Abstract
Background
Massive irreparable rotator cuff tears are a difficult problem. Modalities such as irrigation and debridement, partial repair, tendon transfer and grafts have been utilized with high failure rates and mixed results. Synthetic interpositional patch repairs are a novel and increasingly used approach. The present study aimed to examine the biomechanical properties of common synthetic materials for interpositional repairs in contrast to native tendon.
Methods
Six ovine tendons, six polytetrafluoroethylene (PTFE) felt sections and six expanded PTFE (ePTFE) patch sections were pulled-to-failure to analyze their biomechanical and material properties. Six direct tendon-to-bone surgical method repairs, six interpositional PTFE felt patch repairs and six interpositional ePTFE patch repairs were also constructed in ovine shoulders and pulled-to-failure to examine the biomechanical properties of each repair construct.
Results
Ovine tendon had higher load-to-failure (591 N) and had greater stiffness (108 N/mm) than either PTFE felt (296 N, 28 N/mm) or ePTFE patch sections (323 N, 34 N/mm). Both PTFE felt and ePTFE repair techniques required greater load-to-failure (225 N and 177 N, respectively) than direct tendon-to-bone surgical repairs (147 N) in ovine models.
Conclusions
Synthetic materials lacked several biomechanical properties, including strength and stiffness, compared to ovine tendon. Interpositional surgical repair models with these materials were significantly stronger than direct tendon-to-bone model repairs.
Keywords: biomechanics, interpositional patch, irreparable rotator cuff, ovine, PTFE patch, synthetic patch repair
Introduction
Massive rotator cuff tears have been a long-standing surgical dilemma. Repairs of larger and massive tears also fail more frequently with poorer clinical outcomes than smaller rotator cuff tears.1–3 Often massive tears, as a result of their degree of tendon retraction, atrophy or fatty infiltration, are considered irreparable.3,4
Many treatment solutions have been proposed to manage irreparable rotator cuff tears. Operative options have included arthroscopic irrigation and debridement with effective pain relief but little long term benefits in function.4–6 Tendon grafts including allografts, autografts and xenografts have been used in tendon reconstruction and bridging with mixed results and compatibility problems.7,8
Recently, the use of synthetic materials as an interpositional bridge between the retracted torn tendon and the humeral footprint has been proposed as method of repairing irreparable rotator cuff tears. Ozaki et al. performed interpositional synthetic patch repairs in 25 patients with gains in forward flexion and abduction range of motion and reductions in pain at an average 2.1-years follow-up.9 Audenaert et al. also showed improvements in flexion and abduction in 41 patients over a mean follow-up of 43 months following interpositional rotator cuff repair with Marsilene mesh.10 However, studies in synthetic patch rotator cuff repairs have reported complications, including re-tears.9,11 Visuri et al. also reported two instances of cystic degradation of the greater tuberosity following the use of a carbon fibre patch for rotator cuff repair.12
Several studies have described the technique and outcomes of interpositional synthetic patch rotator cuff tears,13–15 including a 10-year follow-up of five patients.16 However, no study has compared the biomechanical properties of synthetic materials to native tendon in an effort to identify the ideal material and material characteristics for use in interpositional synthetic patch repair.
The present study aimed to compare the biomechanical properties of synthetic materials used in interpositional patch repair with ovine tendon at the same time as comparing two different materials to assess ideal mechanical properties, such as strength and stiffness. The primary hypothesis was that BARD PTFE felt (CR BARD, Murray Hill, NJ, USA) would have comparable strength and stiffness to ovine tendon, both in isolated material and repair model testing, and also be superior to Gore-Tex ePTFE (Gore Medical, Flagstaff, AZ, USA) with regard to stiffness. This hypothesis was based on the preliminary in-house testing of BARD PTFE felt. The secondary hypothesis is that both BARD PTFE felt and Gore-Tex ePTFE patch repair method models would have superior failure load than the direct tendon-to-bone repairs.
Materials and methods
The present study involved biomechanical comparison of two synthetic materials (2.87-mm BARD PTFE felt, CR BARD; 2-mm Gore-Tex ePTFE fabric, Gore Medical) with isolated ovine tendon to investigate similarities and differences in biomechanical properties between common synthetic materials and ovine tendon. Biomechanical comparison of surgical repairs using interpositional patches (both BARD and Gore-Tex) with direct tendon-to-bone repair in ovine models was also completed. Ovine infraspinatus was chosen for its similarity to human supraspinatus tendon.17 Polytetrafluoroethylene (PTFE) felt and expanded PTFE (ePTFE) fabric were selected because these are the two materials that have been used in surgery by the senior author with good clinical outcomes.13,16
Material testing
Six isolated ovine infraspinatus, six BARD PTFE felt samples and six Gore-Tex PTFE samples were prepared for comparison of their biomechanical properties against the control ovine tendon.
