Abstract
Background
The aim of this retrospective case series study was to assess the outcomes of patients with recurrent anterior shoulder instability with antero-inferior glenoid bone loss treated with a specific open stabilization technique using intra-substance coracoid bone-grafting and Bankart repair.
Methods
Over a 4-year period, 34 shoulders in all male patients of mean age 21 years were stabilized with this technique. Pre- and postoperative function, motion and stability were assessed as part of Rowe stability scoring, and American Shoulder and Elbow Surgeons (ASES) and Oxford Instability were recorded, with at least 2 years of follow-up in all patients. Union of the graft was determined by post-operative computed tomography (CT) of the affected shoulder.
Results
For all cases, two redislocations (5.9%) and two subluxations occurred when continuing high-risk sport after 2 years. Post-operative scores [median, mean (SD): Rowe 77.5, 77.2 (19.5); ASES 94.2, 92 (7.7); Oxford 43, 41.2 (6)]. CT scans on 28 shoulders at a mean of 4.5 months after surgery showed non-union in three cases (10%).
Conclusions
These results demonstrate a high rate of success in cases of glenoid bone loss in the young contact athlete with recurrent instability treated with open stabilization and bone grafting.
Keywords: bone graft, glenoid deficiency, glenoid reconstruction, shoulder instability
Introduction
Although both arthroscopic and open stabilization techniques without bony augmentation can be used to address recurrent cases of anterior instability, these are generally reserved for cases with less than 25% of glenoid bone loss.1,2 Larger bone defects of the antero-inferior glenoid can be commonly associated with recurrent anterior instability of the shoulder.1,2–9 Although no gold standard exists on how these lesions should be evaluated and quantified, there appears to be consensus that bony reconstruction of the antero-inferior glenoid should be performed in cases of ‘significant’ glenoid bone deficiency. Bigliani et al.3 and Itoi et al.10,11 advocate a bony reconstruction of the glenoid where 25% loss and 21% glenoid loss is evident, respectively. Otherwise, recurrent instability can be seen in up to 75% in cases of isolated Bankart repair without bony reconstruction.1,4
Glenoid reconstruction involving bony augmentation previously described in the literature includes coracoid process transfer with conjoint tendon (Bristow–Latarjet), autograft and allograft techniques.12–16 The Bristow–Latarjet procedure has been reported to have three stabilizing mechanisms: (i) buttress effect of the coracoid bone; (ii) sling effect of the conjoint tendon and subscabularis; and (iii) reinforcement through an anterior capsular duplication with the released coracoacromial ligament.17–19 However, there are several reported complications, such as bony non-union, progressive impingement and loosening or migration of hardware.8,9
We consider, particularly in young patients with anterior instability and glenoid bone loss, that the use of screws and permanent alteration of the anatomy should be avoided. We therefore proposed a study where a free coracoid graft was used followed by reconstruction of the coracoid. The graft was fixed with absorbable nails so that, over the long-term, there was no metal to damage the head should a further dislocation occur. The present study aimed to evaluate the outcomes of a procedure involving the reconstruction of anteroinferior glenoid defects in this population, employing the use of smart nails with a free autograft combined with open Bankart repair of the glenoid capsuloligamentous structures.
Materials and methods
Patient selection
The patients were part of a clinical trial registered in the Australian and New Zealand Clinical Trials Register and ethics approval was obtained. The present study comprises a retrospective case series evaluating the outcomes of these patients. Over a 4-year period, the senior author performed 416 arthroscopic assessment and stabilization procedures. This included a consecutive sample of 34 cases where bone grafting was carried out. Indication for surgery was an ongoing history of pain, including overhead pain and deadarm syndrome, apprehension or instability with recurrent subluxation or frank dislocation from a traumatic event supported by clinical findings. This included excess anterior glide on drawer testing and anterior apprehension with a postiive relocation test. Patients who had had previous stabilization surgery but without grafting and ongoing recurrent instability were included in the present study. All patients reported a traumatic event related to sport at a certain level.
