Introduction
Definition
Frozen shoulder is an extremely painful and debilitating condition leading to stiffness and disability. It typically occurs in the fifth and sixth decades of life, thus affecting individuals of working age. The disability resulting from this condition has considerable economic impact on affected individuals and society.
Frozen shoulder can be either primary (idiopathic) or secondary. Secondary frozen shoulder is defined as that associated with trauma; rotator cuff disease and impingement; cardiovascular disease; hemiparesis; or diabetes (although some classify this in diabetics as primary frozen shoulder). The incidence of frozen shoulder in people with diabetes is reported to be 10% to 36%, and these tend not to respond as well to treatment as in nondiabetics.1
Clinical presentation is typically in three overlapping phases:1
Phase 1 – lasting 2 months to 9 months. Painful phase, with progressive and increasing pain on movement. Pain tends to be constant and diagnosis in the early stages before movement is lost can be difficult.
Phase 2 – lasting 4 months to 12 months. Stiffening or freezing, where there is gradual reduction of pain but stiffness persists with considerable restriction in range of motion. Pain pattern changes from constant to end range pain of reduced intensity.
Phase 3 – lasting 12 months to 42 months. Resolution or thawing phase, where there is improvement in range of motion with resolution of stiffness. End range pain may persist until full resolution.
Because there tends to be considerable overlap between the phases, more recent terminology favours classifying the condition into ‘pain predominant’ and ‘stiffness predominant’ phases.
Shared decision-making
The General Medical Council’s Good Medical Practice2 clearly states in the section on working in partnership with patients that doctors should:
Listen to patients and respond to their concerns and preferences.
Give patients the information they want or need in a way they can understand.
Respect patients’ right to reach decisions with the doctor about their treatment and care.
Support patients in caring for themselves to improve and maintain their health.
This can only be achieved by direct consultation between the patient and their treating clinician. Decisions about treatment taken without such direct consultation between patient and treating clinician are not appropriate, as they do not adhere to principles of good medical practice.
Continuity of care
Continuity and co-ordination of care are essential parts of the General Medical Council’s Good Medical Practice guidance.2 It is therefore inappropriate for a clinician to treat a patient if there is no clear commitment from that clinician or the healthcare provider to oversee the complete care pathway of that patient including their diagnosis, treatment, follow-up and adverse event management.
Background
The prevalence of shoulder complaints in the UK is estimated to be 14%, with 1% to 2% of adults consulting their general practitioner annually regarding new-onset shoulder pain.3
Painful shoulders pose a substantial socioeconomic burden. Disability of the shoulder can impair ability to work or perform household tasks and can result in time off work.4,5 Shoulder problems account for 2.4% of all general practitioner consultations in the UK and 4.5 million visits to physicians annually in the USA.6,7 The annual financial burden of shoulder pain management in the USA has been estimated to be US$3 billion.8
Cumulative incidence of frozen shoulder is estimated at 2.4 per 1000 population per year.9 This condition was first described in 1875 by the French Pathologist Duplay, who named it ‘peri-arthrite scapula-humerale’. The American surgeon E. A. Codman proposed the name ‘frozen shoulder’ in 1934.10 However, there is an acknowledged absence of a specific definition of the condition11,12 and of a diagnostic label12, with additional names for frozen shoulder including retractile capsulitis, adhesive capsulitis, check rein shoulder, contracted shoulder and steroid-sensitive arthritis.
There are different views about the underlying fundamental process: inflammation, reactive angiogenesis and scarring, each involving the shoulder capsule in different stages of the disease.13 The scarring and capsular contracture reduces joint volume to 3 ml to 4 ml compared to a normal capsular volume of 10 ml to 15 ml. Histological studies of the capsule have confirmed significant increase in fibroblasts with presence of myofibroblasts. In addition, inflammatory cells (mast cells, T cells, B cells and macrophages) have been identified, suggesting a process of inflammation leading to scarring.14
To generalize and consider this a self-limiting condition can be misleading because there is variation across published reports in the proportion of patients who do not regain full shoulder motion,1 possibly a reflection of variation in how outcome was assessed. Based on the largest published series of patients with mean follow-up of 4.4 years from onset of symptoms, 59% made full recovery, 35% had mild to moderate symptoms, with pain being the most common complaint, and 6% had severe symptoms at follow-up.15 Recurrence is unusual, although the contralateral shoulder gets affected in 6% to 17% of patients within 5 years.
