Introduction
Definition
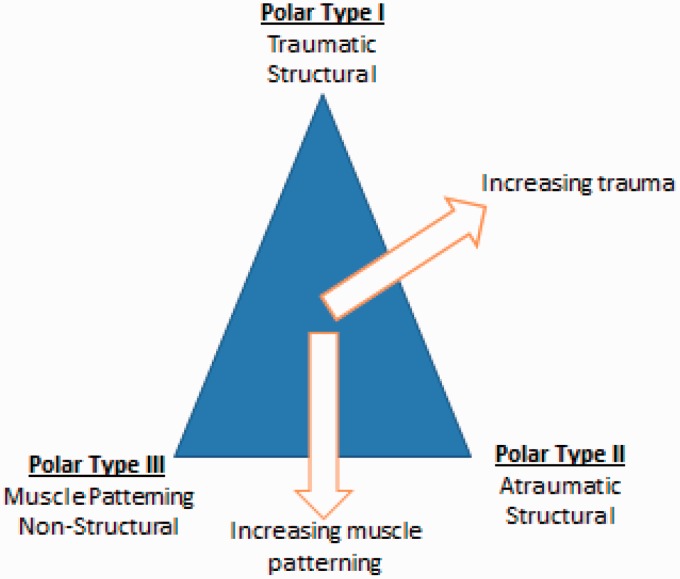
Anterior traumatic shoulder instability can be defined as excessive anterior translation of the humeral head on the glenoid fossa caused primarily by a traumatic event. This results in symptoms including pain, discomfort, subluxation or dislocation. This has also been referred to as Type 1 instability (Figure 1) on the Stanmore triangle of instability.1
Figure 1.
Stanmore classification of shoulder instability.
Shared decision-making
The General Medical Council’s ‘Good Medical Practice guide2 clearly states in the section on working in partnership with patients that doctors should:
Listen to patients and respond to their concerns and preferences.
Give patients the information they want or need in a way they can understand.
Respect patients’ right to reach decisions with the doctor about their treatment and care.
Support patients in caring for themselves to improve and maintain their health.
This can only be achieved by direct consultation between the patient and their treating clinician. Decisions about treatment taken without such direct consultation between patient and treating clinician are not appropriate, as they do not adhere to principles of good medical practice.
Continuity of care
Continuity and co-ordination of care are essential parts of the GMC’s Good Medical Practice guidance.2 It is therefore inappropriate for a clinician to treat a patient if there is no clear commitment from that clinician or the healthcare provider to oversee the complete care pathway of that patient including their diagnosis, treatment, follow-up and adverse event management.
Background
Historically, 96% of shoulder dislocations have been attributed to a traumatic episode with anterior dislocation accounting for 97% of these.3
Traumatic dislocation of the glenohumeral joint is the most common joint dislocation with an incidence of 8.2 to 23.9 per 100,000 per year.3–5 The male to female ratio is 2.55: 1 with almost 50% occurring in patients between the age of 15 years and 29 years.5 A second peak in incidence is seen in elderly females over the age of 80 years.
The glenohumeral joint has both static and dynamic factors that contribute to stability. The static factors include the conformity of the articular surfaces, the glenoid labrum and the glenohumeral ligaments.6 Concavity-compression,7 scapular rotators, proprioception, the rotator cuff and the long head of biceps comprise the dynamic stabilizers.
- Anterior dislocation most commonly occurs following a fall onto an outstretched hand.
- ○ The patient falls forward, elevating their arms to protect their fall
- ○ This causes the arm to extend (or abduct) and externally rotate placing the inferior glenohumeral ligament at maximal tension and resultant failure
- ○ Other mechanisms of injury can happen but are less common
- Patterns of pathological lesions.
- ○ Bankart lesion8 – avulsion injury of the labrum
- ○ Inferior capsular injury
- ○ anterior labral periosteal sleeve avulsion (ALPSA)
- ○ Humeral avulsion of the glenohumeral ligament (HAGL)
- ○ Glenoid rim fracture
- ○ Chronic glenoid defect
- ○ Hill–Sachs lesion (compression fracture of postero-supero-lateral humeral head)
Patients may present with a mixed (i.e. nonpolar type of instability). In such cases, there may be associated pathological lesions eg. Posterior labral tears and superior labral anterior posterior (SLAP) tears. Such lesions require additional treatment, which should be addressed separately, and are beyond the scope of this care pathway.
Associated injuries
- Neurological injury.
- ○ Clinically apparent neurological injury occurs in approximately 13.5% of dislocations with axillary nerve injury accounting for two thirds of these9
- ○ Electromyography at the time of injury, however, demonstrates a much higher incidence of nerve injury of 48%.10 The age of the patient (1.3 times greater risk per 10 years) and presence of haematoma (4.4 times greater risk) are risk factors for neurological injury
- Greater tuberosity fracture.
- ○ Present in approximately 16% of anterior traumatic dislocations9 with over 50% reducing to a satisfactory position following shoulder relocation
- Rotator cuff tear.
- ○ Radiologically proven rotator cuff tears following anterior glenohumeral dislocation are common with an increasing incidence seen with increasing age.11–13 In one study, rotator cuff tears were identified in 41% aged 40 years to 55 years, 71% aged 56 years to 70 years and 100% aged over 70 years11
- ○ However, it is difficult to predict the incidence of clinically relevant rotator cuff tears following anterior glenohumeral dislocation due to the increasing incidence of asymptomatic cuff tears with age. Clinically relevant cuff tears (i.e. patients with weakness and consequently investigated) are present in approximately one in 10 patients with a mean age of 69 years9
Natural history and recurrence
The decision to treat isolated traumatic anterior glenohumeral dislocation will depend on the likelihood of recurrent dislocations and the risk of undesirable sequelae such as post traumatic osteoarthritis.
The risk of recurrent dislocation is inversely proportional with the age of the patient at the time of dislocation.14 Therefore the younger the patient, the more likely the recurrence of dislocation (Table 1).
Almost 90% of recurrent dislocations occur within 2 years of primary dislocation.15
Males under the age of 20 years have approximately 72% chance of recurrent instability.15
Table 1.
