Abstract
In the U.S., 90 million adults have low health literacy. An important public health challenge is developing obesity treatment interventions suitable for those with low health literacy. The objective of this study was to examine differences in sociodemographic and clinical characteristics, as well as weight and intervention engagement outcomes by health literacy. We randomized 194 participants to usual care or to the Shape Program intervention, a 12 month digital health treatment aimed to prevent weight gain among overweight and class I obese black women in primary care practice. We administered the Newest Vital Sign instrument to assess health literacy. Over half (55%)of participants had low health literacy, which was more common for those with fewer years of educational attainment and lower income. There was no effect of health literacy on 12-month weight change or on intervention engagement outcomes (completion of coaching calls and interactive voice response self-monitoring calls). Low health literacy did not preclude successful weight gain prevention in the Shape Program intervention. Goal focused behavior change approaches like that used in Shape may be particularly helpful for treating and engaging populations with low health literacy.
Keywords: Health literacy, primary care, obesity, weight gain prevention, intervention, black women
As the pervasiveness of obesity shows no signs of abating in the United States (Ogden, Carroll, Kit, & Flegal, 2014), effective and scalable weight loss interventions are desperately needed. Evidence-based behavioral weight loss interventions can consist of several key components, including communication with trained interventionists, self-monitoring of food intake and physical activity, written health materials with instructions on how to change behavior, and progress reports that depict changes in behaviors over the duration of the intervention. While these multicomponent behavioral interventions have been shown to be effective in producing weight loss (Eckel et al., 2013), they contain inherent expectations about participants' literacy and numeracy skills.
Health literacy refers to the ability to read and interpret health information and make appropriate health decisions (Institute of Medicine, 2004). It encompasses both prose literacy and quantitative literacy (i.e., numeracy) skills. Having adequate health literacy allows individuals to be able to interpret nutrition labels, understand the concept of body mass index, and adhere to treatment regimens. Low health literacy challenges 90 million U.S. adults (USDHHS, 2010). Individuals most at risk include those from low socioeconomic status groups, those of older age, and some racial/ethnic minority groups (Adams et al., 2009; Huizinga, Beech, Cavanaugh, Elasy, & Rothman, 2008; Kutner, Greenburg, Jin, & Paulsen, 2006). However, unlike the link between education and general literacy skills (Kutner et al., 2006), even individuals with high educational attainment may have low health literacy (Kutner et al. 2006; Shigaki, Kruse, Mehr, & Ge, 2012). In two recent studies, among individuals with at least some college education, 32%-53% lacked adequate health literacy (Adams et al., 2009; Shigaki et al., 2012).
The high prevalence of limited health literacy is concerning because of its many negative correlates, including poor health status (Kutner et al., 2006)and higher body mass index (Huizinga et al., 2008). Among overweight and obese individuals, limited health literacy is associated with misperception of weight status (Darlow, Goodman, Stafford, Lachance, & Kaphingst, 2012), poorer diet quality (Cha et al., 2014), failure to understand adverse health consequences of excess weight and to recognize the need to lose weight (Kennen et al., 2005), decreased readiness to change (Cardozo et al., 2013; Kennen et al., 2005), and lower self-efficacy (Cha et al., 2014), which may all complicate the weight loss process.
A major challenge is to design obesity treatments that are accessible to individuals across the spectrum of health literacy. Such was the aim for the Shape Program, a digital health intervention to prevent weight gain in primary care patients (Bennett et al., 2013; Foley et al., 2012). We designed the Shape Program to accommodate a medically vulnerable population with low literacy and numeracy. We utilized the interactive obesity treatment approach (iOTA) (Bennett et al., 2012; Foley et al., 2012), which had individuals track concrete, easily comprehensible behavior change goals (e.g., no sugary drinks, eat breakfast, no late night snacking). iOTA was designed to minimize the literacy and numeracy barriers associated with traditional lifestyle interventions for weight management. No published studies have examined whether health literacy impacts intervention engagement or weight change outcomes in a weight management trial. The purpose of this investigation was to examine differences in sociodemographic and clinical characteristics by health literacy, and to assess the extent to which health literacy is associated with 12-month weight change and intervention engagement. We developed the intervention so that the impact of health literacy would be minimized; we hypothesized that there would be no difference in outcomes by health literacy level.
Methods
Study Design
The Shape Program was a two-arm randomized controlled trial that aimed to prevent weight gain. Details of the study design, enrollment process (Foley et al., 2012), and outcomes (Bennett et al., 2013) are presented elsewhere. Briefly, participants (N=194) were randomized to either the Shape intervention (n=97) or to a usual care group (n=97) using a computer-generated algorithm. After the initial baseline visit, additional assessment visits took place at 6, 12, and 18 months post-randomization. Participants were reimbursed $50 for attending each assessment visit. The study was conducted between December 2009 and October 2012. The university Institutional Review Board approved and monitored this study.
Participants
Patients were recruited from five North Carolina federally qualified community health centers affiliated with Piedmont Health. Piedmont serves a predominantly socioeconomically disadvantaged (98% are <200% of the federal poverty level) and racial/ethnic minority (77%) population. Inclusion criteria consisted of the following: black women aged 25 to 44 years, body mass index (BMI) of 25 to 34.9 kg/m2, ability to read and write in English, and one or more visits in the prior 24 months to a Piedmont Health community health center. Exclusion criteria included current or recent pregnancy (≤ 12 months postpartum), myocardial infarction or stroke in prior 2 years, and history of profound cognitive, developmental, or psychiatric disorders.