Frozen shoulder: care pathway
Aims of treatment
The overall treatment aim for the conditions that cause frozen shoulder is to ‘improve pain and function’; however, treatment success needs to be defined individually with patients in a shared decision-making process. The degree of improvement and level of acceptance to a patient will depend on starting level of symptoms, patient demographics, personal circumstances and patient expectations.
Pre-primary care (at home)
For causes of glenohumeral shoulder pain, there is potential for simple patient self-management strategies and prevention strategies at home prior to the need for a general practitioner consultation, although research to develop and assess the impact of such strategies would be needed.
Assessment in primary care/community triage services
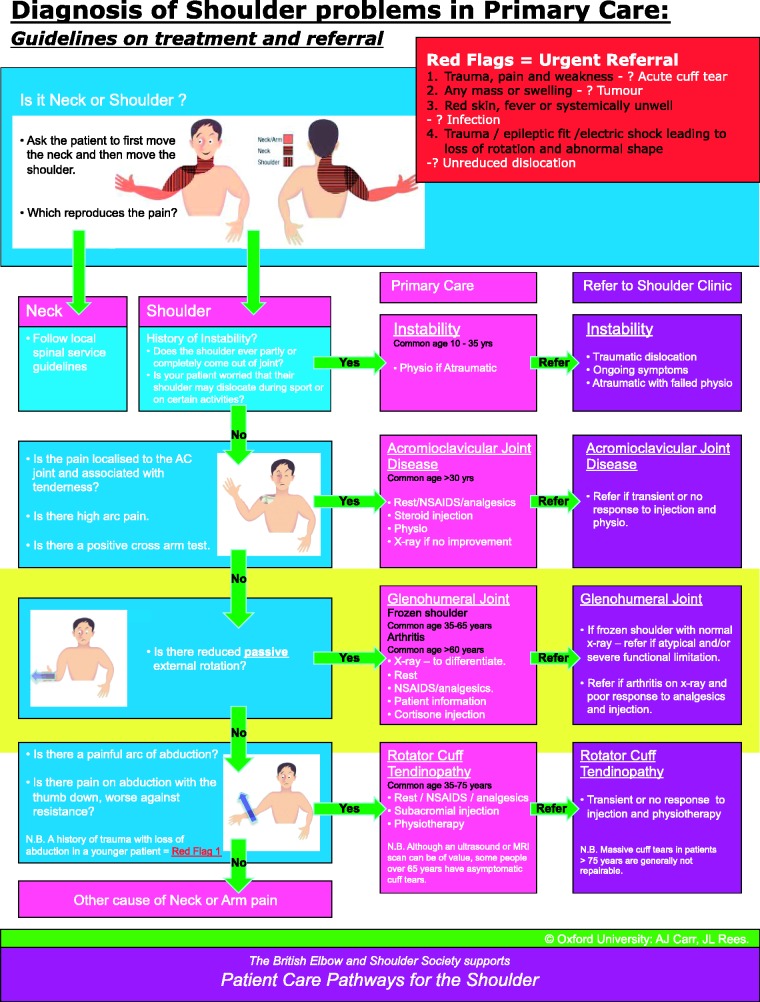
Diagnosis is based on history and examination (Fig. 1)
Making the correct diagnosis is crucial, and will ensure an efficient and optimum treatment for the patient.
- Features of importance are;
- ○ Hand dominance
- ○ Occupation and level of activity or sports
- ○ Location, radiation and onset of pain
- ○ Duration of symptoms (see phases of disease in the Definition earlier above)
- ○ Global reduction in range of motion with a capsular pattern, defined as disproportionately severe loss of passive external rotation in the affected shoulder with arm by the side, over other movements.
- ○ History of diabetes, cardiovascular disease or other associations.
- ○ Normal X-rays in two planes to rule out mechanical glenohumeral incongruity such as arthritis, avascular necrosis or dislocation of the shoulder, which produce a similar clinical picture.
Figure 1.
Diagnosis of shoulder problems in primary care. Guidelines on treatment and referral.
