Abstract
Background
Rotator cuff repair aims to reattach the torn tendon to the greater tuberosity footprint with suture anchors. The present study aimed to assess the diagnostic accuracy of ultrasound in predicting rotator cuff tear repairability and to assess which sonographic and pre-operative features are strongest in predicting repairability.
Methods
The study was a retrospective analysis of measurements made prospectively in a cohort of 373 patients who had ultrasounds of their shoulder and underwent rotator cuff repair. Measurements of rotator cuff tear size and muscle atrophy were made pre-operatively by ultrasound to enable prediction of rotator cuff repairability. Tears were classified following ultrasound as repairable or irreparable, and were correlated with intra-operative repairability.
Results
Ultrasound assessment of rotator cuff tear repairability has a sensitivity of 86% (p < 0.0001) and a specificity of 67% (p < 0.0001). The strongest predictors of rotator cuff repairability were tear size (p < 0.001) and age (p = 0.004). Sonographic assessments of tear size ≥4 cm2 or anteroposterior tear length ≥25 mm indicated an irreparable rotator cuff tear.
Conclusions
Ultrasound assessment is accurate in predicting rotator cuff tear repairability. Tear size or anteroposterior tear length and age were the best predictors of repairability.
Keywords: diagnostic imaging, irreparable, repairability, rotator cuff tear, surgery, ultrasound
Introduction
Rotator cuff tears are a common cause of shoulder discomfort and dysfunction. Full-thickness rotator cuff tears often need surgical repair, with the aim of restoring the normal anatomy of the rotator cuff and returning the shoulder to normal function and comfort. The main aim is to reattach the torn tendon to the greater tuberosity footprint (primary repair). However, primary repair of a rotator cuff tear may not be possible if the tendon tear is very large, atrophied, retracted and/or immobile. It is in the interest of both the patients and surgeons to have optimum pre-operative imaging to determine rotator cuff tear repairability.
Massive tears with defects that cannot be completely reattached, severe fatty atrophy of the supraspinatus muscle1–6 and superior humeral head migration7–11 are indicators of irreparability. In our shoulder service, if the standard primary repair method is not feasible yet a tendon edge will accept sutures, the tear is treated with a synthetic interposition graft using Gore-Tex expanded polytetrafluoroethylene (ePTFE) patch (WL Gore and Associates, Inc., Flagstaff, AZ, USA). Without a tendon edge, or with a very poor quality edge, the rotator cuff dysfunction is often managed with a reverse total shoulder arthroplasty (e.g. Aequalis reversed shoulder prosthesis, Tornier, Inc., St Ismeir, France).
Traditionally, magnetic resonance imaging (MRI) has been the gold standard in the assessment of rotator cuff tears for determining repairability and to indicate the most suitable repair method. A few studies have investigated the pre-operative MRI variables that influence the choice of reconstruction technique.12–15
Tear size has been found to be an important determinant of rotator cuff tear repairability. Ultrasound is accurate in assessing the location, size, retraction and extent of full-thickness rotator cuff tears.16–31 Studies have shown ultrasound accuracy is comparable to that of MRI in detecting rotator cuff tears and determining tear characteristics20,30 (e.g. for assessing rotator cuff muscle atrophy).32–34 Ultrasound assessment of rotator cuff fatty atrophy is moderately to strongly accurate, correlating well with MRI and surgical assessment. To our knowledge, there has yet to be a study that investigates the capacity of ultrasound for determining rotator cuff tear repairability.
The present study aimed to assess how accurately ultrasound determines feasibility for primary repair of a rotator cuff tear. The secondary aim was to determine which pre-operative features are most important for predicting whether the tear is repairable.
Materials and methods
Ethics approval for this study was granted by the South Eastern Sydney Local Health District – Southern Sector Human Research Ethics Committee (IRB approval number: LNR/11/STG/221). This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The study is a retrospective analysis of measurements made prospectively in a cohort of 368 patients who had ultrasounds of their shoulder(s) carried out by a single sonographer, who subsequently came to surgery performed by a single surgeon and met the study’s inclusion criteria.