Patients were assessed prospectively with questionnaires, clinical examination, and pre-operatively and postoperatively, sent at beyond 2 years since their surgery. All patients responded. Patient demographics are reported in Table 1. All data were analyzed using parametric data in Excel (Microsoft Corp., Redmond, WA, USA). The entire sample was male, with 47% operated on the right shoulder and the same number on the dominant side. Half the cases had prior stabilization surgery without grafting, three cases of which each had two failed stabilizations. Specific details, other than no use of graft, were not available for those prior procedures.
Table 1.
Demographic information on patients undergoing this technique.
| Characteristic | n (%) |
|---|---|
| Men | 34 (100%) |
| Right shoulder | 16 (47%) |
| Left shoulder | 18 (53%) |
| Dominant | 16 (47%) |
| Average age at surgery (years) | 21 (range 15 to 29) |
| Previous surgeries | 17 shoulders (50%) |
Traumatic dislocation and subluxations attributed to a sporting event occurred in all cases. Seven cases suffered a single dislocation and two an apparent subluxation, with ongoing apprehension. Twelve suffered between two and five dislocations and a further thirteen had more than five dislocations.
Any previous surgery for the same condition was recorded. Pre-operative assessment of the level and type of sport was also obtained, including patients’ intentions in terms of continuing or returning to high- or low-risk sport in the long term and their ability to do so. Pre- and postoperative Rowe scoring for stability, function and motion were also recorded accordingly. American Shoulder and Elbow Surgeons (ASES) and Oxford Instability scoring was also recorded at beyond 2 years.
Surgical technique
The surgical technique involved an initial arthroscopic assessment in the lateral decubitus position to establish the degree of capsular injury, bony glenoid loss, and evidence of any associated Hill–Sachs lesion.20 All other pathology was assessed and recorded, looking particularly at articular cartilage damage, as well as associated superior labrum anterior to posterior (SLAP), anterior labral periosteal sleeve avulsion and humeral avulsion glenhumeral ligament lesions.
A deltopectoral approach was used with the patient repositioned supine. Splitting of subcapularis in line with its fibres was performed and elevated off the capsule. Rotator interval was assessed palpably for redundancy and plicated where indicated. The capsule was then split transversely as far medially as possible and the bony Bankart lesion prepared as a graft bed. The middle two-thirds of the coracoid were harvested as a free graft using a right angled Micro 100 Oscillating Saw (Hall Surgical, Linvatec, Largo, FL, USA). The coracoid tip and its musculoligamentous attachments were retained and re-attached to the base using small drill holes and transosseous Ethibond (Ethicon, North Ryde, NSW, Australia) sutures after the reconstruction had been completed.
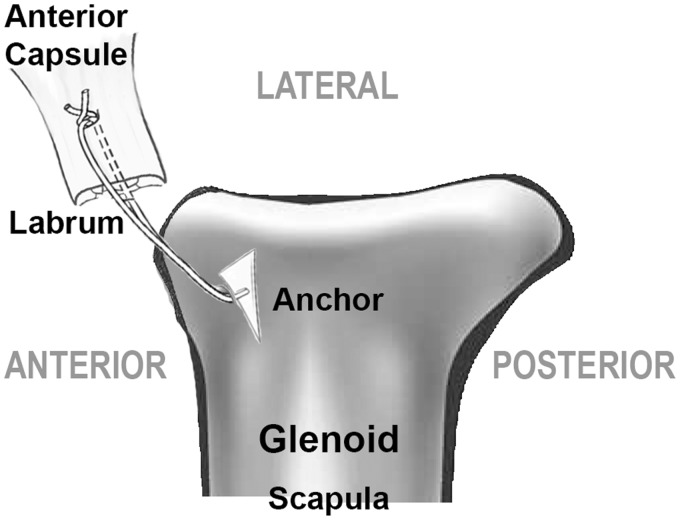
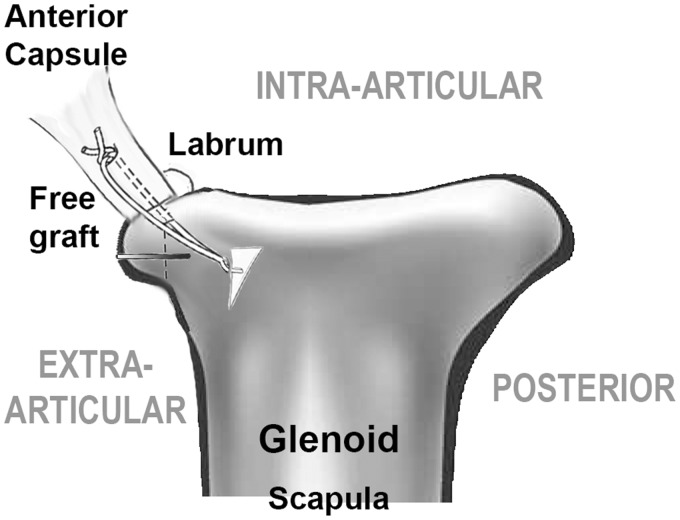