Red flags for the shoulder
Acute severe shoulder pain needs proper and competent diagnosis. Any shoulder ‘red flags’ identified during primary care assessment needs urgent secondary care referral.
A suspected infected joint needs same day urgent referral.
An unreduced dislocation needs same day urgent referral.
Suspected malignancy or tumour needs urgent referral following the local 2-week cancer referral pathway.
An acute cuff tear as a result of a traumatic event needs urgent referral and ideally should be seen in the next available outpatient clinic.
Suspected inflammatory oligo or poly-arthritis or systemic inflammatory disease should be considered as a ‘rheumatological red flag’ and local rheumatology referral pathways should be followed.
Treatment in primary care/community triage services
- Treatment depends on the phase of the disease, severity of symptoms and degree of restriction of work, domestic and leisure activities. The aims of treatment are:
- ○ Pain relief
- ○ Improving range of motion
- ○ Reducing duration of symptoms
- ○ Return to normal activities
- Following interventions are suitable for primary care:
- ○ Analgesics/nonsteroidal anti-inflammatory drugs (NSAIDs)
- ○ Corticosteroid injection
- ○ Domestic exercise programme
- ○ Supervised physiotherapy/manual therapy
This is a painful and debilitating condition, where the pain is often severe, mimicking malignant disease (e.g. night pain). The onset of stiffness may be rapid, and cause significant functional deficit, typically in individuals of working age. Treatment should be tailored to individual patient needs depending on response and severity of symptoms.
Beware of red flags such as tumour, infection, unreduced dislocation or inflammatory polyarthritis.
Overall, a step-up approach may be adopted in terms of degree of treatment invasiveness. Some patients may have particular treatment preferences based on their needs and referral to secondary care may need to be considered early in such circumstances. Shared decision-making is particularly important for this condition.
A proportion of patients with frozen shoulder will respond to conservative treatment, and the response needs to be monitored. The most frequent indications for invasive treatments are persistent and severe functional restrictions that are resistant to conservative measures.
Symptoms usually of up to 3 months with failure of conservative treatment measures may trigger referral to secondary care for consideration of more invasive treatment. Severity of symptoms may necessitate earlier referral; it would not be appropriate to persist with ineffective treatment measures and delay referral of patients who experience severe pain and restriction.
Shared decision-making is important, and individual patients’ needs are different. Failure of initial treatment to control pain, if degree of stiffness causes considerable functional compromise, or if there is any doubt about diagnosis, prompt referral to secondary care is indicated.
Physiotherapy rehabilitation is usually for 6 weeks unless patients are unable to tolerate the exercises, or physiotherapists identify a reason for earlier referral to secondary care. If there is patient improvement in the first 6 weeks of physiotherapy, then a further 6 weeks of therapy is justified.
Treatment timelines should include primary care and intermediate care time. Intermediate care should not delay appropriate referral to secondary care.
Secondary care
In a UK study of patterns of referral of shoulder conditions, 22% of patients were referred to secondary care up to 3 years following initial presentation, although most referrals occurred within 3 months.16 There is little evidence available on referral patterns for frozen shoulder specifically.
Confirm diagnosis with history and examination.
Obtain imaging with plain radiographs to rule out mechanical glenohumeral incongruence such as arthritis, avascular necrosis or dislocation.
Counsel patient fully regarding operative and non-operative options.
Ensure multidisciplinary approach to care with availability of specialist shoulder physiotherapists and shoulder surgeons.
The most commonly used secondary care interventions are:
○ Manipulation under anaesthesia (MUA)
○ Arthroscopic capsular release (ACR)
○ Distension arthrogram (DA) or hydrodilatation
○ Physiotherapy and corticosteroid injection, usually to supplement any of the above interventions
If symptoms fail to resolve with conservative treatment, then MUA, DA or ACR may be considered. This choice depends mainly on expertise and clinician preference.
MUA is performed under general anaesthesia where the arm is manipulated to ‘tear’ the contracted shoulder capsule in a controlled fashion, thus restoring external rotation and other movements. This is supplemented with corticosteroid injection for pain relief and with physiotherapy to maintain range of motion post MUA.
