Abstract
Background:
The present study aimed to compare medium-term clinical outcomes of patients following arthroscopic subacromial decompression (ASAD): those with intact rotator cuff with two groups of increasing size of partial thickness bursal-side tears.
Methods:
Patients undergoing shoulder arthroscopy by a single surgeon had pre- and postoperative Constant scores prospectively recorded. Arthroscopic surgery included the assessment of any supraspinatus tears using the Ellman criteria, as well as ASAD and cuff debridement. Groups were created based on the status of rotator cuff and size of bursal tear. Outcome in these patient groups was then compared and analyzed
Results:
Seventy-four patients were suitable for inclusion in the study: 32 patients without a cuff tear; 21 patients with a cuff tear of 9 mm or less in length; and 21 patients with a cuff tear of 10 mm or more in length. Baseline characteristics of the three groups were similar. All three groups showed a significant improvement in their Constant scores following surgery. There was, however, no significant difference in Constant scores between the three groups.
Conclusions:
The results of the present study show that patients with varying sizes of bursal-side tears respond to ASAD as well as those with no rotator cuff tear.
Keywords: Arthroscopic subacromial decompression, ASAD, partial thickness rotator cuff tears
Introduction
The rotator cuff is a musculotendinuous unit essential for normal shoulder biomechanics with a mean tendon thickness of 10 mm to 12 mm.1 It plays a major role in shoulder pathology2 with impingement pain and or rotator cuff tendon tears (RCT) being some of the most common causes of pain and disability in the upper extremity.3 Partial thickness tears of the rotator cuff are common amongst patients with impingement and can be a cause of unexplained pain in the shoulder.4 Ellman classified these based on depth and location within the tendon.1 The depth he graded with a 3-mm probe as: grade, 1 < 3 mm; grade 2, 3 mm to 6 mm; grade 3, > 6 mm (involving half the tendon). The location is classified as: bursal-side tear (BT), intratendinous tear and joint-side tear (JT). The natural history for partial thickness tears and the best treatment for symptomatic partial thickness tears (which have failed conservative management) is not clear. Increasingly, partial thickness tears are treated aggressively as a result of their poor healing and propensity to propagate to full thickness tears. Subacromial decompression has been historically the treatment of choice, although, increasingly, surgeons tend to repair associated partial thickness tears involving greater than 50% tendon thickness.5 The present study aimed to compare the results of ASAD in different groups: those with no cuff tear and partial cuff tears of different lengths.
Materials and methods
Patient selection
Patients undergoing arthroscopic surgery for rotator cuff disease of the shoulder at a single shoulder unit over a 4-year period were included in the present study. All patients had failed a 6-month trial of conservative treatment, including physiotherapy, and, in most cases, a steroid injection prior to being listed for surgery. Pre-operative exclusion criteria included: full thickness tears of the rotator cuff; acromioclavicular joint pain; and suspected instability or internal impingement. Patients found to have: glenohumeral arthritis, labral lesions, full thickness rotator cuff tears, articular-sided partial thickness tears, and tears to other rotator cuff muscles at the time of arthroscopy were also excluded.
Surgical technique
All operations were performed by the senior author under general anaesthesia in an upright beach chair position. Arthroscopy included diagnostic evaluation of the glenohumeral joint and subacromial space for rotator cuff tears and other pathology
Careful bursal resection and clearance allowed evaluation of the bursal surface of the cuff. Only patients who had a totally intact cuff, as seen from the bursal and joint sides, and patients who had BT involving <50% thickness of the tendon were included. Patients who were considered to have >50% thickness partial tears underwent tendon repair and were excluded from the analysis.
An arthroscopic probe with a 3-mm right-angled tip and 5-mm markings on the stem was used to measure the depth of the tear and tear dimensions. The depth of the tear was graded as described by Ellman.1 Patients with grade 3 involving more than 50% of the tendon, were excluded from the present study. The arthroscopic probe was also used to measure the length of bursal side tear in its longest dimension. This measurement was used as an indicator of size of the tear.
Following rotator cuff assessment, all patients underwent release of the coracoacromial ligament, subacromial bursectomy, and anterior acromioplasty. In addition, debridement of the edges of partial thickness bursal tears, if present, was performed.