Age- and sex-specific estimated probability of recurrent instability within the first 2 years after primary glenohumeral dislocation (extracted from Robinson et al.15).
| Age (years) | Males | Females |
|---|---|---|
| 15 | 0.86 | 0.54 |
| 16 | 0.84 | 0.51 |
| 17 | 0.81 | 0.48 |
| 18 | 0.78 | 0.45 |
| 19 | 0.75 | 0.42 |
| 20 | 0.72 | 0.40 |
| 21 | 0.69 | 0.37 |
| 22 | 0.66 | 0.34 |
| 23 | 0.62 | 0.32 |
| 24 | 0.59 | 0.30 |
| 25 | 0.56 | 0.28 |
| 26 | 0.53 | 0.26 |
| 27 | 0.50 | 0.24 |
| 28 | 0.47 | 0.22 |
| 29 | 0.43 | 0.20 |
| 30 | 0.41 | 0.19 |
| 31 | 0.39 | 0.17 |
| 32 | 0.36 | 0.16 |
| 33 | 0.34 | 0.15 |
| 34 | 0.31 | 0.14 |
| 35 | 0.29 | 0.13 |
Aims of treatment
Acute setting
The overall treatment aim for traumatic anterior shoulder instability in the acute setting is to identify the dislocation and any associated injuries and to reduce the dislocation in an appropriate environment minimizing additional trauma.
Non-acute setting
The treatment aim in the non-acute setting is to minimize the risk of recurrence and ‘improve pain and function’. Treatment success needs to be defined individually with patients in a shared decision-making process. The degree of improvement and level of acceptance to a patient will depend on recurring symptoms of instability, patient demographics, personal circumstances and patient expectations.
Pre-hospital care
Almost all traumatic anterior shoulder instability will occur out of hospital. It is not advisable for patients or bystanders to attempt to reduce the dislocation unless medically trained to do so. The risk of unidentified associated injuries is not insignificant and so transfer to hospital for clinical assessment and radiological investigations should be organized. Reduction of the dislocation can then be performed in a controlled environment.
Primary care/fracture clinic/community triage services
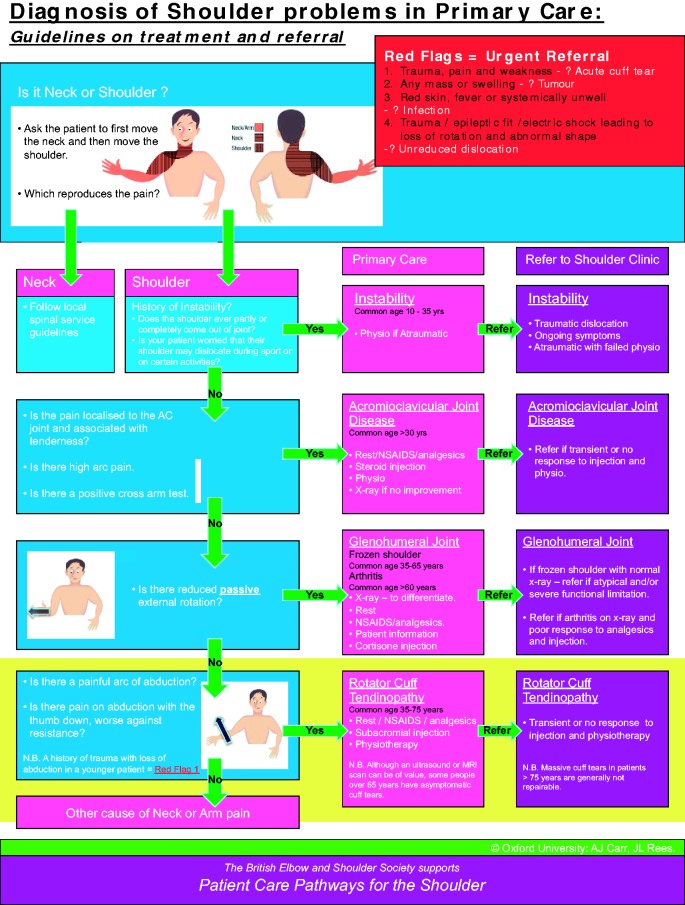
Diagnosis is based on history and examination (Fig. 2).
Making the correct diagnosis is very important and will ensure an efficient and optimum treatment experience for the patient. Primary care doctors can work through the algorithm below.
The algorithm below emphasizes the importance of history in the diagnosis of traumatic anterior shoulder instability.
- Features of importance are:
- ○ Patient expectation
- ○ Hand dominance
- ○ Occupation and level of activity or sports
- ○ Age at primary dislocation
- ○ Sex of patient
- ○ Symptoms of on-going instability
- ○ Number of dislocations
- ○ Systemic illnesses and comorbidities
- ○ Red Flags (Fig. 3)
Figure 2.
Diagnosis of shoulder problems in primary care. Guidelines on treatment and referral.
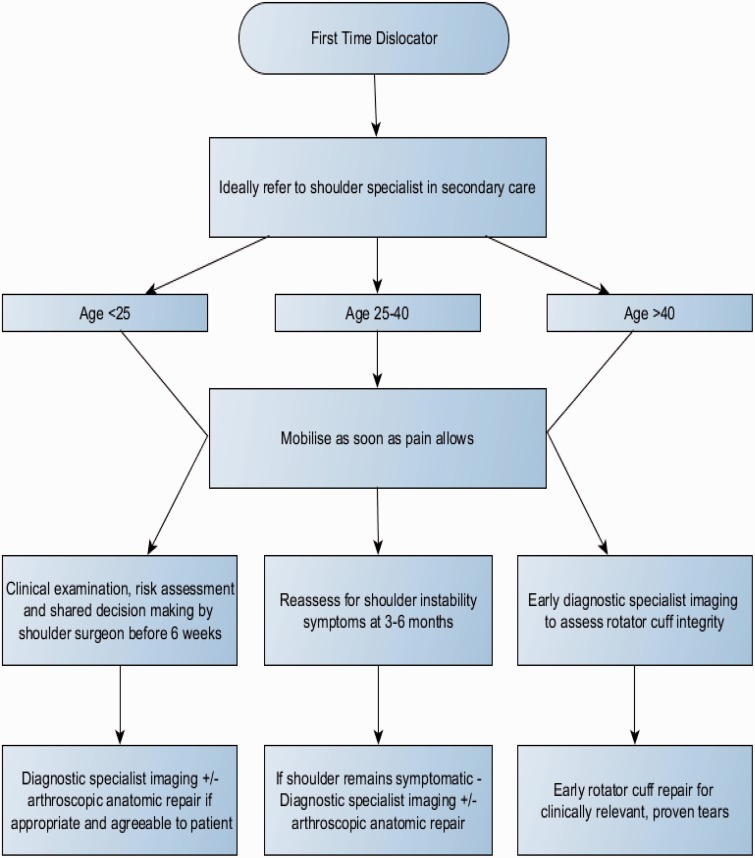
Figure 3.
