Abstract
Historically, scapular dyskinesia has been used to describe an isolated clinical entity whereby an abnormality in positioning, movement or function of the scapula is present. Based upon this, treatment approaches have focused on addressing local isolated muscle activity. Recently, however, there has been a progressive move towards viewing the scapula as being part of a wider system of movement that is regulated and controlled by multiple factors, including the wider kinetic chain and individual patient-centred requirements. We therefore propose a paradigm shift whereby scapular dyskinesia is seen not in isolation but is considered within the broader context of patient-centred care and an entire neuromuscular system.
Keywords: scapula, dyskinesis, shoulder, assessment, rehabilitation
Introduction
‘Optimal’ scapular motion is considered to be crucial to the functioning of the shoulder and, as such, any alteration in scapular kinematics is believed to be a contributing factor to the development of shoulder pathology.1 In particular, any variation in the amount of scapular upward rotation that occurs is particularly implicated as a predisposing factor in the development of shoulder symptoms. This is because the scapula must upwardly and externally rotate and posteriorly tilt adequately to prevent the humeral head from compressing and shearing against the under surface of the acromion: one of the proposed mechanisms for producing the syndrome commonly referred to as subacromial impingement. Based on this widely held view, the aim of many shoulder rehabilitation programmes is to correct aberrant, local scapula mechanics.
The notion of scapular dyskinesis for the purposes of the present review does not include presentations where there is a defined abnormality of the neuromuscular system; for example, neuritis, neuropathy, neuropraxia or other forms of peripheral nerve injury.
The purpose of the present review is to summarize current concepts and provide the clinician with not only a foundation of reasoning on which to base clinical decision-making, but also some practical suggestions as to how these could be incorporated and utilized in daily practice.
What is normal and does it matter?
Scapulohumeral rhythm (SHR) is the co-ordination between humeral and scapular movements and was first described by Codman2 and subsequently popularized by Inman.3 X-rays were used to calculate scapula movement of seemingly one subject and the conclusion reached that there was an overall constant scapulohumeral rhythm of 2 : 1 during shoulder flexion and abduction. Considering that a full arc of shoulder movement is 180°, this is a result of 120° of glenohumeral movement and 60° of upward rotation.
With the benefit of time and technology, it is clear that SHR is much more complex than the reported 2 : 1 ratio. Ratios are characteristically inconsistent, suggesting that the relationship is variable and nonlinear. In a survey of practicing physiotherapists which asked how reliable and valid they felt that the SHR theory is in predicting pathological sequences in the shoulder complex Kirby et al.4 reported that 77% held the belief that it was reliable. The study by Kirby et al.4 therefore demonstrates that SHR is a widely held belief and that physiotherapists therefore routinely make clinical decisions based on principles that may lack validity. Upward rotation is of course, just one component of scapula movement, with internal/external rotation and antero/posterior tipping occurring simultaneously around three different axes.
If, as the evidence suggests, there is a wide range of physiological normal with high degrees of variability within and between individuals5,6 and populations,7 benchmarking ‘normal’ against ‘pathological’ poses a considerable challenge. There are also variations of scapular movement within individuals depending on the speed at which movement is performed,8 the load used,9 whether movement is concentric or eccentric10 and is performed unilaterally or bilaterally11 or even the hand dominance of the subject.12 Against this background, establishing what ‘abnormal’ is in the absence of an accepted norm is a fundamental flaw in the traditional concept.
Assessing the ‘abnormal’ scapula: the traditional model
Historically, there have been attempts to establish a threshold for what is and what isn’t a dyskinetic scapula such as the scapular lateral slide test.13 Tests have generally involved (i) quantitative measures of abnormality or (ii) visual observation and a subjective judgement by the clinician as to whether or not it is normal. Although static and/or dynamic scapular asymmetry is commonly integrated into clinical assessment, the collective body of literature undermines its ubiquity. Both quantitative and qualitative methods are of little clinical value when it is considered that:
Postural asymmetries of greater than 1.5 cm are commonplace in asymptomatic individuals7,12
Measurement is subject to measurement error and observer bias14
No difference in scapular dyskinesis between symptomatic and asymptomatic shoulders have been found across several studies15–17
Observed dyskinesis may actually be a strategy to optimize certain individuals or cohorts18–20
Only low–moderate reliability and/or agreement is found between therapists regarding identification or categorization of dyskinesis21,22
Subjects identified by visual and three-dimensional tracking as having dyskinesis are no more likely to report symptoms.23
There is also the problem of relevance. If the subject of the measurement (in this case whether or not a scapula is dyskinetic) is a flawed concept, then the tests themselves are of limited use.