Patient assessment and postoperative management
All patients followed the same pre- and postoperative standardized regime. Patients were analyzed pre- and postoperatively by a senior physiotherapist with a specialist interest in shoulders who was blinded to the imaging and operative findings. Postoperatively, patients were discharged on the day of surgery without a sling or immobilization. They commenced active motion exercises with a physiotherapist on the day of surgery, progressing to strengthening exercises at 4 weeks. Patients were followed up at 8 weeks, 12 months and at a further review to obtain data for the present study. Evaluation at 12 months included the recording of Constant scores using standardized strength testing with the Nottingham McMesin myometer (Mecmesin Co., Nottingham, UK).
Statistical analysis
To determine the influence of the presence of a BT and the length of the tear on outcome, three groups were created (based on the arthroscopic findings) for analysis: group 1 included patients with no cuff tear; group 2 included patients with a cuff tear of less than 9 mm in length; and group 3 was made up of patients with a cuff tear of 10 mm in length or greater.
Paired t-tests were performed for pre- and postoperative Constant scores for each group (no cuff tear; ≤ 9 mm; ≥ 10 mm) to demonstrate the change in means of Constant score from pre-operative to postoperative evaluation.
A one-way analysis of variance (ANOVA) was used to compare the levels of absolute change (pre-operative scores to postoperative scores) in Constant scores between the three groups. Data processing and statistical tests were performed using SPSS, version 10 (SPSS Inc., Chicago, IL, USA). p < 0.05 was considered statistically significant.
Results
Four hundred and thirty-five patients underwent ASAD over a 4-year period for primary impingement and rotator cuff disease; of these, 74 were suitable for inclusion in the present study. These patients were classified into three groups based on the cuff appearance at surgery: 32 patients had no cuff tear; 21 patients had a cuff tear less than or equal to 9 mm in length (mean 7 mm), out of which nine were Ellman grade 1; and 21 patients had a cuff tear 10 mm or greater in length (mean 13 mm), out of which 12 were Ellman grade 1. Overall, the mean (SD) patient age was 52 years (13.9 years); the male to female ratio was 2:1. The age and sex distribution of all three groups are summarized in Table 1. The mean follow-up was 20 months (mean 12 months to 36 months) with no difference between groups. There were no intra-operative or postoperative complications. At the time of discharge from outpatients, no patients had required further surgery.
Table 1.
Age and sex distribution in the three groups.
| Demographics | No tear | Tear size ≤9 mm | Tear size ≥10 mm |
|---|---|---|---|
| Age: mean (range) | 51.28 (36 to 66) | 49.70 (32 to 74) | 51.33 (30 to 67) |
| Sex (male:female) | 23:9 | 16:5 | 12:9 |
| Previous shoulder Surgery | Nil | Nil | Nil |
The pre- and postoperative Constant scores of the three groups are shown in Table 2.
Table 2.
Constant scores (pre- and postoperatively) for each group.
| Size of tear | No tear (n = 32) | ≤9 mm (n = 21) | ≥10 mm (n = 21) | Total (n = 74) |
|---|---|---|---|---|
| Pre-operative | ||||
| Mean (SD) | 44.5 (18.9) | 44.4 (15.9) | 39.3 (16.2) | 43.0 (17.3) |
| Range (minimum–maximum) | 12 to 86 | 17 to 71 | 12 to 82 | 12 to 86 |
| Postoperative (12 months) | ||||
| Mean (SD) | 61.9 (21.9) | 65.8 (18.7) | 63.6 (22.7) | 63.5 (21.1) |
| Range (minimum–maximum) | 18 to 100 | 31 to 100 | 17 to 91 | 17 to 100 |
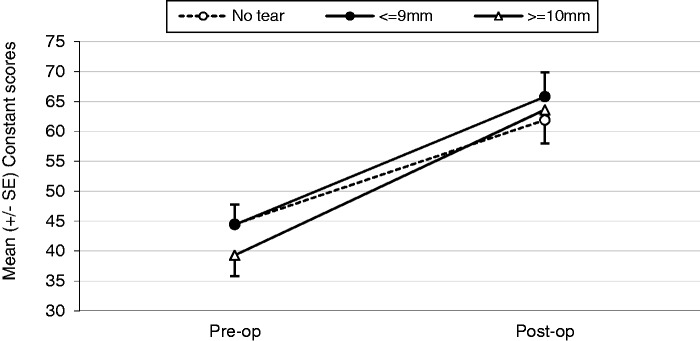
When analyzed, the overall improvement in Constant score was statistically significant (p < 0.01). Statistical significance (paired t-test, p < 0.01) was also maintained when examining each group individually. Figure 1 demonstrates graphically the improvement in Constant score for each group. Comparing the levels of absolute change in Constant scores (from pre- to postoperative) between the three groups, there was no significant difference (one-way ANOVA, F2,71 = 0.72, p = 0.49) between the groups.