Proposed algorithm for management of uncomplicated primary traumatic anterior instability.
Red flags for the shoulder
Acute severe shoulder pain needs proper and competent diagnosis. Any shoulder ‘Red Flags’ identified during primary care assessment need urgent secondary care referral.
A suspected infected joint needs same day emergency referral.
An unreduced dislocation needs same day emergency referral.
Suspected tumour and malignancy will need urgent referral following the local 2-week cancer referral pathway.
An acute rotator cuff tear as a result of a traumatic event needs urgent referral and ideally should be seen in the next available specialist shoulder clinic.
It should be noted that 40% of patients over the age of 40 years suffering from a traumatic anterior glenohumeral dislocation will have a rotator cuff tear.13,14 Although not all of these will be clinically relevant, a careful examination of the rotator cuff strength should be performed and urgent referral sought if doubt remains regarding cuff integrity. The presence of infraspinatus weakness may indicate a large acute tear.
Treatment in primary care/community triage services
Adopt shared decision-making and define treatment goals, taking into account personal circumstances.
Most patients will be managed following an acute anterior dislocation through the fracture clinic in secondary care. However, this is not always the case.
Conservative treatment following dislocation should focus on early mobilization. The risk of recurrence is not reduced with prolonged immobilization of greater than 1 week.14,16
Failure of these community treatments will prompt secondary care referral.
Physiotherapy rehabilitation is usually for 4 weeks to 12 weeks depending on patient response unless patients are unable to tolerate the exercises, or physiotherapists identify a reason for earlier referral to secondary care.
Treatment timelines should include primary care and intermediate care time. Intermediate care should not delay appropriate referral to secondary care.
Although shoulder X-rays with two views in primary care can be useful in patients not improving with conservative treatment, specialist imaging of the shoulder with magnetic resonance imaging with arthrography (MRA) or computed tomography with arthrography (CTA) is rarely indicated in primary care.
Secondary care
Acute dislocation: initial assessment and reduction
It is essential, for clinical and medico-legal reasons, that a detailed and documented neurological (and circulatory) examination is performed prior to shoulder relocation.
Two views are required to confirm glenohumeral dislocation and the direction of dislocation. An anteroposterior radiograph is obligatory. Ideally, an axial view should also be obtained as the second view. If pain precludes this view, then a modified axial (Wallace)17 or lateral scapular view are acceptable alternatives.
- Numerous reduction techniques have been described. The principles of safe reduction are:
- ○ Consent
- ○ Adequate analgesia with/wiithout sedation (which may be a general anaesthetic, particularly in muscular individuals)
- ○ Avoidance of rotational forces
- ○ Post reduction X-rays in two planes to confirm relocation
- ○ Reassessment and documentation of neurological and circulatory examination post reduction
Further investigations
Factors that will influence the decision to perform special investigations include the age of the patient and likelihood of operative intervention, the number of dislocations and the suspicion of associated injuries.
- Patients between the ages of 40 years and 60 years have an increased risk of clinically relevant rotator cuff tears (approximately 40%) and, consequently should undergo routine ultrasound/magnetic resinance imaging to assess cuff integrity.
- ○ Sensitivity and specificity significantly increases when MRA is also performed with the shoulder in an abducted and externally rotated position (ABER)20
- ○ CT is the most accurate at calculating glenoid bone loss21, a potential complication of recurrent instability. However, magnetic resinance imaging is also satisfactory and has the advantage of defining soft tissue abnormalities better
Non-operative management
Patients should be encouraged to mobilize as comfort dictates. Early referral to physiotherapy may be helpful in aiding mobilization.
- External rotation splintage has been proposed as a non-operative treatment because it allows the displaced labrum to return to a more physiological position22 and therefore potentially reduce recurrence rates.
- ○ One randomized controlled trial has supported the use of external rotation braces applied on the day of dislocation at reducing the risk of recurrence from 42% to 26% (p = 0.033) over 2 years23
Summary: The evidence for external rotation splintage is equivocal. In the cohort of patients in whom recurrent instability is most likely, external rotation gave no additional benefit over simple immobilization in a sling. Given the extra costs and possible poor compliance, external rotation immobilization is not recommended in the non-operative management of traumatic anterior shoulder instability.
Operative management of uncomplicated anterior shoulder instability
Operative choices: anatomic versus non-anatomic repair
When Bankart first described the labral pathology observed with anterior glenohumeral dislocation he advocated anatomic repair8, namely a Bankart repair.
Despite this, a number of non-anatomic repairs have been utilized, the most common being the Putti-Platt procedure.26–28 This procedure shortened the subscapularis tendon by tenotomy and repair with the lateral end sutured to the anterior glenoid rim and the medial part sutured to its original insertion, effectively ‘double breasting’ the tendon.
Only one randomized controlled trial has been performed comparing the results of anatomic (Bankart) and non-anatomic (Putti-Platt) repairs and this demonstrated equivocal results.26
Other cohort studies, however, have shown not only an increase in recurrence rates with non-anatomic repair (27) but also an increased incidence of early glenohumeral osteoarthritis.28,29
Summary: Non-anatomic repair is associated with an increased risk of secondary osteoarthritis, pain and reduction in movement without any perceived reduction in redislocation rates. Anatomic repair is therefore recommended as the surgery of choice when surgical intervention is indicated.
Operative choices: arthroscopic vs open repair
In a survey of members of BESS in 2002, arthroscopic stabilization was practiced by only 16% of surgeons as their preferred technique.30 This increased exponentially to 71% by 2009 with a corresponding fall in the number of surgeons preferring open stabilization.
