Abstract
Background
Controversy presently exists surrounding the management of patients with subacromial impingement. This study aims to highlight current UK practices in the management of these patients.
Methods
BESS members were invited to complete a questionnaire and responses were received from 157 consultant shoulder surgeons.
Results
Physiotherapy is an integral part of management for 93% of surgeons with a minimum period of 12 weeks being most popular prior to consideration of arthroscopic subacromial decompression. Subacromial steroid injection is used by 95% and 86% repeat this if the patient has failed to respond to a previous injection by the general practioner. From initial presentation, 77% felt there should be at least 3 months of conservative management before proceeding to surgery. Good but transient response to subacromial injection was considered the best predictor of good surgical outcome by 77%. The coracoacromial ligament is fully released by 78%, although there was greater variation in how aggressive surgeons were with acromioplasty. Most (59%) do not include the nontender acromioclavicular joint to any extent in routine acromioplasty. Hospital physiotherapy protocols are used by 63% for postoperative rehabilitation.
Conclusions
Variation exists in the management regimes offered to patients with subacromial impingement, but most employ a minimum period of 12 weeks of conservative management incorporating physiotherapy and at least 2 subacromial steriod injections.
Keywords: Acromioplasty, arthroscopic decompression, subacromial impingement
Introduction
There has been recent controversy surrounding the management of patients with subacromial impingement syndrome. Previous studies1–5 and a Cochrane review6 have questioned the efficacy of arthroscopic subacromial decompression compared with conservative management in the form of a structured physiotherapy regime. Despite this, there has been a dramatic and consistent increase in the number of subacromial decompressions being performed in the National Health Service in England.7
The aim of this observational study was to demonstrate current practices in the management of patients with subacromial impingement within the UK.
Materials and Methods
A questionnaire was designed relating to the management of patients with subacromial impingement syndrome. A final version of this questionnaire was agreed upon with the British Elbow & Shoulder Society (BESS). The questionnaire was hosted by an online survey company (SurveyMonkey; https://www.surveymonkey.com). A web link to this survey was e-mailed to all UK-based consultant orthopaedic surgeons who were Members of BESS at that time (January 2014). Responders were directed to a web page containing the questionnaire and answers were archived by the survey host. A reminder e-mail was circulated 2 weeks later inviting anybody who had not yet completed the questionnaire to do so. Following a further 2-week period, the survey was closed.
Results
Completed questionnaires were received from 157 surgeons. Repliers were given the option to skip any of the questions; therefore, there were not 157 responses to each question.
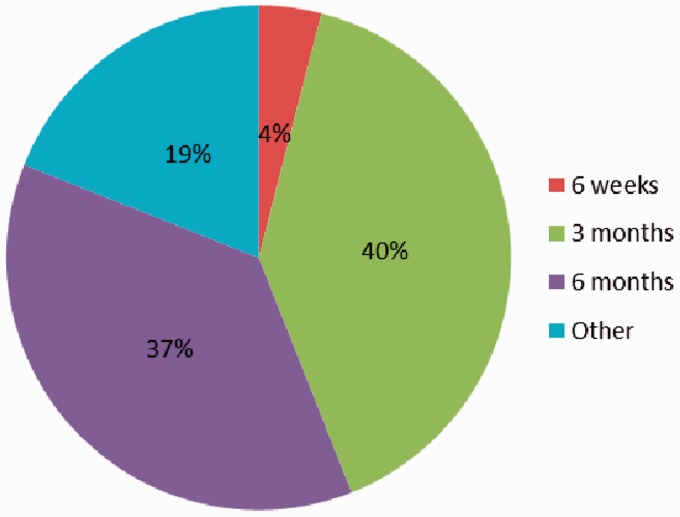
Of 155 responses, 127 (82%) felt that patients should have physiotherapy and an injection prior to referral to secondary care. In excess of 95% of surgeons utilize a minimum period of conservative management. Physiotherapy forms an integral part of 94% of responder’s conservative management, with 3 months being the most popular time period (Figure 1) of physiotherapy prior to considering surgery.
Figure 1.
Utilization of physiotherapy prior to surgery.
Subacromial steroid injection formed an integral part of conservative management for 97%, with 87% electing to repeat this if previously performed by the patients general practioner and found to be ineffective. There was significant variation in the number of injections performed before considering surgical intervention, although 83% would perform two or more injections, and many vary this depending of the length of benefit achieved. Multiple comments stated that injection should only be performed if there is no concern of rotator cuff tear.
