Abstract
Background
Distal biceps tendinopathy is an uncommon cause of elbow pain. The optimum treatment for cases refractory to conservative treatment is unclear. Platelet-rich plasma has been used successfully for other tendinopathies around the elbow.
Methods
Six patients with clinical and radiological evidence of distal biceps tendinopathy underwent ultrasound-guided platelet-rich plasma (PRP) injection. Clinical examination findings, visual analogue score (VAS) for pain and Mayo Elbow Performance scores were recorded.
Results
The Mayo Elbow Performance Score improved from 68.3 (range 65 to 85) (fair function) to 95 (range 85 to 100) (excellent function). The VAS at rest improved from a mean of 2.25 (range 2 to 5) pre-injection to 0. The VAS with movement improved from a mean of 7.25 (range 5 to 8) pre-injection to 1.3 (range 0 to 2). No complications were noted.
Discussion
Ultrasound-guided PRP injection appears to be a safe and effective treatment for recalcitrant cases of distal biceps tendinopathy. Further investigation with a randomized controlled trial is needed to fully assess its efficacy.
Keywords: Distal biceps, PRP injection, tendinopathy, ultrasound-guided
Introduction
Distal biceps tendinopathy is a relatively uncommon cause of elbow pain. It is characterized by anterior elbow pain exacerbated by repetitive lifting or twisting activities. Clinical examination reveals an intact distal biceps tendon but pain on resisted elbow flexion and supination. By contrast to distal biceps tendon rupture, where surgical repair is advocated,1–6 distal biceps tendinoapthy can, in most cases, be treated conservatively with physiotherapy and activity modification. Corticosteroid injection has traditionally been avoided for this condition given the proximity to neurovascular structures and the risk of tendon rupture, although satisfactory results have been reported with its use.7
Platelet-rich plasma (PRP) injection is becoming an increasingly popular treatment for tendinopathies at various anatomical sites.8–11 Favourable results have been shown with its use for lateral epicondylitis.12,13 As far as we aware, there have been no previous reports in the literature of the use of PRP injections for the treatment of distal biceps tendinopathy. We report the magnetic resonance imaging findings (MRI) findings, ultrasound-guided injection technique and clinical results obtained in a small cohort of six patients.