A systematic review comparing open and arthroscopic repair demonstrated no statistically significant difference in recurrence rates for open Bankart repair and arthroscopic repair using anchors.31 Recurrence rates were 8% at a mean of 3.7 years and 8.5% at a mean of 2.2 years, respectively. Arthroscopic repair using tacks (as opposed to suture anchors) however, had a recurrence rate of 17% at a mean of 3.1 years.
A further systematic review again showed no difference between the techniques but did show a trend to improved outcomes with arthroscopic surgery with later publications.32
Two meta-analyses performed comparing arthroscopic and open stabilization concluded in favour of open techniques.33,34 However, the studies included a variety of fixation methods (transglenoid sutures, bio absorbable tack and suture anchors) and, when the randomized controlled studies comparing modern arthroscopic techniques (i.e. suture anchors) were considered independently, there were no differences in recurrence rates compared to open surgery.
Arthroscopic techniques using transglenoid sutures or bioabsorbable tacks have worse outcomes than open or arthroscopic techniques using suture anchors.35,36
Further randomized controlled trials have again shown no difference in outcome between open and arthroscopic techniques.37–39
Strength in internal and external rotation is reduced compared to the contralateral limb regardless of surgical approach.40
Summary: Modern arthroscopic stabilization techniques using suture anchors appear to be as effective as open anatomic repair in the treatment of traumatic anterior glenohumeral dislocation with a recurrence rate of approximately 8% at 2 years to 4 years. Less contemporary techniques, such as transglenoid suture fixation, are inferior and should not be used.
Operative choices: timing of surgery
Patients presenting with recurrent instability represent a simple problem to solve as the majority will require surgical intervention. The management of primary (first dislocation) anterior instability, however, is less well defined and will depend on a number of factors including the age and sex of the patient, their leisure activities and occupation.
Arciero et al.41 first proposed arthroscopic stabilization in young athletes following primary anterior glenohumeral dislocation demonstrating a significant reduction in recurrent instability of 14% versus 80% treated with sling immobilization.
A Cochrane review comparing nonsurgical and surgical management for acute anterior shoulder dislocation demonstrated a relative risk reduction of 0.2 (95% confidence interval = 0.11 to 0.33) in the surgical group.42 Of note, half of the patients randomized to conservative management opted for subsequent surgical intervention.
Chahal et al.43 published a systematic review comparing surgical repair with arthroscopic lavage or conservative management. Recurrent instability was significantly lower with Bankart repair when compared to arthroscopic lavage (relative risk = 0.14, 95% confidence interval = 0.06 to 0.31) and conservative treatment (relative risk = 0.26, 95% confidence interval = 0.10 to 0.67).
- Statistically significant risk factors (p < 0.05) for recurrent instability following arthroscopic anterior shoulder stabilization include:44
- ○ Age at the time of first dislocation (< 22 years)
- ○ Male sex
- ○ Time (> 6 months) to surgical intervention from initial dislocation
Summary: The risk of recurrent dislocation in young males is high and the evidence would support primary arthroscopic Bankart repair, particularly in those involved in contact sports or occupations involving overhead activities (Figure 3).
Operative management of complicated anterior instability
Glenoid bone loss
A loss of 20% of the glenoid surface area significantly increases the risk of recurrent instability. Methods used to restore glenoid bone include the use of iliac crest graft45 but the most accepted widely used method is a coracoid bone block transfer (Latarjet procedure).
The Bristow procedure (transfer of the coracoid tip under subscapularis to the anteroinferior glenoid) has been superseded by the Latarjet or modification of the Latarjet procedure. This procedure passes a large part of the coracoid process through a subscapularis split to the anteroinferior glenoid.
The majority of studies assessing coracoid bone block transfer are case series (level IV evidence).
Recurrent instability rates following the Latarjet procedure range from 2.9% to 8%.47–51
Reported complication rate though is high (25% to 30%) with non/fibrous union, neurological injury, recurrence and infection accounting for the majority.47,48
- A modification of the Latarjet procedure is to rotate the coracoid bone block 90 degrees to produce a ‘congruent arc’ bone block.
- ○ There are, however, no clinical trials which have compared the two techniques
More recently, arthroscopic Latarjet techniques have been described. It is too early to provide meaningful information regarding this.
Summary: An open Latarjet procedure should be considered in patients suffering from recurrent anterior glenohumeral instability in whom 20% glenoid bone loss is present or those in whom soft tissue stabilizations have failed. It should not be considered routinely as a primary procedure when glenoid bone loss is not present as a result of the significant risks of complications and the good results associated with soft tissue reconstructive procedures.
The use of a congruent arc modification has been described but no clinical trials have been completed. Arthroscopic techniques may, in the future, show comparable results, although there remains a lack of evidence for this at the present time.
Humeral bone loss
Hill–Sachs defects are present following almost all anterior glenohumeral dislocations because of the soft posterosuperior head impacting on the hard anteroinferior glenoid.
Hill–Sachs defects of greater than 40% of the humeral head are highly likely to exhibit instability requiring surgical intervention.54 Examination under anaesthetic through a physiological range of movement is best at identifying the clinically relevant engaging Hill–Sachs defect.55
Options in treating this issue include bony augmentation to the glenoid, in the form of coracoid bone block transfer, or treating the humeral defect directly.
The current available evidence is of low quality, mainly representing case series, and so should be used with caution.
Latarjet procedure
Burkhart et al.51 reported a recurrence rate of 3.9% at 4.3 years for patients undergoing a modified Latarjet procedure for significant bony loss on either the glenoid, humeral or both sides. The study did not differentiate between Hill–Sachs or glenoid defects.
Remplissage
Remplissage (meaning ‘to fill’ in French) is an arthroscopic capsulotenodesis of the posterior capsule and infraspinatus tendon to fill the Hill–Sachs lesion.56
A case series of 47 patients undergoing combined arthroscopic remplissage and Bankart repair had only one patient with recurrent instability.57 There was a mean reduction of external rotation with the arm in abduction of 9°.
A case–control study comparing arthroscopic stabilization with stabilization and remplissage (total of 50 patients) showed recurrence rates of 20% and 0%, respectively.46,58
Summary: The management of engaging Hill–Sachs defects remains contentious. Currently, the Latarjet procedure or remplissage in combination with arthroscopic Bankart repair appear the most acceptable methods in treatment but there have been no randomized controlled trials performed to substantiate their use.
