Abstract
The scapula fulfils many roles to facilitate optimal function of the shoulder. Normal function of the shoulder joint requires a scapula that can be properly aligned in multiple planes of motion of the upper extremity. Scapular dyskinesis, meaning abnormal motion of the scapula during shoulder movement, is a clinical finding commonly encountered by shoulder surgeons. It is best considered an impairment of optimal shoulder function. As such, it may be the underlying cause or the accompanying result of many forms of shoulder pain and dysfunction. The present review looks at the causes and treatment options for this indicator of shoulder pathology and aims to provide an overview of the management of disorders of the scapula.
Keywords: Dyskinesis, instability, scapula
Introduction
Normal scapula function is essential for optimal shoulder function in all individuals and, in particular, the overhead throwing athlete. Scapula control and positioning allows for optimal positioning of the humerus in relation to the glenoid transferring power from the core to the distal upper extremity. Abnormalities of scapula function can be seen in many patients. It presents clinically as asymmetry in scapular motion compared to the contralateral side, either in elevation or descent, leading to a disrupted motion.
In a static sense, it may present as a prominence of the scapula or a resting position of protraction compared to the other side. Scapular dyskinesis can be defined as a collective term that refers to movement of the scapula that is dysfunctional and may create a possible impairment of overall shoulder function, although it may also represent the cause of persistent shoulder symptoms or may be the manifestation of underlying structural shoulder pathology in many types of shoulder injury.1 In this review, we explore contemporary concepts in the understanding and management of scapular dyskinesis from the surgeon’s perspective.
Anatomical concepts of the scapula
The scapula is attached to the axial skeleton via the clavicle through the acromioclavicular (AC) and sternoclavicular joints. It has muscular attachments to the posterior aspect of the ribcage via trapezius, rhomboids and serratus anterior. Core strength is transferred via the glenohumeral joint to the arm and hand by optimal coupling of the muscle activations and bony motion. The scapula has relatively limited bony attachments and is therefore dependent on mostly muscle activation for mobility and stability.
Normal movement of the scapula comprises components of three motions: (i) upward/downward rotation around a horizontal axis perpendicular to the plane of the scapula; (ii) internal/external rotation around a vertical axis through the plane of the scapula; and (iii) anterior/posterior tilt around a horizontal axis in the plane of the scapula. The clavicle acts as a strut for the shoulder complex, connecting the scapula to the axial skeleton. Normality of this linkage enables two translations: (i) upward/downward translation on the thoracic wall and (ii) retraction/protraction around the rounded thorax (Figure 1).2,3
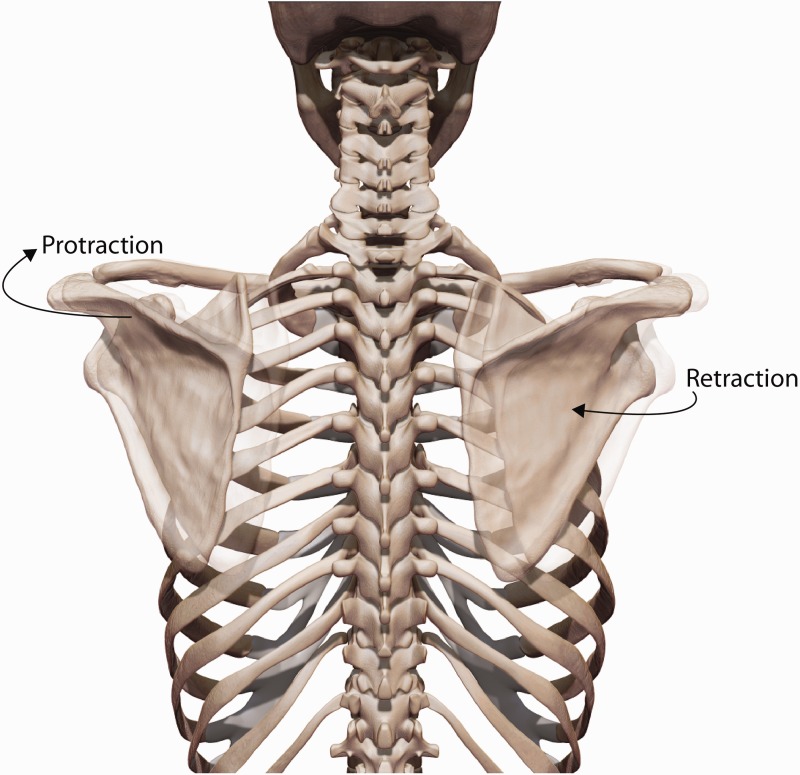
Figure 1.