Six ovine shoulders were dissected down to the infraspinatus, scapula and humerus. The infraspinatus was then dissected away from the posterior scapula and the infraspinatus tendon dissected from its humeral footprint with a No. 22 scalpel. The infraspinatus muscle belly was removed from the tendon, leaving just the infraspinatus tendon, which was trimmed to create a 50-mm strip of tendon. Each tendon was then frozen at −20℃ as in our previous model.14
The width and thickness of each 50-mm strip was measured with digital calipers. Twelve strips of PTFE patch material, six of Gore-Tex and six of BARD were then cut to 20 mm × 50 mm (i.e. length of 50 mm with an width equal to average tendon width to allow for comparison of the PTFE material properties with native tendon).
An additional twelve strips of patch material (six Gore-Tex and six BARD) were cut to 30 mm × 50 mm to give equal width to the patch material utilized in the surgical repair method testing (see Part 2) to allow comparison in properties between the isolated material properties and those of the surgical repair constructs.
Surgical repair method testing
Eighteen ovine shoulders were dissected to leave the humerus, infraspinatus and scapula. The infraspinatus was then separated from its insertion on the humerus creating a full-thickness tear. The thickness of each infraspinatus tendon was measured. The corresponding humeral footprint of each tendon was subsequently measured.
Each tendon was then cut across its full width medially to the footprint/insertion to simulate an ‘irreparable’ rotator cuff tear. It should be noted, however, that the tendon utilized here does not share the same atrophy, fatty infiltration and retraction as a true ‘irreparable’ tear. Three repair groups were formed by randomizing the eighteen shoulders; six ovine shoulders were utilized for direct tendon-to-bone repair (control group), six shoulders were used for synthetic patch repair with ePTFE patch (Gore-Tex) and six with a PTFE patch (BARD). It should be noted that direct tendon-to-bone repair reflects more closely a repair of a massive tear, as a true ‘irreparable tear’ would be unable to be directly repaired to the greater tuberosity.
Tendon-to-bone repair
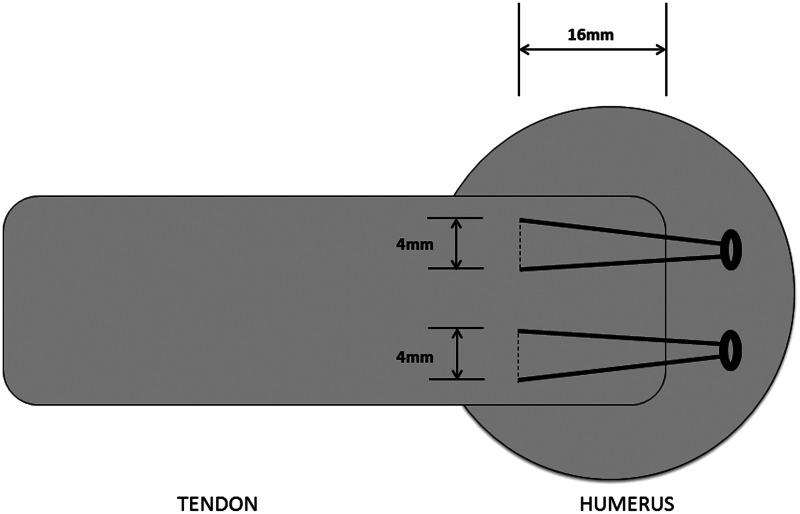
Two sutures (FibreWire; Arthrex, Naples, FL, USA) were passed through the medial infraspinatus tendon in an inverted mattress fashion (4 mm apart) using a suture passer (Scorpion; Arthrex), placing the suture 16 mm medial to the tendon edge.
Two holes were tapped in the corresponding humerus 5 mm lateral to the tendon footprint with a 4.7-mm SwiveLock punch (Arthrex). The free ends of the first suture were then passed through a SwiveLock (Arthrex) which was placed in the corresponding punched hole in the humerus and tapped into place before the sutures were tensioned until the torn tendon was mobilized to cover the footprint. The SwiveLock anchor was then screwed into the bone. The same process was then repeated for the second suture to complete the repair (Fig. 1).
Figure 1.
Direct tendon-to-bone repair method for the control group.
