Abstract
Background
The elbow is an important but complex structure, with movement in both the sagittal plane in flexion and extension, as well as the rotational plane in forearm supination and pronation. Trauma is a common cause of elbow stiffness, which significantly hampers daily function. There are currently no gold-standard management guidelines for post-traumatic elbow stiffness, and most of the published literature focuses solely on the sagittal plane of motion.
Methods
This is a retrospective case series reviewing all patients who underwent a surgical release for treatment of post-traumatic elbow stiffness during a 36-month period. Motion range and the shortened version of the Disabilities of the Arm, Shoulder and Hand scores were serially measured and analyzed.
Results
The results obtained showed that both the sagittal and rotational range of motion directly influenced upper limb function; however, the relationship between these two motion planes was weak, meaning that both sagittal and rotational motion in the elbow need be addressed individually. Post-traumatic elbow stiffness could be aptly managed by various surgical approaches, including arthroscopic-assisted procedures; these were all effective in increasing both the sagittal and rotational range of motion. More importantly, this gain in range translated to a statistically significant improvement in upper limb function.
Conclusions
Management of elbow stiffness needs to be tackled in both the sagittal and rotational motion planes.
Keywords: Elbow joint, elbow rotational motion, elbow sagittal motion, post-traumatic elbow stiffness, pronation, supination
Introduction
The elbow joint is formed by the bony radiocapitellum and ulnatrochlear articulations, which are bounded by strong lateral ligamentous complexes and by a weaker joint capsule anterior–posteriorly [1]. The radiocapitellar joint, along with the interosseous membrane and proximal and distal radio-ulnar joints, contributes to forearm rotation [2]. Motion in the elbow joint is essential for positioning of the upper limb in space; an arc of 100° in both the sagittal and rotational range was described as a requirement for normal daily functions [3].
Trauma is a common cause of elbow stiffness, especially in the younger demographic. An exact pathogenesis is unclear, although cases can be broadly categorized into bone or soft tissue problems. Bony causes such as fracture malunions and interposed fragments can impair movement range. Heterotrophic ossification is another bony cause of stiffness that occurs in osteoinductive environments such as postfractures. Soft tissues such as capsules, ligaments and muscles can also cause elbow stiffness; myofibroblasts, which are influenced by hormonal and mechanical factors, play a key role in the development of soft tissue contractures and subsequent joint stiffness [4].
Although no gold-standard protocol for the management of post-traumatic elbow stiffness is available, most advocate a 6-month trial of conservative measures, such as physiotherapy, static/dynamic bracing or serial casting, before attempting operative procedures. Operative options are abundant and can be divided into surgical release or arthroplasty. Arthroplasty is seldom used as a first-line management in this young demographic, although available options include interposition, distraction, partial and total elbow arthroplasty [6]. Multiple open release techniques have been described, including the lateral column procedure [7], as well as medial over the top [8] and anterior approaches [9]. In recent decades, arthroscopic procedures have become more common, although the learning curve is steep and they carry a relatively higher risk of neurovascular complications compared to open approaches [10]. Much of the literature reports good outcomes, with a sustained gain of flexion and extension motion regardless of the management protocol followed. However, most only place emphasis on the sagittal flexion and extension range, with little elaboration on the rotational range [4]. Because the radiocapitellum joint is involved in forearm rotation, the main objective of the present study was to investigate the significance of restoring the often neglected rotational range in the elbow and forearm; in conjunction with the sagittal range.
Materials and Methods
This was a retrospective level IV case series of all patients who underwent surgical release for post-traumatic elbow stiffness between January 2009 and December 2012. The release surgery was performed by a single surgeon, although the exact procedure was tailored to each case according to the initial trauma. Most underwent an arthroscopic soft tissue release, which was often performed in conjunction with surgery for implant removal. All cases underwent a standardized physiotherapy regime; with continuous passive mobilization starting from day 1, followed by an aggressive rehabilitation protocol including both passive and active mobilization at our physiotherapy department, three times a week. Outcome measures were documented on three occasions (pre-operative, immediate postoperative and long-term follow-up) by measuring the active range of motion and calculating the upper limb functions scores. Range measurements were obtained with the limb in standardized positions using a handheld goniometer by a single assessor; sagittal motion was measured with the forearm at full supination whenever possible. Measurement of forearm rotation was with the elbow at 70° flexion, which is when the radial-capitulum joint is most congruent; the arm was held against the trunk to eliminate shoulder rotation and the wrist was locked in a neutral position (Fig. 1) and a chopstick was held in each hand to aid visualization. Functional scores were calculated using the Chinese translation of the shortened version of the Disabilities of the Arm, Shoulder and Hand (QuickDASH) upper limb assessment score [11] because it has been shown to be reproducible and effective [12].
