Abstract
Clinical examination techniques need to allow the physician to determine the underlying pathology of a patient’s condition with confidence. This review examines the evidence for two common conditions: impingement and rotator cuff disease
Keywords: Evidence, examination, shoulder; tests
Introduction
The purpose of any examination is to allow the clinician to establish the anatomical, pathological and functional conditions of a patient. The examination should be able to determine the underlying causes of the presenting problem with confidence and assurity. The techniques used must give, where possible, a clarification of the suspected derangement, and the examiner must be aware of the possibility that the tests employed may misdirect a diagnosis by giving a falsely positive finding. The purpose of the development of many examination tests has been to try to focus down on specific anatomical structures, and to improve the reliability of the test in defining the structural integrity of the tissue, and its function. The present review aims to guide the examiner to utilize tests that provide both confidence in their ability to determine the problem, and that are reproducible over a period of time, allowing comparison between one examination and another, thus giving an accuracy of the progress of a condition. Clearly, there are subjective elements to any examination, with the most obvious being pain, although the objective findings still help in directing diagnosis.
This review article aims to look at the examination techniques used to diagnose two common conditions: subacromial impingement and rotator cuff disease.
The rotator cuff complex is defined as a group of tendons that envelope the humeral head, arising from four muscles that have their origin on the scapula. These muscles, subscapularis, supraspinatus, infraspinatus and teres minor, act in synergy as the glenohumeral joint is utilized to allow positioning of the hand in space for function. Their primary role appears to be stabilizing the humeral head on the glenoid surface, ensuring that it remains centred as the head rotates in all the different planes of movement required. Pure internal and external rotation of the humeral head does not involve any cranial translational force, yet these movements are rarely needed in isolation. The function of the more superiorly placed tendon fibres appears to both aid abduction initiation of the humeral head and resist cranial translation of the head as the shoulder continues to elevate the arm. Thus, any dysfunction of the tendon complex is likely to lead to an upward movement of the head as the arm is actively raised, which will inevitably cause an increase contact pressure of both the upper surface of the tendon and the interposed subacromial bursa upon the undersurface of the acromion and the coraco-acromial ligament1.
Although this cause for pain is intrinsic to the tendon itself, regardless of whether it is caused by inflammation (with or without calcification) or partial and full-thickness tears, there may also be extrinsic causes, such as an alteration in the dimensions of the subacromial space (as is found with the differing morphological types of acromial development)2, hypertrophy of the coraco-acromial ligament3 or bursal anomalies such as a plica4 or thickening5 from repeated episodes of inflammation, or regional thickening of the tendons themselves, as found in chronic calcinosis after episodes of acute calcific tendinitis6. Finally, the complex dynamic coordination of scapular movements as the arm is elevated can give rise to pain from the subacromial structures7. The diagnosis of impingement aims to isolate the pathological process to the subacromial space; it does not, however, define the cause.
Subacromial impingement
Impingement syndrome is characterized by pain experienced through an arc of elevation as the shoulder abducts. It should be appreciated that this is a condition that is associated with active movement of the shoulder (after all, the patient never functionally lifts the arm passively), so it occurs when the subacromial structures are actively brought into contact with the acromion and coracoacromial ligament during the act of elevating the arm.
The two most commonly used tests for impingement are Neer's Sign and the Hawkins–Kennedy test8,9.
Neer’s sign
This test allows demonstration of a pain during passive abduction of the arm with the scapula stabilized, the examiner lifting the arm in the scapular plane with the arm internally rotated (Figure 1). It was described originally in 1977, and did not as such describe an ‘arc’ of pain. However, a painful arc through abduction is often associated with the eponym. As a supplementary part to this manoeuvre, the effect on the pain following an injection of local anaesthetic placed into the subacromial space is called Neer's test. A significant reduction or abolition of the pain is seen as a positive test.
Figure 1.

Neer.
Hawkins–Kennedy test
Described in 1980, this test is again a passive test, with the examiner positioning the patient's arm at 90° in the scapular plane, the elbow bent to 90°, and the arm taken passively into internal rotation. Creation of pain during this maneuver is indicative of a positive test (Figure 2).
Figure 2.
Hawkins–Kennedy.
