Carbohydrate (g/kg) | 3.1 [2.8;7.1] | 3.5 [1.8;8.1] | 4.9 [2.7;7.4] | 0.197 | |
| Protein (g/kg) | 1.6±0.7 | 1.5±0.5 | 1.9±0.7 | 0.071 | |
| Fat (%) | 35.1±4.7 | 33.7±4.8 | 32.1±5.9 | 0.599 | |
| Cholesterol (mg) | 401 [263;947] | 317 [226;518] | 669 [216;992] | 0.012 | 0.25 |
a T2 vs. T3 p < .05,
b T1 vs. T3 p < .05 BMI, body mass index
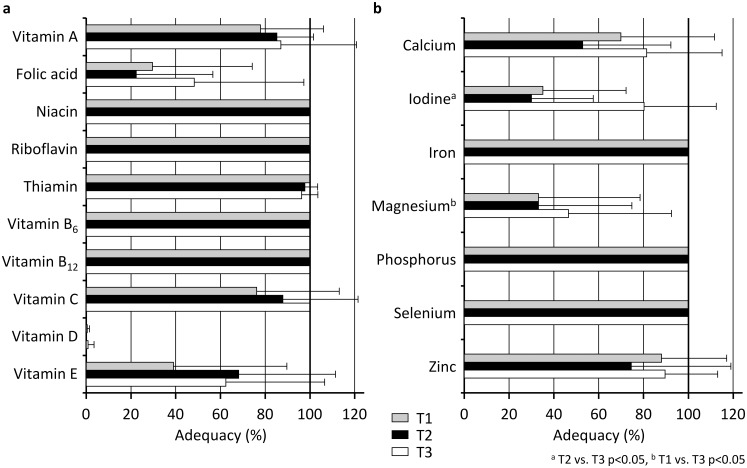
The probabilities of adequate micronutrient intake for the three evaluations are shown in Fig 3. Iodine (p = .008, W = 0.61; T1-T2 n.s., T2-T3 p = .035, T1-T3 p = .045) and magnesium (p = .030, W = 0.44; T1-T2 n.s., T2-T3 p = .788, T1-T3 p = .023) showed significant differences, with three players over the EAR for iodine at T1, one over at T2 and seven over at T3 and with three over the EAR for magnesium at T1, two over at T2 and three over the RDA at T3.
Fig 3. Probabilities of adequate vitamin (a) and mineral intake (b) for the eight players who took part in all three evaluations (T1, T2 and T3).
The adequacySUM values were 12.5±2.4 at T1, 12.3±1.8 at T2 and 14.0±1.7 at T3 (p = .039, η2 = 0.37, T1-T3 p = .043).
Discussion
Our study reveals a relationship between total energy intake and adequate micronutrient intake in male wheelchair basketball players. Additionally, it shows that a variety of food groups are needed for one to achieve adequate micronutrient intake.
Although a higher total energy intake among able-bodied athletes should result in adequate micronutrient intake [4, 5], it is less certain whether sufficient energy intake can help Paralympic athletes to achieve this goal. Athletes with SCI in particular often have a lower muscle mass than able-bodied athletes as a result of paralysis [26], which is caused by a reduction in sympathetic nervous system activity below the level of the lesion [27]. Together with lower activity levels or even immobility in the affected limbs, this leads to less active muscle mass, and therefore, their energy expenditure is likely to be lower than that of their able-bodied peers [28, 29]. Likewise, their total energy intake may be equally reduced to maintain energy balance, possibly resulting in inadequate micronutrient intake. Krempien and Barr [17] reported on the energy intake levels of male Canadian wheelchair athletes, and Goosey-Tolfrey and Crosland [15] reported similar results for male British wheelchair athletes. Both groups were found to have lower intake levels than able-bodied professional basketball players [30]. Although the mean total energy intake levels found in the present study are higher than those found for comparable disabled athletes [15, 17], the values ranged from 1,597 to 3,651 kcal/d, highlighting the need for individualized nutritional advice for athletes with different disabilities and even among those who play the same sport. Similarly, the participants in the present study varied in terms of body weight, explaining the similarly high variability in energy intake relative to body weight, which ranged from 25 to 64 kcal/kg.