Fig. 1.
Clinical photograph of limited range in the left elbow.
Software used for data analysis comprised Numbers 09 (Apple Inc., Cupertino, CA, USA) and SPSS, version 19 (IBM Corp., Armonk, NY, USA).
Results
There were 14 cases (eight males and six females) in total, with a mean age of 48.5 years (range 19 years to 66 years, with a median of 50 years). All subjects were right-hand dominant; seven had injury to the dominant right upper limb, whereas the remaining seven had involvement of the left side.
Regarding the initial injury, the most common mechanisms were cycling accidents, followed by falls. Most subjects sustained a combination of radius, ulna and humeral fractures. Four cases had associated radial head dislocations and three cases had an open fracture. The initial management depended on the injury pattern; the majority underwent internal fixation and two cases with open wounds were managed with a dynamic joint distractor. The duration from the initial injury to the release surgery ranged from 5 months to 30 months with an average of 11 months. During this period, all patients underwent a period of physiotherapy and rehabilitation until their condition plateaued. Patients who developed post-traumatic elbow stiffness show significant difficulties in performing daily activities with an average pre-operative QuickDASH score of 70.1 (range 47.7 to 84.1).
Of the 14 cases, two cases had significant complications. One of the cases underwent arthroscopic release in conjunction with percutaneous removal of an olecranon plate; however, an undisplaced crack over the proximal ulna was noticed during intra-operative fluoroscopy screening, probably at a weak point in the bone after implant removal. This undisplaced fracture was fixed internally, allowing the patient to proceed uneventfully with the standard post-release mobilization regime. The other case underwent an arthroscopic release with percutaneous removal of radial head screws; he complained of persistent postoperative numbness over the ulna nerve distribution without significant weakness. Subsequent nerve conduction studies performed at 18 months after the symptom onset showed ulnar sensory and motor demyelination and mild sensory axonal degeneration; because the symptoms were tolerable, the patient opted for observation only.
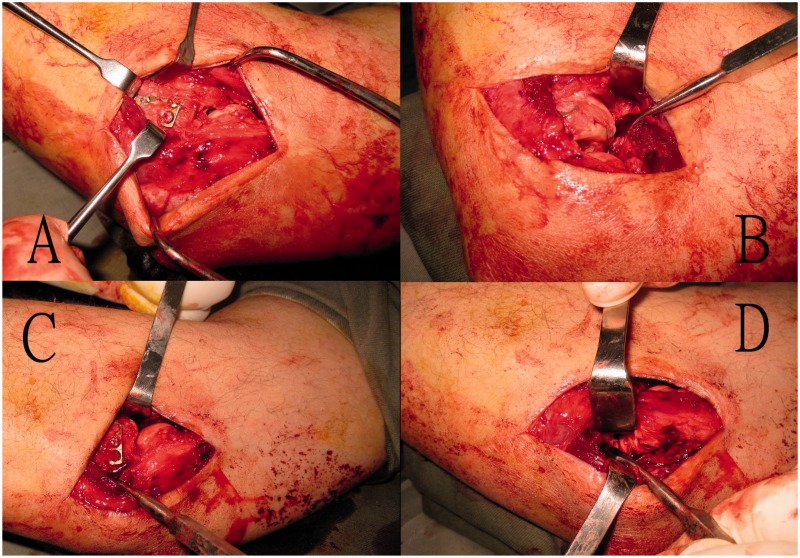
Regarding the release procedures, 10 patients underwent arthroscopic release together with a percutaneous incision for implant removal. Three cases underwent arthroscopy first with subsequent open release, whereas one case proceed straight to open release (Fig. 2). That same case proceeded directly to open release using the lateral approach because the patient required excision of heterotrophic bone over the radial neck in addition to removal of the radial head T-plate and screws. This procedure was considered more straightforward with an open approach, rather than attempting arthroscopy first. Regarding the three cases who underwent both arthroscopy and open release, one case was complicated by an iatrogenic undisplaced olecranon crack during implant removal, which required revision fixation. The second case involved an unsuccessful attempt to percutaneously remove an olecranon plate, and re-exposure of the entire wound was required before the implant was successfully removed. The remaining case failed to achieve a satisfactory range of motion after arthroscopic release; therefore, a formal open release was performed, which succeeded in gaining an acceptable range of option. All cases were found to have marked capsular fibrosis; six cases had mild to moderate synovitis, whereas only one case had significant heterotrophic ossification that required excision. Six cases underwent implant removal; four of these implants were removed via a percutaneous incision.