The glenoid defect was freshened and prepared for the graft with the goal of creating a flat surface of glenoid on which the bone block can be stably placed. The coracoid graft should sit flat on the margin of the glenoid defect and 2 mm from the lateral bony margin. The graft was then fashioned with a burr to eliminate any rocking and to produce a curved surface toward the humeral head that matches the curve of the glenoid. Prior to attachment of the graft, multiple Panalok anchors (DePuy Synthes, Warsaw, IN, USA) were inserted on the margin of the glenoid for the labral repair and interpositional capsuloplasty. The sutures were then passed through the labrum as for a normal anterior stabilization without graft (Figure 1). The bone graft was placed on the prepared glenoid bed 2 mm from the lateral bony margin. Fixation was achieved using two bioabsorbable Smart Nails (Linvatec, Largo, FL, USA). The sutures from the anchors through the labrum were then tied creating vertical mattress plication of the capsule and labral repair to snug the capsule inside the bone graft (Figure 2). A capsular shift was performed as necessary and the subscapularis split was repaired. The wound was closed and the arm rested in a sling.
Figure 1.
Attachment of the suture anchor to the glenoid defect.
Figure 2.
Extra-articular attachment of the free bone graft over the Bankart repair.
Rehabilitation
Postoperatively, patients were immobilized in a sling for comfort for a maximum of 2 weeks. Exercises were commenced immediately with active but not passive external rotation and self-assisted active elevation, progressing to active elevation. A physio-guided strengthening programme was instituted after 6 weeks. This involved graduated restoration of terminal external rotation and proprioceptive directed muscle balancing. The average proposed return to noncontact sport was at a minimum of 3 months and to contact sport at 5 months.
Imaging
Finally, standard helical computed tomography (CT) scans to assess graft incorporation on the operated shoulder were requested in all patients in the postoperative period and reviewed by a radiologist and senior surgeon.
Results
Intra-operative findings
All patients demonstrated evidence arthroscopically of having greater than 25% glenoid bone loss. Almost all of them showed evidence of a significant Hill–Sachs lesion. There were two recorded cases of type I SLAP lesions neither requiring repair. One-half of the patients went on to have interval closure carried out accordingly. A mean of four Panalok anchors were used with an average capsular shift of between 2 mm and 5 mm. The mean on-table external rotation at the end of the procedure was 30°.
Clinical
The mean (SD) pre-operative Rowe score was 32.4 (9.85), which significantly improved to 77.2 (19.5) (p < 0.00001) at a mean follow-up of 3 years (range 2 years to 5 years). More specifically, the Rowe function showed 94% as having no or mild loss of function. With regard to range of movement at follow-up, 82% had a minimum of 75% of combined normal internal and external rotation. In terms of stability, there were two true redislocations. Both occurred beyond 2 years following a further injury involving Australian Rules Football. Up to that point, both patients had returned to normal activities in this sport. There were two reported subluxations involving the same sport but no prolonged apprehension. The remaining shoulders remained stable with little to no pain or apprehension.
The ASES score index was available on all cases at over 2 years follow-up. This showed a mean (SD) result of 92 (7.7) (range 67 to 100). Similarly, the Oxford Instability Score at the same follow-up achieved a mean (SD) of 41.2 (6) (range 26 to 48) from 27 responses.