Intervention
Details of the intervention design are reported elsewhere (Bennett et al., 2013; Foley et al., 2012). Briefly, the Shape Program was a 12-month, theory- (Bandura, 1977) and evidence-based intervention (Bennett et al., 2012) to prevent weight gain. As mentioned previously, the foundation of the intervention was the interactive obesity treatment approach (iOTA), which aimed to create a small calorie deficit to counter weight gain. Participants were asked to walk 7-10,000 steps a day, and to retain this goal for the duration of the intervention. A computer algorithm prescribed two other behavior change goals at baseline, based on each participant's need for change and self-efficacy, as well as the goal's potential to produce an energy deficit. These two goals changed automatically, by algorithm, every 6 weeks. Participants were mailed a new set of paper tracking logs each cycle. At the 6-month assessment, participants completed a questionnaire that assessed need for change and self-efficacy related to a new set of weight gain prevention goals. Sample goals included “no sugary drinks,” “no snacking after dinner,” and “eat five fruits and vegetables a week.”
Aside from these tailored behavior change goals, four other components comprised the intervention: (1) weekly (52) self-monitoring of goals via interactive voice response (IVR) telephone calls; (2) tailored skills training verbal messages and materials; (3) 12 one-on-one counseling calls delivered monthly by a Piedmont Health registered dietitian (“a health coach”); and (4) a year long membership to the YMCA. Together, these five components were mutually reinforcing. Participants tracked their assigned goals via 3-5 minute automated IVR calls to provide adherence and receive brief feedback on progress. IVR technology facilitates the collection of self-monitoring data with the aid of a computer-based system. The IVR system's pre-recorded voice prompts asked participants about their progress on each of their three goals, and participants inputted responses via a telephone keypad, which subsequently triggered automated, individualized feedback from a linked computer database. Concurrently, each month health coaches spoke with participants for 20 minutes, on average, using motivational interviewing strategies to promote goal setting, problem solving, and self-efficacy, as well as to provide accountability, social support, and skills training. Additional skills training consisted of printed goal sheets with tips and recipes. The usual care arm received wellness newsletters every six months. Study staff made no attempt to impact these participants' standard of care from their Piedmont Health providers.
As previously reported (Bennett et al., 2013), the Shape Program intervention produced significant mean (SE) weight change of -1.0 kg (0.5) at 12 months, compared to a gain of +0.5 kg (0.5) in the usual care arm (mean difference, -1.4 kg, 95% CI, -2.8 to -.01 kg; p = .04). The intervention also produced high engagement rates. Of the eligible intervention participants (n=91) remaining in the primary 12-month analysis, the mean coaching call completion rate was 81.9% (median was 12 out of 12 calls). Intervention participants completed a median of 83.0% (IQR, 52%-96%) of IVR tracking calls. Weight change at 12 months correlated significantly with IVR call completion rate (Spearman r = -0.2; p = .04), but not with coaching call completion rate (Spearman r = -0.2; p = .16).
Measures
Health literacy
At the 18-month assessment visit, study staff administered verbally the Newest Vital Sign (NVS) (Pfizer, 2011; Weiss et al., 2005). This 6-item screening measure was designed to quickly assess numeracy and literacy skills in a primary care setting. Study evaluation staff instructed participants to locate and interpret information on a printed nutrition label of an ice cream container; participants provided their answer orally. Correct responses received one point each, resulting in a range of 0 to 6 points possible. Scores of 0 to 1 indicate a “high likelihood that the patient has limited literacy,” scores of 2 to 3 indicate a “possibility of limited literacy,” and scores of 4 to 6 almost always indicate “adequate literacy”(Weiss et al., 2005). Consistent with previous studies, we combined the two lower categories into one called “low health literacy” (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011; Darlow et al., 2012).
The Newest Vital Sign has moderate internal consistency reliability (Cronbach's alpha = 0.71 to 0.76) and acceptable criterion validity with the Test of Functional Health Literacy in Adults (TOFHLA) (r = 0.59 to 0.61) (Osborn et al., 2007;Weiss et al., 2005). To detect low health literacy using a cut-off of <4 on the Newest Vital Sign, the ROC curve demonstrated high sensitivity (100%) and moderate specificity (64%) (Weiss et al., 2005). Four NVS items assess numeracy skills, while two assess prose literacy skills. In the current study, Cronbach's alpha was .65. Due to logistical matters, this measure was not administered in earlier assessment visits (see discussion for further details).
Anthropometrics and cardiometabolic risk factors
Participants changed into medical gowns and removed their shoes for physical measurements. Study staff measured participants' heights to the nearest 0.1 centimeters with a wall-mounted stadiometer (Seca 214) (Centers for Disease Control and Prevention, 2007). Weights were measured to the nearest 0.1 kilogram using an electronic scale (Seca Model 876) (Centers for Disease Control and Prevention, 2007). BMI was calculated by dividing weight in kilograms by height in centimeters squared. Study evaluation staff were trained, and they collected anthropometric data at all four assessment visits. As described in detail elsewhere (Foley et al., 2012), blood pressure, cholesterol (total, high-density lipoprotein, low-density lipoprotein), triglycerides, and glucose were also assessed.
Intervention engagement
We examined two measures of engagement: (1) the completion rate of interactive voice response (IVR) calls (maximum 52 calls over 12 months), and (2) the completion rate of coaching calls (maximum 12 calls over 12 months). An IVR call was considered completed if it contained self-monitoring data on all three assigned goals. Health coaches marked successful telephone calls as completed in the intervention database. Successful engagement was considered as rates of ≥ 80% completion.