Materials and methods
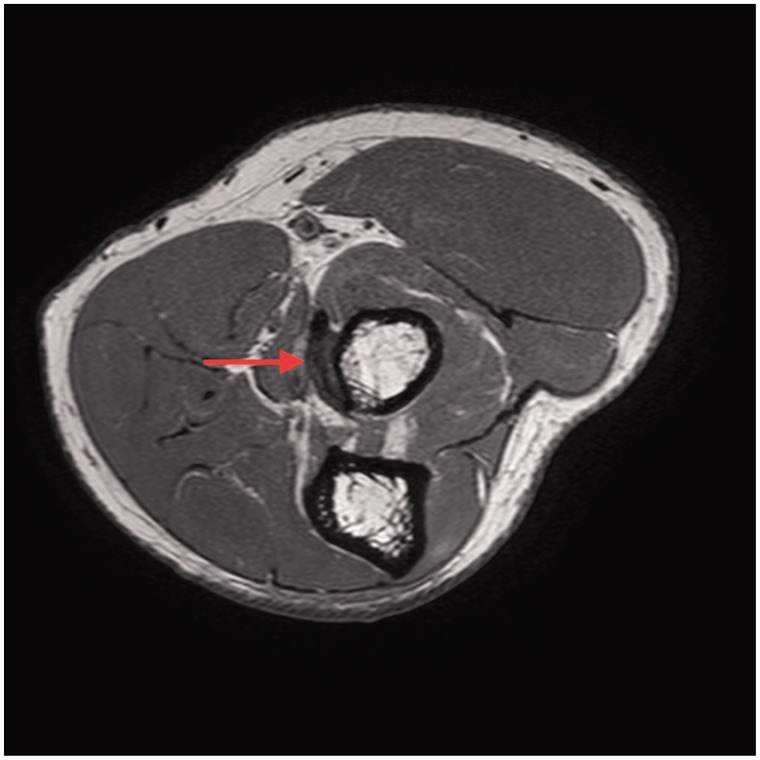
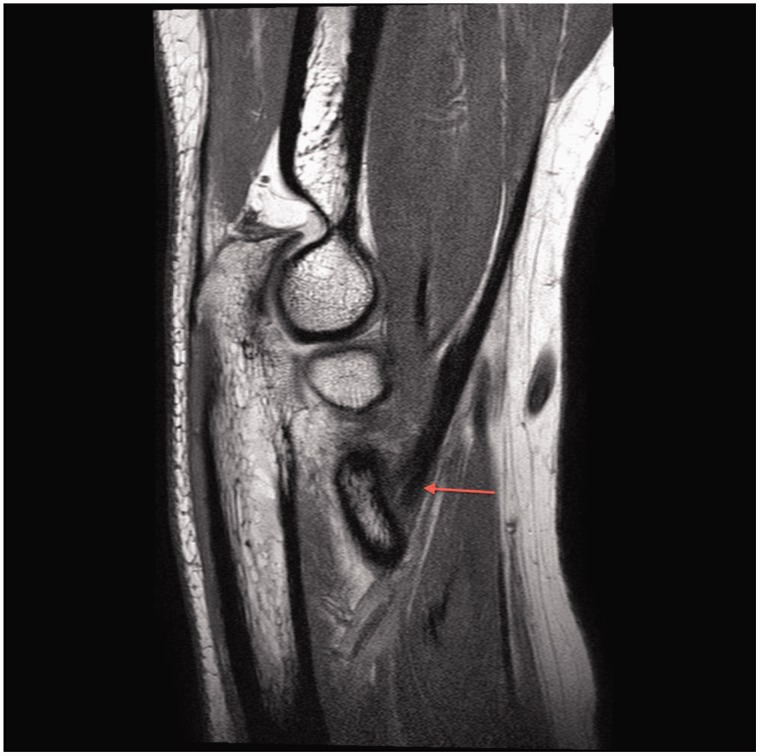
Six patients with a diagnosis of distal biceps tendinopathy, treated with ultrasound-guided PRP injection, were identified from the senior author’s database. Conservative treatment measures had failed. In all cases, distal biceps tendinopathy was diagnosed clinically. The ‘Hook test’14 was used to confirm that the biceps tendon was intact. Resisted flexion and supination (distal biceps provocation test) resulting in discomfort in the anterior aspect of the elbow indicated pathology in the distal biceps tendon. The clinical diagnosis was confirmed by an MRI scan in five patients and ultrasound in one patient. Standard T1 and T2 sequences with the elbow in extension were used. Although the FABS (flexion, abduction, supination) position15 has been described as optimal for visualizing the distal biceps tendon on MRI, adequate images for diagnosis were obtained on standard views and therefore the FABS position was not utilized (Figure 1 and 2).
Figure 1.
Magnetic resonance imaging axial T1. Mild thickening with hyperintensity of distal biceps (red arrow).
Figure 2.
Magnetic resonance imaging sagittal T1. Mild thickening with hyperintensity of distal biceps (red arrow).
A standardized technique for ultrasound-guided PRP injection was performed. In total, 10 mL of blood was drawn from the contralateral arm into a CPDA (citrate phosphate dextrose adenine) blood tube. This was centrifuged for 7 min at 2700 revolutions per minute (r/min). The central ‘buffy coat layer’ containing approximately 3 mL of PRP was syphoned from the centrifuged tube. According to the Sports Medicine PRP Classification system, this is Type 1B PRP (leucocyte rich, no activation, platelet concentration <5 × serum).16
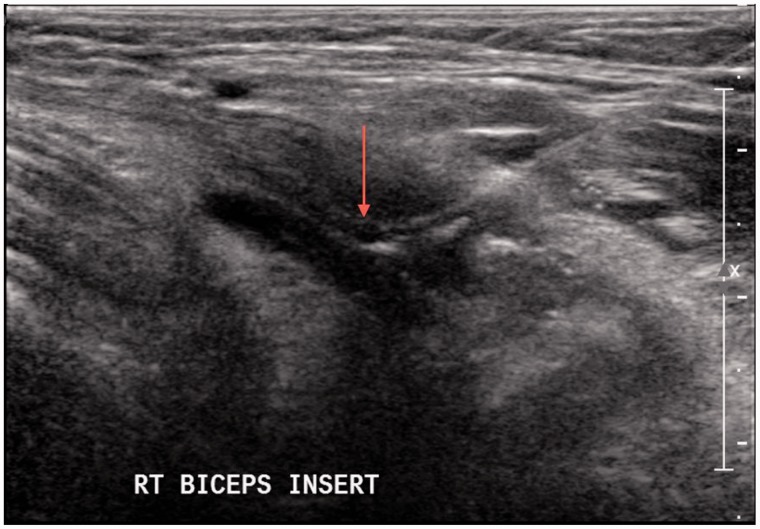
Longitudinal orientation of the ultrasound probe was used to visualize the distal biceps tendon. After injection of 3 mL of bupivacaine local anaesthetic into the bicipital bursa, the distal biceps tendon was injected with the PRP. A dry needling technique was utilized to create intrasubstance cleavage planes within the tendon for the PRP to be injected into (Figure 3).