However, total energy intake is not the only factor that affects the adequacy of micronutrient intake. For example, similar energy intake levels of 2,558 kcal/d and 2,479 kcal/d were found in our study between two players and resulted in the adequate intake of ten micronutrients for one player and sixteen for the other, with only vitamin D showing inadequate intake levels, which will be discussed later. Consequently, a varied diet is also important [4, 5]. In our study, intake of eleven of the fourteen food groups we examined (see detailed information in S1 Table) showed a positive correlation with adequate intake levels for at least one micronutrient. From these groups, four (cereals, fruits, dairy, and fats and oil) accounted for 72% of the variance in the overall adequacy of micronutrient intake (Table 3). Fruits were found to be associated with five vitamins and three minerals, fish were associated with four vitamins and three minerals, and cereals were associated with three vitamins and five minerals. Dairy was the only significant source of calcium intake found, even though we expected additional sources (e.g., specific vegetables or legumes) to play an important role as the food available in the buffet included all the necessary food groups to support optimal nutritional requirements.
Compared with the levels found in the study by Krempien and Barr [16] on male Canadian athletes with SCI, micronutrient intake levels were generally found to be higher in our study. This observation can partly be explained by the higher energy intake levels used (2,673±486 kcal/d) relative to those employed by Krempien and Barr (2,285 kcal/d) [16]. However, Krempien and Barr [16] did not consider issues relating to dietary variety, which we found to have a considerable effect. Comparisons between energy intake levels of non-athlete adults with SCI revealed even greater differences, with Perret and Stoffel-Kurt [31] reporting an energy intake of 1,775 kcal/d and lower absolute micronutrient intake levels, with the exception of those for calcium.
The dietary intake levels of our participants showed a high adequacy for 13.3±2.1 of the 17 micronutrients examined. Micronutrients involved in bone health, such as calcium, magnesium and vitamin D, showed low adequacy levels, and the levels of phosphorus were high in relation to those of calcium [32], which could negatively affect progress among wheelchair athletes who are susceptible to osteoporosis [11]. Only one player, an amputee, used a multivitamin and mineral supplement that included calcium and vitamin D, which provided adequate levels of both micronutrients for this individual.
However, the DRI for vitamin D represents intake levels under minimal sun exposure conditions, and in the summer, the endogenous synthesis of vitamin D in Madrid, Spain, (40° in latitude) is achieved with 10 minutes of daily sunlight exposure. Nonetheless, limited sun exposure can occur because of the season and at latitudes higher than 35°. In such cases, calcium and vitamin D supplements should be considered during fall and winter and especially for athletes presenting low total energy intake levels.
In addition to improve performance, micronutrients play an important role in enhancing immune function, and illness can result in players being absent from training and competition [15, 33]. To prevent the spread of illness and to support immune system health, ensuring adequate levels of vitamins A, D, E, C, B6, and B12, as well as folic acid, iron and zinc should be of great concern [34, 35]. In our study, vitamin B6 and vitamin B12 intake levels were found to be adequate as animal food groups were well represented and no player followed a vegetarian diet. Vitamin A, vitamin C, iron and zinc intake levels were above their EAR. Various food groups served as significant sources of vitamin A and iron, although only fruits served as sources of vitamin C, and only cereals served as sources of zinc. Regarding the low adequacy levels of vitamin E and folic acid intake, a higher intake of nutrient-dense legumes may prove beneficial, as legumes are good sources of these micronutrients. However, due to the low legume intake in this study, legumes were not found to serve as a significant source of any micronutrient. Although digestion is slower in players with SCI [36] and certain food groups induce flatulence, it seems likely that some legumes or vegetables (e.g., boiled greens, potatoes, carrots and alliums) offered as purees would be easier to digest and could be beneficial nutrient-dense foods. In this regard, individual solutions should be found [6] and discussed between the athlete and nutritionist.
