Abstract
Background
Recurrent shoulder instability is usually caused by a traumatic event resulting in structural pathology, although a small subgroup of patients experience symptomatic recurrent shoulder instability without trauma. These patients are usually treated non-operatively but limited evidence exists regarding effective conservative management. In particular, there is a lack of reproducible exercise regimes and none that have been tested with condition-specific outcome measures.
Methods
A service evaluation was conducted over a 15-month period to assess our current treatment protocol used in the management of patients with atraumatic recurrent shoulder instability. The regime is reproducible with target-led progression milestones. Oxford Instability Shoulder Scores (OISS) and Western Ontario Shoulder Index (WOSI) scores were compared between baseline and final follow-up.
Results
Eighteen consecutive patients were included with mean follow-up of 4.5 months (range 1.35 months to 11.77 months). A statistically significant improvement was seen in both outcome measures. Mean OISS improved by 16.67 points (confidence interval: 12.34 to 20.99; p < 0.001). Mean WOSI improved by 36.76% (confidence interval: 28.46 to 45.06; p < 0.001).
Conclusions
For this small group of patients with recurrent atraumatic shoulder instability, the Derby Shoulder Instability Programme produced significant improvements over the short term, with a high level of patient compliance. This is the first study to include pathology-specific patient-reported outcome measures to assess outcomes from a specific and reproducible exercise regime in this group of patients. The findings support further research to evaluate the exercise protocol in a larger group of patients over the longer term.
Keywords: atraumatic, exercise, instability, rehabilitation, shoulder
Introduction
Instability is a common problem to affect the shoulder, particularly in young active individuals. The majority of shoulder dislocations occur as a result of trauma and may result in recurrent instability if the injury caused structural damage.1–4 In this group of patients, particularly when of young age and high activity levels, surgery is usually advised to repair the damaged structures.1,3 A small group of patients, however, suffer from recurrent shoulder instability in the absence of trauma. This scenario is more difficult to manage and usually surgery is not recommended.1,3,4 The mainstay of treatment is non-operative in the form of exercise-based physiotherapy to improve the muscle strength, proprioception and muscle balance around the shoulder girdle.
The atraumatic group of patients tend to present with either generalized joint hypermobility or localized shoulder hypermobility.1,3 The fact that the joint is excessively mobile does not mean it is always unstable, as demonstrated by the fact that many patients have unilateral symptoms. The Stanmore Classification3 can be used to classify shoulder instability and is a useful tool when selecting a treatment approach. Patients are broadly classified by proximity to the three poles of a triangle:
Type 1: traumatic with structural pathology
Type 2: atraumatic with structural pathology
Type 3: atraumatic with no structural pathology but abnormal muscle pattern
Further subclassifications can be made, such as Type 2(1) where there has been minor trauma resulting in a structural defect because patients’ characteristics may not relate exactly to the polar descriptions, although, generally, the recommended treatment regime is surgical for those closest to Type 1 and non-operative for those in the Type 2 or 3 categories. It is notable therefore that the evidence to support non-operative treatment is lacking. A systematic review performed in 2004 highlighted the limited and low quality evidence available.2 The recommendations were for future research using ‘well-defined conservative management protocols’ and using specific scales that measure the impact of shoulder instability, such as the Western Ontario Shoulder Index (WOSI).5 Unfortunately, subsequent to these recommendations, little additional research has been published. A further systematic review in 2014 drew similar conclusions.6 After a thorough literature search, only seven studies met the generous inclusion criteria that included studies with just 10 patients or more. The analysis found that the studies used outcome measures not sufficiently sensitive to detect changes in the shoulder instability patient population and that, overall, the evidence for exercise treatment for shoulder instability was of low quality. A specific concern was the lack of specific detail in relation to the exercises used because most studies only broadly classified the exercises in terms of rotator cuff strengthening or proprioception exercises rather than stating the exact exercise performed and the frequency/repetitions used. The exercise regimes are therefore not reproducible. The one exception is Burkhead & Rockwood’s regime from 1992,7 which employs simple strengthening techniques using elastic exercise bands and pulleys alongside a progressive push-up regime starting in standing, then progressing to an incline and finally horizontal. This regime was found to be beneficial, with 83% of patients achieving a ‘good or excellent result’, although the evaluation was based on the Modified Rowe Score, a very simple scoring system using just four variables. Only one variable measures stability with the responses being: no instability, instability with strenuous sports/work or instability with daily activity. A similar but less specific exercise regime was used by Misamore et al. with the same outcome measure and evaluated patients at 2-year follow-up.8 Out of 57 patients with atraumatic instability, 21 had undergone surgery and of the remaining 36 only 17 had a good or excellent result. This suggests that there may be short-comings with just a simple strengthening regime in the longer term.