The two tests differ in relation to the position of the humeral head below the acromion. Pappas et al. determined the in vivo relationship of the insertion of the supraspinatus tendon with magnetic resonance imaging using both tests, demonstrating that the Hawkins–Kennedy test caused both an increased incidence of, and a greater decrease in, the distance of the supraspinatus to the acromion than Neer’s sign10.
A recent pooled data analysis from Hegedus et al. has shown the sensitivity (a true positive) of each of the tests varies (79% for Hawkins–Kennedy; 72% for Neer’s test) but, importantly, specificity (the statistical ability of a test to be negative when a defined pathological condition is not present) is lower, calculated at 59% and 60%, respectively11. Hegedus et al. also used a similar meta-analysis including a number of studies to demonstrate that, although neither test had sufficient sensitivity to diagnose impingement, there was evidence to conclude that a negative Hawkins–Kennedy test was sufficiently powerful to rule it out. Conditions such as acromioclavicular arthrosis, superior labral tears, internal impingement and even Bankart lesions may also yield positive tests12.
Lim et al. investigated the prognostic use of a subacromial injection when a diagnosis of impingement had been made, and a subacromial decompression was considered as a surgical option. They found that there was a significant correlation between the positive effect of the injection of the local anaesthetic and a good surgical outcome, considering both symptom improvement and the length of the postoperative recovery13.
Rotator cuff disease
The tests that aim to diagnose rotator cuff disease are numerous. The examiner should attempt to separate out the individual tendons that comprise the cuff to determine the integrity of the tendon. True isolation of the individual tendons is almost impossible because of the coupling effects across the rotator cuff complex. This is especially so when the superior cuff (the supraspinatus and infraspinatus) in conjunction with the long head of biceps tendon are being considered14. The exception appears to be the ability to isolate subscapularis.
Pain elicited from these tests may be a result of either tendinitis/tear or subacromial impingement. Differentiation between tendinitis and a small tear (partial thickness or full thickness) is often difficult. Tears that involve a significant proportion of a tendon will tend to show signs of weakness, although the clinician must be aware that, even in the presence of a large or massive rotator cuff defect, the patient may still only demonstrate mild or subtle signs15. This is a result of the ability of the shoulder to compensate for the absence of part of the rotator cuff with residual intact cuff and surrounding intact muscles.
In the determination of an accurate assessment from each test, two basic requirements are adequate pain relief (else pain inhibition may mimic true weakness) and a sufficient range of passive movement to allow appropriate positioning of the arm in which to perform the test.
Supraspinatus
Jobe’s empty can test was first described in 1983. This sets out to preferentially test supraspinatus (complete isolation of supraspinatus from the deltoid is difficult), the most commonly affected tendon when considering degenerative cuff disease. It positions the arm such that the supraspinatus tendon is placed under maximal stress as the arm is pushed down, attempting to invoke pain, weakness, or both, from the examination. It does not, however, completely isolate supraspinatus, and some fibres from the anterior part of infraspinatus are also tested.
The arm is flexed to 90°in the scapular plane and the forearm maximally pronated, so internally rotating the shoulder joint (the classical ‘thumbs down’ position). This position of internal rotation disadvantages the action of deltoid, so improving the accuracy of testing supraspinatus. Pressure is applied to the arm and any pain or weakness recorded (Figure 3). The examiner should note where the pain is because it is not uncommon for this test to produce pain in the common extensor origin at the elbow, especially if pressure is applied distal to the elbow joint. Some examiners therefore exert pressure above the elbow, aiming to minimize the effect of triceps extending the elbow and compensating for an absent supraspinatus. This can be performed unilaterally or with both arms tested at the same time for comparison. Some examiners prefer to have less flexion at the shoulder when performing the test. This maybe to reduce the possibility of causing an inadvertent impingement position, and thus a falsely positive outcome if pain appears to be the main feature.
Figure 3.

Jobe.
Park et al. calculated the sensitivity of the empty can test to be 44% but with a specificity of 90%16. This gives the test significant validity but it should be noted that, although the review stated a positive predictive value (PPV) of 88%, it was almost 50% when the negative predictive value was calculated16. This may reflect the anatomical ability of the rotator cuff complex to ‘balance’ a tear, as was suggested by Burkhart17, and may help explain why a significant number of patients remain asymptomatic despite a supraspinatus tear being confirmed on a shoulder scan.