Sociodemographic and clinical characteristics
At baseline, all participants provided sociodemographic information (e.g., age, highest education level, employment status, annual household income) and reported any diagnosis of hypertension or type 2 diabetes mellitus. Depression was assessed with the 8-item Patient Health Questionnaire (PHQ-8) measure, with scores of 10 and above indicating moderate to severe depression (Kroenke et al., 2009). At the 18-month visit, participants reported whether they currently have health insurance, and, if applicable, type of health insurance. Additional measurement details can be found in Foley et al. (2012).
Statistical Analysis
Our analyses are limited to 175 participants (90.2% of sample) who completed the Newest Vital Sign measure at the 18-month visit. This included 89 participants from the usual care arm and 86 participants from the intervention arm. Those who did not complete the Newest Vital Sign included participants who became ineligible by the 12-month visit (n=9) due to pregnancy, relocation, or cancer diagnosis, and those who missed the 18-month visit (n=9). One participant completed the 18-month visit before the Newest Vital Sign was included as part of the assessment. Health literacy is relatively stable over time, with fluctuations commonly due to ageing, cognitive decline, or literacy training skill development (Baker, 2006). Chi-square and ANOVA models were conducted to examine differences in baseline characteristics between the low and adequate health literacy groups. We used Fisher's exact test to determine significance when at least one expected cell size was less than five. ANOVA was used to determine differences in health literacy by treatment arm. To examine differences in completers versus non-completers, we conducted chi-square and ANOVA models. Fixed effects linear mixed models (Littell, 2006) with an unstructured covariance matrix and restricted maximum likelihood estimates were conducted to assess the effect of health literacy on weight change over time. Participants with missing values were treated as missing at random. Models were estimated separately for each treatment arm. Logistic regression and linear regression analyses were employed to examine the association between intervention engagement outcomes and dichotomous health literacy level. We used Spearman's rank correlation to examine associations between intervention engagement rates and continuous health literacy score. Analyses were conducted using SAS version 9.3 (SAS Institute, Inc., Cary, NC). An alpha <0.05 was used to assess statistical significance.
Results
Baseline characteristics and main outcomes have been published in detail elsewhere (Bennett et al., 2013; Foley et al., 2012). Briefly, participants in this analysis (n=175) were black females with a mean age of 35.41± 5.48 years and a mean BMI of 30.19± 2.55 kg/m2. Many (75%) participants reported a household income less than $30,000 per year, with 21% reporting an income less than $10,000. Most (80%) had less than a college degree. One-third (33%) of participants had hypertension and one in four reported moderate to severe depression. Baseline characteristics did not differ by treatment arm. Our 18-month retention rate was 96%. Most participants (91.4%) completed all 4 study assessment visits. Completers did not differ from non-completers on any sociodemographic or clinical characteristics except cholesterol levels. Non-completers (n=9) had lower high-density lipoprotein cholesterol (M = 43.11; SD = 12.98) than did completers (M = 54.23; SD = 15.87), p< .05. Non-completers also had greater low-density lipoprotein cholesterol (M = 146.17; SD = 31.38) than did completers (M = 105.28; SD = 33.64), p< .01.
The mean (SD) number of health literacy items answered correctly was 3.19 (1.56) out of 6 total items. Over half of participants (55%) obtained scores in the low health literacy range, while 45% obtained scores in the adequate range. Most (83%) participants responded correctly to the two questions that tested prose literacy skills. In comparison, only 7% of participants responded correctly to the four numeracy questions, while 31% failed to answer any of the numeracy questions correctly. Mean health literacy did not differ significantly by treatment arm (M (SD): intervention 3.27 (1.44); usual care 3.12 (1.67), p = .54).
Table 1 presents baseline sociodemographic and clinical characteristics, stratified by health literacy. Compared to participants with adequate health literacy, those with low health literacy reported significantly less educational attainment (p < .0001). Roughly half (52%) of individuals with low health literacy completed no education beyond high school, compared to 16% of those with adequate health literacy. Among individuals who had at least some college education, over one in three (39%) has low health literacy. Household income differed by health literacy (p = .03). Over half (59%) of individuals with low health literacy reported a household income < $20,000 per year, compared to 38% of those with adequate health literacy. No significant differences between health literacy groups were found for age, employment or health insurance status, presence of any medical condition, or baseline anthropometrics or cardiometabolic risk factors.
Table 1. Sociodemographic and Clinical Characteristics by Health Literacy.