ACR involves arthroscopic surgery under general anaesthesia. The contracted capsule is released in a controlled fashion using arthroscopic instruments, frequently with radiofrequency ablation. The most prominent contracture occurs anteriorly and release of this improves external rotation. The inferior capsule may be released with arthroscopic instruments, or with a controlled MUA.
DA is a procedure where the shoulder capsule is injected with saline and local anaesthetic under pressure to distend and disrupt the capsule. This procedure is usually performed by an interventional radiologist, and does not require general anaesthesia. It is performed under fluoroscopy or ultrasound guidance and a radio-opaque dye may be used to confirm accuracy of placement of the injected fluid. Both DA and ACR are supplemented with post-procedural physiotherapy to maintain range of motion in the affected shoulder.
- It would be expected that surgical units performing ACR or MUA:
- ○ Ensure patients undergo appropriate pre-operative assessment to ensure fitness for surgery and to confirm discharge planning.
- ○ Perform surgery or MUA in appropriately resourced and staffed units.
- ○ Both procedures are typically performed as day care or 23-hour admission (depending on the time of the day the procedure takes place), unless clinical or social circumstances dictate otherwise.
- ○ Standard postoperative care should involve prompt start of physiotherapy and pain relief as required.
- ○ Physiotherapy services vary across the country, although up to 12 weeks of physiotherapy are typically required to maintain range of motion in the treated shoulder.
- ○ Up to three outpatient follow-up appointments may be needed, depending on progress.
Linked metrics
Current interventions
BESS has led a survey of health professionals to determine treatment pathways in current use in the UK, aiming to inform design of future studies of effectiveness of interventions for frozen shoulder.
MUA for frozen shoulder
Diagnosis codes M750.
Procedure codes (OPCS 4.5) W919, Z814.
ACR
Diagnosis codes M750.
Procedure codes (OPCS 4.5) W784, Y767, Z814.
Outcome metrics
Length of stay – day case (23 hours) and overnight.
Re-admission rate within 90 days.
Patient-reported outcome measure (PROM) pre-procedure, and 12 months post-procedure.
Infection/other adverse events.
Research and audit
In partnership with Centre for Reviews and Dissemination in York, BESS members were commissioned to conduct an evidence synthesis on frozen shoulder by the National Institute for Health Research Health Technology Assessment (NIHR-HTA) Program. This report titled ‘Management of frozen shoulder: a systematic review and cost-effectiveness analysis’ has now been published, and forms a key reference document that summarises current evidence, and areas for future research on this topic.17
A recent survey of health professionals in the UK has found that the professional groups (general practitioners, general practitioner with a special interest, physiotherapists, orthopaedic surgeons) had different views on the most appropriate treatment pathway for the frozen shoulder.18. There was, however, consensus that treatment should depend on phase of the disease and a step-up approach would be appropriate.
In addition, a scoping review identified that most previous reviews have concentrated on one particular intervention and there is general paucity of good primary research on frozen shoulder.19
Members of BESS involved in the above evidence syntheses are currently designing an interventional trial for frozen shoulder investigating commonly used interventions for management in secondary care.
A validated clinical score, preferably a PROM, should be used pre-operatively and following treatment.
Acceptable scores include the Shoulder Pain and Disability Index (SPADI), Disability of Arm, Shoulder and Hand (DASH) and the Oxford Shoulder Score (OSS). The disability subscale of the SPADI has been used by several published reports for this condition. Other measures such as EQ 5D may be used for economic analysis.
Scores should be captured pre-operatively and 1 year following intervention, which allows longitudinal analysis to determine sustenance of treatment effect and consequences of any treatment-related adverse events.
Patient/public/clinician information
Patient and public information – ensure all available information is provided regarding the benefits and risks of all treatment options
Clinician information – ensure access to available evidence.
Evidence for effectiveness and cost effectiveness of treatment
NIHR-HTA commissioned evidence synthesis has led to publication of report titled ‘Management of frozen shoulder: a systematic review and cost-effectiveness analysis’.17 This report provides full details of methodology, search strategy, economic analysis, decision model, and suggestions for future research. An analysis of the effectiveness and cost effectiveness of interventions from available primary research is also included in this report.
Summary
It is important to note that evidence to support the effectiveness of conservative treatment, surgical treatment or the potential benefit of one over the other remains limited. Until such evidence becomes available, clinical and shared decision-making on accessing available interventions based on level of symptoms and functional restriction is recommended.