Combined translational movements of the scapula in three planes lead to protraction and retraction around the thorax.
The coupling of scapular external rotation, posterior tilt, upward rotation and medial translation is called retraction. The coupling of internal rotation, angular tilt, downward rotation and lateral translation is called protraction. The coupling of upward translation, anterior tilt and internal rotation is seen as a shrug.1
The scapula fulfils important functions in dynamic and static modes. In addition to upward rotation, the scapula is required to tilt posteriorly and externally rotate to clear the acromion from the moving arm in elevation and abduction. In addition, the scapula must be able to internally/externally rotate in a synchronous manner to maintain the glenoid as a congruent socket for the arm in motion, thereby maximizing concavity compression and ball and socket kinematics. The scapula must be dynamically stabilized in a position of retraction during use of the arm to achieve maximal activation of all of the muscles that originate on the scapula.4,5
Another important role of the scapula in the normal shoulder is as a link in the proximal to distal sequencing of velocity, energy and forces of shoulder function. In most cases, sequencing begins at ground level and individual body segments are coordinated by muscle activation and body position to generate, summate and transfer forces through these segments to the terminal link. This sequence is termed the kinetic chain.6
The upper and lower trapezius muscles in addition to the serratus anterior muscles have been shown to be the greatest contributors to scapular stability and mobility (Figure 2).5,7 The trapezius and serratus anterior muscles initiate upward rotation and posterior tilt of the scapula. Activation of the lower trapezius muscle plays an important role in the stability of the arm in the overhead position and in descent of the arm from a position of maximum elevation. The rhomboids assist the trapezius in stabilizing the scapula contributing to control of medial and lateral scapular translation. Latissimus dorsi and pectoralis minor, which are both extrinsic shoulder girdle muscles, affect scapular motion in their role as prime movers of the arm. These muscles act mainly as force couples. The appropriate force couples for scapular stabilization include the upper and lower portions of the trapezius muscle working together with the rhomboid muscles, paired with the serratus anterior muscle (Figure 3).8 The appropriate force couples for acromial elevation are the lower trapezius and the serratus muscles working together paired with the upper trapezius and rhomboid muscles.6
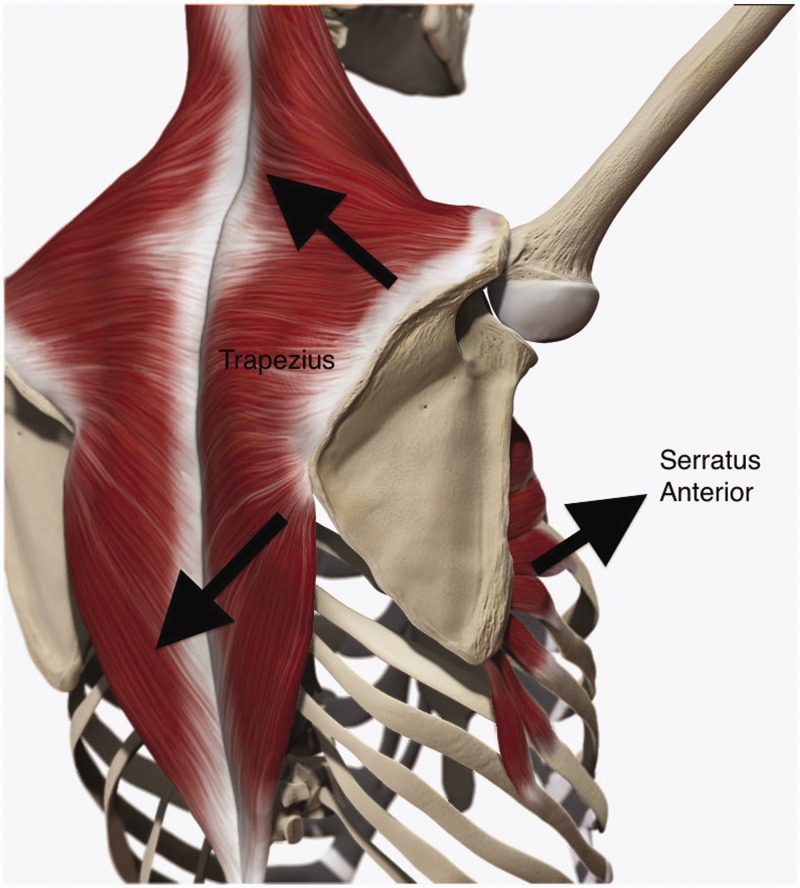
Figure 2.