More recent studies have considered the role of the sensorimotor system in controlling humeral head position, in particular joint proprioception and methods of retraining this.9–14 Exercises that involve plyometric training, the kinetic chain and also closed chain weight bearing exercises, especially when combined with uneven surfaces (e.g. balls or wobble boards), are considered to help restore shoulder proprioception and joint stability.
Materials and methods
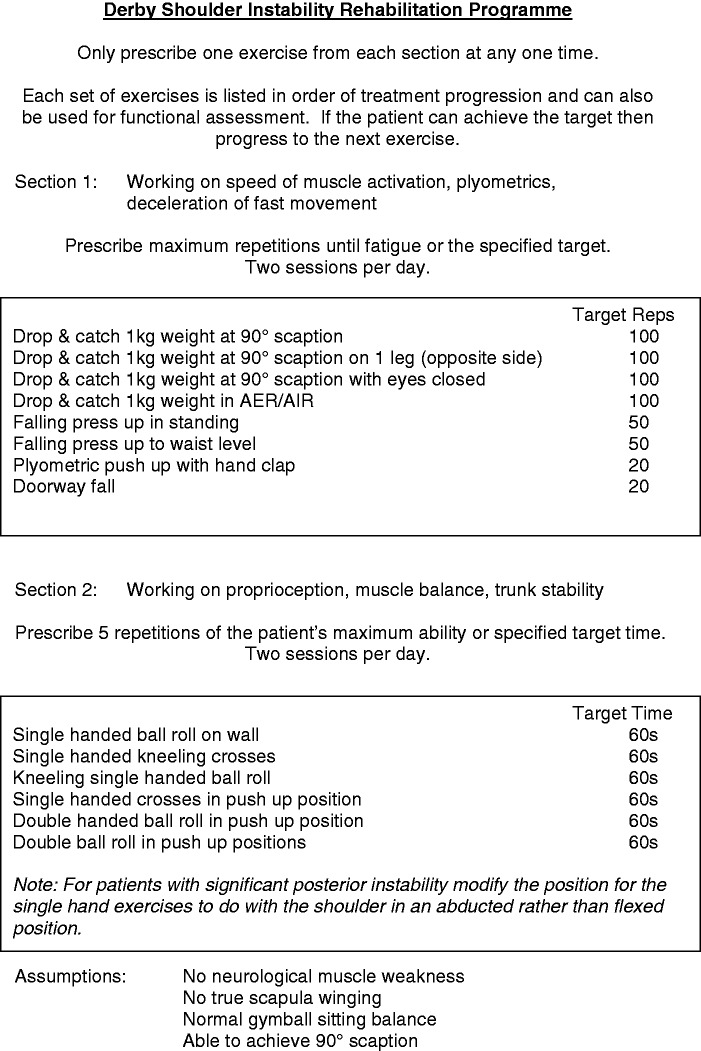
The Derby Shoulder Instability Programme was designed to incorporate all of the aformentioned aspects of strength, proprioception and plyometric training within a specific target driven exercise regime. Full details of the programme are provided in the online Supporting Information or at www.derbyshoulderunit.co.uk, although a summary is provided in Figure 1. Exercise progression is determined by the patient meeting defined targets for exercise repetitions or length of time exercising. This is re-assessed by the therapist at each follow-up appointment before the next exercise is taught. The length of time between appointments is variable and agreed between patient and therapist based on pragmatic expectations of the patient. The overall length of follow-up therefore varies between patients until an agreed time for discharge when the patient no longer reports symptoms and is confident to self-manage. This target-led approach has inherent measures of compliance because patients would be unlikely improve at the specific exercises without practice.
Figure 1.
Summary of the Derby Shoulder Instability Rehabilitation Programme.
A service evaluation was undertaken at Derby Hospitals NHS Foundation Trust to include patients treated in the adult and paediatric physiotherapy departments between August 2013 and November 2014. Only patients with a history of recurrent atraumatic shoulder instability were included. All patients were assessed clinically by experienced musculoskeletal physiotherapists and findings were correlated with imaging/arthroscopy. Those with a single episode and those with a traumatic onset were excluded. All patients were treated using the Derby Shoulder Instability Rehabilitation Programme assuming that they met the basic inclusion criteria detailed in the programme:
No clinical evidence of neurological muscle weakness compared to the contralateral side
No true scapula winging that would indicate a long thoracic nerve lesion (but assymmetrical patterning is accepted)
Able to maintain sitting balance on a gymball as a means of assessing basic trunk stability
Able to achieve 90° scaption as required to perform the exercises in section 1
At the initial physiotherapy assessment, if any of the criteria are not met, then the patient is first instructed on specific exercises to address the issues before commencing the programme. In this series, only one patient, when first assessed, was unable to achieve 90° scaption as a result of posterior subluxation of the humeral head. They were taught to activate the rotator cuff using lateral tension on an elastic exercise band at the same time as performing the movement and, after 2 weeks, were then able to perform the movement and begin the programme.