An improbable model?
As has happened so many times in our profession, the original concept of a pure, delineated and possibly dogmatic theory and its associated assessment has, over time and with a growing body of research become questionable. A recent consensus of assessment of visual observation of scapula dyskinesis has further reduced attempts to quantitatively assess scapula dyskinesis to a qualitative yes/no category.24
The traditional model of assessment of scapular dyskinesis appears to be becoming more implausible (Table 1). The evidence challenging the existence of and the assessment for scapular dyskinesis is broad based but, to compound matters, it would appear that attempts to correct identified scapular dyskinesis with rehabilitation are largely unsuccessful. McClure et al.25 found that shoulder impingement patients with supposed scapular dyskinesis, as measured with three-dimensional motion sensor equipment, had significant improvements in their pain and function following a 6-week exercise programme. The identified dyskinesis, however, did not change. Similar results were demonstrated in a more recent study by Struyf et al.26 that improvements in pain and function following rehabilitation were not accompanied by alterations in the so-called dyskinetic movement.
Table 1.
Challenges to the evidence regarding scapula dyskinesia
| In the absence of an identified normal, abnormal is an unknown entity |
| What is perceived as abnormal may in fact be a normal adaptation strategy |
| Tests used to supposedly identified abnormalities cannot be claimed to do so given that they lack construct validity |
| Measurements are unreliable and prone to measurement error and bias |
| A causal relationship between the existence of scapular dyskinesis and the presence of symptoms cannot be established |
The whole concept of scapula dyskinesis as an isolated condition is therefore facing some kind of existential crisis. Perhaps it does not exist at all.
Dissolve or evolve: the theory limps on?
It would be remiss at this point to advocate the dissolution of all things pertaining to aberrant scapula humeral rhythm and throw the baby out with the kinematic bathwater. Whether it is subjectively labelled as normal or abnormal, what is observed is the association and interdependence of the neuromusculoskeletal system around the trunk, shoulder girdle and wider kinetic chain.
The end result should be production of smooth, controlled movement between the humeral and scapula components of movement and this requires significant co-ordination. It is perhaps time to evolve our thinking and move towards a systems-based approach.
During the course of movement, muscles almost never work in isolation. Co-ordinated, controlled movement is the outcome of a functioning neuromuscular system. If something goes wrong with the movement, it could be attributed to any part of the system. The complexity of this extraordinary process is reliant on an integrated process of sensoriomotor control. Such control requires successful interaction of its component parts such as the motor cortex, thalmic system and cerebellum, as well as higher cognitive functions such as perception.27 The interdependence of all of these systems is underpinned by a vast network of neuronal circuitry, which is far from being understood.
Scapula assessment revisited: if you can affect it, suspect it
The very nature of the complexity and the interdependency of all the systems required for motor control render the existence of a litmus test for the presence of scapular dyskinesis extremely unlikely and the search for one a potentially fruitless task. Over the last decade, there has been a gradual move in the assessment of musculoskeletal conditions from the limited value of the traditional orthopaedic test toward a more global, systems-based approach. The publication of the shoulder symptom modification procedure (SSMP)28 signalled a paradigm shift in the way shoulder assessment was conducted. This approach involves subjecting patients with shoulder pain to a series of independent manoeuvres in an attempt to reduce the patient’s numerical symptom rating scale by 30%. Such interventions include thoracic (postural) correction, scapula movement facilitation, humeral head procedures and neuromodulation procedures. The muscle contraction element of the humeral head and scapula interventions aim to modify muscle activity around the shoulder with the intention of positively altering the pattern of muscular recruitment of the external rotators, humeral head depressors and/or humeral head adductors. If successful, the facilitation of these muscle groups can be incorporated into early treatment programmes.