Prime movers and stabilizers of the scapula: upper and lower trapezius with serratus anterior.
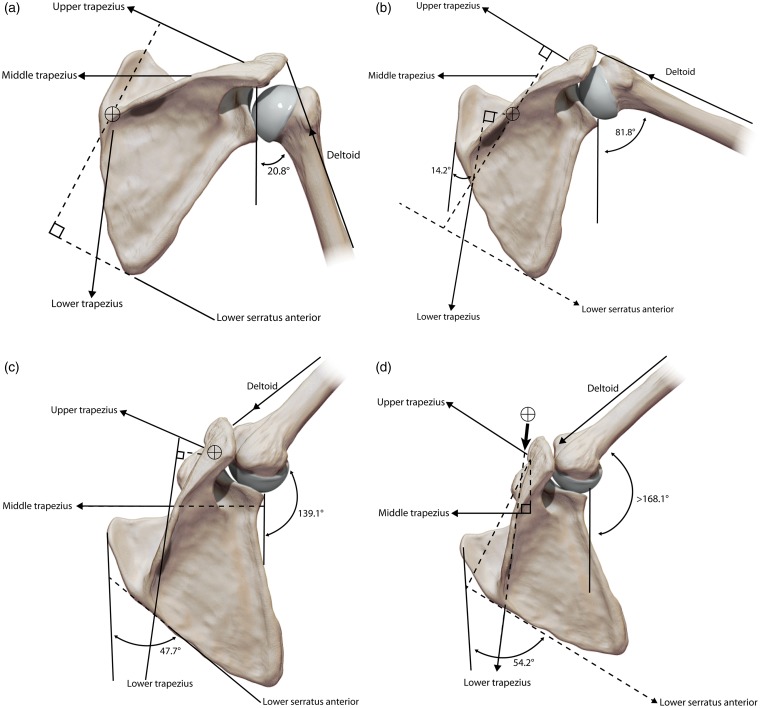
Figure 3.
Force couples for scapula motion: in early elevation (a, b), the upper and lower trapezius and serratus anterior muscles have long lever arms, being effective rotators and stabilizers. With higher arm elevation (c), the upper trapezius moment arm is shorter, whereas the lower trapezius and serratus anterior moment arms remain long, continuing to rotate the scapula. With maximum arm elevation (d), the lower trapezius maintains scapula position and the instant centre of rotation moves from the medial border of the spine to the acromioclavicular joint (adapted from Bagg SD, Forrest W).8.
Scapular dyskinesis
Scapular dyskinesis (alteration of motion) is a term that denotes loss of control of normal scapular motion, physiology or mechanics. Dyskinesis as opposed to dyskinesia is the more accurate terminology because the latter is applied to abnormal active movements mediated by neurological factors (e.g. tardive dyskinesia), whereas dyskinesis is more inclusive, incorporating many other factors that may be causative.1
Dyskinesis as a finding in the examination of the shoulder may be the result of an injury, although it may also not be related to any form of previous trauma. The clinical characteristics may include prominence of the medial or inferomedial scapular border, early scapular elevation or shrugging on arm elevation and/or rapid downward rotation on lowering of the arm.9 The efficacy of shoulder function is altered in many ways, with resulting changes in 3D glenohumeral angulation, AC joint strain, subacromial space dimensions, maximal muscle activation and optimal arm position and motion. This may result in augmentation of pre-existing symptoms related to concurrent shoulder pathology or produce new symptoms of pain/discomfort where none existed previously.