Neurological injury
There is limited evidence on the management of neurological injury following traumatic anterior shoulder instability.
A case series of over 100 patients with axillary nerve injury following blunt trauma undergoing surgical intervention demonstrated moderate improvement in abduction with surgery.59 Surgery was performed at approximately 6 months with a decision for exploration based on poor deltoid recovery on clinical and electromyographic examination.
Surgery performed was neurolysis, nerve resection and repair or nerve resection and grafting depending on intra-operative nerve action potentials.
Summary: Careful clinical examination should be performed to identify neurological injuries. Physiotherapy is essential in minimizing loss of movement in the presence of neurological injury. Electromyography (EMG) studies should be performed at 6 weeks if no clinical recovery is seen. Referral to a nerve injury centre is recommended if EMG studies at 6 weeks do not show evidence of recovery.
Greater tuberosity fracture
Traumatic anterior instability with an associated greater tuberosity fracture has lower recurrence rates of instability.16,60
Fractures that are minimally displaced (< 5 mm) can be treated non-operatively with sling immobilization for 3 weeks followed by active assisted and active exercises.61,62 There was a trend towards worse outcomes for patients with greater than 3 mm displacement but this did not achieve statistical significance. Full recovery takes an average of 8 months.
Fractures displaced by greater than 5 mm have significantly better outcomes if managed operatively.63 Open reduction and internal fixation had slightly better functional results than closed reduction and percutaneous fixation but this was not statistically significant.
Summary: The majority of displaced greater tuberosity fractures will reduce once the anterior dislocation is relocated. Those that remain greater than 5 mm displaced on post reduction radiographs should be treated surgically. Regular imaging for 4 weeks following injury should be performed to identify late displacement. In patients who perform regular overhead activities a lower threshold for surgical intervention should be considered.
Rotator cuff tears
Clinically relevant (i.e. symptomatic) rotator cuff tears following traumatic anterior instability most likely represent tears through degenerate tendon or ‘acute on chronic’ tears. Nevertheless, they are best treated with surgical repair.
A systematic review of glenohumeral instability with associated rotator cuff tears (level III and IV evidence) showed improved pain relief and satisfaction with surgical repair compared to non-operative management.64 It was unclear whether rotator cuff repair alone or repair with anterior stabilization was better.
Further studies corroborate that traumatic rotator cuff tears treated with surgical repair have better functional results.65 Outcome appears better in those treated with early repair.66,67
Summary: Patients over the age of 40 years should, ideally, undergo ultrasound or magnetic resinance imaging to assess cuff integrity following traumatic anterior instability. If a tear is present, they should be assessed by a shoulder surgeon for consideration of early surgical repair. All patients should be assessed for rotator cuff weakness following injury, especially those over 60 years, and any patients with a suspected rotator cuff tear should be investigated accordingly.
Linked metrics
Shoulder dislocation
- Diagnosis Codes (ICD-10-CM)
- ○ S43.00 – unspecified subluxation and dislocation of shoulder joint
- ○ S43.01 – Anterior subluxation and dislocation of humerus
- ○ S43.02 – Posterior subluxation and dislocation of humerus
- ○ S43.03 – Inferior subluxation and dislocation of humerus
- ○ M24.41 – Recurrent dislocation of shoulder
- ○ Procedure Codes (OPCS 4.4)
- ○ W77.12 – Stabilization of unidirectional instability of shoulder joint, including anterior, posterior and arthroscopic
- ○ W77.60 – Labral repair (shoulder stabilization)
- ○ W77.80 – Revision stabilization of shoulder joint
- ○ W88.20 – Diagnostic arthroscopic examination of shoulder joint
- ○ Procedure Codes (OPCS 4.5) O29.1
- Y76.7 is added for arthroscopic approach to joint
Outcome metrics
Length of stay – day case (23 hours) and overnight.
Re-admission rate within 3 months.
Oxford Shoulder Instability Score, pre-operatively and 12 months post-surgery.
Infection.
Data from any National Registries.
Research
Patient-reported outcome measures – a validated clinical score, preferably a patient reported outcome measure (PROM) should be used pre-operatively and at one and three years following treatment.
Acceptable scores include the Oxford Shoulder Instability Score (OSIS).
EQ 5D scores should be captured pre-operatively and one year following intervention to allow for a health economic analysis
There are currently no national trials being performed on shoulder instability.
Quality specification: audit
Oxford Shoulder Instability Score pre-operatively and 1-year follow-up.
Consider National Registry.
Directory: patient/public/clinician information
Patient and public information – ensure all available information is provided regarding the benefits and risks of all treatment options.
Clinician information – ensure access to available evidence.
Evidence
Evidence for effectiveness and cost effectiveness of treatment
A systematic search of 14 databases including Medline, Pubmed and Evidence Based Medicine Reviews between January 1984 and December 2004 was undertaken68 comparing arthroscopic and open stabilization. The review found 11 studies that met the inclusion criteria, of which only two were randomized controlled trials. The studies were of poor to fair methodological quality. When comparable data were pooled, there were no significant differences (p > 0.05) between arthroscopic and open stabilization.
Cost effectiveness analysis69 showed cost saving and reduced recurrence with primary surgery for 15-year-old males and females and 25-year-old males compared to non-operative management. Primary surgery was not only more effective, but also more costly for 25-year-old females and 35-year-old males and females
Expected-value decision analysis70, a tool evaluating patients’ expectations for different disease states, was performed on arthroscopic repair versus non-operative management. Using utility values (where 0 represents the worst possible outcome and 10 is the best), non-operative treatment was associated with a utility value of 5.9 versus 7.6 for arthroscopic treatment. It was also found that, when the rate of recurrence fell below 32%, the utility value between the two groups were similar and so non-operative management should be considered.
Summary
It is important to note that evidence to support the effectiveness of one method over another and the timing of surgical treatment remains limited. Until such evidence becomes available, clinical and shared decision-making on available interventions based on level of symptoms and functional restriction is recommended.
The risk of recurrent instability correlates strongly with age and sex with males under the age of 18 having an 80% chance of further dislocation.