Nutritional advice was found to increase the overall adequacy of micronutrient intake after one year, which can be attributed to a higher total energy intake and to a more varied diet characterized by the higher fruit and egg intake of our participants. Considering the marginal differences found after the second training camp (T2), which was only four weeks after the first (T1), it appears that eating habits take time to change and that advice should be given more frequently than it was in our study to achieve adequate micronutrient intake. Even a nutrition education program involving three sessions over four months did not improve micronutrient intake among able-bodied professional handball players [37], despite the fact that the motivation of elite athletes should be high to support effective training and to improve performance levels during training and competition. Despite lower levels of cholesterol intake found after four weeks (T2), our data revealed an increasing trend after one year (T3) (Table 4). This finding could partly be explained by a higher egg intake, which on the one hand led to a high protein intake but on the other hand led to a cholesterol intake that was above the recommended amount (Table 4). Our recommendations to increase the consumption of fat-free and fat-reduced dairy products were not followed over a full year. Consequently, nutritional advice seems more effective when provided over a shorter timeframe.
Study Limitations
Although the DRI values were used to study the intake adequacy of all micronutrients, our analysis conducted over three consecutive days may have been too short to fully analyze the requirements for some micronutrients [21]. Other potential reasons for intake deficiencies (e.g., the bioavailability of micronutrients) were not examined in this study and should be considered before vitamin or mineral supplements are recommended. Blood analyses must also be conducted when confirming inadequate intake. In regards to vitamin D status, varying levels of sun exposure across seasons have a considerable effect on the endogenous synthesis, and therefore, supplements may prove beneficial during fall and winter but are likely unnecessary during spring and summer. Finally, the micronutrient contents in food are unstable, so the actual levels taken in may be different than we estimated, and some of our data on nutrient content may have been inaccurate as food databases do not include the chemical compositions of all available foods.
Conclusion
The adequacy of the micronutrient intake by elite male Spanish wheelchair basketball players is positively related to their total energy intake. However, a variety of food groups must be included in one’s diet to achieve adequate levels for the most important micronutrients, and nutrient-dense food groups such as fruit are associated with more micronutrients than less nutrient-dense groups. As some micronutrients showed inadequate intake levels, additional nutritional advice should be provided to avoid adverse effects resulting from personal dislike of certain food groups, and the consumption of beneficial foods (especially vegetables and legumes prepared in ways that are easy to digest) should be promoted as some of these groups, legumes in particular, were only consumed in minimal amounts. In addition, shorter time frames between nutritional advice are more successful than longer periods, such as one year.
Food variety with special attention to nutrient-dense foods is especially important in players with low energy intake. Consequently, it might be necessary to use supplements for players with SCI, especially for micronutrients involved in bone health. Nutritional monitoring in Paralympic athletes should be incorporated into the regular routine of their training periods throughout the year so that a short time frame between repeated sessions of receiving nutritional advice can be used to raise their knowledge of the benefits of sports nutrition.
Supporting Information
(DOCX)
Acknowledgments
We thank the Higher Sport Council (CSD) for their support and the Spanish Sports Federation for People with Physical Disabilities (FEDDF) and their wheelchair basketball players for participating in the study.
Data Availability
Data is available on request from the Ethics Committee of the Technical University of Madrid (Spain). The publicly available roster of the male Spanish Wheelchair Basketball National Team precludes public data deposition, because the participants could be identifiable from additional data such as age or impairment which would compromise participant privacy.