As a result of its close association with the wider kinetic chain, techniques to reduce the appearance of dyskinesis by incorporating elements chain activity (e.g. single leg standing and standing on tip toes) have been used with demonstrably good effect.29 The use of isometric glenohumeral external rotation with or without concurrent shoulder flexion as proposed by the SSMP can be easily applied with substantial affect. The exact mechanism by which these procedures reduce symptoms is unknown but, clinically, it appears that, by accessing posterior rotator cuff activity via glenohumeral external rotation, a patient with what could be described as visible scapular dyskinesis performs this manoeuvre and, as far as the limitations of visual observation allow, the dyskinesis significantly reduces or disappears altogether. If accompanied by a reduction in pain, this would be a favourable response to the procedure. As mentioned previously studies by Tate et al.23 McClure et al.25 and Struyf et al.26 highlighted patient’s outcome in terms of pain and function appears to be unrelated to changes in scapular kinematics. It is therefore not alterations to the appearance of dyskinesis per se that is the intended aim of the improvement tests but rather the reduction in reported symptoms that can be achieved with their use.
The fact that such a spectrum of different interventions all have the potential to reduce the dyskinesis introduces another thought dimension. If multiple and varying actions all have the potential to ‘correct’ the scapular dyskinesis, then there can be no single mechanism by which said scapular dyskinesis occurred in the first instance. Subgroup analysis of which type of patients respond best to which type of intervention would be revealing. However, no such predictive measures have been validated and clinicians do not have the luxury of waiting until they are.
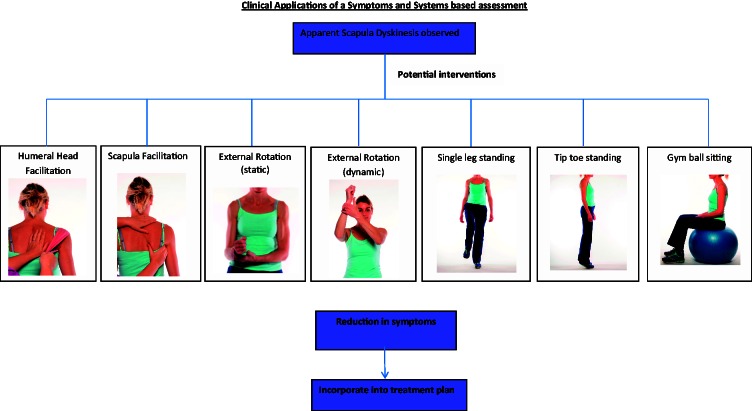
In an attempt to signpost therapists or indeed our surgical colleagues, the assessment tools in Fig. 1 are suggested as a starting place to attempt to find an intervention that affects either the patient’s symptoms that may include pain and/or instability.
Figure 1.
Potential symptom modification procedures.
Making sense of the assessment
If these ‘improvement’ or ‘symptom modification’ procedures have a significant effect on symptoms, they could be used at the starting point for rehabilitation and exercise prescription. However, some elements are easier to integrate than others. For example, if dynamic external rotation or tip toe/single leg standing reduces the symptoms or the appearance of dyskinesis, then this can easily be used as a foundation on which any number of other exercises functionally relevant to the patient can be built. If, however, humeral facilitation or scapular upward rotation improves the patients symptoms, then this is less straightforward. Scapular upward rotation is not a movement that exists in isolation and the translational anterior posterior glide movement of humeral head facilitation requires an externally applied pressure.
The challenge then becomes finding an exercise that capitalizes on the symptom reduction achieved during symptom modification. For this, clinical reasoning needs to take one step further and this is significantly aided by understanding the roles and function of the scapula and rotator cuff.
Understanding the functional anatomy
When glenohumeral movement occurs, the scapula must also move to allow the repositioning of the glenoid fossa thus increasing the available range of movement. During this movement, the scapulohumeral and axioscapular muscles must collectively function to maintain optimal mechanical alignment. Rotator cuff activity prevents unwanted humeral head translation but, when left unchecked, would pull the scapula laterally, essentially creating a destabilizing force. The axioscapular muscles respond by preventing the scapulohumeral muscles from destabilizing the scapula and produce the upward rotation, posterior tilting and externally rotate necessary for optimal movement and function.30 A high correlation therefore exists between the action of scapulohumeral and axioscapular muscles and activity in one group does not exist without corresponding activity in the other.
Just like the rotator cuff, scapula muscles have multiple roles which vary, dependent on the task, the load, the speed or the range in which the movement is occurring.30 At any time, dependent on these factors, any part of the rotator cuff, other scapulohumeral or axioscapular muscles could be acting in an agonist, antagonist, stabilizing (static or dynamic) or synergistic function (Table 2). Glenohumeral external rotation exercises, for example, are classically regarded as working the rotator cuff in its agonist role. This is true, but it is also true of all shoulder rotator torque generators and is therefore not specific to the rotator cuff. Glenohumeral external rotation however also requires the scapular muscles to function in their stabilizing role, explaining why either static or dynamic rotation utilized through symptom modification procedures can change apparent scapula dyskinesis.