Patients were included in this study if they had a full-thickness rotator cuff tear determined by pre-operative ultrasound and were excluded if they had a partial-thickness or intrasubstance rotator cuff tear, prior rotator cuff repair, prior shoulder arthroplasty or a concurrent procedure (e.g. debridement of calcific tendinitis) with the rotator cuff repair.
Ultrasound
A highly qualified ultrasonographer (LH), with 20 years of experience in musculoskeletal ultrasound and 6 years of specialized experience in shoulder ultrasound, performed pre-operative ultrasounds using a General Electric Logiq E9 instrument (General Electric, Milwaukee, WI, USA) with a Linear ML 6–15 MHz transducer with a 50 × 10 mm footprint.
The ultrasound scan followed a standard procedure35 with the patient seated in an upright position. The elbow of the shoulder being examined was flexed at 90° and the supraspinatus tendon was examined in transverse and longitudinal planes. With the probe in the transverse plane, the supraspinatus tendon was observed from the bicipital groove through to the acromion as the humeral head was brought anterior to the acromion by extending the arm. The probe was then adjusted to the longitudinal plane and the insertion of the supraspinatus tendon at the greater tuberosity was assessed with the patient extending his/her arm. Full-thickness tears were identified as areas of decreased echogenicity and flattening over the humeral head. A flat insertion site or bare humeral head with no observable tendon indicated a retracted full-thickness tear. Partial tendon tears were identified by hypoechoic disruptions within the tendon fibres. The sonographer measured and mapped the size, morphology and percentage thickness of the rotator cuff tear on a purpose-designed form.
The probe was placed over the acromioclavicular joint in the transverse plane and dropped back posteriorly over the trapezius muscle to identify the supraspinatus muscle belly. Fatty atrophy of the supraspinatus muscle was demonstrated by poor definition and heterogeneous echotexture of the supraspinatus muscle belly. The sonographer graded and recorded the muscle belly as normal or with mild, moderate or severe muscle atrophy as per Khoury et al.32
Integrity of the subscapularis, infraspinatus and biceps brachii long head tendons was also assessed during ultrasound examination and recorded in the report. The insertion of the subscapularis tendon into the lesser tubercle was observed in transverse and longitudinal planes with the patient still sitting upright. Assessment of the infraspinatus tendon required repositioning of the patient. The patient’s arm was extended across the chest with the ipsilateral hand resting on the contralateral arm or shoulder. The tendon was viewed with the probe placed slightly obliquely. Assessment of the biceps brachii long head tendon was performed after identifying its proximal entrance to the bicipital groove. Thereafter, the tendon was viewed from the transverse and longitudinal planes to identify tendon pathology.
The surgeon assessed, on the basis of sonographic and clinical findings, whether the supraspinatus tear was either repairable by primary repair, or required primary repair with an ePTFE patch or reverse shoulder arthroplasty. Rotator cuff tears were assessed to be repairable or irreparable with primary repair.
Guidelines for sonographic determination of pre-operative repairability were as follows. Primary repair was suggested if tear size was less than 25 mm anteroposteriorly and the muscle belly was normal. If the tear exceeded 25 mm in anteroposterior length, or the tendon was retracted to the glenoid by 25 mm to 30 mm and the muscle belly was normal, the tear was predicted to be irreparable.
Surgical assessment
Patients were positioned in the upright beach-chair configuration under interscalene block and sedation. A posterior portal was created as a viewing portal while a lateral portal was established as a working portal for rotator cuff repair. The rotator cuff and biceps brachii were visually examined from the articular side. The rotator cuff tear was measured from anterior to posterior and from medial to lateral directions with an instrument of known dimensions as a reference (e.g. a 5 mm shaver).
At surgery, defect size and the most appropriate repair method were assessed and recorded by the surgeon. Rotator cuffs that were predicted to have primary repair ± patch graft were assessed during surgery and final judgement was made whether to proceed with primary repair ± patch graft or to elect reverse shoulder arthroplasty. Patients who were predicted pre-operatively to require reverse shoulder arthroplasty had their rotator cuff assessed intra-operatively. At this point, a decision was made over whether to proceed with a reverse shoulder replacement or if the rotator cuff tear was amenable to primary repair ± patch graft.