| Low Health Literacya (n =96) | Adequate Health Literacy (n = 79) | |
|---|---|---|
| Age, mean (SD), y | 35.19 (5.67) | 35.68 (5.27) |
|
| ||
| Education, No. (%) | ** | |
| Less than high school | 16 (17.02) | 3 (3.85) |
|
| ||
| High school | 33 (35.11) | 10 (12.82) |
|
| ||
| Vocational or trade school after high school | 8 (8.51) | 8 (10.26) |
|
| ||
| Some college | 25 (26.60) | 36 (46.15) |
|
| ||
| College or above | 12 (12.77) | 21 (26.92) |
|
| ||
| Employment status, No. (%) | ||
| Employed | 64 (68.09) | 60 (76.92) |
|
| ||
| Not employed | 30 (31.91) | 18 (23.08) |
|
| ||
| Household income/y, No. (%) | * | |
| <$10,000 | 21 (22.11) | 16 (20.51) |
|
| ||
| $10-19,999 | 35 (36.84) | 14 (17.95) |
|
| ||
| $20-29,999 | 21 (22.11) | 23 (29.49) |
|
| ||
| >$30,000 | 18 (18.95) | 25 (32.05) |
|
| ||
| Insurance status, No. (%)b | ||
| Private | 24 (25.00) | 25 (31.65) |
|
| ||
| Medicaid | 22 (22.92) | 16 (20.25) |
|
| ||
| Medicare | 4 (4.17) | 2 (2.53) |
|
| ||
| Other | 3 (3.13) | 3 (3.80) |
|
| ||
| No insurance | 43 (44.79) | 33 (41.77) |
|
| ||
| Weight, mean (SD), kg | 80.55 (9.28) | 82.02 (8.35) |
|
| ||
| Body mass index, mean (SD), kg/m2 | 29.92 (2.57) | 30.52 (2.49) |
|
| ||
| Blood pressure, mean (SD), mmHg | ||
| Systolic | 123.77 (15.38) | 122.66 (14.69) |
|
| ||
| Diastolic | 80.49 (11.42) | 80.91 (10.91) |
|
| ||
| Lipids, mean (SD), mg/dL | ||
| Total cholesterol | 180.27 (39.87) | 175.32 (32.71) |
|
| ||
| Triglycerides | 100.92 (46.97) | 104.54 (49.94) |
|
| ||
| HDL cholesterol | 54.61 (14.98) | 53.79 (16.96) |
|
| ||
| LDL cholesterol | 109.36 (36.28) | 100.78 (30.24) |
|
| ||
| Glucose, mean (SD), mg/dL | 101.48 (32.88) | 107.63 (52.21) |
|
| ||
| Medical conditions, No. (%) | ||
|
| ||
| Hypertensionc | 31 (32.29) | 26 (33.33) |
|
| ||
| Diabetesc | 4 (4.17) | 5 (6.41) |
|
| ||
| Metabolic syndromed | 32 (33.33) | 27 (34.18) |
|
| ||
| Depressione | 26 (27.08) | 18 (22.78) |
Abbreviations:HDL cholesterol, high-density lipoprotein cholesterol; LDL cholesterol, low-density lipoprotein cholesterol; No. = Number; SD = standard deviation.
SI conversion factors: To convert HDL-cholesterol, LDL-cholesterol, and total cholesterol values to mmol/L, multiply by 0.0259; to convert triglycerides to mmol/L, multiply by 0.0113;to convert glucose values to mmol/L, multiply by 0.0555.
p< .05 for comparison between participants with lot and adequate health literacy.
p< .0001 for comparison between participants with lot and adequate health literacy.
Low literacy: Newest Vital Sign score of 0-3. Adequate literacy: Newest Vital Sign score of 4-6.
Insurance status was assessed at the 18-month visit via a self-report questionnaire.
Self-reported.
The criteria for metabolic syndrome were based on the guidelines developed by the National Cholesterol Education Program's Adult Treatment Panel III report. Metabolic syndrome was defined as the presence of three or more of the following risk determinants: 1) increased waist circumference (>102 cm [>40 in] for men, >88 cm [>35 in] for women); 2) elevated triglycerides (≥150 mg/dL); 3) low HDL cholesterol (<40 mg/dL in men, <50 mg/dL in women); 4) hypertension (≥130/≥85 mmHg); and 5) impaired fasting glucose (≥110 mg/dL).
Depression score of ≥10 on the PHQ-8 measure.
Intervention Engagement
Participants with low health literacy completed, on average, 71.83% (SD = 28.17) of interactive voice response (IVR) calls, compared to 73.64% (SD = 27.91) of participants with adequate literacy. Health literacy was not associated with rate of IVR call completion, F(1, 84) = 0.09, p = .77. Individuals with low health literacy had similar odds of achieving successful IVR engagement (≥80% completion), compared to those with adequate health literacy [OR(95% CI): 0.98(0.42-2.28); p = .95].
Participants with low health literacy completed, on average, 83.16% (SD = 24.17) of coaching calls, compared to a 85.47% (SD = 25.63) coaching call completion rate for those with adequate literacy. Health literacy was not associated with coaching call completion rate, F(1, 84) = 0.18, p = .67. Individuals with low health literacy had similar odds of achieving high levels of coaching call engagement (≥80% completion), compared to those with adequate health literacy [OR(95% CI): 1.53(0.59-3.99); p = .38].
Figure 1 displays the mean intervention engagement rate by health literacy score, where higher scores indicate that more items were answered correctly. Consistent with the dichotomous results, health literacy score was not significantly correlated with either IVR call completion rate (Spearman r = 0.06, p = .60) or coaching call completion rate (Spearman r = 0.10, p = .37).
Figure 1.