Table 2.
The varying roles of muscles
| Type | Role |
|---|---|
| Agonist | Mover: prime or assistant mover |
| Antagonist | Muscle which must relax or work eccentrically to allow the desired movement to occur |
| Stabilizer | Muscle that supports a body part so that another muscle will have a firm base from which to act |
| Synergist | Muscle that eliminates an undesired movement that would otherwise be produced by the mover(s) and stabilizer(s) |
| Scapulohumeral muscles | |
| Rotator cuff | |
| Deltoid | |
| Teres major | |
| Long head of triceps | |
| Axioscapular muscles | |
| Trapezius | |
| Levator scapulae | |
| Rhomboid major + minor | |
| Serratus anterior | |
| Pectoralis minor | |
| Axiohumeral muscles | |
| Pectoralis major | |
| Latissimus dorsi | |
In addition to their agonistic role specific shoulder muscles also stabilize against destabilizing forces created by other shoulder muscles but this is far from static. Rotator cuff muscles prevent unwanted translation of the humeral head caused by other humeral muscles (e.g. deltoid and pectoralis major). Axioscapular muscles work against the destabilizing force of the scapulohumeral muscles to prevent the scapulohumeral muscles from translating the scapula off the thoracic cage. To rehabilitate the stabilizing function of the axioscapular muscles (and also, by virtue of their interdependence, the rotator cuff), it is perhaps more useful to consider strategies that allow the shoulder complex to react to de-stabilizing forces.30
If a particular movement cannot be performed without apparent scapula dyskinesis, it is worth considering that the cause of this is not ‘weakness’ and inability of, for example, the serratus anterior to perform its agonistic role but the inability of the scapular and/or rotator cuff muscles to work simultaneously in both their mobilizer and dynamic stabilizing roles. Delayed activation of serratus anterior in the early stages of movement has been implicated as a potential source of scapula dyskinesis in patients with shoulder symptoms.17,31 Data from these studies have indicated that such movement lag has normalized before 90°, which is outside the range of the painful arc classically associated with impingement type symptoms. Although conjecture, there is speculation that any increased rate of upward rotation and/or posterior tipping to overcome latency contributes to the appearance of dyskinesia.
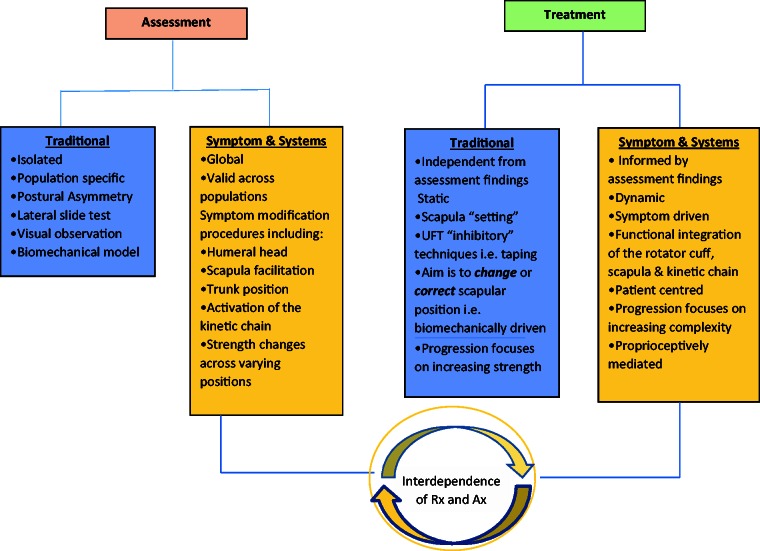
When interpreting assessment findings it is perhaps helpful to consider the process outlined in Fig. 2.
Figure 2.
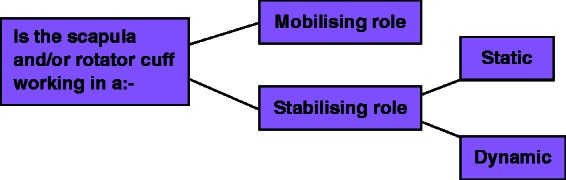
Assessment findings and treatment planning.