Corticosteroid injection. Based on best available evidence, corticosteroid injection has mainly short-term benefit with a single injection. There appears to be added benefit with providing physiotherapy promptly following steroid injection compared to home exercise alone and physiotherapy alone.20–23 There is insufficient evidence to conclude with reasonable certainty in what clinical situations steroid injection, with or without physiotherapy, is most likely to be effective for treatment of frozen shoulder.
Sodium hyaluronate injection. A small number of diverse studies, all of which may have a high risk of bias, provide insufficient evidence to make conclusions about effectiveness of sodium hyaluronate in the treatment of frozen shoulder.24–26
Physiotherapy/physical therapy. Primary studies comparing different types of physiotherapy/physical therapies support the use of various techniques to provide short- to medium-term benefit. Some interventions in current use that were investigated include therapeutic ultrasound,27 end range mobilization,28 short-wave diathermy plus stretching29 and high-grade mobilization therapy.30 These interventions should be stage of disease and response-dependent. Based on best available evidence, there may be benefit from short-wave diathermy plus stretching and high-grade mobilization techniques in patients who have already had physiotherapy or a steroid injection. There is insufficient evidence to make conclusions on best mode of physiotherapy for frozen shoulder
Acupuncture. The role of acupuncture in treatment of frozen shoulder is not clear. Available evidence does not demonstrate clear benefit.
Oral drug treatment
Likely to be beneficial
NSAIDS (oral) reduce pain in people with acute capsulitis.
Unknown effectiveness
Oral corticosteroids, opioid analgesics and paracetamol.
Topical drug treatment
Unknown effectiveness
NSAIDs (topical).
Local injections
Likely to be beneficial
Intra-articular corticosteroid.
Unknown effectiveness
Hyaluroinc acid injections.
Nondrug treatment
Likely to be beneficial
Short-wave diathermy and stretching.
Physiotherapy (manual treatment, exercises).
Unknown effectiveness
Acupuncture.
Electrical stimulation.
Distension arthrogram
Surgery
Likely to be beneficial
ACR.
MUA.
Additional evidence regarding the effectiveness of surgery
Evidence to support MUA remains limited. Most published studies have limitations. Their diverse nature makes comparison of studies or pooling of data difficult. Studies are generally underpowered and have a potential risk of bias.
A single study of adequate quality reported no statistically significant difference between MUA (and home exercise) and home exercise alone in pain, function, range of motion or working ability at 6 weeks, as well as at 3 months,6 months and 12 months.34
Two studies comparing MUA with capsular distension had mixed findings. One found no significant difference between MUA and distension in pain or function at 16 weeks.35 The second study found a significantly greater improvement in pain, function and disability at 6 months with distension than with MUA.36
ACR is a relatively new intervention that is increasingly performed for treatment of frozen shoulder. The evidence to support this is limited, with only two case series of over 50 patients reported to date, which support the use of ACR. Further research with well designed prospective randomised clinical trials will be required to determine the true effectiveness of this intervention.
The two reported case series of 6637 and 1833,8 patients found significant improvement in mean external rotation from 3° to 39° and in mean abduction from 34° to 154°. There were also significant improvements in pain, function and disability postoperatively compared to the pre-operative status at mean follow-up of 10 months and 29 months.37,38
Open capsular release is rarely performed in contemporary practice for primary frozen shoulder. The evidence for this intervention is very poor.
There are currently no comparative studies involving arthroscopic capsular release. In the absence of a comparator, the true effectiveness of this intervention is yet to be established.
There is current lack of studies providing data on health-related quality of life specific to frozen shoulder populations. This information is required to enable assessments of cost-utility to be undertaken. The inclusion of preference based quality of life measures alongside clinical trials in frozen shoulder populations is a necessity. Cost-effectiveness analysis of any of the interventions for frozen shoulder is therefore not feasible with currently available evidence.
The NIHR-HTA commissioned United Kingdom Frozen Shoulder Trial (UKFROST) is a multicentre randomized trial comparing interventions for treatment of primary frozen shoulder that started recruitment in April 2015.39
Acknowledgements
Contributions from the BESS Working Group: Amar Rangan, Lorna Goodchild, Rohit Kulkarni, Andrew Carr, Jonathan Rees, Peter Brownson and Michael Thomas.