Fig. 2.
Open heterotropic ossification excision and lateral release.
Motion range of the sagittal and rotational planes was measured at the pre-release, post-release and follow-up consultations. Regression analysis showed that the sagittal range only had a weak relationship with the rotational range with a correlation coefficient r = 0.566 (Fig. 3).
Fig. 3.
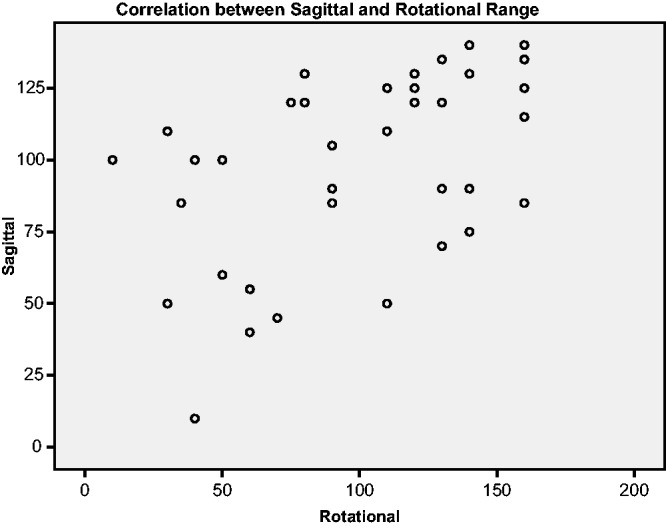
Correlation between sagittal and rotational range was weak.
The sagittal range and rotational range were separately paired with their respective QuickDASH scores during the pre-release and follow-up consultations. Correlation between the sagittal range and the QuickDASH score was strong, with a correlation coefficient of r = 0.716 (Fig. 4). Regression analysis using data from elbow rotation also showed a linear relationship between the rotational range and the QuickDASH function score, with a correlation coefficient of r = 0.871 (Fig. 5).
Fig. 4.
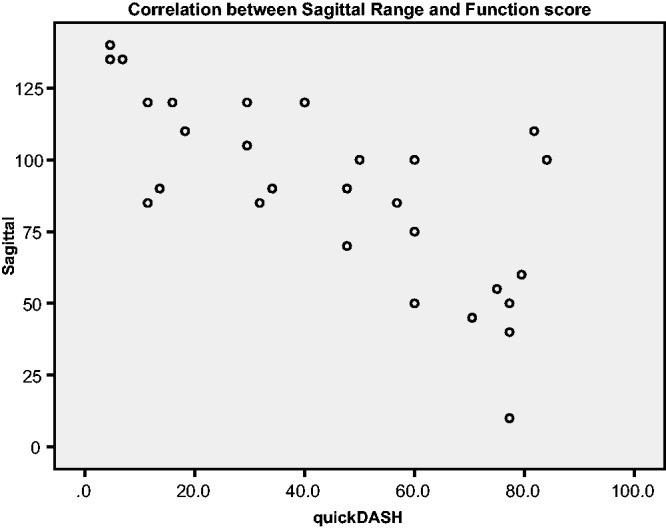
Correlation between sagittal range and function was strong.
Fig. 5.