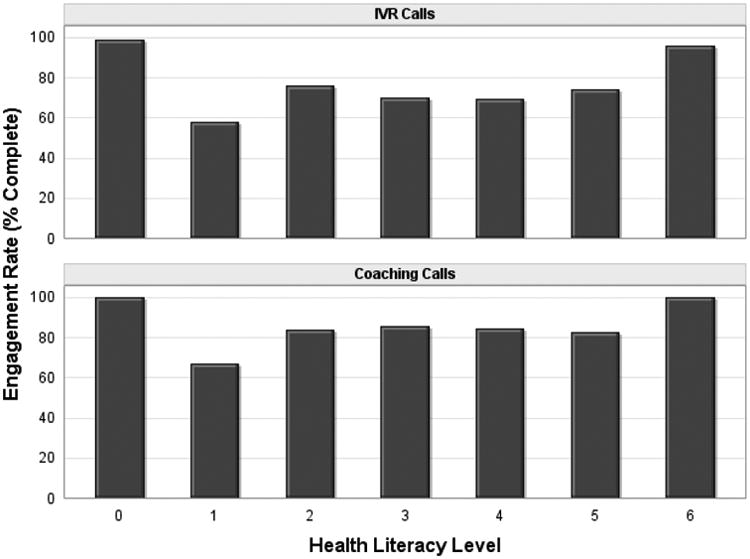
Intervention engagement rates by health literacy score.
Weight Change
Figure 2 displays mean weight change by health literacy. There was no significant effect of health literacy on 12-month weight change outcomes. Within the intervention arm, participants with adequate health literacy lost, on average, -0.40 kg (SE 0.81), compared to those with low health literacy who lost, on average, -1.19 kg (SE 0.74); this difference was not statistically significant (mean difference, 0.79 kg; 95% CI, -1.39 to 2.96; p = .47) (see Table 2). Within the usual care arm, participants with adequate health literacy gained, on average, 1.55 kg (SE 0.73) compared to those with low health literacy who gained, on average, -0.18 kg (SE 0.67); this difference was not statistically significant (mean difference, 1.72 kg; 95% CI, -3.68 to 0.24; p = .09). There was no significant interaction between treatment arm and health literacy in predicting weight change, F(1, 171) = 0.42, p = .52.
Figure 2.
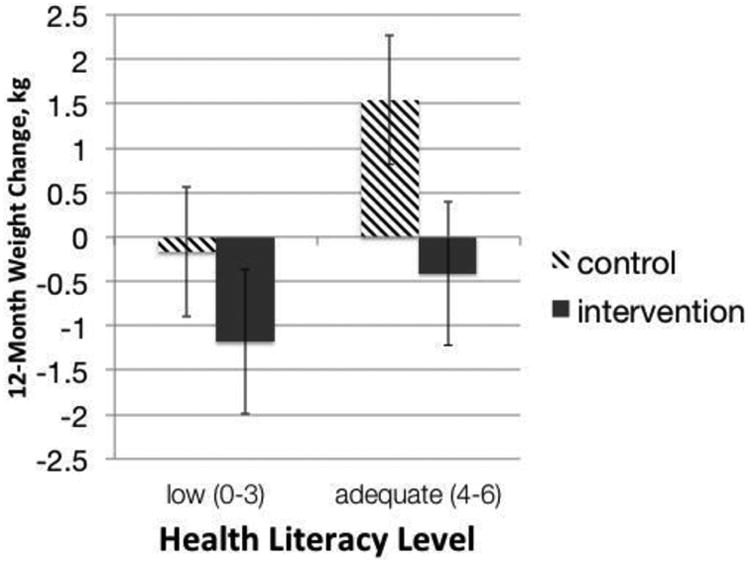
Health literacy level and weight change, by treatment arm. Error bars indicate standard error for weight change.
Table 2. Change in Weight (kg) by Health Literacy Level and Treatment Arm.
| Mean (SE) Change | Difference, Mean [95% CI], p-value | ||
|---|---|---|---|
|
| |||
| Low Health Literacya(n = 96) | Adequate Health Literacy (n = 79) | ||
| Intervention (n=86) | |||
| Month 6 | -0.77 (0.58) | -0.88 (0.63) | -0.11 [-1.82, 1.60], .90 |
|
| |||
| Month 12 | -1.19 (0.74) | -0.40 (0.81) | 0.79 [-1.39, 2.96], .47 |
|
| |||
| p-value, BL to 12 Mo. | .11 | .62 | |
|
| |||
| Usual Care (n=89) | |||
| Month 6 | 0.17 (0.55) | 0.18 (0.61) | 0.00 [-1.62, 1.62], 1.00 |
|
| |||
| Month 12 | -0.18 (0.67) | 1.55 (0.73) | 1.72 [-3.68, 0.24], .09 |
|
| |||
| p-value, BL to 12 Mo. | .79 | .04 | |
Abbreviations: 12 Mo., 12 Month; BL, baseline; kg, kilograms; 95% CI = 95% confidence interval; SE = standard error.
Low literacy: Newest Vital Sign score of 0-3. Adequate literacy: Newest Vital Sign score of 4-6.
Discussion
We found that health literacy did not impair the ability of a behavioral intervention to promote long-term weight stability among a high risk population. Intervention group participants maintained or even lost some weight over the course of the 12-month Shape Program treatment, regardless of their level of health literacy. Thus, low health literacy did not serve as a barrier to the successful prevention of weight gain through the Shape Program intervention. This is the first study, to our knowledge, that examines the relation between health literacy and weight outcomes in a weight management trial.
In its seminal report, the American Medical Association reported that health literacy predicts health outcomes more strongly than any other sociodemographic characteristic, including age, race, income, education, and employment status (Parker et al., 1999). In light of this finding and the many adverse correlates of low health literacy, recent recommendations have encouraged interventionists to assess participants' health literacy and evaluate the effect of health literacy on weight and engagement outcomes (Huizinga et al., 2008; Noel, 2012).