Figure 3.
Ultrasound-guided platelet-rich plasma injection into distal biceps tendon (red arrow).
No specific physiotherapy was employed. Heavy repetitive activity with the affected arm was to be avoided for 6 weeks post-injection.
Data were collected prospectively with pre-injection outcome scores and clinical examination findings recorded at the initial clinical review. The senior author (SNB) performed further clinical assessment approximately 6 weeks after each PRP injection. Postal questionnaires were used as the final follow-up assessment to avoid patients having the inconvenience of attending an unnecessary clinic appointment.
A modified Mayo Elbow Performance Score was used both pre- and post-injection. Pain, motion, stability and function were subjectively assessed to give a maximum total score of 100.
Visual analogue scores (VAS) (0 to 10) for pain (VAS pain) at rest and with movement were also recorded.
In addition, as part of the final follow-up postal questionnaire, two ‘Yes/No’ questions were asked: (i) is your elbow better than it was prior to the injection and (ii) if your symptoms recurred, would you have a repeat injection?
Results
The clinical history and radiological findings for each patient are summarized.
Patient 1
The patient was a 55-year-old male. Symptoms were precipitated by minor injury when hitting a punch bag during martial arts training. MRI showed ‘mild insertional biceps tendinopathy’.
Patient 2
The patient was a 37-year-old male. Symptoms were precipitated by hyperextension injury at work when his arm caught in a machine. MRI showed ‘mild thickening and hyperintensity of the biceps tendon where it inserts onto the radial tuberosity but no partial tear is seen’.
Patient 3
The patient was a 42-year-old male. No specific injury. Symptoms were exacerbated by repetitive lifting when working as a landscape gardener. MRI showed ‘there is hyperintensity and thickening of the distal biceps tendon where it approaches the radial tuberosity’.
Patient 4
The patient was a 68-year-old female. Symptoms were precipitated by minor injury following a mis-hit backhand shot when playing tennis. MRI showed ‘the major abnormality relates to the distal biceps tendon. The tendon itself is thickened, hyperintense. The extreme distal aspect of the tendon is almost impossible to identify and I suspect there is a high-grade partial tear’.
Patient 5
The patient was a 36-year-old male. No specific injury. Symptoms were exacerbated by repetitive weight training at the gym. MRI showed ‘oedema is present at the distal biceps insertion consistent with enthesopathy’.
Patient 6
The patient was a 34-year-old female. No specific injury. Symptoms were exacerbated by repetitive activity working as a hairdresser. She elected not to have MRI as she was pregnant. Ultrasound showed ‘there is mild thickening and hypoechoic change of the distal biceps tendon where it inserts onto the greater tuberosity’.
Four patients were male and two were female. All were right handed; the dominant arm was affected in four patients and the nondominant in two. Three patients had minor injuries that precipitated their symptoms; the other three had no injury but felt that their symptoms were related to repetitive activity of the affected arm. All patients had a clinically intact distal biceps tendon and a positive distal biceps provocation test. Five patients had at least 6 months of conservative treatment prior to the PRP injection. This consisted of anti-inflammatories, physiotherapy and activity modification. One patient was referred for PRP injection 2 months after the onset of symptoms. As a result of the severity of her symptoms and the presence of a partial tear on her MRI scan, it was felt that early intervention was indicated.
Four patients had one PRP injection. At the 6-week post-injection clinical assessment, their symptoms had resolved and their distal biceps provocation tests were negative.
Two patients had two PRP injections. This included the aforementioned patient with a partial tear on MRI. At the 6-week clinical assessment, although their symptoms had improved to a degree, their distal biceps provocation tests were still positive and they were referred for a repeat injection. Further clinical assessment at 6 weeks after the repeat injection was performed. Both patients had further improvement in their symptoms with negative distal biceps provocation tests.
The average age at presentation was 45.3 years (range 34 years to 68 years). The average duration of symptoms was 9 months (range 2 months to 24 months). The average final follow-up with postal questionnaires was 16.3 months (range 12 months to 30 months).