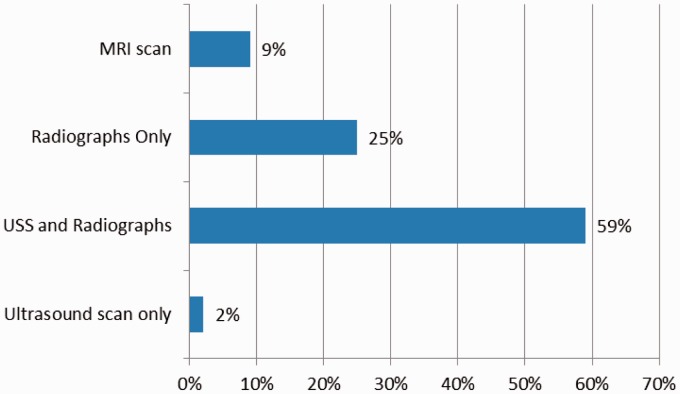
All responding surgeons perform routine investigation of the patients before proceeding to surgery (Figure 2). Ultrasound scan and radiographs in combination were most popular, followed by radiographs. Ultrasound scan only and magnetic resonance imaging were used less commonly, with the remainder of surgeons using variable combinations of these investigations depending on the clinical scenario.
Figure 2.
Pre-operative investigations.
A large number of surgeons (77%) consider a good but transient response to subacromial steroid injection to be an indicator of a patient who is likely to achieve a good result from subacromial decompression. A small number (6%) felt the presence of an acromial spur on X-ray was predictive of a good outcome, although no other single factor was considered by a significant number of surgeons (>2%) to be of any relevance.
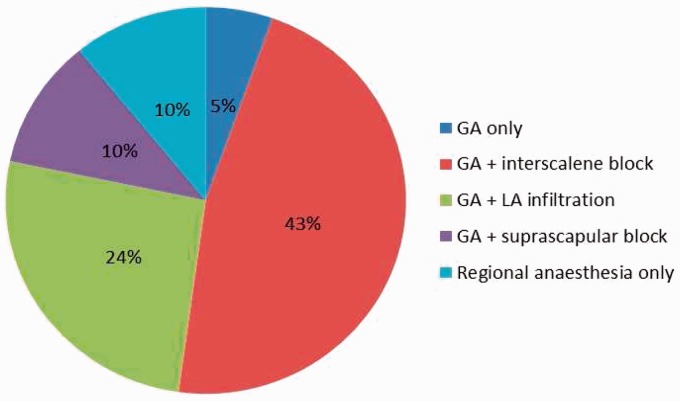
Subacromial decompression is performed routinely as day surgery by 94% of surgeons, 23-hour stay by 6% and as an inpatient in only one case. The most popular anaesthetic option is general anaesthetic with interscalene block (43%), followed by general anaesthetic with local anaesthetic infiltration. General anaesthetic with suprascapular nerve block, regional anaesthesia and general anaesthetic only were less popular options (Figure 3). The remaining 8% of surgeons vary their practice depending on the anaesthetist who they are working with.
Figure 3.
Anaesthetic type used to perform subacromial decompression.
The coracoacromial ligament is routinely fully released by 78% and partially released by 15%. The remaining 8% do not routinely perform any form of coracoacromial ligament release.
There was wider variation in the extent to which acromioplasty is routinely performed. The anterior hook/protuberance is removed by 33%, and a depth of bone 5 mm to 8 mm from the anterior half of the acromion is removed by 30%. The remaining third of responders varied from performing no bony resection to complete excision of all accessible acromion.
Variation also exists in whether or not the nontender acromioclavicular joint (ACJ) should be excised any degree. The majority (59%) do not routinely perform any degree of ACJ excision. Acromioplasty is performed up to the ACJ capsule by 22%, with co-planing of the inferior ACJ by 14% and a small number (4%) perform complete ACJ excision.
Postoperatively, the majority of surgeons (71%) provide patients with a sling. Most surgeons (63%) also utilize a hospital agreed physiotherapy regime.