Funding Statement
This study was supported by the Ministry of Economy and Competitiveness’ (MINECO) National Plan R&D&I 2012-2016 (DEP2012-38785). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Perret C. Elite-adapted wheelchair sports performance: a systematic review. Disabil Rehabil 2015. October 27;Oct 27:1–9. [DOI] [PubMed] [Google Scholar]
- 2.Goosey-Tolfrey V. Supporting the paralympic athlete: focus on wheeled sports. Disabil Rehabil 2010;32(26):2237–2243. 10.3109/09638288.2010.491577 [DOI] [PubMed] [Google Scholar]
- 3.Broad E, Burke L. Principles of Sports Nutrition In: Broad E, editor. Sports Nutrition for Paralympic Athletes. 1st ed Baco Raton; FL: CRC Press; 2014. p. 23–66. [Google Scholar]
- 4.American Dietetic Association, Dietitians of Canada, American College of Sports Medicine, Rodriguez NR, Di Marco NM, Langley S. American College of Sports Medicine position stand. Nutrition and athletic performance. Med Sci Sports Exerc 2009. March;41(3):709–731. 10.1249/MSS.0b013e31890eb86 [DOI] [PubMed] [Google Scholar]
- 5.Kreider RB, Wilborn CD, Taylor L, Campbell B, Almada AL, Collins R, et al. ISSN exercise & sport nutrition review: research & recommendations. J Int Soc Sports Nutr 2010. February 2;7:7-2783-7-7. [Google Scholar]
- 6.Thomas DT, Erdman KA, Burke LM. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and Athletic Performance. J Acad Nutr Diet 2016. March;116(3):501–528. 10.1016/j.jand.2015.12.006 [DOI] [PubMed] [Google Scholar]
- 7.Deakin V. Micronutrients In: Lanham-New SA, Stear SJ, Shirreffs SM, Collins AL, editors. Sport and Exercise Nutrition. 1st ed Oxford, UK: Wiley-Blackwell; 2011. p. 66–88. [Google Scholar]
- 8.Halliday TM, Peterson NJ, Thomas JJ, Kleppinger K, Hollis BW, Larson-Meyer DE. Vitamin D status relative to diet, lifestyle, injury, and illness in college athletes. Med Sci Sports Exerc 2011. February;43(2):335–343. 10.1249/MSS.0b013e3181eb9d4d [DOI] [PubMed] [Google Scholar]
- 9.Ruohola JP, Laaksi I, Ylikomi T, Haataja R, Mattila VM, Sahi T, et al. Association between serum 25(OH)D concentrations and bone stress fractures in Finnish young men. J Bone Miner Res 2006. September;21(9):1483–1488. [DOI] [PubMed] [Google Scholar]
- 10.Goktepe AS, Yilmaz B, Alaca R, Yazicioglu K, Mohur H, Gunduz S. Bone density loss after spinal cord injury: elite paraplegic basketball players vs. paraplegic sedentary persons. Am J Phys Med Rehabil 2004. April;83(4):279–283. [DOI] [PubMed] [Google Scholar]
- 11.Miyahara K, Wang DH, Mori K, Takahashi K, Miyatake N, Wang BL, et al. Effect of sports activity on bone mineral density in wheelchair athletes. J Bone Miner Metab 2008;26(1):101–106. [DOI] [PubMed] [Google Scholar]
- 12.Flueck JL, Hartmann K, Strupler M, Perret C. Vitamin D deficiency in Swiss elite wheelchair athletes. Spinal Cord 2016. March 15:In press. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine (US: ) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Dietary Reference Intakes for Calcium and Vitamin D. 2011. [Google Scholar]
- 14.National Research Council. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 15.Goosey-Tolfrey VL, Crosland J. Nutritional practices of competitive British wheelchair games players. Adapt Phys Activ Q 2010. January;27(1):47–59. [DOI] [PubMed] [Google Scholar]
- 16.Krempien JL, Barr SI. Risk of nutrient inadequacies in elite Canadian athletes with spinal cord injury. Int J Sport Nutr Exerc Metab 2011. October;21(5):417–425. [DOI] [PubMed] [Google Scholar]
- 17.Krempien JL, Barr SI. Eating attitudes and behaviours in elite Canadian athletes with a spinal cord injury. Eat Behav 2012. January;13(1):36–41. 10.1016/j.eatbeh.2011.11.005 [DOI] [PubMed] [Google Scholar]
- 18.Williams JR. The Declaration of Helsinki and public health. Bull World Health Organ 2008. August;86(8):650–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canda A. Stature estimation from body segment lengths in young adults—application to people with physical disabilities. J Physiol Anthropol 2009. March;28(2):71–82. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine (US) Subcommittee on Interpretation and Uses of Dietary Reference Intakes, Institute of Medicine (US: ) Standing Committee on the Scientific; Evaluation of Dietary Reference Intakes. DRI Dietary Reference Intakes: Applications in Dietary Assessment. 2000. [PubMed] [Google Scholar]