The mean modified Mayo Elbow Performance Score pre-injection was 68.3 (range 65 to 85), classified as fair function. This improved to a mean of 95 (range 85 to 100), classified as excellent function, at final follow-up (P = 0.03125 Wilcoxon rank test, SPSS, version 22.0; IBM Corp., Armonk, NY, USA)
The VAS pain at rest improved from a mean of 2.25 (range 2 to 5) pre-injection to 0 at final follow-up. The VAS pain with movement improved from a mean of 7.25 (5 to 8) pre-injection to 1.3 (range 0 to 2) at final follow-up.
All six patients felt that they were better than they were prior to the injection. All six patients would have another injection if their symptoms recurred.
No complications were noted.
Discussion
Ultrasound-guided PRP injection appears to be a safe and efficacious treatment for distal biceps tendinopathy. All six patients reviewed in our series had almost complete resolution of their symptoms with a return to normal function. Early improvement in symptoms with resolution of clinical signs by 6 weeks was evident in four patients. Although a repeat injection was required in two patients, this resulted in further improvement and resolution of clinical signs in both cases. At final follow-up (minimum of 1 year), the improvement in symptoms was maintained.
As tendinopathies are now generally accepted as a degenerative rather than inflammatory process,17 the use of PRP to stimulate tendon healing is more logical than the use of corticosteroid. Growth factors, cytokines and chemokines released by platelets stimulate protein production in the target cells responsible for cellular proliferation and collagen synthesis. Proteins contained in PRP also act as cell adhesion molecules and promote fibroblast migration. It is therefore suggested that activation of these cells by PRP promotes tendon healing.18
Our results compare favourably with those of Maree et al. with respect to their study using ultrasound-guided corticosteroid injection for the treatment of distal biceps tendinopathy.7 In total, 73% of their patients had complete resolution of their symptoms compared to 83.3% in our smaller series. They adopted a different injection technique, choosing to inject the steroid directly onto the bony radial tuberosity. Our technique of ultrasound-guided intrasubstance injection of PRP is safe and reproducible. The needle is easily visualized within the biceps tendon; meaning that accurate placement of the PRP is achieved. The potential for damage to nearby neurovascular structures is minimal. Dry needling of the tendon is an important part of the technique. Although dry needling itself may contribute to the tendon healing process, the addition of PRP has been shown to have a beneficial effect.19
Our method of PRP preparation is quick, easy and reliable. It gives a platelet concentration of approximately two to three times serum. Although other methods of PRP preparation result in higher platelet concentrations, there is no consensus as to which type of PRP is actually best. Platelet concentrations greater than five times normal may actually have a detrimental effect on tendon healing.20
The main weakness of the present study is the small number of patients. Distal biceps tendinopathy is, however, a rare condition. There is very little published literature on its aetiology, treatment or natural history.21 There is no figure quoted in the literature regarding the incidence of distal biceps tendinopathy but it is considered to be less than that of distal biceps rupture, which is in the region of 1.2 in 100,000.21,22 In particular, there is no published evidence regarding the natural history of distal biceps tendinopathy. It is not clear whether this condition goes on to resolution with conservative treatment or whether it is a precursor to complete rupture. No cohort group of patients who were treated conservatively was available for comparison. We therefore accept that it is possible that the symptoms of the patients in our series may have eventually settled with prolonged continued conservative treatment. It should be pointed out, however, that five out of six patients had at least 6 months of conservative treatment with no sign of improvement. Following PRP injection, their symptoms improved rapidly. This improvement was maintained over the long term.
The senior author (SNB) sees approximately 1450 new patients with shoulder and elbow problems each year. In the 4-year period (2010 to present) during which PRP injection has been available, there have only been seven cases diagnosed with distal biceps tendinopathy. Six of these cases had PRP injections as described. In the other case, the patient travelled overseas and elected not to have the injection.
A randomized controlled trial comparing PRP injection to placebo would be required to further prove the efficacy of PRP injection for distal biceps tendinopathy. If a difference in improvement in the Mayo Elbow Performance Score of 10 points, or VAS pain score of 2 points,23 is taken to be significant, using the SD from the scores in our series, assuming p < 0.05 and a power of 80%, the number of patients in each arm would need to be 17. Given the rarity of this condition, recruiting 34 patients would require a multicentre trial and would take a period of several years. We are currently assessing the viability of performing this study.
Conclusions
Although our numbers are small, ultrasound-guided PRP injection does appear to be a safe and effective treatment for distal biceps tendinopthy. We would recommend its use for cases refractory to conservative treatment.
Acknowledgments
We would like to thank Mr Ken Sharpe, Statistician, Statistical Consulting Centre, Richard Berry Building, University of Melbourne, Parkville, VIC 3052, Australia, for his help with the statistical analysis.