There are multiple causes of dyskinesis. Joint-related causes include high-grade AC arthrosis and instability and glenohumeral joint internal derangement. Bony causes include thoracic kyphosis, clavicular fracture non-union and clavicular malunion with shortening, rotation or angulation. Neurological causes include palsies of the long thoracic or spinal accessory nerves and cervical radiculopathy.
The commonest causative mechanisms of dyskinesis have a soft tissue components, involving either intrinsic muscle pathology or inflexibility or inhibition of normal muscle activation. Decreased flexibility of either the short head of biceps muscle or pectoralis minor have been shown to create anterior tilt and protraction of the scapula as a result of their pull on the coracoid.10
Periscapular muscle activation alterations may be seen in patients with dyskinesis. Strength and activation of serratus anterior are reduced in cases of impingement and shoulder pain. This can cause a loss of posterior tilt and upward rotation of the scapula leading to scapular dyskinesis.11
Regardless of the particular cause of dyskinesis, the final result in most cases is a protracted scapula either at rest or with the arm in motion. Protraction is not favourable for optimal shoulder function and results in decreased subacromial space with increased symptoms of impingement and increased extrinsic rotator cuff compression. Rotator cuff strength can also be decreased.4,5 Protraction can also lead to an increase in strain of the anterior glenohumeral ligaments and a greater risk of internal impingement.12
Scapular dyskinesis and specific shoulder injuries
Labral injury
Scapular dyskinesis has a high association with labral injury.13 The altered position and motion of internal rotation and anterior tilt changes GH alignment, placing increased tensile strain on the anterior ligaments, increasing ‘peel-back’ of the biceps/labral complex on the glenoid, and creating pathological internal impingement. These effects are magnified in the presence of glenohumeral internal rotation deficit, which creates increased protraction as a result of ‘wind-up’ of the tight posterior structures in follow-through. The demonstration of dyskinesis in patients with suspected labral injury provides a key component of rehabilitation protocols. Correction of the symptoms of pain found in the modified dynamic labral shear test14 can be frequently demonstrated by the addition of manual scapular retraction. This indicates the presence of dyskinesis as part of the pathophysiology and the need for scapular rehabilitation to improve scapular retraction, including mobilization of tight anterior muscles and institution of the scapular stability series of strengthening exercises.
Impingement
Impingement is frequently seen in throwing athletes. Most commonly in this group, impingement is secondary to other pathology such as instability, labral injury or biceps pathology. Scapular dyskinesis is associated with impingement by altering the scapular position at rest and upon dynamic motion. Scapular dyskinesis in impingement is characterized by loss of acromial upward rotation, excessive scapular internal rotation and excessive scapular anterior tilt.15,16 These positions create scapular protraction, which decreases the subacromial space and decreases demonstrated rotator cuff strength.4,17
Activation sequencing patterns and strength of the muscles that stabilize the scapula are altered in patients with impingement and scapular dyskinesis. Increased upper trapezius activity, imbalance of upper trapezius/lower trapezius activation, such that the lower trapezius activates later than normal, and decreased serratus anterior activation have been reported in patients with impingement.15 Increased upper trapezius activity is clinically observed as a shrug manoeuvre, resulting in a variation of the scapular dyskinesis pattern. This causes impingement as a result of a lack of acromial elevation. Frequently, lower trapezius activation is inhibited or delayed, creating impingement because of loss of acromial elevation and posterior tilt. Serratus anterior activation has been shown to be decreased in patients with impingement, creating a lack of scapular external rotation and elevation with arm elevation.
The pectoralis minor has been shown to be shortened in length in patients with impingement. This tight muscle creates a position of scapular protraction at rest and does not allow scapular posterior tilt or external rotation upon arm motion, predisposing patients to impingement symptoms.