The repair method utilized was recorded on the operative report either as complete reattachment of the tendon to the greater tuberosity, partial reattachment with a remaining defect, reconstruction with an ePTFE patch or reverse shoulder arthroplasty. If the tear was reconstructed with complete reattachment of the torn tendon to the greater tuberosity, the rotator cuff tear was classified as repairable.
Statistical analysis
Sonographic and intra-operative tear size dimensions (anteroposterior, mediolateral and area) were compared with Pearson’s correlation coefficient (r) to assess the ultrasound accuracy for quantifying tear size. Likelihood ratios, sensitivities and specificities for ultrasound prediction of rotator cuff repairability were calculated with chi-squared tests using the Yates correction factor. The strength of relationships between sonographic findings and operative repairability were assessed with Spearman’s (nonparametric) correlation coefficient (rs). This test was also used to compare assessments of ultrasound-determined muscle atrophy grades (normal, mild, moderate or severe) with final repairability.
Regression analyses were performed with repairability as the dependent variable and pre-operative tear size, muscle atrophy and age as the independent variables. The purpose was to predict which of these variables are important for repairability. Analyses were carried out on SPSS, version 20 (SPSS Inc., Chicago, IL, USA).
Results
Study cohort
Between May 2009 to June 2012, 1012 patients underwent rotator cuff repair or reverse shoulder arthroplasty by a single surgeon. Additional procedures were performed concurrently with 104 rotator cuff repairs. Of the cases, 91 had revision rotator cuff surgery, 168 cases lacked a pre-operative ultrasound examination by our sonographer. Two hundred and seventy-six were assessed as partial-thickness or intrasubstance tears at pre-operative ultrasound and a total of 639 rotator cuff repairs were thus excluded from the study, leaving 373 cases that met the inclusion criteria.
Patient demographics
The study included 216 males and 152 females, involving 146 left shoulders, 217 right shoulders and 10 shoulders from five bilateral cases (Table 1). Their age range was 30 years to 90 years and the mean (SD) age was 61 (11) years.
Table 1.
Patient demographics and ultrasound repair groups.
| Total sample | Primary repair | ePTFE patch repair | |
|---|---|---|---|
| Male: female | 216:152 | 167:126 | 49:24 |
| Age at surgery (years), mean (SD) (range) | 62 (11) (30–90) | 61 (11) (30–90) | 68 (9) (46–88) |
| Affected shoulder L: R | 151:222 | 124:169 | 23:50 |
At ultrasound, 293 tears of the supraspinatus tendon were assessed as appropriate for primary repair, 73 were recommended for possible repair with the ePTFE patch and seven for reverse shoulder arthroplasty. At surgery, 321 of these cases proceeded with primary repair, 18 cases involved primary repairs with a remaining defect, 27 repairs utilized an ePTFE patch and seven shoulders were managed with reverse shoulder arthroplasty.
Ultrasound prediction of repairability and the most suitable repair method
The current study found that ultrasound prediction of repair method, correlated positively with the method the surgeon intra-operatively deemed to be the most suitable (r = 0.4, p < 0.0001). Sonographic prediction of rotator cuff tears requiring reverse shoulder arthroplasty correlated strongly with the final repair method (r = 0.9, p < 0.0001).
Our study showed 321/373 (87%) rotator cuff tears were repairable by suture anchors and 52/373 (13%) were deemed as irreparable at surgery. Ultrasound assessment of rotator cuff repairability was very good in predicting these outcomes [positive likelihood ratio: 2.6 (95% confidence interval = 1.81 to 4.10); sensitivity: 0.86 (95% confidence interval = 0.84 to 0.87); specificity: 0.67 (95% confidence interval = 0.52 to 0.79) (p < 0.0001)].