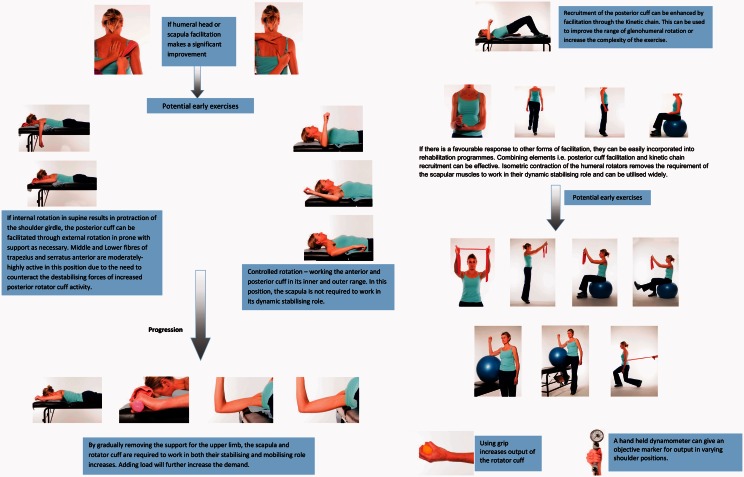
Given their interdependence, a thorough assessment of the rotator cuff should also be conducted (Fig. 3) to complement the scapula assessment.
Figure 3.
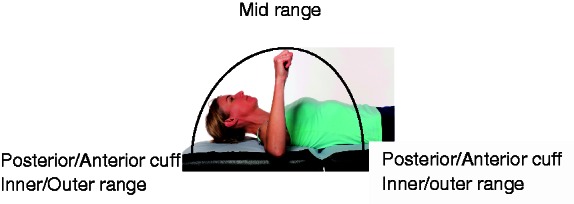
Through range assessment of the rotator cuff. The scapula is stabilized and therefore not working in its dynamic role.
If weakness of a portion of the rotator cuff is found, together with the findings from symptom modification tests, a clearer picture about where to start with rehabilitation may start to materialize. An example of this process is shown in Fig. 4.
Figure 4.
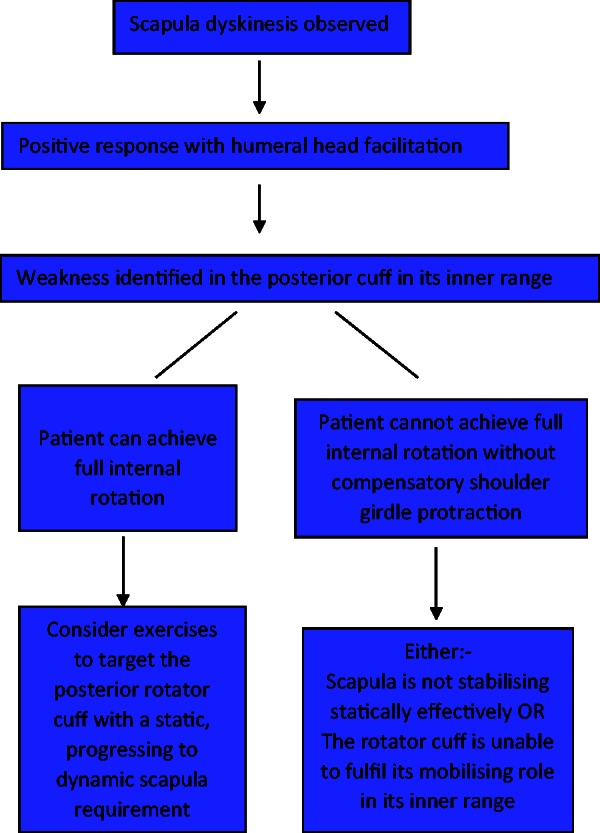
Assessment reasoning.