Contributions from the BOA Guidance Development Group: Rohit Kulkarni (Chair), Joe Dias, Jonathan Rees, Andrew Carr, Chris Deighton, Vipul Patel, Federico Moscogiuri, Jo Gibson, Clare Connor, Tim Holt, Chris Newsome, Mark Worthing and James Beyer.
Conflict of interest statement
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ 2005; 331: 1453–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Good Medical Practice. http://www.gmc-uk.org/guidance/good_medical_practice/duties_of_a_doctor.asp (accessed 25 June 2015).
- 3.Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998; 557: 649–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harkness EF, Macfarlane GJ, Nahit ES, Silman AJ, McBeth J. Mechanical and psychosocial factors predict new onsent shoulder pain: a prospective cohort study of newly employed workers. Occup Env Med 2003; 60: 850–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Windt D, Thomas E, Pope DP, et al. Occupational risk factors for shoulder pain: a systematic review. Occup Env Med 2000; 57: 433–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Linsell L, Dawson J, Zondervan K, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology 2006; 45: 215–21. [DOI] [PubMed] [Google Scholar]
- 7.Oh LS, Wolf BR, Hall MP, et al. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res 2007; 455: 52–63. [DOI] [PubMed] [Google Scholar]
- 8.van der Windt DA, Koes BW, Boeke AJ, Devillé W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 1996; 46: 519–23. [PMC free article] [PubMed] [Google Scholar]
- 9.Van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics and management. Ann Rheum Dis 1995; 54: 959–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Codman E. Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa, Malabar, FL: Krieger, 1965. [Google Scholar]
- 11.Schellingerhout JM, Verhagen AP, Thomas S, Koes BW. Lack of uniformity in diagnostic labeling of shoulder pain: time for a different approach. Man Therap 2008; 13: 478–83. [DOI] [PubMed] [Google Scholar]
- 12.Zuckerman J, Rokito A. Frozen shoulder: a consensus definition. J Shoulder Elbow Surg 2010; 20: 322–5. [DOI] [PubMed] [Google Scholar]
- 13.Hanchard N, Goodchild L, Thompson J, et al. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder, London: Chartered Society of Physiotherapy, 2011. [DOI] [PubMed] [Google Scholar]
- 14.Hand GCR, Athanasou NA, Matthews T, Carr AJ. The pathology of frozen shoulder. J Bone Joint Surg Br 2007; 89: 928–32. [DOI] [PubMed] [Google Scholar]
- 15.Hand C, Clipsham K, Rees JL, Carr AJ. Long term outcome of frozen shoulder. J Shoulder Elbow Surg 2008; 17: 231–6. [DOI] [PubMed] [Google Scholar]
- 16.Linsell L, Dawson J, Zondervan K, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology 2006; 45: 215–21. [DOI] [PubMed] [Google Scholar]
- 17.Maund E, Craig D, Sukerran S, et al. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess 2012; 16: 1–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dennis L, Brealey S, Rangan A, et al. Managing idiopathic frozen shoulder: a survey of health professionals’ current practice and research priorities. Shoulder Elbow 2010; 2: 294–300. [Google Scholar]
- 19.Rookmoneea M, Dennis L, Brealey S, et al. The effectiveness of interventions in the management of patients with primary frozen shoulder. J Bone Joint Surg Br 2010; 92: 1267–72. [DOI] [PubMed] [Google Scholar]
- 20.Carette S, Moffet H, Tardif J, et al. Intraarticular corticosteroids, supervised physiotherapy, or combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo controlled trial. Arthritis Rheum 2003; 48: 829–38. [DOI] [PubMed] [Google Scholar]
- 21.Ryans I, Montgomery A, Galway R, et al. A randomised controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology 2005; 44: 529–35. [DOI] [PubMed] [Google Scholar]