In cases that were predicted to be and were finally classified as irreparable, ultrasound predicted that 22 cases could be repaired by patches and seven with reverse shoulder arthroplasty. Twenty-one of the 22 (95%) proceeded with the predicted procedure and one required a reverse shoulder replacement. Six of the seven (86%) shoulders that were recommended for reverse shoulder arthroplasty proceeded as predicted whilst one shoulder had complete primary repair. Ultrasound prediction of patch repair or reverse shoulder arthroplasty of irreparable tears was highly accurate [positive likelihood ratio: 6.7 (95% confidence interval = 1.6 to 78.7); sensitivity: 0.96 (95% confidence interval = 0.84 to 1.0); specificity: 0.86 (95% confidence interval = 0.49 to 0.99) (p < 0.0001)].
In eight of 80 (10%) cases where irreparable tears were diagnosed by the sonographer, the surgeon attempted primary repair with suture anchors. However, as a result of the large tear size, a small defect remained.
Regression analyses and predictive formula
Stepwise regression analysis revealed that tear size, either expressed as area or anteroposterior length, and age, are significant variables for rotator cuff tear repairability. Table 2 lists the p values for these and other variables tested with stepwise regression. As can be seen, muscle quality (including fatty atrophy) was insignificant in this study, probably due to the small number of cases affected in this way.
Table 2.
Stepwise regression analysis of significance (p values) for pre-operative variables on rotator cuff tear repairability.
| Variable | p value | |
|---|---|---|
| 1 | Tear size (cm2) | <0.001 |
| 2 | Alternatively anteroposterior tear length (mm) | <0.001 |
| 3 | Mediolateral tear length | 0.18 |
| 4 | Patient age | 0.004 |
| 5 | Patient gender | 0.348 |
| 6 | Muscle quality | 0.58 |
Multiple logistic analyses were performed in two ways, either with area and age or anteroposterior length and age as independent variables with repairability as the dependent variable.
For the first example, the multiple logistic equation is:
For the second example, the multiple logistic equation is:
If the logit p for either of these equations is 0.5 or more, the tear is likely to be repairable.
Ultrasound and surgical assessments of tear size
Anteroposterior dimension
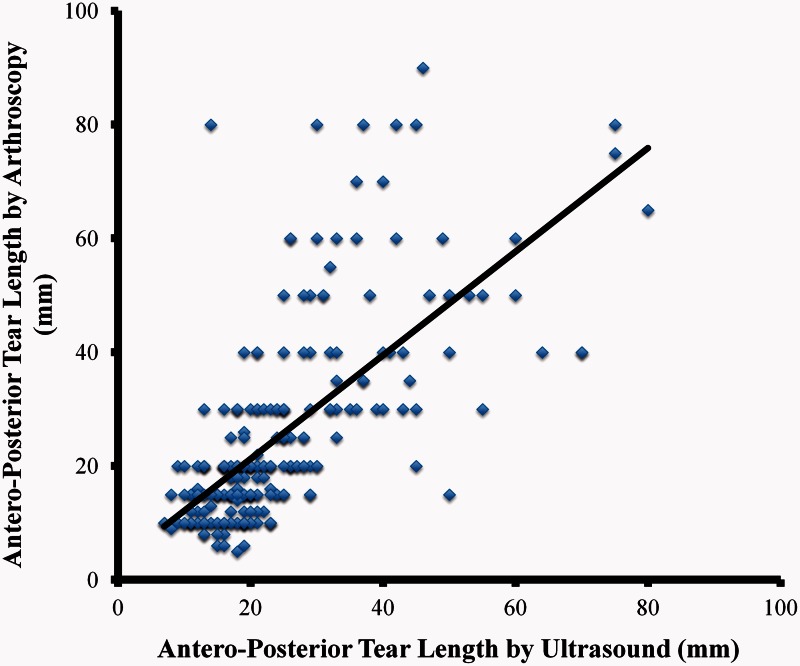
The mean (SD) anteroposterior length of the rotator cuff tears at ultrasound was 23 (12) mm, with a range of 6 mm to 80 mm. The mean (SD) anteroposterior tear length was assessed intra-operatively as 23 (16) mm with a range of 5 mm to 90 mm. The post-hoc anteroposterior cut-off for repairability was determined as the measurement at which at least 80% of irreparable rotator cuff tears exceeded. An ultrasound determined anteroposterior tear length of 25 mm was considered the cut-off threshold for a repairable rotator cuff tear, given that 81% (42/59) of irreparable tears exceeded 25 mm and 10 (19%) were less than 25 mm. Tears ≥25 mm in anteroposterior tear length were associated with being irreparable (p < 0.0001). Ultrasound and surgical assessments of anteroposterior dimensions of rotator cuff tears (Fig. 1) showed strong correlation (r = 0.71, p < 0.0001).