An additional examination is the lateral Jobe test which has a reported 81% sensitivity and 89% specificity, with a PPV of 91%, and should considered a useful addition to the examination18.
Infraspinatus
Hertel in 1996 described the ‘external rotation lag sign’ to diagnose an infraspinatus tear. This test sets out to examine the posterosuperior and posterior cuff elements. It was originally described to evaluate infraspinatus19. The arm is held in 20° of flexion with the elbow bent to 90°. The forearm is passively externally rotated to its maximal range and released. If the arm drops back towards its starting position, even by a few degrees, it is said to have a lag (‘the lag sign’) (Figure 4). The ability of the patient to maintain the arm fully externally rotated implies the effectiveness of the cuff structures, mostly infraspinatus, but, with the element of forward flexion, there is also an element of supraspinatus activity with the test, and so pain may be present even if no lag is recorded.
Figure 4.

External rotation lag.
It should be noted that this test can only be both sensitive and specific when a normal range of external rotation is demonstrated by the patient. With a capsular contraction, the patient loses external rotation, and so they cannot achieve a position in which the rotator cuff tendons can be induced to produce a lag through weakness. Similarly, if there is excessive external rotation (as might be seen in a subscapularis rupture), the passive external rotation of the shoulder will be greater than normal, and a falsely positive lag sign may be elicited.
An additional sign useful for the clinician (as it relates directly to the functional capacity of a patient in activities of daily living) is the drop-arm sign. The patient may be able to elevate the arm to near full range, although often they require assistance to do this (either using their other arm to lift the affected side upward, or needing active help from the examiner) but, when asked to lower the arm slowly back to a resting position, they lose control of the descent through a mid-arc range, and the speed of the lowering increases until it reaches a comfortable resting position again. This sign is often but not always associated with pain as the arm is lowered. It is indicative of a large superior cuff tear involving both supraspinatus and infraspinatus in combination.
Teres minor
The examination of the posterior cuff is the hornblower sign20. The arm is placed passively by the examiner in 90° of abduction and maximal external rotation. The patient is instructed to attempt to maintain the hand in space when the examiner releases the hold on the wrist. If the patient’s arm falls forwards, this is a positive test, and indicates significant weakness of infraspinatus and usually teres minor (Figure 5). If the patient can maintain the position of the arm, gentle forward pressure on the forearm may cause pain, and indicate the presence of a small tear involving infraspinatus.
Figure 5.

Hornblower.
Subscapularis
Testing subscapularis involves the evaluation of the patient’s ability to forcibly internally rotate the humerus. This can be achieved either in front (the belly press test and bear-hug test) or behind (Gerber’s lift-off test) the body. It must be appreciated that, to achieve a satisfactory examination, the patient must be able to comfortably position their arm in the required place and, although this is rarely a problem with a test performed in front of the body, any loss of internal rotation and/or extension of the shoulder may prevent the patient being able to place the hand behind the back, and thus perform the test.
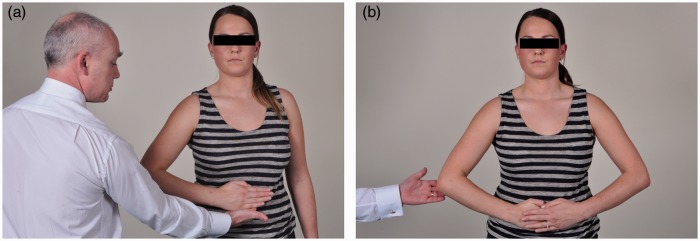
Belly press test (Napoleon sign)
This involves the hand (or hands if done bilaterally) being placed flat on the abdomen, and the patient is requested to press the hand onto the stomach. If the patient is unable to maintain the elbow forward, so extending the shoulder and flexing the wrist to achieve the desired pressure, this indicates a positive test21 (Figure 6).
Figure 6.
Belly-press. (a) One hand. (b) Bilaterally.
