Abstract
Background/Objectives
This study aimed to determine the association between a Mediterranean diet and glycemic control and other cardiovascular risk factors among youth with type 1 diabetes (T1D).
Subjects/Methods
Incident T1D cases aged <20 years at diagnosis between 2002 and 2005 were included. Participants were seen at baseline (N=793), 1-year (N=512) and 5-year follow-up visits (N=501). Mediterranean diet score was assessed using a modified KIDMED index (mKIDMED). Multivariate linear regression and longitudinal mixed model were applied to determine the association between mKIDMED score and log-HbA1c, lipids, blood pressure (BP), and obesity.
Results
In cross-sectional analyses using baseline data, for individuals with an HbA1c of 7.5%, a two-point higher mKIDMED score (one standard deviation) was associated with 0.15% lower HbA1c (P=0.02). A two-point higher mKIDMED score was associated with 4.0 mg/dL lower total cholesterol (TC) (P=0.006), 3.4 mg/dL lower low-density lipoprotein (LDL)-C (P=0.004), 3.9 mg/dL lower non-high-density lipoprotein (non-HDL)-C (P=0.004), and 0.07 lower LDL-C/HDL-C ratio (P=0.02). Using longitudinal data, a two-point increase in mKIDMED score was associated with 0.01% lower log-HbA1c (P=0.07), 1.8 mg/dL lower TC (P=0.05), 1.6 mg/dL lower LDL-C (P=0.03), and 1.8 mg/dL lower non-HDL-C (P=0.03) than would otherwise have been expected. HbA1c mediated about 20% of the association for lipids in both cross-sectional and longitudinal models. An unexpected positive association between mKIDMED score and systolic BP was found among non-Hispanic white youth in cross-sectional analyses (P=0.009). Mediterranean diet was not associated with obesity.
Conclusions
Mediterranean diet may improve glycemic control and cardiovascular health in T1D youth.
INTRODUCTION
Type 1 diabetes (T1D) is associated with 2–4 fold increased risk in cardiovascular mortality and morbidity.1,2 Poor glycemic control is commonly seen in youth with T1D,3 contributing further to the risk of cardiovascular diseases (CVD).2,4 Epidemiological evidence and autopsy data have revealed that pathological processes and risk factors associated with development of atherosclerosis, start early in childhood.2,5 There is an urgent need to devise effective management strategies to improve CVD risk profile and glycemic control in youth with T1D.3
The American Heart Association (AHA) advises that primary prevention of CVD should begin in childhood and that achieving and maintaining a healthy diet is critical.6 Healthful dietary patterns are developed in childhood and accrued health benefits track into adulthood.7 A systematic review of intervention studies reported an inverse association between a Mediterranean diet and dyslipidemia and obesity in adults.8 A Mediterranean diet may also be beneficial for blood pressure (BP)9 and hemoglobin A1c (HbA1c) in adults.10 The recent PREDIMED trial reported a reduction of about 30% in the risk of major cardiovascular events among individuals with diabetes who consumed a Mediterranean style diet.11 However, whether a Mediterranean diet confers similar benefits on glycemic control and CVD risk factors to youth with T1D is unknown. The purpose of the present report is to determine the associations of a Mediterranean diet with glycemic control and CVD risk factors in youth with T1D, using both cross-sectional and longitudinal data.
SUBJECTS AND METHODS
Started in 2001, SEARCH for Diabetes in Youth (SEARCH) is an ongoing multicenter epidemiologic study of physician-diagnosed diabetes among youth <20 years at diagnosis.12 The SEARCH Nutrition Ancillary Study was designed to assess the associations of nutritional factors with the progression of insulin secretion defects and CVD risk factors in youth with T1D. Both studies were reviewed and approved annually by the local institutional review boards that had jurisdiction over the local study population and complied with the Health Insurance Portability and Accountability Act. Written informed consent was obtained from participants age >18 years or their parents or legal guardians if <18 years.