Figure 1.
Correlation of ultrasound and arthroscopic assessments of anteroposterior tear length (r = 0.71, p < 0.0001).
Mediolateral dimension
The mean (SD) sonographic mediolateral measurement for rotator cuff tears was 22 (12) mm, ranging from 5 mm to 80 mm, and the surgical mean (SD) was 21 (13) mm, also ranging from 5 mm to 80 mm. The post-hoc mediolateral threshold for repairability was determined as the measurement at which at least 80% of irreparable rotator cuff tears exceeded. A mediolateral tear length of 21 mm measured with ultrasound, was considered the cut-off threshold for rotator cuff tear repairability, which 81% (42/52) of irreparable tears exceeded. Tears ≥21 mm in mediolateral tear length were associated with being irreparable (p < 0.0001). The sonographic and operative mediolateral measurements of the tendon tear also showed strong correlation (r = 0.73, p < 0.0001).
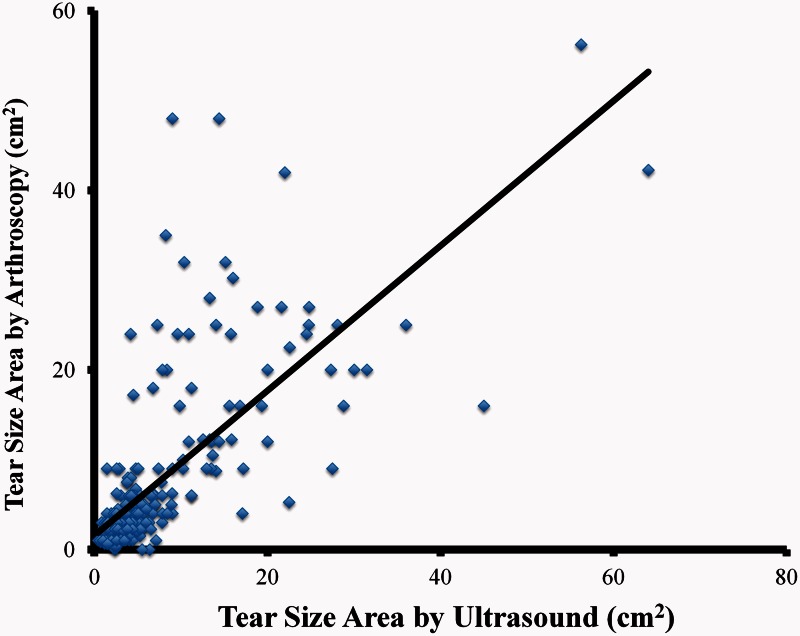
Tear size area
The mean (SD) sonographic tear size area was estimated to be 6.2 (7.9) cm2 with a range of 0.4 cm2 to 64 cm2. Mean (SD) tear size measured at surgery was 6.4 (8.8) mm2, ranging from 0.3 mm2 to 56.3 mm2. The post-hoc threshold cut-off for repairability was determined as the tear size area measurement at which at least 80% of actual irreparable rotator cuff tears exceeded. A tear size of 4 cm2 measured with ultrasound, was considered the cut-off threshold for rotator cuff tear repairability, which 83% (43/52) of irreparable tears exceeded. Tears ≥4 cm2 were associated with being irreparable (p < 0.0001). Sonographic and arthroscopic assessments for tear size area (Fig. 2) correlated well (r = 0.70, p < 0.0001).