Immobilization for more than 1 week is not beneficial in reducing recurrence rates.
External rotation splintage may allow the labrum to heal in a more physiological position but recurrence rates are similar to simple sling immobilization.
Non-anatomic repair (e.g. Putti-Platt procedure) is associated with an increased risk of secondary osteoarthritis, pain and stiffness without an apparent reduction in recurrent instability.
Arthroscopic anatomic repair using suture anchors is as effective as open anatomic repair in the absence of significant bony defects with a recurrence of approximately 8% at 2 years to 4 years.
Latarjet procedure is indicated in patients with significant glenoid bone loss and may also have a role in the management of engaging Hill–Sach’s lesions. It is not routinely indicated as a primary procedure as a result of the high complication rate and good results with arthroscopic soft tissue reconstructive procedures.
Remplissage may be of benefit in the management of humeral bone loss.
Neurological injury is present in over 10% of patients with traumatic anterior glenohumeral instability. Physiotherapy is essential to maintain range of movement when the nerve recovers. EMG should be performed at 6 weeks and, if there is no evidence of clinical or EMG recovery at 6 weeks, then early referral to a nerve injury centre is recommended.
Greater tuberosity fractures that are displaced more than 5 mm should be fixed to minimize functional loss. Weekly radiographs for the initial 4 weeks should be performed to identify delayed displacement in those fractures with less than 5 mm displacement managed non-operatively.
Clinically relevant rotator cuff tears are present in at least 10% of patients. Patients over the age of 40 years should undergo investigation for this with a view to performing early rotator cuff repair to minimize functional loss.
Cost-effectiveness analysis demonstrated cost saving and reduced recurrence with primary surgery for 15-year-old males and females and 25-year-old males compared to non-operative management.
Conservative treatment
- Likely to be beneficial.
- Early mobilization
- Unknown effectiveness.
- External rotation splintage
Surgery (uncomplicated)
- Likely to be beneficial.
- Arthroscopic anatomic repair using suture anchors
- Open anatomic repair
- Not beneficial.
- Bio absorbable tacks
- Transglenoid fixation
- Non-anatomic repair (e.g. Putti-Platt procedure)
Surgery (Complicated)
- Likely to be beneficial.
- Glenoid bone loss – Latarjet procedure
- Greater tuberosity fixation if >5 mm displacement
- Rotator cuff repair for traumatic cuff tears
- Unknown effectiveness.
- Humeral bone loss – remplissage or Latarjet procedure
Acknowledgements
Contributions from the BESS Working Group: Peter Brownson, Oliver Donaldson, Mike Fox, Jonathan Rees, Amar Rangan, Anju Jaggi, Graham Tytherleigh-Strong, Julie McBirnie, Michael Thomas and Rohit Kulkarni. Contributions from the BOA Guidance Development Group: Rohit Kulkarni (Chair), Joe Dias, Jonathan Rees, Andrew Carr, Chris Deighton, Vipul Patel, Federico Moscogiuri, Jo Gibson, Clare Connor, Tim Holt, Chris Newsome, Mark Worthing and James Beyer.
References
- 1.Jaggi A, Lambert S. Rehabilitation for shoulder instability. Br J Sports Med 2010; 44: 333–340. [DOI] [PubMed] [Google Scholar]
- 2.Good Medical Practice. http://www.gmc-uk.org/guidance/good_medical_practice.asp.
- 3.Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg 1989; 108: 288–90. [DOI] [PubMed] [Google Scholar]
- 4.Simonet WT, Melton LJ, III, Cofield RH, Ilstrup DM. Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orth Relat Res 1984; 186: 186–91. [PubMed] [Google Scholar]
- 5.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg (Am) 2010; 92: 542–9. [DOI] [PubMed] [Google Scholar]
- 6.Bowen MK, Warren RF. Ligamentous control of shoulder stability based on selective cutting and static translation experiments. Clin Sports Med 1991; 10: 757–82. [PubMed] [Google Scholar]
- 7.Lippitt SB, Vanderhooft E, Harris SL, Sidles JA, Harryman DT, Matsen FA., III Glenohumeral stability from concavity-compression: a quantitative analysis. J Shoulder and Elbow Surg 1993; 2: 27–35. [DOI] [PubMed] [Google Scholar]
- 8.Bankart AS. Recurrent or habitual dislocation of the shoulder joint. Br Med J 1923; 2: 1132–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg (Am) 2012; 94: 18–26. [DOI] [PubMed] [Google Scholar]
- 10.Visser CP, Coene LN, Brand R, Tavy DL. The incidence of nerve injury in anterior dislocation of the shoulder and its influence on functional recovery. A prospective clnical and EMG study. J Bone Joint Surg (Br) 1999; 81: 679–85. [DOI] [PubMed] [Google Scholar]
- 11.Simank HG, Dauer G, Schneider S, Loew M. Incidence of rotator cuff tears in shoulder dislocations and results of therapy in older patients. Arch Orthop Trauma Surg 2006; 126: 235–40. [DOI] [PubMed] [Google Scholar]
- 12.Toolanen G, Hildingsson C, Hedlund T, Knibestöl M, Oberg L. Early complications after anterior dislocation of the shoulder in patients over 40 years. An ultrasonographic and electromyographic study. Acta Orthop Scand 1993; 64: 549–52. [DOI] [PubMed] [Google Scholar]
- 13.Shin SJ, Yun YH, Kim DJ, Yoo JD. Treatment of traumatic anterior shoulder dislocation in patients older than 60 years. Am J Sports Med 2012; 40: 822–7. [DOI] [PubMed] [Google Scholar]
- 14.Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger, a prospective twenty-five year follow up. J Bone Joint Surg (Am) 2008; 90: 942–52. [DOI] [PubMed] [Google Scholar]
- 15.Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg (Am) 2006; 88: 2326–36. [DOI] [PubMed] [Google Scholar]