Rotator cuff injury
The rotator cuff is frequently clinically involved in throwers with shoulder symptoms and symptoms can be exacerbated by dyskinesis. The dyskinetic position that results in an internally rotated and anteriorly tilted glenoid increases the internal impingement on the posterior superior glenoid with arm external rotation and increases the torsional twisting of the rotator cuff, which may create the undersurface rotator cuff injuries seen in throwers.12 In addition, positions of scapular protraction have been shown to be limiting to the development of maximal rotator cuff strength. Recent work in laboratory models of rotator cuff disease has shown that surgically induced scapular dyskinesis results in changes in cell morphology, gene expression and tendon characteristics that are similar to those seen in rotator cuff tendinopathy.18
AC joint injuries
AC joint injuries are rare in throwing athletes except American football quarterbacks, although they can create major functional deficits as a result of the disruption of the important AC linkage. Dyskinesis is found in a high percentage of patients with high-grade AC symptoms.19 AC separations lessen and high-grade AC separations remove the strut function of the clavicle on the scapula. Loss of the strut function permits the ‘third translation’ of the scapula, allowing it to move inferior and medial to the clavicle, changing the biomechanical screw axis of scapulohumeral rhythm, allowing excessive scapular internal rotation and protraction and decreased dynamic acromial elevation when the arm is elevated. Iatrogenic AC joint injury as a result of excessive distal clavicle resection and detachment of the AC ligaments shortens the bony strut and allows excessive scapular internal rotation as a result of excessive anterior/posterior motion at the AC joint. The protracted scapular position creates many of the dysfunctional problems associated with chronic AC separations, including impingement and decreased demonstrated rotator cuff strength. However, scapular and shoulder dysfunction can also occur in type II injuries if the AC ligaments are torn. This creates an anterior/posterior AC joint laxity and can be associated with symptoms of pain, clicking, decreased arm elevation and decreased shoulder function.
If dyskinesis is demonstrated on the clinical examination, then increased attention should be directed toward correcting the biomechanical abnormality rather than just placing the arm in a sling. Treatment should include not only CC ligament reconstruction, but also AC ligament reconstruction to completely restore the screw axis mechanism.
Clavicle fractures
Clavicle fractures may produce dyskinesis if the anatomy is not completely restored. The dyskinesis can be associated with alterations in shoulder function such as decreased strength and decreased arm motion in elevation.20 Shortened malunions or non-unions decrease the length of the strut, and alter the scapular position towards internal rotation and anterior tilt. In addition to changes in length, changes in clavicle curvature or rotation will affect scapular position or motion. Angulated fractures result in functional shortening and loss of rotation. The distal fragment in midshaft fractures often internally rotates, decreasing the obligatory clavicle posterior rotation and scapular posterior tilt during arm elevation. Dyskinesis can be a clinical sign of potentially harmful alteration of clavicle anatomy, and can provide information to clarify indications for operative treatment in these fractures.
Clinical examination of the scapula
Evaluation of the scapula should be carried out as a routine component of the shoulder examination. To detect scapular dyskinesis, clinical observation is used to determine whether winging of the inferior or medial borders of the scapula is present. Assessment for scapular prominence because of lift off from the thoracic wall is carried out in addition to detection of the lack of a smooth coordinated movement of the scapula during forward flexion, shrugging or arm lowering from a position of full flexion. The motion can then be characterized as dyskinesis as a ‘yes’ (presence of deviation or dysrhythmia/asymmetry bilaterally or ‘no’ (no presence). This scoring system has proven interobserver reliability and clinical utility.21,22
A number of clinical tests have been devised that employ dynamic corrective manoeuvres to assess the effect of correction of dyskinesis on shoulder symptoms. The scapular assistance test (SAT) and scapular retraction test (SRT) help evaluate the degree to which scapular dyskinesis, when corrected, may alter the patient’s symptoms. The SAT evaluates scapular contributions to impingement and rotator cuff strength whereas the SRT can be used for evaluation in cases of labral symptoms and rotator cuff strength.