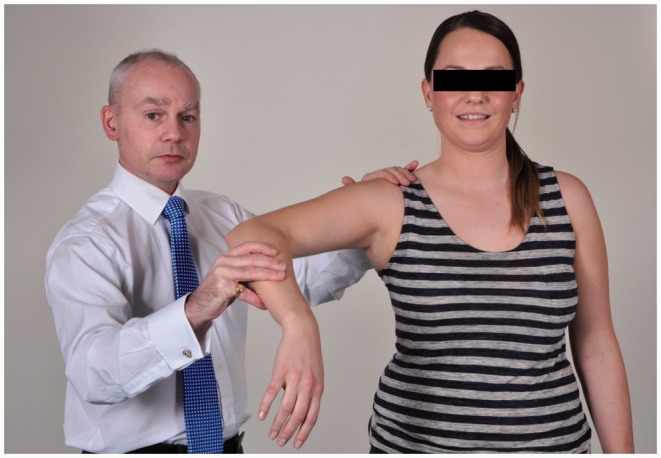
Bear-hug test
This test was described by Burkhart and De Beer, and involves the arm reaching across the body to hold the opposite latissimus dorsi and, with the elbow held forward of the body, the strength of the resistance to the hand being pulled away from the body is evaluated22. Some examiners modify this slightly, asking the patient to simply place the hand on the opposite chest wall, with the examiner’s hand between the patient’s and their chest wall, and ask them to resist a pull off (Figure 7).
Figure 7.

Bear hug.
Gerber’s lift-off test
The dorsum of the hand is placed on the sacrum and the patient is asked to take the hand off the back, when the examiner maintains a fixed angle of elbow flexion23. If the elbow is allowed to extend, the test is false because there is recruitment of triceps to the manoeuvre and so any determination of the strength of the lift off is inaccurate (Figure 8). In addition to this test, a lag sign may be looked for, with the arm held away from the sacrum by the examiner, so maximizing the internal rotation of the humerus, and the patient is then asked to maintain that position as the hand is released. If the hand falls back onto the sacrum, it indicates a weakness of subscapularis.
Figure 8.

Lift-off.
Electrophysiological validation of these tests has been performed, notably by separating the upper and lower parts of the subscapularis. The anterior tests are more sensitive in recording weakness in the upper fibres of the tendon, and a positive lift-off test indicates a weakness in the lower elements of the tendon24,25. Yoon et al. explored the different tests most commonly used for subscapularis pathology, and found the lift-off test to be the most specific at differentiating between an intact and torn tendon (100% of patients studied), whereas the belly-press test was the most sensitive, although only recording a value of 28%26. Similarly, to detect full-thickness from partial thickness tears, the lift-off test was 97% specific, with the belly-press test being the most sensitive at 57%.
One important difference between testing subscapularis anteriorly or posteriorly is the fundamental ability of the patient to position their hand in the correct place. Although this is rarely if ever a problem for the belly press or bear-hug positions, any significant degree of restriction of internal rotation of the shoulder, or a body shape with big hips and buttocks, may prevent the patient being able to reach sufficiently far around their back to allow comfortable positioning of the hand, meaning an accurate and consistent assessment may be impossible to achieve.
The above description of tests is far from exhaustive when aiming to examine the shoulder for any suspected rotator cuff pathology but, as with all musculoskeletal assessments, the findings are to be considered against the background of a full and detailed clinical history, especially noting the activity-related symptoms that a patient reports. This should ultimately allow the examiner to focus on the likely causes of the ongoing complaint with increased accuracy, allowing greater specificity in the use of diagnostics and a greater confidence in the prescription of appropriate forms of treatment for the patient and their condition.
Declaration of conflicting interests
None declared.