Note
This paper has not been presented prevously.
Declaration of conflicting interests
None declared.
Funding
No funding was required for this research.
References
- 1.Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg 1985; 67: 418–21. [PubMed] [Google Scholar]
- 2.Rantanen J, Orava S. Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med 1999; 27: 128–32. [DOI] [PubMed] [Google Scholar]
- 3.Miyamoto RG, Elser F, Millett PJ. Distal biceps tendon injuries. J Bone Joint Surg 2010; 92: 2128–38. [DOI] [PubMed] [Google Scholar]
- 4.Bain GI, Johnson LJ, Turner PC. Treatment of partial distal biceps tendon tears. Sports Med Arthrosc Rev 2008; 16: 154–61. [DOI] [PubMed] [Google Scholar]
- 5.Cohen MS. Complications of distal biceps tendon repairs. Sports Med Arthrosc Rev 2008; 16: 148–53. [DOI] [PubMed] [Google Scholar]
- 6.Frazier MS, Boardman MJ, Westland M, Imbriglia JE. Surgical treatment of partial distal biceps tendon ruptures. J Hand Surg 2010; 35: 1111–4. [DOI] [PubMed] [Google Scholar]
- 7.Maree MN, Vrettos BC, Roche SJL, Osch GV. Distal biceps tendinopathy: conservative treatment. Shoulder Elbow 2011; 3: 104–8. [Google Scholar]
- 8.Paoloni J, De Vos RJ, Hamilton B, Murrell GA, Orchard J. Platelet-rich plasma treatment for ligament and tendon injuries. Clin J Sport Med 2011; 21: 37–45. [DOI] [PubMed] [Google Scholar]
- 9.Rabago D, Wilson J, Zgierska A. Platelet-rich plasma for treatment of Achilles tendinopathy. JAMA 2010; 303: 1696–7. [DOI] [PubMed] [Google Scholar]
- 10.Creaney L, Wallace A, Curtis M, Connell D. Growth factor-based therapies provide additional benefit beyond physical therapy in resistant elbow tendinopathy: a prospective, single-blind, randomised trial of autologous blood injections versus platelet-rich plasma injections. Br J Sports Med 2011; 45: 966–71. [DOI] [PubMed] [Google Scholar]
- 11.Kesikburun S, Tan AK, Yilmaz B, Yasar E, Yazicioglu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med 2013; 41: 2609–16. [DOI] [PubMed] [Google Scholar]
- 12.Mishra AK, Skrepnik NV, Edwards SG, et al. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med 2014; 42: 463–71. [DOI] [PubMed] [Google Scholar]
- 13.Gosens T, Peerbooms JC, van Laar W, den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med 2011; 39: 1200–8. [DOI] [PubMed] [Google Scholar]
- 14.O'Driscoll SW, Goncalves LB, Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med 2007; 35: 1865–9. [DOI] [PubMed] [Google Scholar]
- 15.Giuffre BM, Moss MJ. Optimal positioning for MRI of the distal biceps brachii tendon: flexed abducted supinated view. AJR Am J Roentgenol 2004; 182: 944–6. [DOI] [PubMed] [Google Scholar]
- 16.Mishra A, Harmon K, Woodall J, Vieira A. Sports medicine applications of platelet rich plasma. Curr Pharm Biotechnol 2012; 13: 1185–95. [DOI] [PubMed] [Google Scholar]
- 17.Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg 2005; 87: 187–202. [DOI] [PubMed] [Google Scholar]
- 18.Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg 2009; 91: 987–96. [DOI] [PubMed] [Google Scholar]
- 19.Stenhouse G, Sookur P, Watson M. Do blood growth factors offer additional benefit in refractory lateral epicondylitis? A prospective, randomized pilot trial of dry needling as a stand-alone procedure versus dry needling and autologous conditioned plasma. Skeletal Radiol 2013; 42: 1515–20. [DOI] [PubMed] [Google Scholar]
- 20.Dhillon MS, Behera P, Patel S, Shetty V. Orthobiologics and platelet rich plasma. Indian J Orthopaed 2014; 48: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donaldson O, Vannet N, Gosens T, Kulkarni R. Tendinopathies around the elbow part 2: medial elbow, distal biceps and triceps tendinopathies. Shoulder Elbow 2014; 6: 47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthopaed Rel Res 2002; 404: 275–83. [PubMed] [Google Scholar]
- 23.Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 2004; 8: 283–91. [DOI] [PubMed] [Google Scholar]