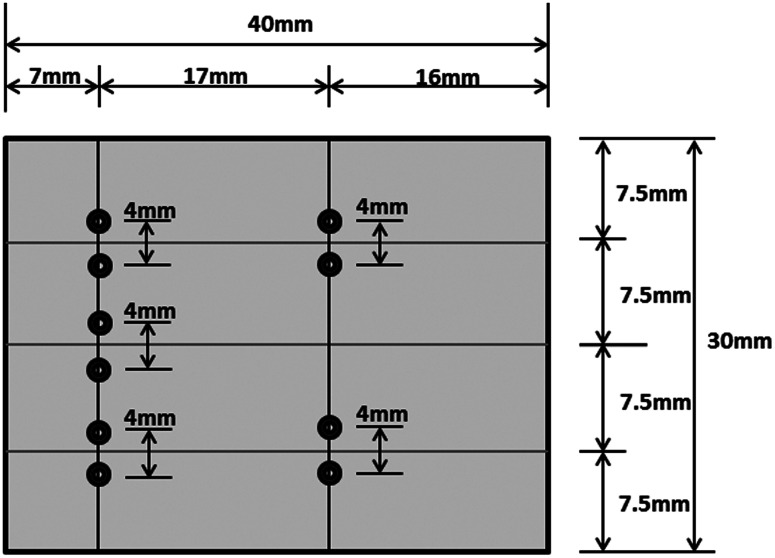
Patch fabrication
A template (Fig. 2) was made for the preparation of twelve synthetic patches to assure consistency. Six 2-mm ePTFE (Gore-Tex) patches were cut measuring 30 mm × 40 mm and ten guide holes made with a 3-0 tapered needle; six holes for tendon-to-patch fixation medially and four for patch-to-bone fixation distally, in accordance with the template. Six 2.87-mm PTFE felt (BARD) patches were then cut measuring the same dimensions, and prepared identically.
Figure 2.
Template used for preparation of expanded polytetrafluoroethylene (ePTFE) and polytetrafluoroethylene (PTFE) synthetic patches.
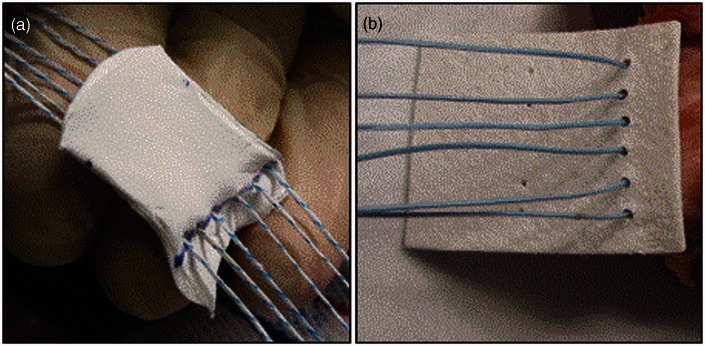
Patch repair
Synthetic patch rotator cuff repair was performed in twelve ovine shoulders; six with a PTFE felt patch and six with an ePTFE patch. The materials are shown in Fig. 3.
Figure 3.
(a) Expanded Polytetrafluoroethylene (ePTFE) patch (Gore-Tex) during surgical repair. (b) PTFE felt (BARD) patch during surgical repair.
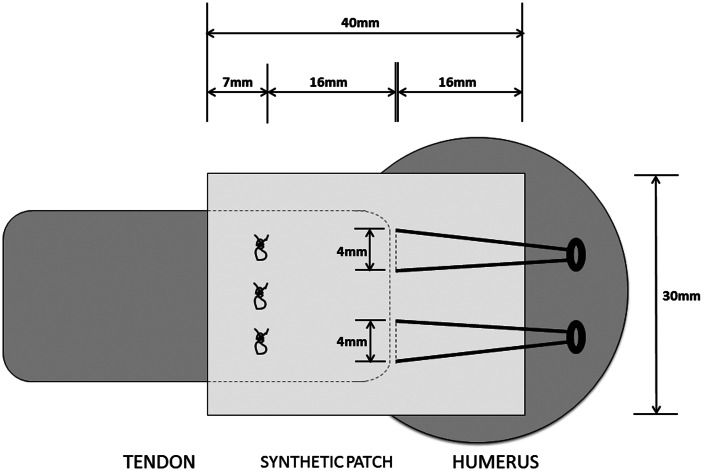
Three sutures (FibreWire) were passed in inverted mattress form (4 mm apart) using a Scorpion suture passer, placing the suture 16 mm medial to the tendon edge. Each of the six suture tails were then passed through previously formed corresponding holes (7 mm from the medial patch edge) in the synthetic patch using a snare. The two free tails of each of suture were then tied using an arthroscopic knot pusher with two standard sliding half-hitches followed by three alternating half-hitches for each of the three sutures.
Two sutures were then passed in an inverted mattress form with a Scorpion suture passer through the lateral end of the patch, previously marked (Fig. 2). Two holes were tapped in the corresponding humerus 5 mm lateral to the tendon footprint with a 4.7-mm SwiveLock punch. The free ends of the inferior patch suture were then passed through a SwiveLock anchor. The anchor was then placed in the inferior punched hole in the humerus and tapped into place before the sutures were tensioned to mobilize the patch over the tendon footprint before the SwiveLock was screwed into the bone. The same process was then repeated for the superior suture to complete the repair (Fig. 4). All repairs were then frozen at −20℃ before biomechanical testing.