Patients completed baseline measures of shoulder pain, function and stability using the validated Oxford Instability Shoulder Score (OISS) [15] and the Western Ontario Shoulder Index (WOSI) at their first appointment.5 The OISS is scored from 12 to 60 points as originally described by Dawson et al., with 12 indicating a perfect score for a normal shoulder.15 The WOSI is presented as a percentage, with a higher score meaning a better level of function and stability. The OISS was completed at every appointment to chart progress and both scores were completed at discharge for comparison against baseline measures. The minimum clinically important difference is 4.5 points for the OISS16 and 10.4% for the WOSI.17
Statistical analysis was performed using STATA, version 12 (StataCorp, College Station, TX, USA). The results for OISS, Total WOSI score and WOSI physical sub-group followed a normal distribution and were analyzed using a paired t-test. The remaining WOSI sub-group results (‘sport, recreation, work’; ‘lifestyle’ and ‘emotions’) were not normally distributed and so these were analyzed using a Wilcoxon matched pairs, signed ranks test.
Ethics
Ethical approval was not required because this was a service evaluation of current treatment practice.
Results
Twenty patients commenced treatment but only 18 patients completed treatment during the evaluated time period. One patient began treatment but withdrew shortly afterwards, stating that they could not commit to the programme as a result of personal and psychological problems unrelated to the shoulder symptoms. This patient was classified with Type 3 instability with only mild baseline symptoms (WOSI 86.00% and OISS 21 points). A second patient relocated geographically, because of work, shortly after starting the programme, and so was lost to follow-up. The 18 patients who completed the programme had a mean age of 21.22 years (range 12 years to 49 years) and included seven males and 11 females. The majority of patients were in their teens or early 20 s but one notable outlier aged 49 years was included after a diagnostic arthroscopy confirming multidirectional instability and was also generally hypermobile as per the Beighton classification.18 Patients attended on average 6.28 sessions (range 3 to 14) over a mean of 4.5 months (range 1.35 months to 11.77 months). Patient demographics are presented in Table 1.
Table 1.
Patient demographics.
| Patient ID | Age | Sex | Length of symptoms (months) | Length of treatment (days) | Number of sessions | Stanmore grade | Direction of instability |
|---|---|---|---|---|---|---|---|
| 1 | 26 | M | 4 | 358 | 14 | 3 | MDI |
| 2 | 16 | F | 12 | 155 | 6 | 2 | Anterior |
| 3 | 33 | M | 12 | 82 | 4 | 3 | Anterior |
| 4 | 17 | M | 4 | 78 | 5 | 2 | Anterior |
| 5 | 19 | F | 12 | 132 | 3 | 3 | Anterior |
| 6 | 18 | M | 30 | 217 | 8 | 2 | MDI |
| 7 | 23 | F | 36 | 140 | 7 | 3 | MDI |
| 8 | 20 | F | 1 | 168 | 12 | 3 | Anterior |
| 9 | 12 | F | 6 | 41 | 3 | 3 | Anterior |
| 10 | 23 | F | 72 | 83 | 4 | 3 | Posterior |
| 11 | 17 | F | 6 | 91 | 4 | 3 | Anterior |
| 12 | 13 | F | 10 | 79 | 5 | 3 | Anterior |
| 13 | 17 | M | 4 | 150 | 4 | 3 | Anterior |
| 14 | 22 | M | 18 | 98 | 6 | 2 | Anterior |
| 15 | 49 | F | 22 | 230 | 12 | 2 | MDI |
| 16 | 17 | M | 10 | 77 | 5 | 3 | Anterior |
| 17 | 17 | F | 12 | 151 | 6 | 3 | Anterior |
| 18 | 23 | F | 48 | 116 | 5 | 3 | Anterior |
M, male; F, female; MDI, multidirectional shoulder instability.
Patients were broadly classified using the Stanmore Triangle Classification3 by proximity to each pole with five × Type 2 and 13 × Type 3. Structural pathology was assessed in six patients by magnetic resonance (MR) arthrogram and in five patients by diagnostic arthroscopy after MR arthrogram. There was a preference towards non-invasive assessment for children and so three patients had clinical assessment with plain X-ray and the four youngest patients had clinical assessment only. All seven were found to be hypermobile based on the Beighton classification18 and were assumed to have no structural pathology.