Study participants
Participants eligible for inclusion were newly-diagnosed T1D cases before 20 years of age between 2002 and 2005. Participants were then invited to attend an initial baseline visit and three subsequent visits scheduled at about 1-year, 2-year, and 5-year of follow-up when demographic, anthropometric, laboratory and clinical data were collected. Food frequency questionnaire (FFQ) data were collected at baseline, 1-year and 5-year visits among those aged ≥10 years. During the study period, we did not perform any dietary intervention or education on participants. A baseline visit was completed for 1,156 incident T1D cases. Youth were sequentially excluded for missing FFQ (N=208), diabetes duration < 3 months (N=82), fasting < 8 hours (N=37) and eating much more or much less than typical (N=36) in the week covered by the FFQ. The same exclusions were applied to 1-year and 5-year follow-up data. The final sample consisted of 793 cases at baseline, 512 at 1-year and 501 at 5-year visits.
Outcome measures
Height, weight, waist circumference, and BP were measured according to standardized protocol by trained and certified staff. BMI was calculated as weight (kg)/height squared (m2) and converted to a BMI z score.13 Blood samples were collected under metabolic stability conditions, defined as no episode of diabetic ketoacidosis within 1 month before the visit, and after ≥8 hours of fasting. All samples were processed at the local site and then shipped within 24 hours to the central laboratory where specimens were assayed for HbA1c, total cholesterol (TC), triglycerides, and high-density lipoprotein (HDL)-C, low-density lipoprotein (LDL)-C and apolipoprotein B. Non-HDL-C was calculated as TC minus HDL-C. The standardized measurement and assay protocol for the SEARCH study was previously described.14 The same standardized protocol was applied to all three visits. Apolipoprotein B was not assayed at follow-up visits.
Dietary assessment and modified KIDMED (mKIDMED) score
Dietary intake was obtained via a FFQ. The details of the SEARCH FFQ and its validation were described elsewhere.15,16 Briefly, the FFQ contained 85 food lines. Participants reported whether the item(s) was consumed in the past week, on how many days, and in what average portion size which was queried for each line item either as a number (e.g., number of slices of bread) or relative to pictures of food in bowls or plates. In our validation study on a subgroup of 172 participants, we collected FFQ twice and used three 24-hour recalls to validate dietary data from FFQ. The mean correlations of food groups and nutrients between the FFQ and true usual intake were 0.41 and 0.38, respectively. Reliability of FFQ intake was with 54 % of Pearson correlation coefficients ≥0.5.16 The FFQ was primarily self-administered after participants were instructed by trained and certified staff. Interview administration was given if necessary.
The KIDMED index developed by Serra-Majem et al.17 has been widely used to evaluate a Mediterranean diet among children and adolescents. The KIDMED index was based on a 16-question survey designed to reflect the principles sustaining the Mediterranean dietary pattern and those that undermine it.17 The SEARCH FFQ was not originally designed for assessing Mediterranean diet through the KIDMED index and thus 5 modifications were necessary. First, because we did not query meal-specific intake, we used dietary intake in a whole day to reflect items specified for consumption at breakfast in the original KIDMED index. Second, we dropped the “skipping breakfast” item because there was no reliable way to impute this from our data. Third, SEARCH FFQ did not query for use of olive oil at home. This item was replaced with the monounsaturated fatty acids (MUFA)/saturated fatty acids (SFA) ratio, which has been widely used to characterize a Mediterranean diet in both the US and European populations.18,19 Fourth, one time/day in the KIDMED index was translated into one serving/day while >1 times/day was treated as ≥two servings/day in the mKIDMED index. Fifth, potato consumption was excluded from the vegetable group due to the possibility of including French fries or potato chips.18 Accordingly, we modified the 16-item KIDMED index into the 15-item mKIDMED index. Items denoting a negative connotation with respect to a Mediterranean diet were assigned a value of −1 while those with a positive aspect were scored +1. The score range of the mKIDMED index was from −3 to 12. Low, median and high Mediterranean diet score was defined as having a mKIDMED score of ≤3, 4–7 and ≥8, respectively.17
Statistical Analysis
Outcome variables with skewed distribution were log transformed (HbA1c and triglycerides). Mean and standard deviation (SD) were presented for normally distributed variables. Analysis of Variance (ANOVA) was used to evaluate the differences of each variable across the three Mediterranean diet categories (low, median and high). For variables that were non-normally distributed, the median and interquartile range (IQR) were presented and Kruskal Wallis test was applied to evaluate the differences. Categorical variables were examined using chi-square test.