Figure 4.
Synthetic interpositional patch repair method.
Biomechanical testing
The protocol used for testing was based on earlier investigations at our institute.18–20
Part 1: Material testing
The six infraspinatus tendons were thawed at room temperature in a moist gauze soaked in normal saline solution. The lateral 15 mm of the tendon was then clamped in a vice attached to the base of the testing machine (Instron 8874; Instron, Norwood, MA, USA). The medial 15 mm of the tendon was secured in a clamp attached to the functional column of the testing machine. Each tendon was preloaded with 10 N for 30 seconds; then pulled at 1.25 mm/seconds to failure, with the data captured at 100 Hz on a computer, as described previously by our institute.14,19,20
The same protocol was repeated for each of the two groups of six synthetic patches (six Gore-Tex and six BARD). Stiffness of the material was calculated from the linear section of the load-displacement curve using MATLAB software (R2007; The MathWorks, Natick, MA, USA). Material displacement was obtained from clamp-to-clamp displacement. The total energy-to-failure was calculated from the area under the load-displacement curve using trapezoid numerical integration with MATLAB (R2007).
Part 2: Surgical repair method testing
Specimens were thawed at room temperature and kept in a moist gauze soaked in a normal saline solution. The infraspinatus muscle was dissected away from the scapula. The infraspinatus tendon was isolated by scraping away the muscle mass using a scalpel. Each humerus was attached to a base plate with an 8-mm bolt, which, in turn, was secured to the base of the testing machine (Instron 8874).
The infraspinatus tendons were secured with tendon-grasping clamps that pulled perpendicular to the sagittal plane and parallel to the longitudinal axis of the tendon. The repairs were tested with the direction of pull 90° to the shaft of the humerus to simulate the position of the supraspinatus tendon when a patient’s arm is at his or her side. Again, the specimens were preloaded with 10 N for 30 seconds before the repaired tendon was pulled at 1.25 mm/second to failure. Modes of failure were recorded with a camera for each repair.
Statistical analysis
Sample size was set at six in accordance with a power calculation (α set at 0.05 and power equaling 0.80) which determined a minimum of four samples was required. Differences in load-to-failure, energy, stiffness and elongation were analyzed by one-way analysis of variance with correction for multiple comparisons with the Holm–Sidak method. p < 0.05 was considered statistically significant.
Results
Part 1: Material testing
All isolated tendons failed by intrasubstance shearing of tendon fibres. There was no evidence of tendon slipping during testing. Similarly, all isolated PTFE felt samples, measuring 20 mm × 50 mm, failed by intrasubstance tearing, with fibres tearing to leave a horizontal tear. All ePTFE patch samples, measuring 20 mm × 50 mm failed by stretching into a thin strand, the fibres of which ultimately tore. No slipping occurred during testing.
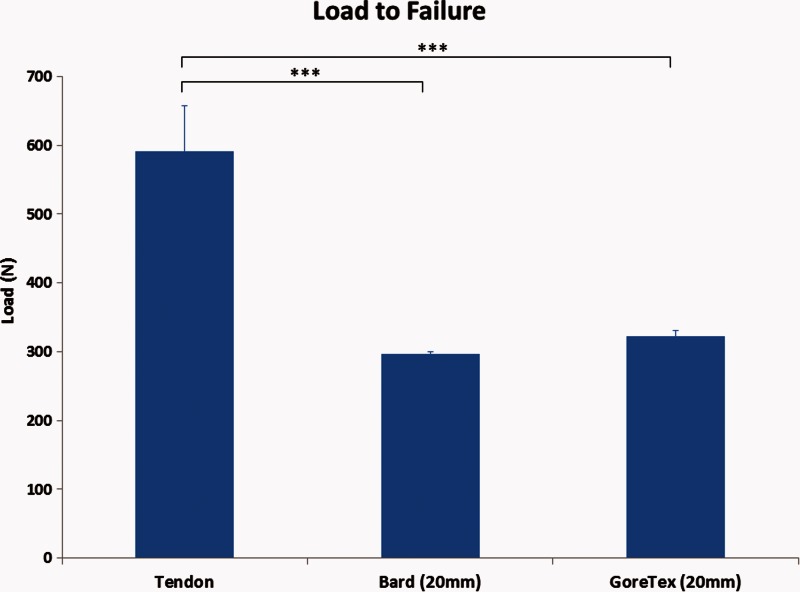
Isolated ovine tendon had a greater load-to-failure (591 ± 66 N) than either PTFE felt or ePTFE patch samples (p < 0.001) (Fig. 5), which had similar failure loads (296 ± 3.7 N and 322 ± 7.9 N, respectively). Similarly, ovine tendon was significantly stiffer (108 ± 16.9 N/mm) than either PTFE felt (28.1 ± 0.5 N/mm) or ePTFE patch (34.4 ± 2.6 N/mm) samples (p < 0.001).