Our intervention was successful in engaging people at a high level. We found no differences in interactive voice response (IVR) or coaching call completion rates by health literacy. Because of the high rates of completion of coaching calls (median 100%) and IVR self-monitoring calls (median 83%) we had limited variability, so perhaps it is unsurprising that we saw no differences by health literacy. We consider this a major strength of our approach. Our findings are consistent with that of Noel (2012), who found that IVR call completion did not vary by health literacy, assessed using the Newest Vital Sign, in an intervention to reduce consumption of sugar-sweetened beverages. Likewise, Schillinger et al. (2008) found that engagement with automated telephone calls (ATDM) did not vary by health literacy for English-speakers in a diabetes self-management intervention.
Over half (55%) of our sample had low health literacy. We observed lower health literacy levels relative to other studies that used this measure (Adams et al., 2009; Darlow et al., 2012; Weiss et al., 2005), likely due to the characteristics of our sample. Lower rates of health literacy have been observed among racial/ethnic minority groups, including blacks (Cha et al., 2014; Darlow et al., 2012; Huizinga et al., 2008; Rothman et al., 2006), and those of low socioeconomic position (Adams et al., 2009; Barber et al., 2009; Cha et al., 2014; Huizinga et al., 2008; Rothman et al., 2006; Shah, West, Bremmeyr, & Savoy-Moore, 2010). These findings are particularly concerning given the lack of efficacious weight management treatment options for black females (Osei-Assibey, Kyrou, Adi, Kumar, & Matyka, 2010), a demographic who has the highest prevalence of overweight or obesity (82%) among any racial/ethnic group in the U.S. (Ogden et al., 2014). However, in contrast to previous findings (Adams et al., 2009; Barber, et al., 2009; Schillinger et al., 2002), we did not find an association between health literacy and age, employment status, or health insurance status, likely due to ceiling effects. We also did not find a link between health literacy and BMI, cardiometabolic indicators, or presence of medical conditions, unlike some prior work (Adams et al., 2009; Barber et al., 2009; Huizinga et al., 2008), but consistent with other past findings (Cha et al., 2014; Rothman et al, 2006; Shah et al., 2010).
There are several reasons that our intervention might have connected with participants at all levels of health literacy. Our intervention was purposefully designed to be comprehensible to individuals with limited health literacy by incorporating components sensitive to those with lower-grade reading levels and limited math skills. First, our intervention was predominantly phone-based. Mobile phone usage is high among individuals with limited health literacy, while internet use and email communication - accessed via computer - are less frequent (Barber et al., 2009). Because IVR technology delivers information aloud over the telephone instead of via written materials, it has been recommended as a viable treatment platform for vulnerable populations, including those with limited literacy (Bickmore & Paasche-Orlow, 2012; Kraft & Androwich, 2012). In addition, telephone-based counseling has been demonstrated to be agreeable for patients with limited health literacy (Sarkar et al., 2008). In the Shape Program intervention, health coaches served to review progress and readiness to change, clarify uncertainties, reinforce learning of important health information, and address barriers and ambivalence. Moreover, health coaches could modify the presentation of information and suggest alternate strategies for goal achievement in order to meet the needs of their clients with limited numeracy or literacy skills. Taken together, these findings suggest that IVR platforms and telephone-based counseling may be appropriate strategies for delivering a weight management intervention to individuals with low health literacy.
Another approach we used to engage participants at all levels of health literacy was to emphasize participant adherence to concrete behavior change goals. For example, we asked “How many sugary drinks did you have last week?” instead of “How many calories did you eat today?” This goal-based approach is the crux of iOTA (Bennett et al., 2013; Foley et al., 2012). Participants were asked to change their behavior by adhering to three easily monitored, and plainly worded goals (e.g., avoid chips, cookies, and candy) that likely were of high need for change and high self-efficacy. That is, healthy behaviors to which the participant did not adhere (e.g., avoiding sugary drinks) were weighted so that the participant would be more likely to be assigned a corresponding goal.
In comparison, traditional weight management programs typically involve adhering to structured diet regimens, tracking caloric intake and nutrients, precisely measuring portion sizes, calculating physical activity durations, or monitoring heart rates and energy expenditure. For instance, the Diabetes Prevention Program, required participants to track their fat intake each day and count their duration of moderate-intensity physical activity (Knowler et al., 2002), while the Weight Loss Maintenance trial involved reducing total caloric intake, limiting sodium to ≤ 2400 mg/day, and following a DASH diet plan (Hollis et al., 2008). These types of intervention components involve numeracy skills and proficiency in reading nutrition labels. We suspect that greater health literacy is required to be successful in these programs, although research is limited in this area. Preliminary findings reveal that low numeracy skills are associated with greater difficulty in interpreting nutrition labels (Rothman et al., 2006), which is problematic for weight management trials that involve self-monitoring caloric intake or nutrients. Low health literacy has also been demonstrated to be associated with lower use of food labels (Cha et al., 2014). Although the U.S. Food and Drug Administration recently proposed to update the Nutrition Facts label found on food and beverage packages (FDA, 2014) -- with the aim to emphasize more clearly a product's calorie count and more accurately depict serving sizes -- food labels may still be under-utilized in the selection of healthy choices and common errors may still persist, including incorrect calculations, misperceptions about one's recommended daily value, confusion surrounding extraneous materials, faulty portion size estimates, and lack of knowledge about the meaning of different nutrients (Cha et al., 2014; Rothman et al., 2006).