Figure 2.
Correlation of ultrasound and arthroscopic assessments of tear size (r = 0.73, p < 0.0001).
Sonographic assessment of tear size and repairability
The mean (SD) anteroposterior tear length of rotator cuff tears as assessed by ultrasound was 21 (10) mm in the repairable group and 36 (15) mm in the irreparable group, revealing significantly longer tears in the irreparable group (p < 0.0001, unpaired t-test). The mean (SD) mediolateral tear length was 19 (10) mm in the repairable group and 34 (14) mm in the irreparable group, revealing significantly larger tears in the irreparable group (p < 0.0001).
Ultrasound assessment of muscle atrophy and repair method
Ultrasound assessment of muscle atrophy revealed 321 (90%) normal shoulders, 30 (8%) with mild atrophy, 5 (2%) with moderate atrophy and none (0%) with severe atrophy. Seventeen ultrasound reports lacked the muscle atrophy assessment record and were excluded from analysis. The grade of muscle atrophy determined at pre-operative ultrasound correlated with rotator cuff tear repairability (rs = 0.28, p < 0.001).
Discussion
The present study shows that ultrasonography can predict whether rotator cuff tears are likely to require primary repair, patch repair or reverse shoulder arthroplasty with a high degree of accuracy in the hands of an experienced ultrasonographer.
As noted above, MRI has been the gold standard in rotator cuff tear assessment. A few studies have evaluated MRI and imaging variables to assess the feasibility of complete primary repair of rotator cuff tears. Sugihara et al.13 found tears equal to or exceeding 40 mm both anteroposteriorly and mediolaterally, with thinning of the supraspinatus muscle (<5 mm) at the superior margin of the glenoid and fatty degeneration of the infraspinatus muscle on MRI, were likely to be unfeasible for primary repair. Their MRI study has neither assessed reliability of these variables for predicting feasibility for primary repair, nor compared their imaging assessment with surgical assessment. Moreover, their study has a much smaller cohort (n = 27) than ours and involved open rotator cuff repair, whereas the present study is based primarily on arthroscopic repair.
Yoo et al.14 found the most significant parameters on MRI indicative of an irreparable tear were sagittal and coronal oblique distances greater than 32 mm and 31 mm, respectively, and a fatty degenerative index score greater than 3 and 2 for the supraspinatus and infraspinatus muscles on sagittal and coronal oblique sections, respectively. However, the present study found fatty atrophy of the supraspinatus muscle plays a minimal role in predicting rotator cuff repairability.
Our findings for tear size in predicting repairability are most consistent with a study by Davidson et al.12 Their study was the only one to assess the accuracy of MRI prediction of repairability. They found tears equal to or greater than 20 mm in length (coronal section) and width (sagittal section) on MRI were likely to be irreparable. They found an MRI of a rotator cuff tear showing mediolateral length less or equal to anteroposterior length and less than 20 mm to have an accuracy of 98%, 100% sensitivity and 98% specificity in predicting a complete primary repair. MRI had an accuracy of 93%, a sensitivity of 85% and a specificity of 100% in predicting side-to-side/margin convergence repair when MRI showed anteroposterior dimensions smaller than mediolateral length and less than 20 mm. When MRI showed mediolateral and anteroposterior tear lengths equal to or exceeding 20 mm, MRI was highly accurate (91%), sensitive (93%) and specific (90%). The present study showed ultrasound has lower sensitivity (86%) and specificity (67%) in predicting the rotator cuff repair method or repairability but it has the advantages of large sample size.
A strength of the present study was that the sonographer who performed ultrasound on the patients was an expert in shoulder pathology. A possible limitation is that the sonographer was unblinded to patient variables. Also, sonographers with less experience may be less accurate. Another strength is that one orthopaedic surgeon performed all the surgeries and made the decision as to which repair method was most suitable. A limitation of the present study is that the surgeon was unblinded to the ultrasound assessment. The surgeon’s practice specializes in shoulder disorders. We acknowledge that the judgments on repairability may differ in the hands of other surgeons.