Imaging
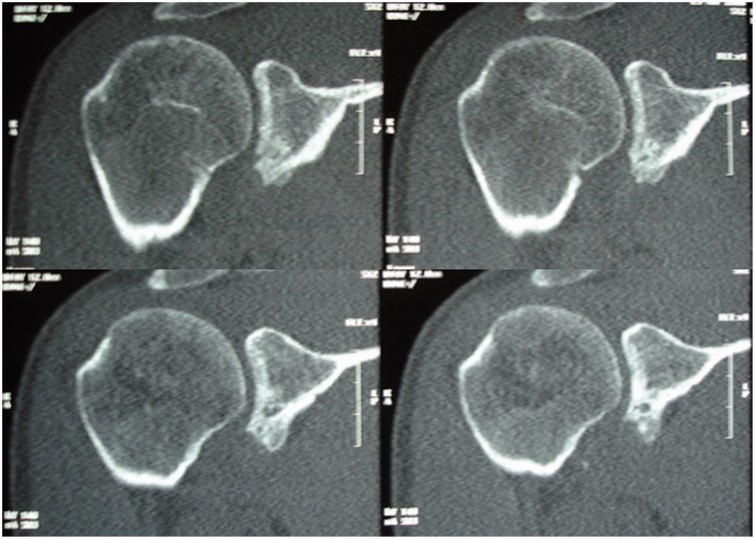
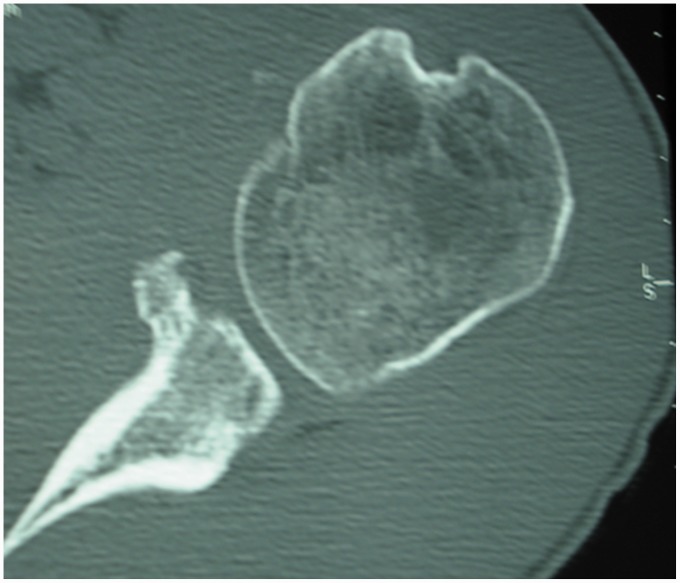
Helical CT scans of the operated shoulder were requested on all patients at mean time of 4.5 months after their surgery. Six patients failed to attend. Twenty-eight scans were available for review by a radiologist and the senior surgeon. Three scans showed non-union, with one showing complete resorption of the graft. Three showed slight resorption, whereas the remaining 22 available (78%) showed evidence of solid union. There was no evidence on CT of graft fracture or migration (Figures 3 and 4). Three-dimensional reconstructions were also added to assess the morphology and appearance of the original glenoid defect (Figure 5). One of the patients who suffered dislocation 3 years after his index surgery when participating in Australian Rules Football had a repeat CT scan with three-dimensional reconstruction, which demonstrates graft fracture (Figure 6).
Figure 3.
Coronal computed tomography images following bony union of the free bone graft.
Figure 4.
Axial computed tomography scan images following bony union of the free bone graft.
Figure 5.
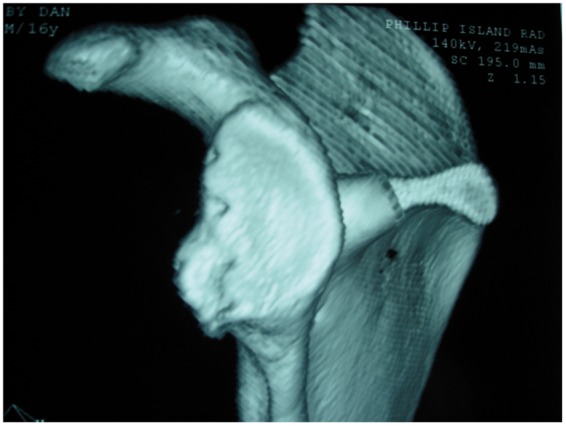
Three-dimensional computed tomography reconstruction of the incoporated graft.