Figure 1.
Graph showing improvement in mean Constant score following surgery. Between group differences: one-way ANOVA, F2,71 = 0.72, p = 0.49.
Discussion
Partial thickness tears may be at least twice as common as a complete rotator cuff tear.6 Extrinsic subacromial impingement4,7,8 and internal factors such as tendinopathy9 or enthesopathy10 have all been proposed to contribute to the development of these tears. The natural history of partial thickness rotator cuff tears including the behaviour differences of JT versus BT and their potential to heal is poorly understood.4
Histological studies show limited potential for spontaneous healing of partial thickness tears, whereas biomechanical studies suggest that the partial thickness tears may be prone to propagate.11 Moreover Yamanaka and Matsumoto showed that JT may increase in size over time with conservative management. Hence, increasingly, surgeons are treating partial thickness tears more aggressively.12
In partial thickness tears greater than 50%, surgical treatment is becoming more uniform. Weber showed that, following acromioplasty and arthroscopic debridement, tears greater than 50% tended to fail.13 Subsequently, study surgeons have tended to repair higher-grade partial thickness tears greater than 50%.5 This has involved techniques such as transtendon repair, tear completion and repair, and transosseous repair, with no techniques being superior to the others.12
It is not clear whether BT and JT behave differently or should be treated as aggressively as type 3 tears. Comparisons of low-grade (Ellman grade 1 to 2) BT and JT treated with SAD and debridement have produced mixed results. Following SAD and debridement, Park et al.14 showed BT performed better than JT, whereas Kartus et al.15 found the Constant score for BT (61.5) to be lower than that for JT (72) but not significantly. Cordasco et al.16 showed that BT were far more likely to fail than JT and, consequently, they are more likely to repair BT. Kamath et al. showed that, in high-grade partial thickness tears, bursal tears had a higher failure rate (22%) than articular sided tears (9%) following repair, although this was not statistically significant and it is not clear whether this failure rate is applicable to low-grade BT.17
The natural history of partial thickness tears is still unknown. In the present study, the size of the low-grade tear did not affect outcome. Tears >10 mm showed similar improvements in Constant score to smaller tears and indeed cuffs with no tears. The relative numbers of Ellman grades 1 and 2 were too small in the two groups with low-grade BT to allow subgroup analyses. We are unaware of previous studies investigating the influence of the length of low-grade partial thickness bursal tears on outcome from ASAD. However studies have shown partial thickness tears (JT and BT) may propagate despite ASAD and debridement.13,15 Given that partial thickness tears have a poor ability to heal and treatment is not protective, partial thickness tears might be expected to enlarge causing patients to re-present with pain and weakness, particularly tears of greater size. This was not reflected in the present study. Thus, until the natural history of partial thickness RCT is better understood, it appears simplistic to repair larger low-grade tears simply on the premise that bigger tears are more likely to progress than small ones. Rotator cuff tears are considered to be more common in older patients. Thus, the groups with partial thickness tears would be expected to have a higher median age than a group without RCT. This was not reflected in the present study at a mean follow-up of 20 months.
In the present study, ASAD and debridement proved a successful treatment for low-grade BT, leading to significant improvements in Constant scores. Because the patients were not re-imaged, we cannot be certain whether tears healed or even progressed; however, the treatment failures in the study by Cordasco et al.16 presented very early on, whereas our patients were symptom free at discharge. Thus, our results suggest that the partial thickness tears were unlikely to have progressed to full thickness tears and support SAD and tear debridement as treatment for low-grade BT. In their systematic review, Strauss et al. support debridement with ASAD as the best treatment for low-grade partial thickness tears, although they admitting that a proportion of patients may progress to full thickness tears.11
The present study has several strengths. One surgeon performed all of the operations, removing variability in technique and arthroscopic assessment including tear assessment. One examiner performed all pre- and postoperative measurements when blinded to surgical findings, thus removing examiner bias and variability in measurements. By excluding other pathology, such as glenohumeral arthritis, acromioclavicular arthropathy and adhesive capsulitis, to create a homogenous group, the benefit of a single treatment such as ASAD and debridement is easier to determine and our results become more meaningful.