Our study has several limitations. Because the purpose of our study was to prevent weight gain, not to promote weight loss, the variability within each treatment group's 12-month weight change is likely less than that seen in weight loss trials. Therefore, future studies are needed to draw conclusions about the impact of health literacy on outcomes in weight loss trials. It is also important to note that the Newest Vital Sign is a health literacy screening instrument, so it may be limited in its capacity to classify appropriately those who scored in the middle range. Moreover, no gold standard has yet to be established for specifying thresholds for health literacy or cutoffs for what constitutes low health literacy (Berkman et al., 2011). Another limitation is that health literacy was assessed only at the 18-month visit. Logistical constraints such as insufficient study evaluation personnel and time during the previous assessment visits to administer the NVS per protocol (which involves interviewer-administration) precluded the assessment of the NVS in our earlier assessment visits. Consequently, we are unable to examine whether trial attrition differed by health literacy. It is possible that individuals who did not complete the 18-month assessment were more likely to have low health literacy, compared to completers. However, as reported earlier, non-completers did not differ from completers on any baseline sociodemographic characteristics, including education level. Moreover, we considered that a one-time assessment of health literacy was acceptable because we did not expect health literacy to change as a function of participation in our Shape intervention or of time (Baker, 2006). Indeed, if our intervention focused on promoting health literacy skills, one would expect that health literacy would differ between the intervention group and the control group (with the former group's health literacy being higher than that of the latter); however, there was no difference in health literacy between these treatment groups. Further, we have no evidence to suggest that our intervention designed to prevent weight gain among primary care patients also promotes health literacy. Our intervention did not include education surrounding the calculation of caloric intake, interpreting nutrition labels, or using portion size tools. Rather, we focused on goal setting, self-monitoring, problem solving, social support, and accountability to promote behavior change. This is in comparison to other studies found to enhance health literacy outcomes that focused primarily on nutritional education and training (Taggart et al., 2012).
In addition, because of low sample size, we are unable to disentangle the effects of prose literacy skills from numeracy skills on weight and engagement outcomes. Lastly, the generalizability of our findings may be limited to overweight and obese black women. It is unknown whether males and individuals of other racial/ethnic groups may respond in a similar way to our intervention.
In summary, low health literacy was prevalent among our sample of Shape Program participants who were overweight and obese (class I) patients from a community health center setting. Our intervention was able to accommodate those with low health literacy skills, and produce weight stability and high engagement in coaching calls and IVR tracking calls. That is, despite having low health literacy, many intervention participants were able to understand and self-monitor their goals in order to successfully offset weight gain. As health literacy is becoming a more prominent public health priority (HealthyPeople.gov, 2014; Institute of Medicine, 2004), it is our hope that health literacy will be assessed more frequently pre-treatment, as is being done in the primary care setting (Kutner et al., 2006), with a universal precautions toolkit has been created for primary care practices (DeWalt & North Carolina Network Consortium, 2010). Obesity interventionists should also aim to design weight management interventions that take into consideration the likelihood that a sizable proportion of patients may have limited health literacy.
Acknowledgments
We express deep gratitude to the administration and staff of Piedmont Health for their continued collaboration and participation in the Shape Program. Most importantly, we would especially like to thank the women who participated in Shape.
References
- Adams RJ, Appleton SL, Hill CL, Dodd M, Findlay C, Wilson DH. Risks associated with low functional health literacy in an Australian population. Medical Journal of Australia. 2009;191(10):530–534. doi: 10.5694/j.1326-5377.2009.tb03304.x. [DOI] [PubMed] [Google Scholar]
- Baker DW. The meaning and the measure of health literacy. Journal of General Internal Medicine. 2006;21(8):878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Barber MN, Staples M, Osborne RH, Clerehan R, Elder C, Buchbinder R. Up to a quarter of the Australian population may have suboptimal health literacy depending upon the measurement tool: Results from a population-based survey. Health Promotion International. 2009;24(3):252–261. doi: 10.1093/heapro/dap022. [DOI] [PubMed] [Google Scholar]
- Bennett GG, Foley P, Levine E, Whiteley J, Askew S, Steinberg DM, et al. Wroth TH. Behavioral treatment for weight gain prevention among black women in primary care practice: A randomized clinical trial. JAMA Internal Medicine. 2013;173(19):1770–1777. doi: 10.1001/jamainternmed.2013.9263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GG, Warner ET, Glasgow RE, Askew S, Goldman J, Ritzwoller DP, et al. Colditz GA. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Archives of Internal Medicine. 2012;172(7):565–574. doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Bickmore TW, Paasche-Orlow MK. The role of information technology in health literacy research. Journal of Health Communication. 2012;17(sup3):23–29. doi: 10.1080/10810730.2012.712626. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey Protocol. Hyattsville: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [Google Scholar]
- Cha E, Kim KH, Lerner HM, Dawkins CR, Bello MK, Umpierrez G, Dunbar SB. Health literacy, self-efficacy, food label use, and diet in young adults. American Journal of Health Behavior. 2014;38(3):331–339. doi: 10.5993/AJHB.38.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chari R, Warsh J, Ketterer T, Hossain J, Sharif I. Association between health literacy and child and adolescent obesity. Patient Education and Counseling. 2014;94(1):61–66. doi: 10.1016/j.pec.2013.09.006. [DOI] [PubMed] [Google Scholar]
- Darlow S, Goodman MS, Stafford JD, Lachance CR, Kaphingst KA. Weight perceptions and perceived risk for diabetes and heart disease among overweight and obese women, Suffolk County, New York, 2008. Preventing Chronic Disease. 2012;9:E81. doi: 10.5888/pcd9.110185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt DA North Carolina Network Consortium. Health literacy universal precautions toolkit. Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- Eckel RH, Jakicic JM, Ard JD, et al. J Am Coll Cardiol. 2013. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. [DOI] [PubMed] [Google Scholar]
- FDA U.S. Food and Drug Administration. Proposed changes to the Nutrition Facts Label. 2015 Aug 1; Retrieved from http://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm385663.htm.