The mean improvement was 16.67 points in OISS [confidence interval (CI): 12.34 to 20.99; p < 0.001] and 36.76% in the WOSI (CI 28.46 to 45.06; p < 0.001). Both scoring systems showed statistically significant outcomes. Further sub-group analysis was performed related to Stanmore Classification and there were no differences in outcomes between Type 2 or Type 3.
The WOSI scores were also analyzed by the four component domains:
Physical symptoms
Sports, recreation and work
Lifestyle
Emotions
The results are summarized in Table 2 and show statistically significant improvements in all domains.
Table 2.
Pre- and post-treatment mean (95% confidence interval) OISS and WOSI Scores.
| Outcome measure | Pretreatment | Post-treatment | Significance |
|---|---|---|---|
| OISS | 37.06 points (32.73 to 41.39) | 20.39 points (17.98 to 22.80) | p < 0.001 |
| WOSI Total | 47.47% (38.47 to 56.46) | 84.23% (77.82 to 90.63) | p < 0.001 |
| WOSI Physical | 52.27% (43.51 to 61.05) | 85.61% (81.78 to 89.44) | p < 0.001 |
| WOSI Sport & Work | 35.13%* (IQR: 24.75 to 61.88) | 88.75%* (IQR: 81.94 to 96.63) | p = 0.0002 |
| WOSI Lifestyle | 50.50%* (IQR: 32.19 to 76.13) | 87.63%* (IQR: 83.75 to 95.44) | p = 0.0003 |
| WOSI Emotions | 30.83%* (IQR: 17.33 to 55.25) | 91.00%* (IQR: 81.75 to 96.52) | p = 0.0002 |
Median (interquartile range; IQR). OISS, Oxford Instability Shoulder Scores; WOSI, Western Ontario Shoulder Index.
Discussion
This is the first study to assess a standardized instability exercise regime using patient-reported outcome measures validated for use in the shoulder instability patient population. It is a regime that is reproducible because each individual exercise is fully described and a clear target-led progression pathway is laid out. It is notable that all 18 patients who completed the programme showed statistically significant improvement for all outcome measures (p = 0.001). Given the lack of published exercise regimes for treating recurrent shoulder instability, the Derby Shoulder Instability Rehabilitation Programme could be used as a starting point for physiotherapists inexperienced in treating this complex pathology. However, some patients may have such severe and complex instability that they are unable to meet the inclusion criteria for the programme and will need an individually tailored treatment regime.
The limitations of the present study include the small sample size, lack of a control group, short follow-up period and lack of cross-sectional imaging in seven patients that may have led to mis-classification in Stanmore grade. However, the overall diagnosis of atraumatic recurrent instability can be easily established based on the patient’s subjective history and clinical findings. A difference in Stanmore grades 2 and 3 does not change the course of treatment because non-operative treatment is recommended for both groups.1,3,4,6
Our recruitment rate of 18 patients in 15 months (=1.2 per month) was comparable to the results of Burkhead & Rockwood7 who recruited 66 patients over 48 months (= 1.375 per month). Burkhead & Rockwood also reported that the length of time for ‘maximum stability’ ranged from 6 weeks to 36 weeks, with a mean of 14 weeks. In our series, the treatment duration ranged from 6 weeks to 51 weeks, with a mean of 19.41 weeks. These factors highlight the difficulty in conducting a large-scale clinical trial for this group of patients because it is a rare presentation taking a long time to treat.
Our observations were that patients initially experienced a slight increase in shoulder pain or discomfort due to performing activities that were unusual for them. Typically, patients improved their ability to perform the exercises but most did not have a dramatic improvement in symptoms until they reached a certain threshold when there was a noticeable change in both pain and sensation of instability. However, this threshold was not consistent between patients. Only two patients needed to complete all components of the programme to feel that their shoulders were sufficiently stable. One was a high-level gymnast and the other was a black belt martial artist. The majority of patients with less demanding occupations or sports typically progressed as far as the falling press-up to waist level in section 1 and the double-handed ball roll in a push-up position in section 2.
The level of compliance was high. Apart from the patient who moved out of area and the patient who withdrew for personal reasons, the remaining 18 patients fully engaged with the programme. The subjective feedback was that performing just two exercises at any one time was acceptable to the patients and could be realistically achieved on a daily basis. We consider that, for this group of patients, exercises need to be repeated frequently and with high repetitions not only to improve strength and stamina, but also to relearn normal movement patterns. This is another novel aspect of the present study. By comparison, the Burkhead & Rockwood7 regime required the patient to perform just five repetitions of five exercises, two or three times a day. Although our target exercise repetitions were high, patients saw this as a motivational goal and the follow-up appointment times were chosen by the individual patients to allow themselves a realistic timescale in which to meet the required target and aid compliance.