Of the pre-operative variables we examined, tear size area (or anteroposterior tear length) and age were the strongest predictors for rotator cuff tear repairability. Tears ≥4 cm2 or anteroposterior tear length ≥25 mm and elderly age are indications of irreparability. Sonographically-assessed fatty atrophy was insignificant in this study, possibly because only 10% of our cases had mild to moderate fatty atrophy and none were severe. To our knowledge, the present study is the first to investigate the accuracy of ultrasound in determining rotator cuff repairability.
Conclusions
The present study shows that ultrasound, performed by an experienced sonographer, can be an accurate imaging modality for predicting rotator cuff tear repairability. Tear size area and age (in order of predictor power) are the most significant predictive independent variables in the determination of rotator cuff tear repairability. Tear size equal to or greater than 4 cm2 is indicative of an irreparable rotator cuff tear. These factors demonstrated stronger relationships with repairability than the measure of muscle quality.
Acknowledgments
This study has been communicated as an oral presentation at the Australian Sports Medicine Be Active Meeting 2014 (15 to 18 October 2014). Presented on 16 October 2014 by the lead author, as ‘Ultrasound Determination of Rotator Cuff Repairability’.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg 2009; 1: 96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2000; 82: 505–15. [DOI] [PubMed] [Google Scholar]
- 3.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 2007; 35: 719–28. [DOI] [PubMed] [Google Scholar]
- 4.Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg 2003; 12: 550–4. [DOI] [PubMed] [Google Scholar]
- 5.Goutallier D, Postel JM, Bernageau J. Lavau L and Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994:78–83. [PubMed]
- 6.Shen PH, Lien SB, Shen HC, Lee CH, Wu SS, Lin LC. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg 2008; 17(Suppl 1): 1S–7S. [DOI] [PubMed] [Google Scholar]
- 7.Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am 2010; 92: 1894–908. [DOI] [PubMed] [Google Scholar]
- 8.Dines DM, Moynihan DP, Dines J, McCann P. Irreparable rotator cuff tears: what to do and when to do it; the surgeon's dilemma. J Bone Joint Surg Am 2006; 88: 2294–302. [DOI] [PubMed] [Google Scholar]
- 9.Green A. Chronic massive rotator cuff tears: evaluation and management. J Am Acad Orthop Surg 2003; 11: 321–31. [DOI] [PubMed] [Google Scholar]
- 10.Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. J Shoulder Elbow Surg 2009; 18: 808–18. [DOI] [PubMed] [Google Scholar]
- 11.Nho SJ, Delos D, Yadav H, et al. Biomechanical and biologic augmentation for the treatment of massive rotator cuff tears. Am J Sports Med 2010; 38: 619–29. [DOI] [PubMed] [Google Scholar]
- 12.Davidson JF, Burkhart SS, Richards DP, Campbell SE. Use of preoperative magnetic resonance imaging to predict rotator cuff tear pattern and method of repair. Arthroscopy 2005; 21: 1428–1428. [DOI] [PubMed] [Google Scholar]
- 13.Sugihara T, Nakagawa T, Tsuchiya M, Ishizuki M. Prediction of primary reparability of massive tears of the rotator cuff on preoperative magnetic resonance imaging. J Shoulder Elbow Surg 2003; 12: 222–5. [DOI] [PubMed] [Google Scholar]
- 14.Yoo JC, Ahn JH, Yang JH, Koh KH, Choi SH, Yoon YC. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy 2009; 25: 573–82. [DOI] [PubMed] [Google Scholar]
- 15.Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NCA, Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev 2013; 9: CD009020–CD009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Shawi A, Badge R, Bunker T. The detection of full thickness rotator cuff tears using ultrasound. J Bone Joint Surg Br 2008; 90: 889–92. [DOI] [PubMed] [Google Scholar]