- 16.Paterson WH, Throckmorton TW, Koester M, Azar FM, Kuhn JE. Position and duration of immobilization after primary anterior shoulder dislocation: a systematic review and meta-analysis of the literature. J Bone Joint Surg (Am) 2010; 92: 2924–33. [DOI] [PubMed] [Google Scholar]
- 17.Wallace WA, Hellier M. Improving radiographs of the injured shoulder. Radiography 1983; 49: 229–33. [PubMed] [Google Scholar]
- 18.Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology 2005; 237: 578–83. [DOI] [PubMed] [Google Scholar]
- 19.Smith TO, Drew BT, Toms AP. A meta-analysis of the diagnostic test accuracy of MRA and MRI for the detection of glenoid labral injury. Arch Orthop Trauma Surg 2012; 132: 905–19. [DOI] [PubMed] [Google Scholar]
- 20.Tian CY, Cui GQ, Zheng ZZ, Ren AH. The added value of ABER position for the detection and classification of anteroinferior labroligamentous lesions in MR arthrography of the shoulder. Eur J Radiol 2013; 82: 651–7. [DOI] [PubMed] [Google Scholar]
- 21.Chuang TY, Adams CR, Burkhart SS. Use of preoperative three dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy 2008; 24: 376–82. [DOI] [PubMed] [Google Scholar]
- 22.Itoi E, Sashi R, Minagawa H, Shimizu T, Wakabayashi I, Sato K. Position of immobilization after dislocation of the glenohumeral joint. A study with use of magnetic resonance imaging. J Bone Joint Surg (Am) 2001; 83: 661–7. [DOI] [PubMed] [Google Scholar]
- 23.Itoi E, Hatakeyama Y, Sato T, et al. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence. A randomized controlled trial. J Bone Joint Surg (Am) 2007; 89: 2124–31. [DOI] [PubMed] [Google Scholar]
- 24.Liavaag S, Brox JI, Pripp AH, Enger M, Soldal LA, Svenningsen S. Immobilization in external rotation after primary shoulder dislocation did not reduce the risk of recurrence: a randomised controlled trial. J Bone Joint Surg (Am) 2011; 93: 897–904. [DOI] [PubMed] [Google Scholar]
- 25.Finestone A, Milgrom C, Radeva-Petrova DR, et al. Bracing in external rotation for traumatic anterior dislocation of the shoulder. J Bone Joint Surg (Br) 2009; 91: 918–21. [DOI] [PubMed] [Google Scholar]
- 26.Salomonsson B, Abbaszadegan H, Revay S, Lillkrona U. The Bankart repair versus the Putti-Platt procedure. Acta Orthop 2009; 80: 351–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hovelius L, Thorling J, Fredin H. Recurrent anterior dislocation of the shoulder. Results after the Bankart and Putti-Platt operations. J Bone Joint Surg (Am) 1979; 61: 566–9. [PubMed] [Google Scholar]
- 28.Kiss J, Mersich I, Perlaky GY, Szollas L. The results of the Putti-Platt operation with particular reference to arthritis, pain, and limitation of external rotation. J Shoulder Elbow Surg 1998; 7: 495–500. [DOI] [PubMed] [Google Scholar]
- 29.Konig DP, Rutt J, Treml O, Hackenbroch MH. Osteoarthritis and recurrences after Putti-Platt and Eden-Hybbinette operations for recurrent dislocations of the shoulder. Int Orthop 1997; 21: 72–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Malhotra A, Freudmann MS, Hay SM. Management of traumatic anterior shoulder dislocation in the 17- to 25-year age group: a dramatic evolution of practice. J Shoulder Elbow Surg 2012; 21: 545–53. [DOI] [PubMed] [Google Scholar]
- 31.Harris JD, Gupta AK, Mall NA, et al. Long-term outcomes after bankart shoulder stabilization. Arthroscopy 2013; 29: 920–33. [DOI] [PubMed] [Google Scholar]
- 32.Petrera M, Patella V, Patella S, Theodoropoulos J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc 2010; 18: 1742–7. [DOI] [PubMed] [Google Scholar]
- 33.Lenters TR, Franta AK, Wolf FM, Leopold SS, Matsen FA. Arthroscopic compared with open repairs for recurrent anterior shoulder instability. A systematic review and meta-analysis of the literature. J Bone Joint Surg (Am) 2007; 89: 244–54. [DOI] [PubMed] [Google Scholar]
- 34.Mohtadi NGH, Bitar IJ, Sasyniuk TM, Hollinshead RM, Harper WP. Arthroscopic versus open repair for traumatic anterior shoulder instability. A meta-analysis. Arthroscopy 2005; 21: 652–8. [DOI] [PubMed] [Google Scholar]
- 35.Freedman KB, Smith AP, Romeo AA, Cole BJ, Bach BR., Jr Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for recurrent anterior instability of the shoulder: a meta-analysis. Am J Sports Med 2004; 32: 1520–7. [DOI] [PubMed] [Google Scholar]
- 36.Hobby J, Griffin D, Dunbar M, Boileau P. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. J Bone Joint Surg Br 2007; 89: 1188–96. [DOI] [PubMed] [Google Scholar]
- 37.Pulavarti RS, Symes TH, Rangan A. Surgical interventions for anterior shoulder instability in adults. Cochrane Database Syst Rev 2009; 4: CD005077–CD005077. [DOI] [PubMed] [Google Scholar]
- 38.Mahiroğulları M, Ozkan H, Akyüz M, Uğraş AA, Güney A, Kuşkucu M. Comparison between the results of open and arthroscopic repair of isolated traumatic anterior instability of the shoulder. Acta Orthop Traumatol Turc 2010; 44: 180–5. [DOI] [PubMed] [Google Scholar]
- 39.Archetti Netto N, Tamaoki MJS, Lenza M, et al. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniques. Arthroscopy 2012; 28: 900–8. [DOI] [PubMed] [Google Scholar]
- 40.Hiemstra LA, Sasyniuk TM, Mohtadi NGH, Fick GH. Shoulder strength after open versus arthroscopic stabilization. Am J Sports Med 2008; 36: 861–7. [DOI] [PubMed] [Google Scholar]
- 41.Arciero RA, Wheeler JH, Ryan JB, McBride JT. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med 1994; 22: 589–94. [DOI] [PubMed] [Google Scholar]