Figure 6.
Three-dimensional computed tomography reconstruction demonstrating a fractured graft after a traumatic dislocation 3 years after the index surgery.
Sport
The majority of these cases of instability occurred as a result of high-risk sports involving overhead high shoulder demand activities (Table 2).
Table 2.
Sports participation among the 34 patients in this case series.
| Sport | n |
|---|---|
| Australian football | 18 |
| Basketball | 3 |
| Soccer | 2 |
| Netball | 1 |
| Cricket | 2 |
| Boxing | 1 |
| Swimming/water polo | 3 |
| Skiing | 2 |
| Tennis | 3 |
At a minimum follow-up of 2 years, 17 (50%) achieved the same level without any restriction, nine (26%) achieved the same level with decreased performance, six (17.6%) returned to a lower-risk sport, and two (5.9%) chose not return to sport for reasons other than their shoulder.
Discussion
Recurrent shoulder instability in the young contact sport athlete represents the most difficult sample of patients for achieving a predictable outcome with success in stabilization surgery. Bone loss greater than 21% to 25% and an engaging Hill–Sachs are increasingly accepted as indications for open surgery and bony adjunct.1,2 Prior studies have demonstrated that there is almost always some amount of bone loss after an acute traumatic dislocation.5,7 Younger patients are predisposed for a bony avulsion given the tensile strength of Sharpey’s fibres at the bony–tendinous junction. Any fragment left is to some extent nonsalvagable compressed bone. In larger fragments greater than 21% to 25%, it is therefore imperative that these patients achieve a bony reconstruction of their glenoid.
All bony techniques try to address the principle of this deficit. Although bone grafts are considered avascular, CT assessment in our group has shown evidence that this type of graft incorprated well with only a 10% non-union rate. Most importantly, there have been no complications with regard to absorbable smart nails impinging, fragmenting or migrating postoperatively, in contrast to patients treated with traditional metal screws.8,9 In addition, re-attachment of the bony coracoid stump has remained asymptomatic in our population.
The most commonly reported techniques of bony glenoid reconstruction involve using free allograft, autograft, or transfer of the coracoid with the attached conjoint tendon in a Bristow–Latarjet.12,16,21 These procedures involve the use of metallic screw fixation to the glenoid neck, which may potentially lead to early arthrosis if the screws impinge on the humeral head or migrate.8,9 Earlier procedures are commonly performed through an approach that divides the subscapularis tendon vertically, which has been shown to be associated with the development of atrophy, fatty infiltration and incomplete healing and a consequent decreased internal rotation strength and lower outcome scores.22,23 The Bristow–Latarjet procedure has also been shown to limit external rotation between 5° and 21° on average.18,24,25 Finally, because the Bristow–Latarjet alters the anatomy anterior to the shoulder joint, it can make revision surgery difficult and potentially put the axillary and musculocutaneous nerves at risk.
Alteration of normal anatomy of the shoulder in stabilization procedures occurs in all cases. Prior studies have extensively evaluated the in vitro biomechanical affects of the Latarjet and other bony glenoid reconstruction techniques.14,17–19 Montgomery et al.14 and Yamamoto et al.19 have both demonstrated that a free bone graft biomechanically restores antero-inferior glenoid stability. Wellman et al. compared the Latarjet to a contoured bony allograft and found that the Latarjet group reduced translation of the glenoid more than the allograft group.17 However, the bone graft was placed intra-articular and a capsular repair was made outside of this, unlike our surgical technique, which includes a Bankart repair followed by extra-articular placement of graft with smart nail fixation. More recently, Yamamoto et al. evaluated the stabilizing mechanism of the Latarjet, and found that the bony glenoid reconstruction contributed 38% to 49% of stability, and the remaining stability was contributed to the conjoint tendons.18 However, the coracoid graft was without a concomitant Bankart repair, which we consider is imperative for adding stability in our described technique.