To correctly carry out the SAT, assistance for scapular elevation is provided by manually stabilizing the scapula and rotating the inferior border of the scapula as the arm moves (Figure 4). This procedure simulates the force-couple activity of the serratus anterior and lower trapezius muscles.23 If symptoms of impingement are diminished or eliminated by this manoeuvre, then rehabilitation of the scapular stabilizing muscles is likely to help alleviate these symptoms.
Figure 4.
Scapula assistance test: the scapula is stabilized with one hand and the other hand ‘assists’ the scapula through its correct motion plane.
The SRT involves manually stabilizing the scapula in a retracted position on the thorax. This position confers a stable base of origin for the rotator cuff and often will improve tested rotator cuff strength. This test frequently demonstrates scapular and glenoid involvement in impingement lesions (Figures 5 and 6).23
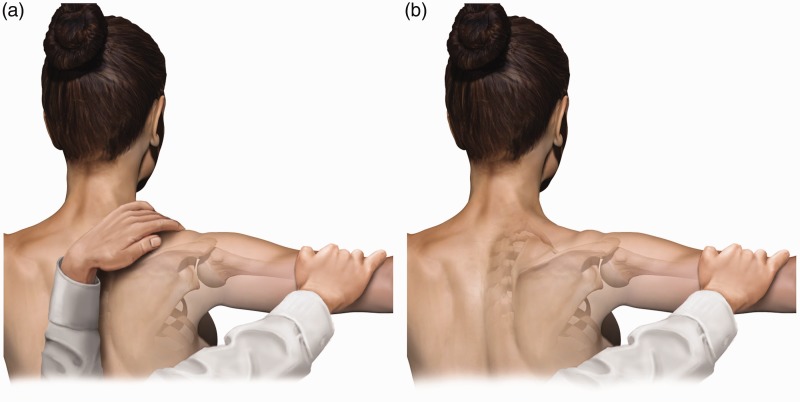
Figure 5.
Scapula retraction test: the examiner stabilizes the medial border of the scapula as the arm is elevated. Relief of impingement symptoms is a positive test.
Figure 6.
Scapula retraction test with resistance. (a) the examiner performs a traditional ‘empty can’ test. (b) The examiner stabilizes the medial border of the scapula and repeats the test. If the impingement symptoms are relieved, the test is positive.
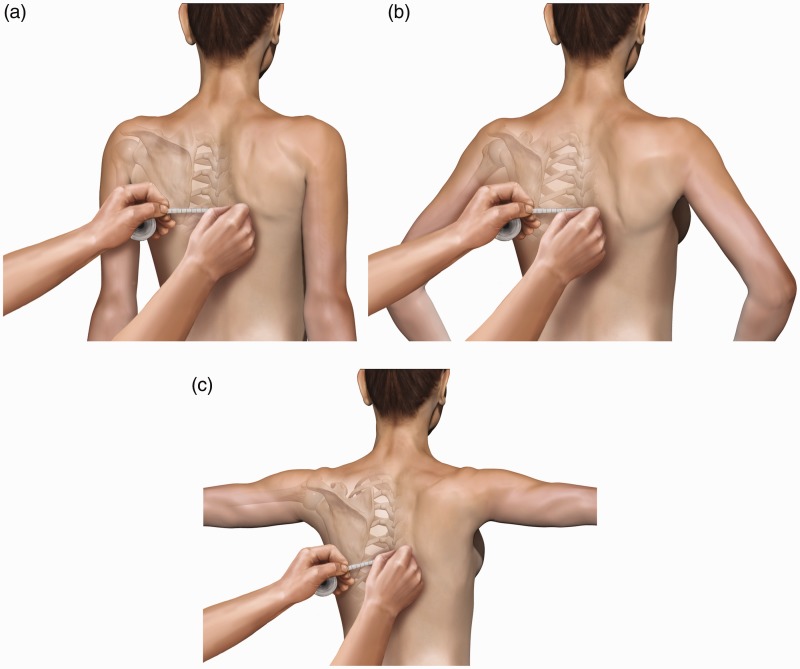
Quantitative assessment of scapular stabilizer strength can be achieved by the lateral scapular slide test (Figure 7).6 This test is semi-dynamic and evaluates three different positions of the scapula on injured and non-injured sides in relation to a fixed point on the spine as varying amounts of loads are put on the supporting musculature. These positions offer a graded challenge to the functioning of the shoulder muscles to stabilize the scapula. The first position is with the arms by the side. The inferomedial angle of the scapula is palpated and marked on both the injured and non-injured sides. The measurements from a fixed reference point are recorded. The second position is with the hands on the hips, the fingers anterior and the thumb posterior with approximately 10° of shoulder extension. The new position of the inferomedial border of the scapula is marked, and the reference point on the spine is maintained. The distances are calculated on both sides. A similar process is carried out for the third position. The arms are held at or below 90° of forward elevation with maximal internal rotation at the glenohumeral joint. The threshold of abnormality is 1.5 cm and significant asymmetry is most commonly measured in the third position.