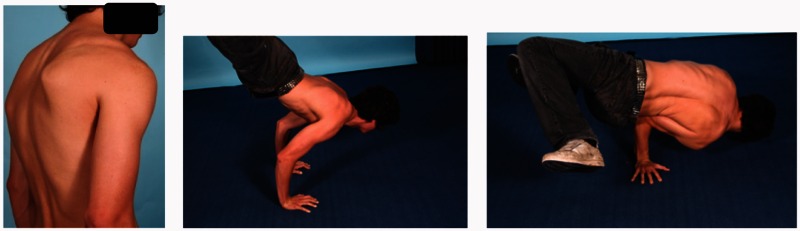
The kinetic chain elements of assessment should not be forgotten. Single leg standing or tip toe standing may not have resulted in the most significant change with symptom modification but they remain a significant part of the bigger picture. If the humeral contingent of the system is unable to perform a pattern of movement without the involvement of the scapular muscles, the scapula is unfairly implicated as the culprit when it is being utilized in an unconventional way in an attempt to maintain function. Similarly, the dyskinesis may not become apparent until the task becomes more complicated and involves co-ordination with the wider chain. Patients may also present differently in an open or closed chain position (Fig. 5). In either case, the observed result is faulty and inefficient motor patterns may be the cause, or equally the response, of pain and/or weakness elsewhere in the system.
Figure 7.
Scapular dyskinesis: traditional model versus a symptoms and systems-based approach.
Figure 5.
The dyskinesis of this breakdancer disappears with closed chain loading.
Rehabilitation: isolate or integrate?
The key to success with this approach to rehabilitation is having a sound appreciation of what the scapula and rotator cuff muscle groups are doing with each exercise, why they may or may not be beneficial, and how to adapt them if the patient is unable to perform them without compensatory movements or symptoms. With this knowledge and armed with some clinical reasoning, creativity and often trial and error, it should be possible to find at least one exercise that a patient can leave with, empowered by the knowledge that they can affect their own symptoms with movement.
As previously noted, it is difficult to justify a position of claiming that a patient is undergoing rotator cuff or scapula specific rehabilitation. To suggest that a particular exercise is purely a ‘scapula stability’ exercise may not only be difficult to substantiate based on the research evidence,32 but also is contradictory to the functional anatomy of the region. What one exercise may do more than another, however, is bias the exercise towards a situation where, for example, the scapula is only working in a static stabilizing, rather than a dynamic stabilizing role, where the former is generally considered an easier or less complex task.
The interdependence of the scapula, rotator cuff and kinetic chain requires clinicians to question the desirability of isolating one part of the system from the other. If the scapular and rotator cuff components are required to work together functionally, they should be trained as such. ‘Scapula specific rehabilitation’ may sound impressive but, unless you are engaged in an activity that does not involve any movement of the humerus, it is in all likelihood an unobtainable goal. Furthermore, it is also not possible to isolate single muscles within a single exercises. Even activities that demonstrate maximum activation do not do so to the exclusion of other muscles.33 These lessons have been learned and are well supported with multiple investigations into both exercise and the overwhelming number of supposed specific manual muscle tests that are proposed for the identification of specific shoulder pathology.34 Because it is almost impossible and generally undesirable to isolate individual muscles, the case for integration strengthens.
Linking assessment to rehabilitation
The flowchart in Fig. 4 illustrates how assessment findings may influence the clinicians decision-making process. The exercises pictured in Fig. 6 are not intended to be prescriptive but, instead, they illustrate how different exercises or progressions can influence the relative contributions from the scapula, rotator cuff and kinetic chain.
Figure 6.
Potential early exercises dependent on response to symptom modification.
Strength or motor control?
Over recent years, there have been a wealth of studies utilizing electromyographic (EMG) data.35–39 With such a plethora of such information now available in the literature, an unintended consequence of this may be that there has been an unwitting over emphasis on EMG output and equating it with strength. The traditional model of scapular assessment relies on increasing strength by progressing through a rainbow of theraband resistance and inhibitory techniques for supposed ‘over active’ muscles such as taping, trigger point release or massage. Exercise progression using a systems-based approach would instead focus not on biomechanically correcting the scapula position but, instead, on regaining and retraining the whole motor control pattern that had been identified through careful assessment, in terms of being problematic for that patient (Fig. 7).