Discussion
There is majority consensus on most aspects of the management of patients with subacromial impingement syndrome. Physiotherapy and subacromial injection form an integral part of the management in the practice of most UK surgeons. This is in keeping with the available published literature supporting the use of a combination of physiotherapy and injection as first-line therapy.8
Most who responded to our survey would agree that this conservative approach should continue for at least 12 weeks with two or more injections prior to consideration of subacromial decompression. There is, however, little supporting evidence detailing an optimum period of conservative management.9,10 Studies have suggested that very specific excercises are required for successful results with conservative management.1,3 Some responders are therefore justified in raising concerns regarding the availability of appropriate physiotherapy expertise in their practice. Another frequently occurring concern is over the ability of general practitioners to reliably locate the subacromial space when injections are performed in primary care, although accuracy when performed by surgeons ranges from 70% to 87% in the literature.11–13
All responding surgeons perform routine investigation before proceeding to surgery. For the majority, this involved plain radiographs, with approximately 60% performing ultrasound scans in addition. Multiple comments describe the use of ultrasound scanning performed by the surgeon in the outpatient clinic and this has proven to be a useful technique.14 Obviously, the availability of equipment and expertise to facilitate this will vary. Interestingly, few felt that the presence of an acromial spur on X-ray had any bearing on the efficacy of subacromial decompression. Around three-quarters felt that a good but transient response to subacromial injection was the only factor of relevance in predicting a positive outcome from surgery, which is supported by the study of Lim et al.15 It has been suggested in the literature, however, that the duration of symptoms prior to decompression is the most important factor in predicting outcome.16 Singh et al.17 recently proposed a new scoring system to predict those who would benefit from subacromial decompression with reported success; however, the usefulness of this scoring system is yet to be proven.
Almost all responding surgeons perform arthroscopic subacromial decompression routinely as a day surgery procedure. The most popular anaesthetic option is general anaesthesia with interscalene block, which is an established technique with good results.18–20 This is clearly also subject to the preferences of the anaesthetist and the patient, although one surgeon commented that the expertise required to perform an interscalene block was not available to them. In such a situation, an alternative is intra-operative infiltration of long-acting local anaesthetic into the subacromial bursa, which was shown to be equally effective by Nisar et al.21
With the exception of coracoacromial ligament release, which is routinely performed by most surgeons, surgical aspects of management were variable. The degree to which acromioplasty was performed ranges widely from no bony resection to removal of all accessible acromion. Two surgeons stated that they no longer perform routine acromioplasty subsequent to the report by Henkus et al.22 suggesting that there is no statistical difference in the results between acromioplasty and bursectomy without any bony resection. Similarly, a narrow majority of surgeons opt not to perform any excision of the nontender ACJ, whereas a significant minority perform a variable degree of ACJ excision.
Most surgeons provide patients with a supportive sling postoperatively and most patients are rehabilitated in line with a hospital agreed physiotherapy protocol.
Conclusions
Currently, variation exists in the management regimes offered to patients with subacromial impingement syndrome in the UK. The majority of shoulder surgeons responding to our questionnaire utilize a minimum period of 12 weeks of conservative management involving physiotherapy and at least two subacromial injections. When necessary, most agree that arthroscopic subacromial decompression should include full release of the coracoacromial ligament and that postoperative rehabilitation should follow a hospital agreed physiotherapy regime. Further work is required to determine whether or not ACJ excision should be routinely performed during subacromial decompression.
Declaration of conflicting interests
None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Haahr JP, Ostergaard S, Dalsgaard J, et al. Exercises versus arthroscopic decompression in patients with subacromial impingement: a randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis 2005; 64: 760–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohadi N. Exercises or arthroscopic decompression for subacromial impingement? Clin J Sport Med 2006; 16: 193–4. [DOI] [PubMed] [Google Scholar]
- 3.Brox JI, Gjengedal E, Uppheim G, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome); a prospective, randomized, controlled study in 125 patients with a 2½ year follow-up. J Shoulder Elbow Surg 1999; 8: 102–11. [DOI] [PubMed] [Google Scholar]
- 4.Nutton RW, McBirnie JM, Phillips C. Treatment of chronic rotator cuff impingment by arthroscopic subacromial decompression. J Bone Joint Surg [Br] 1997; 79B: 73–6. [DOI] [PubMed] [Google Scholar]
- 5.Morrison DS, Frogameni AD, Woodworth P. Non-operative treatment of subacromial impingment syndrome. J Bone Join Surg [Am] 1997; 79A: 732–7. [DOI] [PubMed] [Google Scholar]
- 6.Coghlan JA, Buchbinder R, Green S, et al. Surgery for rotator cuff disease. Cochrane Database Syst Rev 2008; 1: CD005619–CD005619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murphy RJ, Maxwell R, Kulkarni R, et al. Rates of arthroscopic subacromial decompression and rotator cuff repair surgery in the NHS in England from 2000 to 2010 [abstract]. In Procs Bess Congress, 2011.