- 17.Brenneke SM, Morgan CJ. Evaluation of ultrasonography as a diagnostic technique in the assessment of rotator cuff tendon tears. Am J Sports Med 1992; 20: 287–9. [DOI] [PubMed] [Google Scholar]
- 18.Bryant L, Shnier R, Bryant C, Murrell GA. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elbow Surg 2002; 11: 219–24. [DOI] [PubMed] [Google Scholar]
- 19.Chang CY, Wang SF, Chiou HJ, Ma HL, Sun YC, Wu HD. Comparison of shoulder ultrasound and MR imaging in diagnosing full-thickness rotator cuff tears. J Clin Imaging 2002; 26: 50–4. [DOI] [PubMed] [Google Scholar]
- 20.de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. Am J Roentgenol 2009; 192: 1701–7. [DOI] [PubMed] [Google Scholar]
- 21.Fotiadou AN, Vlychou M, Papadopoulos P, Karataglis DS, Palladas P, Fezoulidis IV. Ultrasonography of symptomatic rotator cuff tears compared with MR imaging and surgery. Eur J Radiol 2008; 68: 174–9. [DOI] [PubMed] [Google Scholar]
- 22.Hodler J, Fretz CJ, Terrier F, Gerber C. Rotator cuff tears: correlation of sonographic and surgical findings. Radiology 1988; 169: 791–4. [DOI] [PubMed] [Google Scholar]
- 23.Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am 2005; 87: 1305–11. [DOI] [PubMed] [Google Scholar]
- 24.Martin-Hervas C, Romero J, Navas-Acien A, Reboiras JJ, Munuera L. Ultrasonographic and magnetic resonance images of rotator cuff lesions compared with arthroscopy or open surgery findings. J Shoulder Elbow Surg 2001; 10: 410–5. [DOI] [PubMed] [Google Scholar]
- 25.Milosavljevic J, Elvin A, Rahme H. Ultrasonography of the rotator cuff: a comparison with arthroscopy in one-hundred-and-ninety consecutive cases. Acta Radiol 2005; 46: 858–65. [DOI] [PubMed] [Google Scholar]
- 26.Moosmayer S, Heir S, Smith HJ. Sonography of the rotator cuff in painful shoulders performed without knowledge of clinical information: results from 58 sonographic examinations with surgical correlation. J Clin Ultrasound 2007; 35: 20–6. [DOI] [PubMed] [Google Scholar]
- 27.Naqvi GA, Jadaan M, Harrington P. Accuracy of ultrasonography and magnetic resonance imaging for detection of full thickness rotator cuff tears. Int J Shoulder Surg 2009; 3: 94–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rutten MJ, Spaargaren GJ, van Loon T, de Waal Malefijt MC, Kiemeney LA, Jager GJ. Detection of rotator cuff tears: the value of MRI following ultrasound. Eur Radiol 2010; 20: 450–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sipola P, Niemitukia L, Kroger H, Hofling I, Vaatainen U. Detection and quantification of rotator cuff tears with ultrasonography and magnetic resonance imaging – a prospective study in 77 consecutive patients with a surgical reference. Ultrasound Med Biol 2010; 36: 1981–9. [DOI] [PubMed] [Google Scholar]
- 30.Smith TO, Back T, Toms AP, Hing CB. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol 2011; 66: 1036–48. [DOI] [PubMed] [Google Scholar]
- 31.Teefey SA, Rubin DA, Middleton WD, Hildebort CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. J Bone Joint Surgery Am 2004; 86: 708–16. [PubMed] [Google Scholar]
- 32.Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. Am J Roentgenol 2008; 190: 1105–11. [DOI] [PubMed] [Google Scholar]
- 33.Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M. Fatty Atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology 2005; 237: 584–9. [DOI] [PubMed] [Google Scholar]
- 34.Wall LB, Teefey SA, Middleton WD, et al. Diagnostic performance and reliability of ultrasonography for fatty degeneration of the rotator cuff muscles. J Bone Joint Surg Am 2012; 94: e83–e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Briggs LM, Murrell GA. Diagnostic ultrasound: examination of the shoulder. Tech Shoulder Elbow Surg 2011; 12: 101–7. [Google Scholar]