The present study has some limitations. First, the study compared partial thickness BT with intact rotator cuff without including JT. This provided a homogenous group for comparison; however, the inclusion of JT in future studies might help further our understanding of the natural history of low-grade JT and BT. Second, although our 20-month follow-up is not short, the cuff tears in the present study may still go on to fail at a later date. Two years is a more commonly accepted follow-up period and, ideally, this study would have been longer. A longer follow-up with repeat imaging might help reveal whether patients with partial thickness tears are more likely to have symptom recurrence or tear progression, as suggested in other studies. A more robust study would have comprised a prospectively designed randomized controlled trial including power analysis. We do, however, consider that our data and findings have merit. Our medium-term outcomes not only further our knowledge of a poorly understood topic, but also our data will help other researchers with power/sample size calculations for future randomized studies in the area. Clearly, although our results support ASAD and debridement as a treatment for low-grade BT, our understanding of the natural history of these tears remains poor.
Conclusions
We conclude from our study that ASAD alone, without tendon repair, yields satisfactory results at a medium-term mean follow-up of 20 months in patients with BTs involving <50% thickness, irrespective of the length of the tear.
Declaration of conflicting interests
None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1.Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop 1990; 254: 64–74. [PubMed] [Google Scholar]
- 2.Neer CS. Impingement lesions. Clin Orthop 1983; 173: 70–7. [PubMed] [Google Scholar]
- 3.Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med 1980; l: 151–8. [DOI] [PubMed] [Google Scholar]
- 4.Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg 2003; 85B: 3–11. [DOI] [PubMed] [Google Scholar]
- 5.Kim CK, Shin HD, Cha MS, Park JY. Repair integrity and functional outcome after arthroscopic conversion to a full-thickness rotator cuff tear. Am J Sports Med 2014; 42: 451–6. [DOI] [PubMed] [Google Scholar]
- 6.Yamanaka K, Fukuda H. Pathological studies of the supraspinatus tendon with reference to incomplete thickness tear. In: Takagishi N. (eds). The shoulder, Tokyo: Professional Postgraduate Services, 1987, pp. 220–4. [Google Scholar]
- 7.Neer CS. Anterior acromioplasty for chronic impingement syndrome in the shoulder. A preliminary report. J Bone Joint Surg 1972; 54A: 41–50. [PubMed] [Google Scholar]
- 8.Fukuda K. Partial thickness rotator cuff tears: a modern view on codman’s classic. J Shoulder Elbow Surg 2000; 9: 163–8. [PubMed] [Google Scholar]
- 9.Ozaki, Fujimoto S, Nakagawa Y, Mashuhara K, Tamai S. Tears of the rotator cuff of the shoulder associated with pathological changes in the acromion. A study in cadavera. J Bone Joint Surg 1988; 70A: 1224–30. [PubMed] [Google Scholar]
- 10.Sano H, Ishii H, Yeadon A, Backman DS, Brunet JA, Uhthoff HK. Degeneration at the insertion weakens the tensile strength of the supraspinatus tendon: a comparative mechanical and histological study of the bone-tendon complex. J Orthop Research 1997; 15: 19–26. [DOI] [PubMed] [Google Scholar]
- 11.Strauss EJ, Salata MJ, Kecher J, et al. The arthroscopic management of partial thickness rotator cuff tears: a systematic review of the literature. Arthroscopy 2011; 27: 568–80. [DOI] [PubMed] [Google Scholar]
- 12.Yamanaka K, Matsumoto T. The joint side of the rotator cuff: a follow up study by arthrography. Clin Orthop 1994; 304: 68–73. [PubMed] [Google Scholar]
- 13.Weber SC. Arthroscopic debridement and acromioplasty versus mini-open repair in the treatment of significant partial-thickness rotator cuff tears. Arthroscopy 1999; 15: 126–31. [DOI] [PubMed] [Google Scholar]
- 14.Park JY, Yoo MJ, Kim MH. Comparison of surgical outcomes between bursal and articular partial thickness rotator cuff tears. Orthopaedics 2003; 26: 387–90. [DOI] [PubMed] [Google Scholar]
- 15.Kartus J, Kartus C, Rostgard-Christiansesn L, Sernert N, Read J, Perko M. Long term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Arthroscopy 2006; 22: 44–9. [DOI] [PubMed] [Google Scholar]
- 16.Cordasco FA, Backer M, Craig EV, Klein D, Warren RF. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med 2002; 30: 257–60. [DOI] [PubMed] [Google Scholar]
- 17.Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J Bone Joint Surg 2009; 91A: 1055–62. [DOI] [PubMed] [Google Scholar]