Figure 7.
Lateral scapula slide test. (a) Initial position with arm at side. (b) Second position, arms on hips. (c) Third position with arms at 90° and internal rotation.
An essential part of scapula examination is evaluation of the shoulder pathology or injury that could be causative of or exacerbated by the concurrent presence of scapula dyskinesis. Rotator cuff integrity, labral stability and internal impingement should be sought because they may represent the underlying cause of the dyskinesis.
Investigation and treatment of scapular dyskinesis
Investigations should be directed toward confirming an underlying diagnosis. Nerve conduction studies may be of value if a specific traumatic precipitant causes injury to the long thoracic nerve, dorsal scapular nerve or spinal accessory nerve. Electromyography studies can help identify injury and the potential for recovery in periscapular muscles. X-rays can help identify clavicle or AC joint injury. Magnetic resonance imaging can help delineate muscle injury, whereas MR arthrograms can identify associated labral pathology.
The mainstay of treatment for the scapular dyskinesis is physical therapy to relieve the symptoms associated with inflexibility or trigger points and to re-establish muscle strength and activation patterns.6,23 Dyskinesis can often be caused by muscle inhibition created by soft tissue related pathology such as labral injury, internal impingement or rotator cuff pathology or hard tissue injury such as clavicle fractures and AC separations. In these instances, the surgical problem should be addressed prior to commencing physical therapy to correct the dyskinesis.
Rehabilitation for scapular dyskinesis should start proximally and end distally. The ultimate goal of physical therapy is to achieve the position of optimal scapular function (i.e. posterior tilt, external rotation and upward elevation). Core stability exercises can help improve 3D control of scapular motion and this is achieved through an integrated rehabilitation regimen in which the larger muscles of the lower extremity and trunk are utilized during the treatment of the scapula and shoulder. Scapular protraction and retraction are facilitated by hip and trunk flexion and extension exercises.
Once core stability has been established, a focus on the scapular controlling muscles can be initiated. The serratus anterior muscle acts as a powerful external rotator of the scapula, whereas the lower trapezius acts as a stabilizer of the acquired scapular position. Re-education of these muscles to act as dynamic stabilizers of the scapula is achieved by employing short lever, kinetic chain assisted exercises and finally long lever movements.2 This process may take at least 6 months and appropriate patient counselling to ensure realistic expectations is essential in the management of these cases. After achievement of adequate scapular control and retraction, other issues such as rotator cuff strength optimization or internal impingement can then be addressed. The sequence of rehabilitation exercises may need to be adapted for individual cases based on the rate of progress at each specific stage.
Future directions
Although scapular dyskinesis is a proven clinical entity that can be responsible for shoulder pathology in many cases, there are still a number of unanswered questions that require further clarification. Dyskinesis seen in association with rotator cuff tears was identified as a factor related to lower functional scores.25 It remains unclear whether scapular dyskinesis is a cause, effect or compensation for rotator cuff pathology.