Conclusions
A functioning proprioceptively mediated motor control system requires co-ordination, and therefore integration, of all the different body parts throughout the kinetic chain necessary for that particular movement pattern. For the shoulder, this will require assessment of the constituent parts working in both their agonist and stabilizer roles throughout full ranges of both concentric and eccentric phases of movement. It will also necessitate involvement of the wider kinetic chain to train relevant motor patterns that resemble the functional demands of the patient. In the early stages of rehabilitation, it may be necessary to limit the number of simultaneous functions that the patient is required to perform. Low load, unsupported shoulder rotation tasks can be used to train complex normal motor patterns; therefore, the early part of the motor pattern can be recruited and retrained in the appropriate manner. As rehabilitation progresses, the patient is challenged to maintain the correct motor pattern despite the increasing demand and complexity of the relevant task. This may involve elements of speed, co-ordination, load and specific functional requirements relevant to the individual, until a normal, fully functioning motor control pattern can be established and, crucially, reinforced with repetition. By utilizing the fundamental principles of motor learning and skill attainment with what is understood about proprioceptively mediated musculoskeletal rehabilitation, we can use our skills to their full potential. The coalescence of assessment and treatment techniques results in a symptoms and systems approach that is patient-centred and relevant to the functional requirements of the individual. We advocate that this has advantages over a traditional biomechanical model that utilizes assessment principles focused on minute differences in centimetres and degrees and deviations from a normal that arguably do not exist.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Sauers EL. Clinical evaluation of scapular dysfunction. Athl Ther Today 2006; 11: 10–4. [Google Scholar]
- 2.Codman EA. The shoulder. Rupture of the supraspinatus tendon and the lesions in or about the subacromial bursa, Boston, MA: Thomas Dodd Company, 1934. [Google Scholar]
- 3.Inman VT, Saunders JBDM, Abbott LC. Observations of the function of the shoulder joint. J Bone Joint Surg Am 1944; 26: 1–30. [Google Scholar]
- 4.Kirby K, Showalter C, Cook C. Assessment of the importance of glenohumeral peripheral mechanics by practicing physiotherapists. Physiother Res Int 2007; 12: 136–46. [DOI] [PubMed] [Google Scholar]
- 5.Nijs J, Roussel N, Vermeulen K, Struyf F, Mottram S, Meeusen R. Clinical assessment of scapular positioning in patients with shoulder pain: state of the art. J Man Manip Ther 2007; 30: 69–75. [DOI] [PubMed] [Google Scholar]
- 6.Morais NV, Pascoal AG. Scapular positioning assessment: is side to side comparison clinically acceptable? Manual Ther 2013; 18: 46–53. [DOI] [PubMed] [Google Scholar]
- 7.Oyama S, Myers JB, Wassinger CA, Ricci RD, Lephart SM. Asymetric resting position in healthy overhead athletes. J Athl Training 2008; 43: 565–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sugamoto K, Harada T, Machida A. Scapulohumeral rhythm: relationship between motion, velocity and rhythm. Clin Orthop 2002; 401: 119–24. [DOI] [PubMed] [Google Scholar]
- 9.Forte FC, de Castro MP, de Toledo JM, Ribiero DC, Loss JF. Scapular kinematics and scapulohumeral rhythm during resisted shoulder abduction – implications for clinical practice. Phys Ther Sport 2009; 10: 105–11. [DOI] [PubMed] [Google Scholar]
- 10.Braman JP, Engel SC, LaPrade RF, Ludewig PM. In vivo assessment of scapulohumeral rhythm during unconstrained overhead reaching in asymptomatic subjects. J Shoulder Elbow Surg 2009; 18: 960–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klopčar N, Lenarčič J. Bilateral and unilateral shoulder girdle kinematics during humeral elevation. Clin Biomech 2006; 21: S20–6. [DOI] [PubMed] [Google Scholar]
- 12.Koslow PA, Prosser LA, Strony GA, Suchecki SL, Mattingly GE. Specificity of the lateral scapular slide test: a reliability and validity study. Phys Ther 2003; 81: 799–809. [DOI] [PubMed] [Google Scholar]
- 13.Kibler WB. The role of the scapula in athletic function. Am J Sports Med 1998; 26: 325–37. [DOI] [PubMed] [Google Scholar]
- 14.Hayes K, Walton JR, Szomor ZL, Murrell GAC. Reliability of 5 methods for assessing shoulder range of motion. Aust J Physiother 2001; 47: 289–94. [DOI] [PubMed] [Google Scholar]