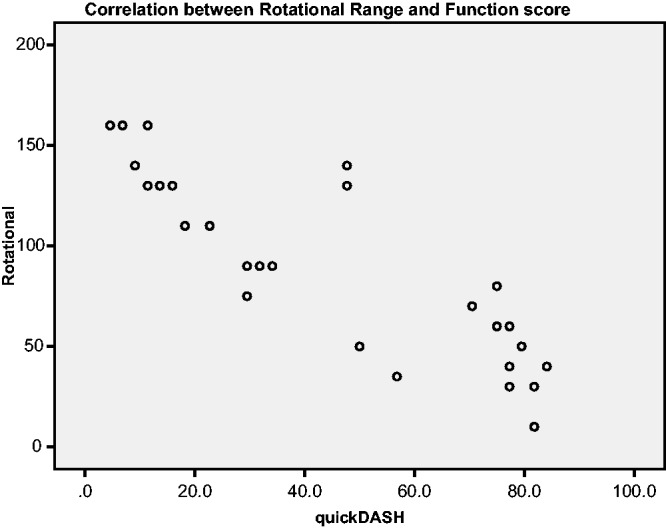
Correlation between rotational range and function was strong.
Surgical release provided good results with significant improvements in both the sagittal and rotational ranges after the procedures (Table 1). Although there was a significant recurrence of stiffness from the immediate post-release measurements to the measurement during the long-term follow-up (Table 2), there was still a significant overall improvement from the pre-release baseline.
Table 1.
Range of movement (ROM) during pre-release, immediate postoperative and long-term assessments.
| Pre-release | Immediate postoperative | Long-term follow-up | |
|---|---|---|---|
| Mean sagittal ROM | 74° (10° to 120°) | 130° (110° to 140°) | 104° (50° to 140°) |
| Difference and Wilcoxon signed rank test | +56° Z = −3.181 P = 0.001 | +30° Z = −2.764 P = 0.006 | |
| Mean rotational ROM | 59° (10° to 140°) | 135° (80° to 160°) | 124° (75° to 160°) |
| Difference and Wilcoxon signed rank test | +76° Z = −3.300 P = 0.001 | +65° Z = −3.302 P = 0.001 |
Table 2.
Recurrence of stiffness despite aggressive rehabilitation.
| Immediate postrelease | Long-term follow-up | Difference | Wilcoxon signed rank test | |
|---|---|---|---|---|
| Mean sagittal ROM | 130° (110° to 140°) | 104° (50° to 140°) | −26° | Z = −2.943 P = 0.003 |
| Mean rotational ROM | 135° (80° to 160°) | 124° (75° to 160°) | −11° | Z = −2.352 P = 0.019 |
R, range of movement.
More importantly, this improvement in motion range translated to a significant functional gain (z = −3.296, p = 0.001), with the QuickDASH improving by an average of 52.7 points from the pre-release range of 47.7 to 84.1 to the follow-up of 4.5 to 34.1 (Fig. 6)
Fig. 6.
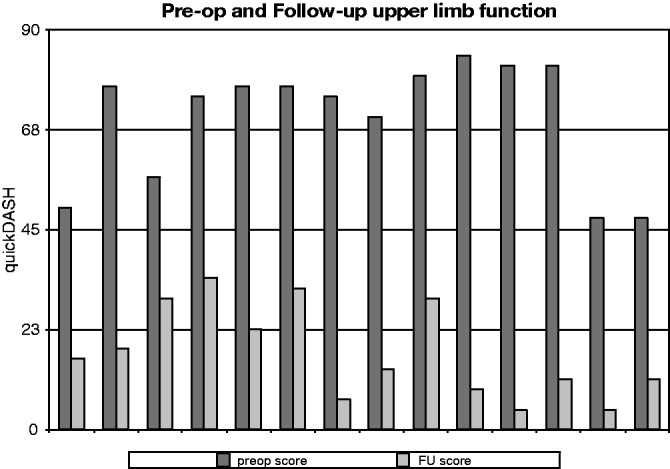
Significant improvements in the shortened version of the Disabilities of the Arm, Shoulder and Hand (QuickDASH) score during follow-up (FU) assessment.