Summary
Scapular dyskinesis is a relatively new concept in the assessment of shoulder pathology. It is likely to be a major contributor to shoulder pain, particularly in cases of recalcitrant shoulder pain and dysfunction. Increasing evidence shows that the condition is eminently treatable in the majority of cases and can improve with physiotherapy rehabilitation. It is advisable that this condition is recognized as a constituent of the routine shoulder examination for shoulder surgeons.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Kibler WB, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg 2012; 20: 364–372. [DOI] [PubMed] [Google Scholar]
- 2.Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med 2010; 44: 300–305. [DOI] [PubMed] [Google Scholar]
- 3.McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg 2001; 10: 269–277. 10.1067/mse.2001.112954. [DOI] [PubMed] [Google Scholar]
- 4.Kibler WB, Sciascia A, Dome D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med 2006; 34: 1643–1647. [DOI] [PubMed] [Google Scholar]
- 5.Smith J, Dietrich CT, Kotajarvi BR, Kaufman KR. The effect of scapular protraction on isometric shoulder rotation strength in normal subjects. J Shoulder Elbow Surg 2006; 15: 339–343. 10.1016/j.jse.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 6.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med 1998; 26: 325–337. [DOI] [PubMed] [Google Scholar]
- 7.Kibler WB, Chandler TJ, Shapiro R, Conuel M. Muscle activation in coupled scapulohumeral motions in the high performance tennis serve. Br J Sports Med 2007; 41: 745–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bagg SD and Forrest WJ. A biomechanical analysis of scapular rotation during arm abduction in the scapular plane. Am J Phys Med Rehabil 1988; 67: 238–45. [PubMed]
- 9.Kibler WB, Ludewig PM, McClure P, Uhl TL, Sciascia A. Scapular Summit 2009: introduction. July 16, 2009, Lexington, Kentucky. J Orthop Sports Phys Ther 2009; 39: A1–A13. [DOI] [PubMed] [Google Scholar]
- 10.Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther 2005; 35: 227–238. [DOI] [PubMed] [Google Scholar]
- 11.Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med 2007; 35: 1744–1751. [DOI] [PubMed] [Google Scholar]
- 12.Mihata T, McGarry MH, Kinoshita M, Lee TQ. Excessive glenohumeral horizontal abduction as occurs during the late cocking phase of the throwing motion can be critical for internal impingement. Am J Sports Med 2010; 38: 369–374. [DOI] [PubMed] [Google Scholar]
- 13.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med 2006; 34: 385–391. [DOI] [PubMed] [Google Scholar]
- 14.Kibler WB, Sciascia AD, Dome DC, Hester PW, Jacobs C. Clinical utility of new and traditional exam tests for biceps and superior glenoid labral injuries. Am J Sports Med 2009; 37: 1840–1847. [DOI] [PubMed] [Google Scholar]
- 15.Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. Journal of Orthopaedic and Sports Physical Therapy 2009; 39: 90–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kebaetse M, McClure PW, Pratt N. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil 1999; 80: 945–950. [DOI] [PubMed] [Google Scholar]
- 17.Tate AR, McClure P, Kareha S, Irwin D. Effect of the scapula reposition test on shoulder impingement symptoms and elevation strength in overhead athletes. J Orthop Sports Phys Ther 2008; 38: 4–11. [DOI] [PubMed] [Google Scholar]
- 18.Reuther KE, Thomas SJ, Tucker JJ, et al. Scapular dyskinesis is detrimental to shoulder tendon properties and joint mechanics in a rat model. J Orthop Res 2014; 32: 1436–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gumina S, Carbone S, Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy 2009; 25: 40–45. [DOI] [PubMed] [Google Scholar]
- 20.McKee MD, Pedersen EM, Jones C, et al. J Bone Joint Surg Am 2006; 88: 35–40. [DOI] [PubMed]
- 21.McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train 2009; 44: 160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uhl TL, Kibler WB, Gecewich B, Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy 2009; 25: 1240–1248. [DOI] [PubMed] [Google Scholar]
- 23.Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg 2003; 11: 142–151. [DOI] [PubMed] [Google Scholar]
- 24.Kuhn JE, Plancher KD, Hawkins RJ. Scapular winging. J Am Acad Orthop Surg 1995; 3: 319–325. [DOI] [PubMed] [Google Scholar]
- 25.Dunn W JG. Factors associated with low outcomes scores in patients with full thickness rotator cuff tears. American Academy of Orthopaedic Surgeons Annual Meeting. San Diego, CA, 2011.