- Foley P, Levine E, Askew S, Puleo E, Whiteley J, Batch B, et al. Bennett G. Weight gain prevention among black women in the rural community health center setting: The Shape Program. BMC Public Health. 2012;12:305-2458-12–305. doi: 10.1186/1471-2458-12-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HealthyPeople.gov. Health Communication and Health Information Technology. 2014 Retrieved from http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=18.
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, et al. Funk K. Weight loss during the intensive intervention phase of the Weight-Loss Maintenance trial. American Journal of Preventive Medicine. 2008;35(2):118–126. doi: 10.1016/j.amepre.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huizinga MM, Beech BM, Cavanaugh KL, Elasy TA, Rothman RL. Low numeracy skills are associated with higher BMI. Obesity. 2008;16(8):1966–1968. doi: 10.1038/oby.2008.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Report Brief Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Kennen EM, Davis TC, Huang J, Yu H, Carden D, Bass R, Arnold C. Tipping the scales: The effect of literacy on obese patients' knowledge and readiness to lose weight. Southern Medical Journal. 2005;98(1):15–18. doi: 10.1097/01.SMJ.0000146617.21240.49. [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraft MR, Androwich I. Interactive voice response technology: A tool for improving healthcare. Paper presented at the NI 2012: Proceedings of the 11th International Congress on Nursing Informatics. 2012;2012 [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009;114(1):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Kutner M, Greenburg E, Jin Y, Paulsen C. The health literacy of America's adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: U.S. Department of Education. National Center for Education Statistics; 2006. [Google Scholar]
- Littell RC, Stroup WW, Milliken GA, Wolfinger RD, Schabenberger O. SAS for mixed models. SAS institute; 2006. [Google Scholar]
- Noel L. Retrieved from VTech Works Electronic Theses and Dissertations. 2012. The Role of health literacy in intervention engagement, teach back performance, and perceptions of intervention components. [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn CY, Weiss BD, Davis TC, Skripkauskas S, Rodrigue C, Bass PF, Wolf MS. Measuring adult literacy in health care: performance of the newest vital sign. American Journal of Health Behavior. 2007;31(Supplement 1):S36–S46. doi: 10.5555/ajhb.2007.31.supp.S36. [DOI] [PubMed] [Google Scholar]
- Osei-Assibey G, Kyrou I, Adi Y, Kumar S, Matyka K. Dietary and lifestyle interventions for weight management in adults from minority ethnic/non- White groups: A systematic review. Obesity Reviews. 2010;11(11):769–776. doi: 10.1111/j.1467-789X.2009.00695.x. [DOI] [PubMed] [Google Scholar]
- Parker RM, Williams MV, Weiss BD, Baker DW, Davis TC, Doak CC, et al. Nurss J. Health literacy-Report of the Council on Scientific Affairs, Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA. 1999;281(6):552–557. [PubMed] [Google Scholar]
- Pfizer. The Newest Vital Sign: A Health literacy assessment tool. 2011 Retrieved from http://www.pfizer.com/files/health/nvs_flipbook_english_final.pdf.
- Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, et al. Elasy TA. Patient understanding of food labels: The role of literacy and numeracy. American Journal of Preventive Medicine. 2006;31(5):391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- Sarkar U, Piette JD, Gonzales R, Lessler D, Chew LD, Reilly B, et al. Regenstein M. Preferences for self-management support: Findings from a survey of diabetes patients in safety-net health systems. Patient Education and Counseling. 2008;70(1):102–110. doi: 10.1016/j.pec.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Hammer H, Wang F, Palacios J, McLean I, Tang A, et al. Handley M. Seeing in 3-D: Examining the reach of diabetes self-management support strategies in a public health care system. Health Education & Behavior : The Official Publication of the Society for Public Health Education. 2008;35(5):664–682. doi: 10.1177/1090198106296772. doi:1090198106296772. [DOI] [PubMed] [Google Scholar]
- Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: The “Newest Vital Sign” ease of use and correlates. Journal of the American Board of Family Medicine: JABFM. 2010;23(2):195–203. doi: 10.3122/jabfm.2010.02.070278. [DOI] [PubMed] [Google Scholar]
- Shigaki CL, Kruse RL, Mehr DR, Ge B. The REALM vs. NVS: A comparison of health literacy measures in patients with diabetes. Annals of Behavioral Science and Medical Education. 2012;18(1):9–13. [Google Scholar]
- Taggart J, Williams A, Dennis S, Newall A, Shortus T, Zwar N, et al. Harris MF. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC family practice. 2012;13(1):49. doi: 10.1186/1471-2296-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National Action Plan to Improve Health Literacy. Washington, DC: U.S. Department of Health and Human Services; 2010. Retrieved from http://www.health.gov/communication/HLActionPlan/ [Google Scholar]
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Hale FA. Quick assessment of literacy in primary care: The Newest Vital Sign. Annals of Family Medicine. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]