- 21.Murphy SP, Barr SI. Practice paper of the American Dietetic Association: using the Dietary Reference Intakes. J Am Diet Assoc 2011. May;111(5):762–770. 10.1016/j.jada.2011.03.022 [DOI] [PubMed] [Google Scholar]
- 22.Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. 2001. [Google Scholar]
- 23.Abel T, Platen P, Rojas Vega S, Schneider S, Struder HK. Energy expenditure in ball games for wheelchair users. Spinal Cord 2008. December;46(12):785–790. 10.1038/sc.2008.54 [DOI] [PubMed] [Google Scholar]
- 24.Collins EG, Gater D, Kiratli J, Butler J, Hanson K, Langbein WE. Energy cost of physical activities in persons with spinal cord injury. Med Sci Sports Exerc 2010. April;42(4):691–700. 10.1249/MSS.0b013e3181bb902f [DOI] [PubMed] [Google Scholar]
- 25.Bernardi M, Guerra E, Di Giacinto B, Di Cesare A, Castellano V, Bhambhani Y. Field evaluation of paralympic athletes in selected sports: implications for training. Med Sci Sports Exerc 2010. June;42(6):1200–1208. 10.1249/MSS.0b013e3181c67d82 [DOI] [PubMed] [Google Scholar]
- 26.Glaser RM. Exercise and locomotion for the spinal cord injured. Exerc Sport Sci Rev 1985;13:263–303. [PubMed] [Google Scholar]
- 27.Leicht CA, Bishop NC, Goosey-Tolfrey VL. Submaximal exercise responses in tetraplegic, paraplegic and non spinal cord injured elite wheelchair athletes. Scand J Med Sci Sports 2012. December;22(6):729–736. 10.1111/j.1600-0838.2011.01328.x [DOI] [PubMed] [Google Scholar]
- 28.Croft L, Dybrus S, Lenton J, Goosey-Tolfrey V. A comparison of the physiological demands of wheelchair basketball and wheelchair tennis. Int J Sports Physiol Perform 2010. September;5(3):301–315. [DOI] [PubMed] [Google Scholar]
- 29.Price M. Energy expenditure and metabolism during exercise in persons with a spinal cord injury. Sports Med 2010. August 1;40(8):681–696. 10.2165/11531960-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 30.Bescos Garcia R, Rodriguez Guisado FA. Low levels of vitamin D in professional basketball players after wintertime: relationship with dietary intake of vitamin D and calcium. Nutr Hosp 2011. Sep-Oct;26(5):945–951. 10.1590/S0212-16112011000500004 [DOI] [PubMed] [Google Scholar]
- 31.Perret C, Stoffel-Kurt N. Comparison of nutritional intake between individuals with acute and chronic spinal cord injury. J Spinal Cord Med 2011. November;34(6):569–575. 10.1179/2045772311Y.0000000026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Calvo MS, Tucker KL. Is phosphorus intake that exceeds dietary requirements a risk factor in bone health? Ann N Y Acad Sci 2013. October;1301:29–35. 10.1111/nyas.12300 [DOI] [PubMed] [Google Scholar]
- 33.Derman W, Schwellnus M, Jordaan E. Clinical characteristics of 385 illnesses of athletes with impairment reported on the WEB-IISS system during the London 2012. Paralympic Games. PM R 2014 Aug;6(8 Suppl):S23–30. [DOI] [PubMed]
- 34.Gleeson M. Nutritional support to maintain proper immune status during intense training. Nestle Nutr Inst Workshop Ser 2013;75:85–97. 10.1159/000345822 [DOI] [PubMed] [Google Scholar]
- 35.Hemila H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev 2013. January 31;1:CD000980 10.1002/14651858.CD000980.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin VW, Kim KH, Hsiao I, Brown W. Functional magnetic stimulation facilitates gastric emptying. Arch Phys Med Rehabil 2002. June;83(6):806–810. [DOI] [PubMed] [Google Scholar]
- 37.Molina-Lopez J, Molina JM, Chirosa LJ, Florea D, Saez L, Jimenez J, et al. Implementation of a nutrition education program in a handball team; consequences on nutritional status. Nutr Hosp 2013. Jul-Aug;28(4):1065–1076. 10.3305/nh.2013.28.4.6600 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Data is available on request from the Ethics Committee of the Technical University of Madrid (Spain). The publicly available roster of the male Spanish Wheelchair Basketball National Team precludes public data deposition, because the participants could be identifiable from additional data such as age or impairment which would compromise participant privacy.