HbA1c and BMI z score were explored as potential mediators20 a priori for the association between a Mediterranean diet and CVD risk factors. Gender and race/ethnicity (non-Hispanic white versus “other”) were evaluated as potential effect modifiers. Effect modification was assessed before the main effect. If effect modification variables were not significant (P >0.05), potential effect modifier(s) would be included as confounder(s). Additional confounders were age, duration of diabetes, parental education, family income, parental history of diabetes, study site, physical activity, sedentary behavior, smoking, total calories from FFQ, insulin regimen, and daily insulin dose per kilogram. Height was additionally adjusted for BP.
Baseline outcome data were modeled using a series of multivariate linear regressions, sequentially adjusting for non-modifiable confounders, modifiable confounders and mediators. To determine the association between the change in mKIDMED score across visits and glycemic control and CVD risk factors, repeatedly measured data were analyzed using mixed-models with a random intercept and random time-effect to account for within-subject dependence. Mixed models explicitly model individual-level change across time and are flexible in terms of repeated measures.21 All tests were conducted at a significance level of 0.05. Results were interpreted in terms of a two-point difference in mKIDMED score, which was approximately equal to one SD of the mKIDMED score. Data analyses were performed using SAS version 9.3 (SAS Institute, Inc., Cary, NC).
RESULTS
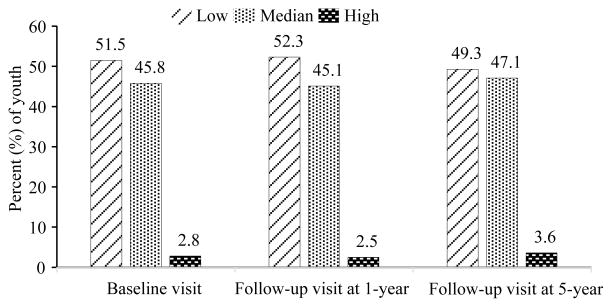
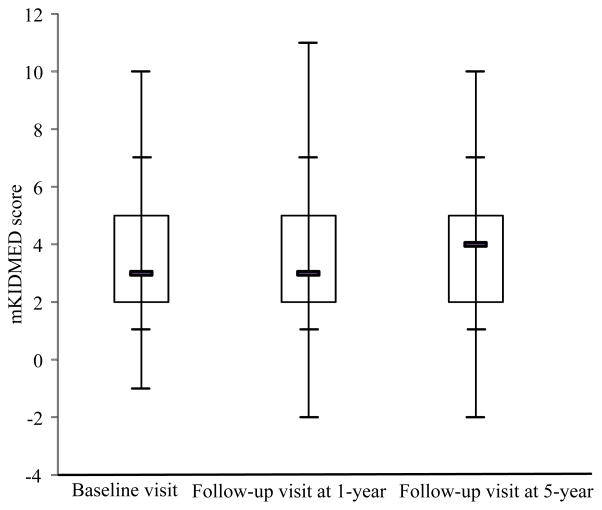
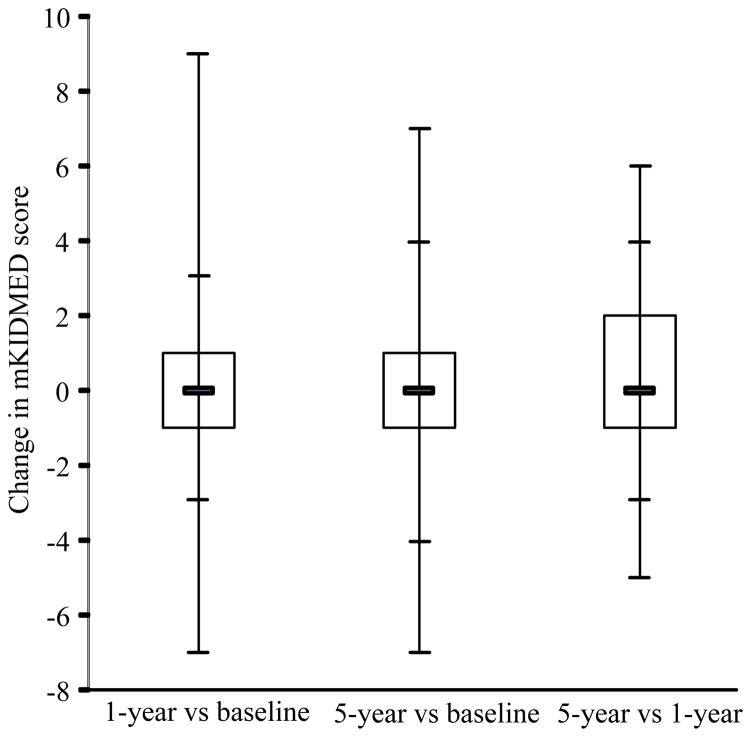
Only 2.8% of the 793 participants at baseline had high Mediterranean diet score while 45.8% had a median score and 51.5% had a low score (Table 1). There were no statistically significant differences between three Mediterranean diet categories in terms of age, gender, diagnosis age, duration of diabetes, race/ethnicity; a difference was seen for parental education (P=0.04). In these unadjusted analyses, TC and LDL-C were inversely associated with Mediterranean diet score, and higher score was associated with higher physical activity level. The distribution of the three Mediterranean diet categories was similar at baseline, 1-year and 5-year follow-up visits (Figure 1). The distribution of the mKIDMED score changed little over time (Figure 2, P=0.23). There was considerable individual-level change in mKIDMED score between different visits, but no difference in the distribution of the change was observed (Figure 3, P=0.84).