Figure 5.
Material testing load-to-failure. ***p < 0.001 calculated using one-way analysis of variance with the Holm–Sidak multiple comparisons test.
The ePTFE patch had higher peak and total energy-to-failure (Table 1) compared to ovine tendon or PTFE felt (p < 0.0001), whereas ovine tendon and PTFE felt had a similar peak and total energy-to-failure.
Table 1.
Material testing.
| Ovine Tendon | BARD (20 mm × 50 mm) | Gore-Tex (20 mm × 50 mm) | Tendon versus BARD* | Tendon versus Gore-Tex* | BARD versus Gore-Tex* | |
|---|---|---|---|---|---|---|
| Load to Failure (N) | 591.3 ± 66.0 | 296.4 ± 3.7 | 322.6 ± 7.9 | p < 0.001 | p < 0.001 | NS |
| Peak Energy (Nm) | 2.1 ± 0.2 | 2.2 ± 0.1 | 6.9 ± 0.4 | NS | p < 0.0001 | p < 0.0001 |
| Total Energy (Nm) | 5.1 ± 0.7 | 4.6 ± 0.2 | 10.3 ± 0.7 | NS | p < 0.0001 | p < 0.0001 |
| Stiffness (N/mm) | 108.3 ± 16.9 | 28.1 ± 0.5 | 34.4 ± 2.6 | p < 0.001 | p < 0.001 | NS |
| Elongation (%) | 140 ± 4.0 | 184 ± 5.0 | 282 ± 0.1 | p < 0.01 | p < 0.0001 | p < 0.0001 |
Calculated using using one-way analysis of variance with the Holm–Sidak multiple comparisons test. NS, not significant. Data are the mean ± SD.
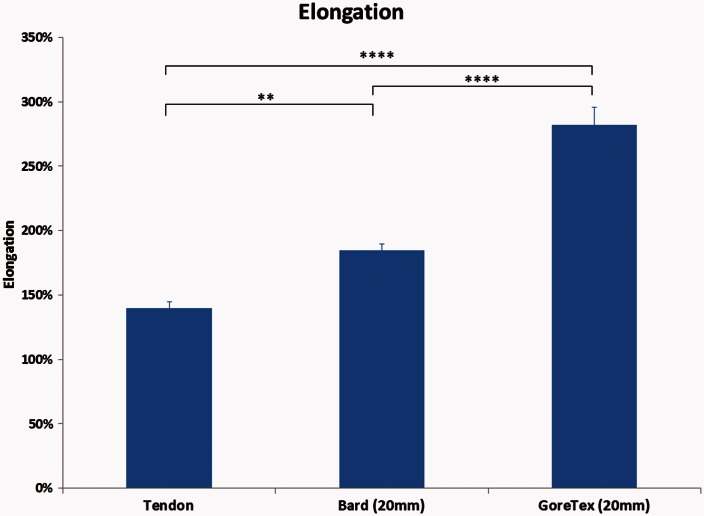
The ePTFE patch underwent significantly greater elongation (282 ± 0.1%) during testing than either ovine tendon (140 ± 4%) or PTFE felt (184 ± 5.0%), p < 0.0001). However, the PTFE felt also stretched more on average than ovine tendon (p < 0.01), with PTFE felt and tendon samples stretching an average of 1.8 and 1.4 times respectively (Fig. 6).
Figure 6.
Material testing elongation. **p < 0.01, ****p < 0.0001 calculated using one-way analysis of variance with the Holm–Sidak multiple comparisons test.