- 42.Handoll HH, Almaiyah MA, Rangan A. Surgical versus non-surgical treatment for acute anterior shoulder dislocation. Cochrane Database Syst Rev 2004; 1: CD004325–CD004325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chahal J, Marks PH, Macdonald PB, et al. Anatomic Bankart repair compared with nonoperative treatment and/or arthroscopic lavage for first time traumatic shoulder dislocation. Arthroscopy 2012; 28: 565–75. [DOI] [PubMed] [Google Scholar]
- 44.Porcellini G, Campi F, Pegreffi F, Castagna A, Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg (Am) 2009; 91: 2537–42. [DOI] [PubMed] [Google Scholar]
- 45.Montgomery WH, Jr, Wahl M, Hettrich C, Itoi E, Lippitt SB, Matsen FA., III Anteroinferior bone-grafting can restore stability in osseus glenoid defects. J Bone Joint Surg (Am) 2005; 87: 1972–7. [DOI] [PubMed] [Google Scholar]
- 46.Buza JA, Iyengar JJ, Anakwenze OA, Ahmad CS, Levine WN. Arthroscopic Hill–Sachs remplissage a systematic review. J Bone Joint Surg Am 2014; 96: 549–55. [DOI] [PubMed] [Google Scholar]
- 47.Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg 2013; 22: 286–92. [DOI] [PubMed] [Google Scholar]
- 48.Shah A, Butler R, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg (Am) 2012; 94: 495–501. [DOI] [PubMed] [Google Scholar]
- 49.Dossim A, Abalo A, Dosseh E, Songne B, Ayite A, Gnandi-Pio F. Bristow-Latarjet repairs for anterior instability of the shoulder: clinical and radiographic results at mean 8.2 years follow up. Chir Main 2008; 27: 26–30. [DOI] [PubMed] [Google Scholar]
- 50.Schmid SL, Farshad M, Catanzaro S, Gerber C. The Latarjet procedure for the treatment of recurrence of anterior instability of the shoulder after operative repair: a retrospective case series of forty-nine consecutive patients. J Bone Joint Surg (Am) 2012; 94: e75–e75. [DOI] [PubMed] [Google Scholar]
- 51.Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007; 23: 1033–41. [DOI] [PubMed] [Google Scholar]
- 52.Boons HW, Giles JW, Elkinson I, Johnson JA, Athwal GS. Classic versus congruent coracoid positioning during the Latarjet procedure: an in vitro biomechanical comparison. Arthroscopy 2013; 29: 309–16. [DOI] [PubMed] [Google Scholar]
- 53.Giles JW, Puskas G, Welsh M, Johnson JA, Athwal GS. Do the traditional and modified Latarjet techniques produce equivalent reconstruction stability and strength? Am J Sports Med 2012; 40: 2801–7. [DOI] [PubMed] [Google Scholar]
- 54.Armitage MS, Faber KJ, Drosdowech DS, Litchfield RB, Athwal GS. Humeral head bone defects: Remplissage, allograft and arthroplasty. Orthop Clin North Am 2010; 41: 417–425. [DOI] [PubMed] [Google Scholar]
- 55.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill–Sachs lesion. Arthroscopy 2000; 16: 677–694. [DOI] [PubMed] [Google Scholar]
- 56.Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill–Sachs ‘remplissage’: an arthroscopic solution for the engaging Hill–Sachs lesion. Arthroscopy 2008; 24: 723–6. [DOI] [PubMed] [Google Scholar]
- 57.Boileau P, O’Shea K, Varga P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill–Sachs remplissage. J Bone Joint Surg (Am) 2012; 94: 618–26. [DOI] [PubMed] [Google Scholar]
- 58.Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair – new frontiers in the prevention of recurrent shoulder instability: a 2 year follow up comparative study. Am J Sports Med 2012; 40: 2462–9. [DOI] [PubMed] [Google Scholar]
- 59.Kline DG, Kim DH. Axillary nerve repair in 99 patients with 101 stretch injuries. J Neurosurg 2003; 99: 630–6. [DOI] [PubMed] [Google Scholar]
- 60.Salomonsson B, von Heine A, Dahlborn M, et al. Bony bankart is a positive predictive factor after primary shoulder dislocation. Knee Surg Sports Traumatol Arthrosc 2010; 18: 1425–31. [DOI] [PubMed] [Google Scholar]
- 61.Platzer P, Kutscha-Lissberg F, Lehr S, Vecsei V, Gaebler C. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Injury 2005; 36: 1185–9. [DOI] [PubMed] [Google Scholar]
- 62.Rath E, Alkrinawi N, Levy O, Debbi R, Amar E, Atoun E. Minimally displaced fractures of the greater tuberosity: outcome of non-operative treatment. J Shoulder Elbow Surg 2013; 22: e8–11. [DOI] [PubMed] [Google Scholar]
- 63.Platzer P, Thalhammer G, Oberleitner G, et al. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma 2008; 65: 843–8. [DOI] [PubMed] [Google Scholar]
- 64.Gombera MM, Sekiya JK. Rotator cuff tear and glenohumeral instability: a systematic review. Clin Orthop Relat Res 2014; 472: 2448–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mall N, Lee A, Chahal J, Sheman S, Romeo A, Verma N, Cole B. An evidence-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy 2013; 29: 366–76. [DOI] [PubMed] [Google Scholar]
- 66.Petersen S, Murphy T. The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg 2011; 20: 62–8. [DOI] [PubMed] [Google Scholar]
- 67.Hantes M, Karidakis G, Vlychou M, Varitimidis S, Dailiana Z, Malizos K. A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 2011; 19: 1766–70. [DOI] [PubMed] [Google Scholar]
- 68.Ng C, Bialocerkowski A, Hinman R. Effectiveness of arthroscopic versus open surgical stabilisation for the management of traumatic anterior glenohumeral instability. Int J Evid Based Healthc 2007; 5: 182–207. [DOI] [PubMed] [Google Scholar]
- 69.Crall TS, Bishop JA, Guttman D, Kocher M, Bozic K, Lubowitz JH. Cost-effectiveness analysis of primary arthroscopic stabilization versus nonoperative treatment for first time anterior glenohumeral dislocations. Arthroscopy 2012; 28: 1755–65. [DOI] [PubMed] [Google Scholar]
- 70.Bishop JA, Crall TS, Kocher MS. Operative versus nonoperative treatment after primary traumatic anterior glenohumeral dislocation: expected-value decision analysis. J Shoulder Elbow Surg 2011; 20: 1087–94. [DOI] [PubMed] [Google Scholar]