References
- 1.Nordt WE III, Garretson RB III, Plotkin E. The measurement of subacromial contact pressure in patients with impingement syndrome. Arthroscopy 1999; 15: 121–5. [DOI] [PubMed] [Google Scholar]
- 2.Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg 1996; 5: 1–11. [DOI] [PubMed] [Google Scholar]
- 3.Gagey N, Ravaud E, Lassau JP. Anatomy of the acromial arch: correlation of anatomy and magnetic resonance imaging. Surg Radiol Anat 1993; 15: 63–70. [DOI] [PubMed] [Google Scholar]
- 4.Funk L, Levy O, Even T, Copeland SA. Subacromial plica as a cause of impingement in the shoulder. J Shoulder Elbow Surg 2006; 15: 697–700. [DOI] [PubMed] [Google Scholar]
- 5.Hurt G, Baker CL., Jr Calcific tendinitis of the shoulder. Orthop Clin North Am 2003; 34: 567–75. [DOI] [PubMed] [Google Scholar]
- 6.Tsai YH, Huang TJ, Hsu WH, Huang KC, Li YY, Peng KT, Hsu RW. Detection of subacromial bursa thickening by sonography in shoulder impingement syndrome. Chang Gung Med J 2007; 30: 135–41. [PubMed] [Google Scholar]
- 7.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon) 2003; 18: 369–79. [DOI] [PubMed] [Google Scholar]
- 8.Neer CS, Welsh RP. The shoulder in sports. Orthop Clin North Am 1977; 8: 583–591. [PubMed] [Google Scholar]
- 9.Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med 1980; 8: 151–8. [DOI] [PubMed] [Google Scholar]
- 10.Pappas GP, Blemker SS, Beaulieu CF, McAdams TR, Whalen ST, Gold GE. In vivo anatomy of the Neer and Hawkins sign positions for shoulder impingement. J Shoulder Elbow Surg 2006; 15: 40–9. [DOI] [PubMed] [Google Scholar]
- 11.Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med 2012; 46: 964–78. [DOI] [PubMed] [Google Scholar]
- 12.Hegedus EJ, Goode A, Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med 2008; 42: 80–92. [DOI] [PubMed] [Google Scholar]
- 13.Lim JT, Acornley A, Dodenhoff RM. Recovery after arthroscopic subacromial decompression: prognostic value of the subacromial injection test. Arthroscopy 2005; 21: 680–3. [DOI] [PubMed] [Google Scholar]
- 14.Brookham RL, McLean L, Dickerson CR. Construct validity of muscle force tests of the rotator cuff muscles: an electromyographic investigation. Phys Ther 2010; 90: 572–80. [DOI] [PubMed] [Google Scholar]
- 15.Kim HM, Teefey SA, Zelig A, Galatz LM, Keener JD, Yamaguchi K. Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am 2009; 91: 289–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am 2005; 87: 1446–55. [DOI] [PubMed] [Google Scholar]
- 17.Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res 1991; 267: 45–56. [PubMed] [Google Scholar]
- 18.Gillooly JJ, Chidambaram R, Mok D. The lateral Jobe test: A more reliable method of diagnosing rotator cuff tears. Int J Shoulder Surg 2010; 4: 41–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg 1996; 5: 307–13. [DOI] [PubMed] [Google Scholar]
- 20.Walsh G, Boulahia A, Calderone S, et al. The ‘Dropping’ and ‘Hornblower’s’ signs in evaluation of rotator cuff tears. J Bone Joint Surg Br 1998; 80: 624–628. [DOI] [PubMed] [Google Scholar]
- 21.Gerber C, Hersche O, Farron J. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am 1996; 78: 1015–1023. [DOI] [PubMed] [Google Scholar]
- 22.Barth JR, Burkhart SS, De Beer JF. The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy 2006; 22: 1076–84. [DOI] [PubMed] [Google Scholar]
- 23.Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br 1991; 73: 389–94. [DOI] [PubMed] [Google Scholar]
- 24.Chao S, Thomas S, Yucha D, Kelly JD IV, Driban J, Swanik K. An electromyographic assessment of the ‘bear hug’: an examination for the evaluation of the subscapularis muscle. Arthroscopy 2008; 24: 1265–70. [DOI] [PubMed] [Google Scholar]
- 25.Tokish JM, Decker MJ, Ellis HB, Torry MR, Hawkins RJ. The belly-press test for the physical examination of the subscapularis muscle: electromyographic validation and comparison to the lift-off test. J Shoulder Elbow Surg 2003; 12: 427–30. [DOI] [PubMed] [Google Scholar]
- 26.Yoon JP, Chung SW, Kim SH, Oh JH. Diagnostic value of four clinical tests for the evaluation of subscapularis integrity. J Shoulder Elbow Surg 2013; 22: 1186–92. [DOI] [PubMed] [Google Scholar]