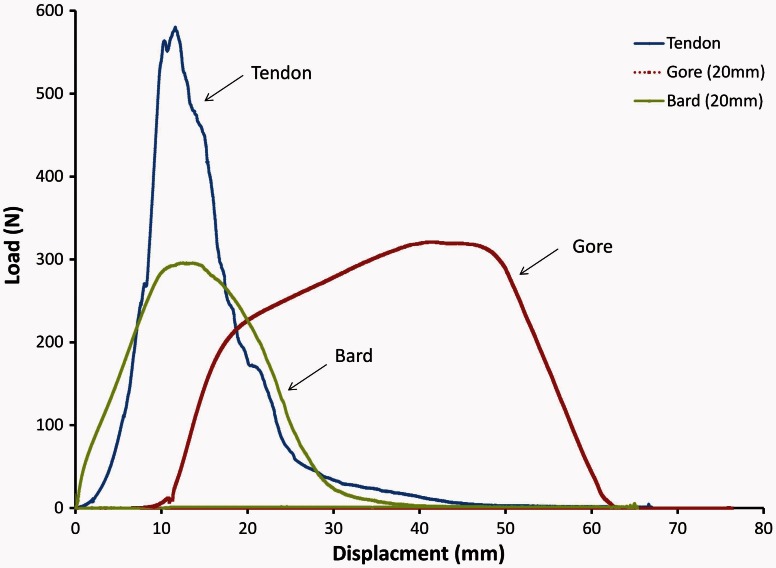
Comparison of three load-displacement curves (one ovine tendon test, one PTFE test and one ePTFE test) chosen from the specimens with the closest load-to-failure to the mean (Fig. 7) revealed that PTFE felt reached its peak load at a similar displacement to ovine tendon; however, its lower load-to-failure resulted in significantly lower stiffness than ovine tendon. On the other hand, ePTFE patches underwent significantly greater displacement than tendon and PTFE felt, requiring much greater energy-to-failure at the same time as undergoing greater deformity with a longer elastic deformation period.
Figure 7.
Load-displacement curves for ovine tendon, polytetrafluoroethylene (PTFE) (BARD) and expanded PTFE (ePTFE) (Gore-Tex) materials. Sample curves chosen from specimens with closest load-to-failure to the mean.
Part 2: Surgical repair method testing
No tendon slippage was observed during pull-to-failure testing. This was confirmed by checking the grip pattern of the tendon in the serrated clamp surface after testing. All six direct tendon-to-bone repairs failed by means of the sutures cutting through the tendon. Among the PTFE felt surgical repairs, three specimens failed by the suture pulling out of the anchor (50%), two failed by sutures pulling through at the patch to tendon interface (33%) and one failed by sutures cutting through the tendon in a button-hole manner (17%). Three ePTFE patch surgical repairs failed by sutures cutting through the tendon in a button-hole manner (50%), whereas the remaining three failed by sutures pulling through at the patch to tendon interface (50%).
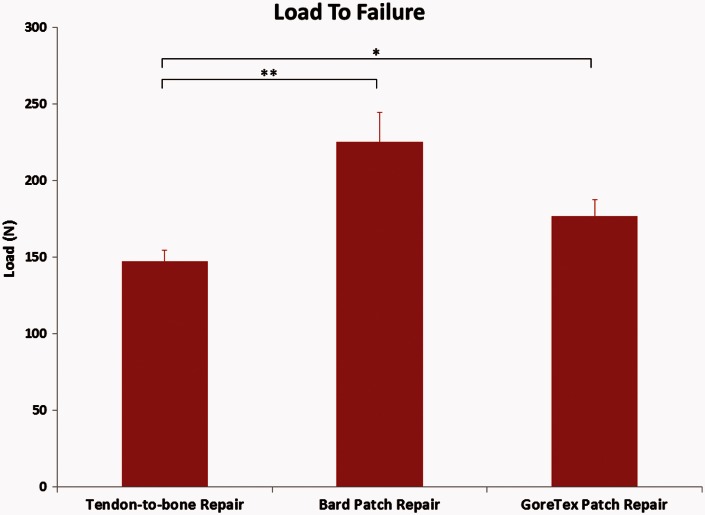
The direct tendon-to-bone repair method had lower load-to-failure (Fig. 8 and Table 2) (147 ± 7 N) than either the PTFE felt or ePTFE patch interpositional patch repair models (225 ±19 N and 177 ± 10 N, respectively) (p < 0.05).
Figure 8.
Surgical repair method testing load-to-failure. *p < 0.05, **p < 0.01 calculated using one-way analysis of variance with the Holm–Sidak multiple comparisons test.
Table 2.
Surgical repair method testing.
| Tendon- to-Bone Repair | BARD Patch Repair | Gore-Tex Patch Repair | Tendon-to-bone versus BARD Repair | Tendon-to-bone versus Gore-Tex Repair | BARD Repair versus Gore-Tex Repair | |
|---|---|---|---|---|---|---|
| Load-to-failure (N) | 147.2 ± 7.4 | 225.3 ± 19.2 | 176.9 ± 10.6 | p < 0.01 | p < 0.05 | NS |
| Peak energy (Nm) | 1.7 ± 0.5 | 3.1 ± 0.7 | 2.5 ± 0.7 | p < 0.01 | NS | NS |
| Total energy (Nm) | 2.6 ± 0.5 | 4.7 ± 0.8 | 3.1 ± 0.6 | p < 0.001 | NS | p < 0.01 |
| Stiffness (N/mm) | 15.4 ± 3.7 | 10.3 ± 2.8 | 10.4 ± 3.7 | p < 0.05 | p < 0.05 | NS |
Calculated using using one-way analysis of variance with the Holm–Sidak multiple comparisons test. NS, not significant. Data are the mean ± SD.