- 8.Johansson K, Oberg B, Adolfsson L, Foldevi M. A combination of systematic review and clinicians’ beliefs in interventions for subacromial pain. Br J Gen Pract 2002; 52: 145–52. [PMC free article] [PubMed] [Google Scholar]
- 9.Gebremariam L, Hay EM, van der Sande R, et al. Subacromial impingement syndrome – effectiveness of physiotherapy and manual therapy. Br J Sports Med 2014; 48: 1202–8. [DOI] [PubMed] [Google Scholar]
- 10.Hanratty CE, McVeigh JG, Kerr DP, et al. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin Arthritis Rheum 2012; 42: 297–316. [DOI] [PubMed] [Google Scholar]
- 11.Henkus HE, Lodewijck PJ, Cobben MD, et al. The accuracy of subacromial injections: a prospective randomized magnetic resonance imaging study. J Arthroscopic Rel Surg 2006; 22: 277–82. [DOI] [PubMed] [Google Scholar]
- 12.Esenyel CZ, Esenyel M, Yesiltepe R, et al. The correlation between the accuracy of steroid injection and subsequent shoulder pain and function in subacromial impingement syndrome. Acta Orthop Traumatol Turc 2003; 37: 41–5. [PubMed] [Google Scholar]
- 13.Kang MN, Rizio L, Prybicien M, Middlemas DA, Blacksin MF. The accuracy of subacromial corticosteroid injections: a comparison of multiple methods. J Shoulder Elbow Surg 2008; 17.1: S61–66. [DOI] [PubMed] [Google Scholar]
- 14.Cholewinski JJ, Kusz DJ, Wojciechowski P, Cielinski LS, Zoladz MP. Ultrasound measurement of rotator cuff thickness and acromio-humeral distance in the diagnosis of subacromial impingement syndrome of the shoulder. Knee Surg Sports Traumatol Arthrosc 2008; 16: 408–14. [DOI] [PubMed] [Google Scholar]
- 15.Lim JT, Acornley A, Dodenhoff RM. Recovery after arthroscopic subacromial decompression: prognostic value of the subacromial injection test. Arthroscopy 2005; 21: 680–3. [DOI] [PubMed] [Google Scholar]
- 16.Patel VR, Singh D, Calvert PT, Bayley JI. Arthroscopic subacromial decompression: results and factors affecting outcome. J Shoulder Elbow Surg 1999; 8: 231–7. [DOI] [PubMed] [Google Scholar]
- 17.Singh HP, Mehta SS, Pandey R. A preoperative scoring system to select patients for arthroscopic subacromial decompression. J Shoulder Elbow Surg 2014; 23: 1251–6. [DOI] [PubMed] [Google Scholar]
- 18.Al-Kaisy A, McGuire G, Chan VW, et al. Analgesic effect of interscalene block using low-dose bupivacaine for outpatient arthroscopic shoulder surgery. Reg Anesth Pain Med 1998; 23: 469–73. [PubMed] [Google Scholar]
- 19.Krone SC, Chan VW, Regan J, et al. Analgesic effects of low dose ropivacaine for interscalene brachial plexus block for outpatient shoulder surgery – a dose finding study. Reg Anesth Pain Med 2001; 26: 439–43. [DOI] [PubMed] [Google Scholar]
- 20.Laurila PA, Lopponen A, Kangas-Saarela T, Flinkkila T, Salomaki TE. Interscalene brachial plexus block is superior to subacromial bursa block after arthroscopic shoulder surgery. Acta Anaesthesiol Scand 2002; 46: 1031–6. [DOI] [PubMed] [Google Scholar]
- 21.Nisar Aamer, Morris MW, Freeman JV, Cort JM, Rayner PR, Shahane SA. Subacromial bursa block is an effective alternative to interscalene block for postoperative pain control after arthroscopic subacromial decompression: a randomized trial. J Shoulder Elbow Surg 2008; 17: 78–84. [DOI] [PubMed] [Google Scholar]
- 22.Henkus HE, de Witte PB, Nelissen RG, et al. Bursectomy compared with acromioplasty in the management of subacromial impingement syndrome: a prospective randomised study. J Bone Joint Surg [Br] 2009; 91: 504–10. [DOI] [PubMed] [Google Scholar]