The free intra-substance coracoid graft and open Bankart repair was designed to address the pathology by restoring the normal anatomy at the same time as avoiding some of the potential pitfalls of the previously described procedures.20 In particular, the ability to use smart nails to stably fix a free autograft bone is beneficial for use in this young patient population plagued with recurrent instability to enable preservation of an essentially virgin shoulder for future revision cases. Young contact sport athletes represent cases with high rates of recurrence for instability surgery.26–29 Our sample includes many of these with evidence of multiple dislocations and subluxations, many with multiple surgeries already when participating in high-risk sports.
We accept that assessment of its effect on function is difficult to measure. Two recent studies evaluated the clinical outcomes of free bone grafts. Weng et al. followed nine patients for a minimum of 4.5 years after intra-articular allograft glenoid reconstruction and reported one dislocation with a mean Rowe score of 84 postoperatively among all patients.16 Warner et al. followed eleven patients for a minimum of 2 years after intra-articular iliac crest autograft and reported no further instability with a mean Rowe score of 94 postoperatively among all patients.
In our case series, free coracoid autograft was selected as a result of its relatively convenient location allowing use of one surgical incision. These grafts are placed extra-articular after a concomittant Bankart repair is performed, which we consider to add to the stability. We currently advocate the use of iliac crest autograft with smart nails in patients aged 22 years and younger, as well as epileptics. The senior author has 10 such cases in an unpublished series, which utilize the same type of repair described in this surgical technique with the exception of utilizing an iliac crest autograft instead of the free coracoid graft. This gives the young patient the best chance for success in our hands, at the same time as not eliminating the possibility of later performing Latarjet or other stabilizations, if necessary, for recurrent instability necessitating revision surgery. The Bristow–Latarjet procedures are reserved for failed cases of recurrent instability in an older age group.
Patient expectations in this young group are commonly to return to the same level of contact sport. Based on our series with an overall dislocation rate of 5.9%, one can expect 76% to return to high-risk sport and, of those, 25% will have some limitation. Given the fact that 17 stabilization procedures had previously been carried out on our sample, this represents an acceptable rate of recurrence.
Conclusions
Extra-articular bony glenoid reconstruction with smart nail fixation of free autograft and Bankart repair can address significant glenoid bony lesions seen in young patients with recurrent anterior shoulder instability. There were no treatment complications. This procedure can provide a surgical option that will preserve the shoulder anatomy. Given the high risk and likelihood of repeat trauma in this contact sport athlete population, it may be advantageous to perform surgeries that will not eliminate future salvage options. Thus far, only two of 34 patients (5.9%) treated in this manner have experienced repeat dislocation and only with significant trauma. These results demonstrate a high rate of success in cases of glenoid bone loss in the young contact athlete with recurrent instability treated with open stabilization and bone grafting.
Declaration of conflicting interests
None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2000; 16: 677–94. [DOI] [PubMed] [Google Scholar]
- 2.Wolf EM, Arianjam A. Hill–Sachs remplissage, an arthroscopic solution for the engaging Hill–Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elb Surg Am Shoulder Elb Surg Al 2014; 23: 814–30. [DOI] [PubMed] [Google Scholar]
- 3.Bigliani LU, Newton PM, Steinmann SP, Connor PM, Mcllveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med 1998; 26: 41–5. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Villalba M, Héry J-Y, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006; 88: 1755–63. [DOI] [PubMed] [Google Scholar]
- 5.Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2003; 19: 732–9. [DOI] [PubMed] [Google Scholar]
- 6.Hovelius L, Lind B, Thorling J. Primary dislocation of the shoulder. Factors affecting the two-year prognosis. Clin Orthop 1983; 176: 181–5. [PubMed] [Google Scholar]
- 7.Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 2003; 85A: 878–84. [DOI] [PubMed] [Google Scholar]
- 8.Young DC, Rockwood CA., Jr Complications of a failed Bristow procedure and their management. J Bone Joint Surg Am 1991; 73: 969–81. [PubMed] [Google Scholar]
- 9.Zuckerman JD, Matsen FA., III Complications about the glenohumeral joint related to the use of screws and staples. J Bone Joint Surg Am 1984; 66: 175–80. [PubMed] [Google Scholar]
- 10.Itoi E, Lee S-B, Amrami KK, Wenger DE, An K-N. Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med 2003; 31: 112–8. [DOI] [PubMed] [Google Scholar]
- 11.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 2000; 82: 35–46. [DOI] [PubMed] [Google Scholar]
- 12.Edwards TB, Walch G. The Latarjet procedure for recurrent anterior shoulder instability: rationale and technique. Oper Tech Sports Med. 2012;20(1):57–64. doi:10.1053/j.otsm.2012.03.007.