The interpositional repair with a PTFE felt patch required significantly more energy for failure than direct tendon-to-bone or ePTFE patch repairs (p < 0.01). Direct tendon-to-bone repair was significantly stiffer than either of the interpositional patch techniques (p < 0.05).
Comparison of interpositional patch repair models with results of material testing revealed that only a small percentage of the innate properties of the patch material translated to the characteristics of the patch repair model (Table 3). In the cases of load-to-failure, energy and stiffness, the isolated material was significantly greater in all compared to the respective surgical interpositional patch repair method (p < 0.0001). Specifically, the PTFE felt surgical repair method on average reached only 32% of the load-to-failure of the material (PTFE felt samples 30 mm × 50 mm). Similarly, ePTFE surgical repair method samples only reached 41% of the material average.
Table 3.
Biomechanical properties of individual synthetic patch materials (30 mm × 50 mm) compared with the biomechanical properties of their respective interpositional surgical repair model (calculated using an unpaired t-test).
| Load-to-failure | Peak energy | Total energy | Stiffness | |
|---|---|---|---|---|
| Bard (30 × 50) | 705.7 ± 13.9 | 5.6 ± 0.1 | 10.4 ± 0.3 | 51.7 ± 1.8 |
| Bard patch repair | 225.3 ± 19.2 | 3.1 ± 0.7 | 4.7 ± 0.8 | 10.3 ± 2.8 |
| Raw material versus patch repair | p < 0.0001 | p < 0.001 | p < 0.0001 | p < 0.0001 |
| 32% | 55% | 45% | 20% | |
| Gore (30 × 50) | 428.5 ± 17.9 | 10.9 ± 0.5 | 17.3 ± 0.9 | 38.3 ± 3.7 |
| Gore patch repair | 176.9 ± 10.6 | 2.5 ± 0.7 | 3.1 ± 0.6 | 10.4 ± 3.7 |
| Raw material versus patch repair | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.001 |
| 41% | 23% | 18% | 27% |
Discussion
The major finding of the present study was that synthetic patch rotator cuff repair, either with a PTFE felt or ePTFE patch, had a greater load-to-failure compared to direct tendon-to-bone repair in an ovine model.
Ovine tendon was significantly stronger than PTFE and ePTFE materials in isolated testing, requiring a much greater load for failure. Similarly, ovine tendon was stiffer compared to either synthetic material tested. Given that these materials were utilized as an interpositional bridge between the remaining rotator cuff tendon and the greater tuberosity, both stiffness and elongation are important considerations. A case can be made in favour of the PTFE felt over ePTFE in terms of elongation, with the ePTFE stretching and distorting significantly more during testing than PTFE felt. If the interpositioned material stretches, the tension in the repair will be lost and the remaining supraspinatus muscle fibres may have difficulty loading and abducting the humerus while concurrently stablising the humeral head against the glenoid fossa. Ultimately, comparison of the load-displacement curves revealed that, although both synthetic materials were weaker than tendon, by reaching its peak load with similar displacement to ovine tendon, PTFE felt shares more mechanical properties with ovine tendon than ePTFE patches.
A limitation of the present study was the modes of failure, with half of the PTFE felt surgical repair methods failing by means of anchor pull out, leaving the remaining tendon-patch constructs intact and, thus, not tested to their full potential. The innate differences between ovine and human shoulders is also a further limitation.
Shepherd et al.20 found, in ovine models, that synthetic patch repair with ePTFE provided greater footprint contact and pull-out strength than direct tendon-to-bone repairs when the repairs were performed either by mattress or the tension-band technique. Comparison of mattress and weave suturing techniques at the patch-to-tendon interface, as performed by Ronquillo et al.14 in an ovine model, found greater pull-out strength following mattress suture repair. Therefore, this technique was used in the present study. Clinical studies by our institute have also shown promising results with a 6-month follow-up of 16 patients;13 eight following weave suture technique and eight following a mattress suture technique at the patch-to-tendon interface found superior abduction strength following weave suturing technique repair. A long-term, 10-year clinical follow-up described healing at the patch-to-tendon interface in four of five patients (80%).16
The major finding of the present study was that interpositional patch repair with either PTFE felt or ePTFE patches had greater load-to-failure than direct tendon-to-bone repair in ovine models. Although no difference in stiffness between PTFE felt (BARD) and ePTFE patch (Gore-Tex) was observed in either material or surgical repair method testing, the significantly greater elongation of Gore-Tex may be a concern when attempting a successful and durable patch repair in a surgical setting. Finally, comparison of isolated material testing with the surgical patch repair models revealed that differences in individual material characteristics are poorly preserved in a surgical repair, with lower load-to-failure and less stiffness, suggesting that the integrity of the tendon-to-patch interface, the suture-anchor system and the patch-to-bone interface may be more important than the patch material used.