Conclusions
The Derby Shoulder Instability Rehabilitation Programme can yield statistically significant results for patients with recurrent atraumatic shoulder instability (Stanmore Type 2 and Type 3) in the short term based on this small series. However, atraumatic recurrent shoulder instability is a condition that requires long-term management and so these results should be interpreted with caution. The regime is reproducible and achieved a high level of compliance amongst patients. Further research with this regime and method of using condition-specific patient-reported outcome measures is recommended. The results from the present study can be used to inform a further large-scale prospective trial to assess results over a longer time period.
Acknowledgement
The authors wish to acknowledge the contributions of Messrs David Clark, Tim Cresswell, Marius Espag and Amol Tambe in the initial diagnostic imaging and arthroscopic assessment of our patients.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Hayes K, Callanan M, Walton J, Paxinos A, Murrell GAC. Shoulder instability: management and rehabilitation. J Orthop Sports Phys Ther 2002; 32: 497–509. [DOI] [PubMed] [Google Scholar]
- 2.Gibson K, Growse A, Korda L, Wray E, MacDermid JC. The effectiveness of rehabilitation for nonoperative management of shoulder instability: a systematic review. J Hand Ther 2004; 17: 229–42. [DOI] [PubMed] [Google Scholar]
- 3.Lewis A, Kitamura T, Bayley JI. (ii) The classification of shoulder instability: new light through old windows!. Curr Orthop 2004; 18: 97–108. [Google Scholar]
- 4.Tibone JE, Bradley JP. The treatment of posterior subluxation in athletes. Clin Orthop Relat Res 1993; 291: 124–37. [PubMed] [Google Scholar]
- 5.Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med 1998; 26: 764–72. [DOI] [PubMed] [Google Scholar]
- 6.Warby SA, Pizzari T, Ford JJ, Hahne AJ, Watson L. The effect of exercise-based management for multidirectional instability of the glenohumeral joint: a systematic review. J Shoulder Elbow Surg 2014; 23: 128–42. [DOI] [PubMed] [Google Scholar]
- 7.Burkhead WZ, Rockwood CA. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am 1992; 74: 890–6. [PubMed] [Google Scholar]
- 8.Misamore GW, Sallay PI, Didelot W. A longitudinal study of patients with multidirectional instability of the shoulder with seven- to ten-year follow-up. J Shoulder Elbow Surg 2005; 14: 466–70. [DOI] [PubMed] [Google Scholar]
- 9.Kiss J, Damrel D, Mackie A, Neumann L, Wallace WA. Non-operative treatment of multidirectional shoulder instability. Int Orthop 2001; 24: 354–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright RW, Matava MJ. Treatment of multidirectional shoulder instability in the athlete. Oper Tech Sports Med 2002; 10: 33–9. [Google Scholar]
- 11.Naughton J, Adams R, Maher C. Upper-body wobbleboard training effects on the post-dislocation shoulder. Phys Ther Sport 2005; 6: 31–7. [Google Scholar]
- 12.Lephart SM, Jari R. The role of proprioception in shoulder instability. Oper Tech Sports Med 2002; 10: 2–4. [Google Scholar]
- 13.Myers JB, Wassinger CA, Lephart SM. Sensorimotor contribution to shoulder stability: effect of injury and rehabilitation. Man Ther 2006; 11: 197–201. [DOI] [PubMed] [Google Scholar]
- 14.Ide J, Maeda S, Yamaga M, Morisawa K, Takagi K. Shoulder-strengthening exercise with an orthosis for multidirectional shoulder instability: quantitative evaluation of rotational shoulder strength before and after the exercise program. J Shoulder Elbow Surg 2003; 12: 342–5. [DOI] [PubMed] [Google Scholar]
- 15.Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br 1999; 81: 420–6. [DOI] [PubMed] [Google Scholar]
- 16.Moser JS, Barker KL, Doll HA, Carr AJ. Comparison of two patient-based outcome measures for shoulder instability after nonoperative treatment. J Shoulder Elbow Surg 2008; 17: 886–92. [DOI] [PubMed] [Google Scholar]
- 17.Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy 2005; 21: 55–63. [DOI] [PubMed] [Google Scholar]
- 18.Beighton P, Horan F. Orthopaedic aspects of the Ehlers–Danlos syndrome. J Bone Joint Surg Br 1969; 51: 444–53. [PubMed] [Google Scholar]