- 22.Dacre JE, Beeney N, Scott DL. Injections and physiotherapy for the painful stiff shoulder. Ann Rheum Dis 1989; 48: 322–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bal A, Eksioglu E, Gulec B, et al. Effectiveness of corticosteroid injection in adhesive capsulitis. Clin Rehabil 2008; 22: 503–12. [DOI] [PubMed] [Google Scholar]
- 24.Calis M, Demir H, Ulker S, et al. Is intra-articular sodium hyaluronate injection an alternative treatment in patients with adhesive capsulitis? Rheumatol Int 2006; 26: 536–40. [DOI] [PubMed] [Google Scholar]
- 25.Rovetta G, Monteforte P. Intra-articular injection of sodium hyaluronate plus steroid versus steroid in adhesive capsulitis. Int J Tissue React 1998; 20: 125–30. [PubMed] [Google Scholar]
- 26.Takagishi K, Saito A, Segawa K, et al. Evaluation of intra-articular injection in patients with so called Gojyukata: comparison of hyaluronate and steroid. Jpn J Med Pharm Sci 1996; 35: 377–81. [Google Scholar]
- 27.Dogru H, Basaran S, Sarpel T. Effectiveness of therapeutic ultrasound in adhesive capsulitis. Joint Bone Spine 2008; 75: 445–50. [DOI] [PubMed] [Google Scholar]
- 28.Yang J-I, Chang C-W, Chen S-Y, et al. Mobilisation techniques in subjects with frozen shoulder syndrome: randomised multiple treatment trial. Phys Ther 2007; 87: 1307–15. [DOI] [PubMed] [Google Scholar]
- 29.Leung MSF, Cheing GLY. Effects of deep and superficial heating in the management of frozen shoulder. J Rehabil Med 2008; 40: 145–50. [DOI] [PubMed] [Google Scholar]
- 30.Vermeulen HM, Rozing MP, Obermann WR, et al. Comparison of high grade and low grade mobilisation techniques in the management of adhesive capsulitis of the shoulder: a randomised controlled trial. Phys Ther 2006; 86: 355–68. [PubMed] [Google Scholar]
- 31.Tveita EK, Tariq R, Sesseng S, et al. Hydrodilatation, corticosteroids and adhesive capsulitis: a randomised controlled trial. BMC Musculoskelet Disord 2008; 9: 53–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buchbinder R, Green S, Forbes A, Hall S, Lawler G. Arthrographic joint distension with saline and steroid improves function and reduces pain in patients with painful stiff shoulder: results of a randomised, double blind, placebo controlled trial. Ann Rheum Dis 2004; 63: 302–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gam AN, Schydlowsky P, Rossel I, et al. Treatment of ‘frozen shoulder’ with distension and glucocorticoid compared with glucocorticoid alone: a randomised controlled trial. Scand J Rheumatol 1998; 27: 425–30. [DOI] [PubMed] [Google Scholar]
- 34.Kivimaki J, Pohjolainen T, Malmivaara A, et al. Manipulation under anaesthesia with home exercises versus home exercises alone in the treatment of frozen shoulder: a randomised controlled trial. J Shoulder Elbow Surg 2007; 16: 722–6. [DOI] [PubMed] [Google Scholar]
- 35.Jacobs LG, Smith MG, Khan SA, Smith K, Joshi M. Manipulation or intraarticular steroids in the management of adhesive capsulitis of the shoulder? J Shoulder Elbow Surg 2009; 18: 348–53. [DOI] [PubMed] [Google Scholar]
- 36.Quraishi NA, Johnston P, Bayer J, Crowe M, Chakrabarti AJ. Thawing the frozen shoulder, a randomised controlled trial comparing manipulation under anaesthesia with hydrodilatation. J Bone Joint Surg Br 2007; 89: 1197–200. [DOI] [PubMed] [Google Scholar]
- 37.Austgulen OK, Oyen J, Hegna J, Solheim E. Arthroscopic capsular release in treatment of primary frozen shoulder. Tidsskr Nor 2007; 127: 1356–8. [PubMed] [Google Scholar]
- 38.Chen S-K, Chien S-H, Fu Y-C, Huang P-J, Chou P-H. Idiopathic frozen shoulder treated by arthroscopic brisement. Kaohsiung J Med Sci 2002; 18: 289–94. [PubMed] [Google Scholar]
- 39.The United Kingdom Frozen Shoulder Trial (UKFROST). http://www.nets.nihr.ac.uk/projects/hta/132601 (accessed 25 June 2015).