Acknowledgements
We would like to thanks Arthrex Inc. for providing the suture-anchors, as well as W.L Gore and Associates and BARD for providing the synthetic patches.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg 2004; 86A: 219–24. [DOI] [PubMed] [Google Scholar]
- 2.Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. J Bone Joint Surg (Am) 2009; 18: 808–18. [DOI] [PubMed] [Google Scholar]
- 3.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg (Am) 2000; 82A: 505–15. [DOI] [PubMed] [Google Scholar]
- 4.Khair MM, Gulotta LV. Treatment of irreparable rotator cuff tears. Curr Rev Musculoskelet Med 2011; 4: 208–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rockwood CA, Jr, Williams GR, Jr, Burkhead WZ., Jr Debridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg (Am) 1995; 77: 857–66. [DOI] [PubMed] [Google Scholar]
- 6.Dines DM, Moynihan DP, Dines J, McCann P. Irreparable rotator cuff tears: what to do and when to do it; the surgeon's dilemma. J Bone Joint Surg (Am) 2006; 88: 2294–302. [DOI] [PubMed] [Google Scholar]
- 7.Moore DR, Cain EL, Schwartz ML, Clancy WG., Jr Allograft reconstruction for massive, irreparable rotator cuff tears. Am J Sports Med 2006; 34: 392–6. [DOI] [PubMed] [Google Scholar]
- 8.Warner JJ. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instructional Course Lectures 2001; 50: 63–71. [PubMed] [Google Scholar]
- 9.Ozaki J, Fujimoto S, Masuhara K, Tamai S, Yoshimoto S. Reconstruction of chronic massive rotator cuff tears with synthetic materials. Clin Orthop 1986:173–83. [PubMed]
- 10.Audenaert E, Van Nuffel J, Schepens A, Verhelst M, Verdonk R. Reconstruction of massive rotator cuff lesions with a synthetic interposition graft: a prospective study of 41 patients. Knee Surg Sports TR A 2006; 14: 360–4. [DOI] [PubMed] [Google Scholar]
- 11.Hirooka A, Yoneda M, Wakaitani S, et al. Augmentation with a Gore-Tex patch for repair of large rotator cuff tears that cannot be sutured. J Orthop Sci 2002; 7: 451–6. [DOI] [PubMed] [Google Scholar]
- 12.Visuri T, Kiviluoto O, Eskelin M. Carbon fiber for repair of the rotator cuff. A 4-year follow-up of 14 cases. Acta Orthop Scand 1991; 62: 356–9. [DOI] [PubMed] [Google Scholar]
- 13.Ronquillo JC, FPOA M, Lam P, Murrell GA. Arthroscopic ePTFE patch repair for irreparable rotator cuff tears: part II: preliminary clinical results. Tech Should Elb Surg 2013; 14: 33–41. [Google Scholar]
- 14.Ronquillo J, Lam P, Murrell AGC. Arthroscopic ePTFE patch repair for irreparable rotator cuff tears. Part I: surgical technique and biomechanical comparison of 2-suture techniques at the patch to tendon interface. Tech Should Elb Surg 2013; 14: 29–32. [Google Scholar]
- 15.Shepherd H, Murrell GAC. Use of synthetic patches as tendon substitutes in knotless arthroscopic repairs of massive rotator cuff tears. Tech Should Elb Surg 2012; 13: 32–5. [Google Scholar]
- 16.Shepherd H, Murrell GAC. Synthetic patch rotator cuff repair – a 10-year follow-up. Shoulder Elbow 2011; doi: 10.1111/sae.12046. [DOI] [PMC free article] [PubMed]
- 17.Gerber C, Schneeberger AG, Beck M, Schlegel U. Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg (Br) 1994; 76: 371–80. [PubMed] [Google Scholar]
- 18.Andres BM, Lam PH, Murrell GAC. Tension, abduction and surgical technique effect footprint compression following rotator cuff repair in an ovine model. J Shoulder Elbow Surg (Am) 2010; 19: 1018–27. [DOI] [PubMed] [Google Scholar]
- 19.Peters KS, Lam PH, Murrell GAC. Repair of partial-thickness rotator cuff tears: a biomechanical analysis of footprint contact pressure and strength in an ovine model. Arthroscopy 2010; 26: 877–44. [DOI] [PubMed] [Google Scholar]
- 20.Shepherd HM, Lam P, Murrell GAC. Biomechanics of synthetic patch rotator cuff repairs. Tech Should Elb Surg 2011; 12: 94–100. [Google Scholar]