- 15.Nijs J, Roussel N, Vermeulen K, Souvereyns G. Scapular positioning in patients with shoulder pain: a study examining the reliability and clinical importance of 3 clinical tests. Arch Phys Med Rehabil 2005; 86: 1349–55. [DOI] [PubMed] [Google Scholar]
- 16.Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther 1999; 29: 574–86. [DOI] [PubMed] [Google Scholar]
- 17.Graichen H, Stammberger T, Bonél H, et al. Three dimensional analysis of shoulder girdle and supraspinatus motion patterns in patients with impingement syndrome. J Orthop Res 2001; 19: 1192–8. [DOI] [PubMed] [Google Scholar]
- 18.Kardua AR, Kerner PJ, Lazarus MD. Contact forces in the subacromial space: Effects of scapula orientation. J Shoulder Elbow Surg 2005; 14: 393–9. [DOI] [PubMed] [Google Scholar]
- 19.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Scapular position and orientation in throwing athletes. Am J Sports Med 2005; 33: 263–71. [DOI] [PubMed] [Google Scholar]
- 20.Laudner KG, Stanek JM, Meister K. Differences in scapular upward rotation between baseball pitchers and position players. Am J Sports Med 2007; 35: 2091–5. [DOI] [PubMed] [Google Scholar]
- 21.Kibler WB, Uhl TL, Jackson WQ, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg 2002; 11: 550–6. [DOI] [PubMed] [Google Scholar]
- 22.McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis. Part 1: Reliability. J Athl Training 2009; 44: 160–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tate AR, McClure PW, Kareha S, et al. A clinical method for identifying scapular dyskinesis. Part 2: validity. J Athl Training 2009; 44: 165–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uhl TL, Kibler WB, Gecewich B, et al. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy 2009; 25: 1240–8. [DOI] [PubMed] [Google Scholar]
- 25.McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement before and after a 6-week exercise programme. Phys Ther 2004; 84: 832–48. [PubMed] [Google Scholar]
- 26.Struyf F, Nijs J, Mollekens S, Jeurissen I, Truijen S, Mottram S, Meeusen R. Scapular-focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clin Rheumatol 2013; 32: 73–85. [DOI] [PubMed] [Google Scholar]
- 27.Roijen U, Clark NC, Treveleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Manual Ther 2015; 20: 368–377. [DOI] [PubMed] [Google Scholar]
- 28.Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment? Br J Sports Med 2009; 43: 259–64. [DOI] [PubMed] [Google Scholar]
- 29.Le Leu A, Alexander S, Higgs D, et al. The importance of scapula control in postero-inferior glenohumeral joint instability. In: Manning P (ed.) BESS annual scientific meeting, BESS. Nottingham, UK, 25--27 June 2014.
- 30.Boettcher CE, Cathers I, Ginn K. The role of shoulder muscles is task specific. J Sci Med Sport 2010; 13: 651–6. [DOI] [PubMed] [Google Scholar]
- 31.Ludewig PM, Cook TM. Alteration in scapula kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther 2000; 80: 276–91. [PubMed] [Google Scholar]
- 32.Wattanaprakomkul D, Halaki M, Boettcher C, Cathers I, Ginn K. The rotator cuff muscles have a direction specific recruitment pattern during flexion and extension exercises. J Sci Med Sport 2011; 14: 376–82. [DOI] [PubMed] [Google Scholar]
- 33.Boettcher C, Ginn K, Cathers I. The ‘empty can’ and ‘full can’ tests do not specifically activate supraspinatus. J Sci Med Sport 2009; 12: 435–9. [DOI] [PubMed] [Google Scholar]
- 34.Hegedus E, Goode A, Cambell S, et al. Physical examination tests of the shoulder: a systematic review with meta analysis of individual tests. Br J Sports Med 2008; 42: 80–92. [DOI] [PubMed] [Google Scholar]
- 35.Kibler WB, Sciascia AD, Uhl TL, et al. Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. Am J Sports Med 2008; 36: 1789–98. [DOI] [PubMed] [Google Scholar]
- 36.Decker MJ, Hintermeister RA, Faber KJ, et al. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med 1999; 27: 784–91. [DOI] [PubMed] [Google Scholar]
- 37.Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapula muscle balance: which exercises to prescribe? Am J Sports Med 2007; 35: 1744–51. [DOI] [PubMed] [Google Scholar]
- 38.De Mey K, Cagnie B, Danneels LA, et al. Trapezius muscle timing during selected shoulder rehabilitation exercises. J Orthop Sports Phys Ther 2009; 39: 743–52. [DOI] [PubMed] [Google Scholar]
- 39.Hardwick DH, Beebe JA, McDonnell MK, et al. A comparison of serratus anterior muscle activation during a wall slide exercise and other traditional exercises. J Orthop Sports Phys Ther 2006; 36: 903–10. [DOI] [PubMed] [Google Scholar]