Discussion
The present study showed that post-traumatic elbow stiffness significantly affects both the sagittal plane of motion in flexion and extension, as well as the rotational plane of motion in forearm pronation and supination. Motion in both these planes is integral for positioning the arm in space. Restriction as seen in post-trauma patients of either plane significantly impairs daily functions. Our patients with post-traumatic elbow stiffness were initially moderate–severely disabled, with a mean pre-operative QuickDASH score of 70.1 (range 47.7 to 84.1), where a DASH score of approximately 10.1 is considered as normal [13].
The data show that sagittal range and rotational range are independent of each other and we consider that they should be managed as two separate entities. However, the majority of the available literature often neglects the importance of rotational motion in the elbow, with many studies solely focusing on the sagittal motion. From our experience, it was observed that patients frequently have a severely limited sagittal range but a relatively preserved rotational range, or vice versa. Regression analysis of our data supported that observation by showing that the correlation between the elbow sagittal and rotation ranges was weak. This leads us to conclude that, although the habit of solely measuring sagittal range is a common phenomena [4], it is not representative of the overall motion in the elbow. Furthermore, our results also show that both variables, the sagittal and rotational motion plane ranges, significantly influence upper limb function (Figs 4 and 5). Because the sagittal and rotational range show only a weak inter-correlation (Fig. 3), we suggest that rotational stiffness affects upper limb function regardless of the sagittal range (and the reverse is also true). Thus, we consider that, if a satisfactory regain of function is desired, a thorough surgical release of elbow stiffness must correct the motion in both the sagittal and rotational planes.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of interest
None declared
References
- 1.Nandi S, Maschke S, Evans PJ, Lawton JN. The stiff elbow. Hand (NY) 2009; 4: 368–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gray H. Anatomy of the human body, Philadelphia, PA: Lea & Febiger, 1918. [Google Scholar]
- 3.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 1981; 63: 872–7. [PubMed] [Google Scholar]
- 4.Charalambous CP, Morrey BF. Posttraumatic elbow stiffness. J Bone Joint Surg Am 2012; 94: 1428–37. [DOI] [PubMed] [Google Scholar]
- 5.Morey BF, Sanchez-Sotelo J. The elbow and its disorders, Fourth edn Philadelphia, PA: Elsevier Health Sciences, 2009. [Google Scholar]
- 6.Liu S, Liu J, Li X, Ruan H, Fan C. Open arthrolysis and prosthetic replacement of the radial head for elbow stiffness associated with rotation limitation. J Shoulder 2013; 22: 275–9. [DOI] [PubMed] [Google Scholar]
- 7.Mansat P, Morrey BF. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am 1998; 80: 1603–15. [PubMed] [Google Scholar]
- 8.Kasparyan NG, Hotchkiss RN. Dynamic skeletal fixation in the upper extremity. Hand Clin 1997; 13: 643–63. [PubMed] [Google Scholar]
- 9.Urbaniak JR, Hansen PE, Beissinger SF, Aitken MS. Correction of post-traumatic flexion contracture of the elbow by anterior capsulotomy. J Bone Joint Surg Am 1985; 67: 1160–4. [PubMed] [Google Scholar]
- 10.Keener JD, Galatz LM. Arthroscopic management of the stiff elbow. J Am Acad Orthop Surg 2011; 19: 265–74. [DOI] [PubMed] [Google Scholar]
- 11.Lee EWC, Lau JSY, Chung MMH, Li APS, Lo SK. Evaluation of the Chinese version of the Disability of the Arm, Shoulder and Hand (DASH-HKPWH): cross-cultural adaptation process, internal consistency and reliability study. J Hand Ther 2004; 17: 417–23. [PubMed] [Google Scholar]
- 12.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 2006; 7: 44–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am 2002; 84A: 208–15. [DOI] [PubMed] [Google Scholar]
- 14.Transport Department Hong Kong SAR.Cycling study. http://www.td.gov.hk/filemanager/en/publication/cyclingstudy.pdf.
- 15.Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg 2006; 14: 113–20. [DOI] [PubMed] [Google Scholar]
- 16.Dumonski ML, Arciero RA, Mazzocca AD. Ulnar nerve palsy after elbow arthroscopy. Arthroscopy 2006; 22: 577e1–3. [DOI] [PubMed] [Google Scholar]
- 17.Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg 2009; 18: 920–6. [DOI] [PubMed] [Google Scholar]