- 13.Hovelius L, Körner L, Lundberg B, et al. The coracoid transfer for recurrent dislocation of the shoulder. Technical aspects of the Bristow–Latarjet procedure. J Bone Joint Surg Am 1983; 65: 926–34. [PubMed] [Google Scholar]
- 14.Montgomery WH, Jr, Wahl M, Hettrich C, Itoi E, Lippitt SB, Matsen FA., III Anteroinferior bone-grafting can restore stability in osseous glenoid defects. J Bone Joint Surg Am 2005; 87: 1972–7. [DOI] [PubMed] [Google Scholar]
- 15.Warner JJP, Gill TJ, O’hollerhan JD, Pathare N, Millett PJ. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med 2006; 34: 205–12. [DOI] [PubMed] [Google Scholar]
- 16.Weng P-W, Shen H-C, Lee H-H, Wu S-S, Lee C-H. Open reconstruction of large bony glenoid erosion with allogeneic bone graft for recurrent anterior shoulder dislocation. Am J Sports Med 2009; 37: 1792–7. [DOI] [PubMed] [Google Scholar]
- 17.Wellmann M, Petersen W, Zantop T, et al. Open shoulder repair of osseous glenoid defects: biomechanical effectiveness of the Latarjet procedure versus a contoured structural bone graft. Am J Sports Med 2009; 37: 87–94. [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto N, Muraki T, An K-N, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am 2013; 95: 1390–7. [DOI] [PubMed] [Google Scholar]
- 19.Yamamoto N, Muraki T, Sperling JW, et al. Stabilizing mechanism in bone-grafting of a large glenoid defect. J Bone Joint Surg Am 2010; 92: 2059–66. [DOI] [PubMed] [Google Scholar]
- 20.McCleland D, Bell SN. Free coracoid buttress graft for anterior instability. Tech Shoulder Elb Surg 2005; 6: 214–7. [Google Scholar]
- 21.Bhatia S, Van Thiel GS, Gupta D, et al. Comparison of glenohumeral contact pressures and contact areas after glenoid reconstruction with latarjet or distal tibial osteochondral allografts. Am J Sports Med 2013; 41: 1900–8. [DOI] [PubMed] [Google Scholar]
- 22.Norlin R. Intraarticular pathology in acute, first-time anterior shoulder dislocation: an arthroscopic study. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 1993; 9: 546–9. [DOI] [PubMed] [Google Scholar]
- 23.Singer GC, Kirkland PM, Emery RJ. Coracoid transposition for recurrent anterior instability of the shoulder. A 20-year follow-up study. J Bone Joint Surg Br 1995; 77: 73–6. [PubMed] [Google Scholar]
- 24.Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 1998; 80: 841–52. [DOI] [PubMed] [Google Scholar]
- 25.Symeonides PP. The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J Bone Joint Surg Br 1972; 54: 476–83. [PubMed] [Google Scholar]
- 26.Good CR, MacGillivray JD. Traumatic shoulder dislocation in the adolescent athlete: advances in surgical treatment. Curr Opin Pediatr 2005; 17: 25–9. [DOI] [PubMed] [Google Scholar]
- 27.Kerr ZY, Collins CL, Pommering TL, Fields SK, Comstock RD. Dislocation/separation injuries among US high school athletes in 9 selected sports: 2005–2009. Clin J Sport Med 2011; 21: 101–8. [DOI] [PubMed] [Google Scholar]
- 28.Mazzocca AD. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med 2005; 33: 52–60. [DOI] [PubMed] [Google Scholar]
- 29.Roberts SN, Taylor DE, Brown JN, Hayes MG, Saies A. Open and arthroscopic techniques for the treatment of traumatic anterior shoulder instability in Australian rules football players. J Shoulder Elb Surg Am Shoulder Elb Surg Al 1999; 8: 403–9. [DOI] [PubMed] [Google Scholar]