Table 1.
Demographic and clinical characteristics of youth ≥10 years of age with incident type 1 diabetes, stratified by a Mediterranean diet score at baseline visit
| Low (≤3) | Median (4–7) | High (≥8) | P valuea | |
|---|---|---|---|---|
| N (%) | 408 (51.45) | 363 (45.78) | 22 (2.77) | |
| Age, years, mean ± SD | 13.78 ± 2.46 | 13.67 ± 2.48 | 13.70 ± 1.98 | 0.84 |
| Female, % | 45.34 | 49.86 | 40.91 | 0.38 |
| Diagnosis age, years, mean ± SD | 12.40 ± 2.47 | 12.30 ± 2.47 | 12.23 ± 1.95 | 0.82 |
| Duration of diabetes, months, mean ± SD | 11.29 ± 6.31 | 10.98 ± 6.15 | 11.32 ± 5.90 | 0.79 |
| Race/ethnicity, % | 0.23 | |||
| Non-Hispanic white | 79.41 | 74.10 | 77.27 | |
| Non-Hispanic Black | 10.54 | 10.47 | 13.64 | |
| Other | 10.05 | 15.43 | 9.09 | |
| Parental education, % | 0.04 | |||
| Less than high school | 3.46 | 4.16 | 4.55 | |
| High school | 18.77 | 9.97 | 13.64 | |
| Some college | 34.32 | 34.90 | 40.91 | |
| College or more | 43.46 | 50.97 | 40.91 | |
| Vigorous physical activity ≥ 3 days/week, % | 59.90 | 66.11 | 81.82 | 0.04 |
| Watch television ≥ 2 hours/day, % | 56.33 | 52.81 | 40.91 | 0.28 |
| HbA1c, %, median (IQR) | 7.40 ± 2.00 | 7.30 ± 1.90 | 7.10 ± 1.00 | 0.54 |
| Total Cholesterol, mg/dL, mean (SD) | 161.57 ± 34.33 | 157.69 ± 32.78 | 143.55 ± 18.50 | 0.03 |
| LDL Cholesterol, mg/dL, mean (SD) | 95.49 ± 27.35 | 91.76 ± 26.44 | 77.10 ± 16.46 | 0.004 |
| HDL Cholesterol, mg/dL, mean (SD) | 51.78 ± 12.12 | 51.98 ± 11.89 | 53.80 ± 9.47 | 0.76 |
| Apolipoprotein B, mg/dL, mean (SD) | 71.53 ± 20.40 | 69.53 ± 17.29 | 61.44 ± 12.98 | 0.20 |
| Triglycerides, mg/dL, median (IQR) | 60.50 ± 37.00 | 58.50 ± 35.00 | 57.50 ± 29.50 | 0.61 |
| Systolic BP, mm Hg, mean (SD) | 104.23 ± 10.32 | 105.64 ± 10.92 | 107.87 ± 10.79 | 0.09 |
| Diastolic BP, mm Hg, mean (SD) | 65.11 ± 9.35 | 65.61 ± 9.63 | 64.10 ± 10.22 | 0.66 |
| BMI z score, mean (SD) | 0.54 ± 0.96 | 0.51 ± 0.97 | 0.66 ± 0.74 | 0.75 |
| Waist circumference, cm, mean (SD) | 77.33 ± 12.04 | 76.80 ± 12.93 | 77.57 ± 8.09 | 0.83 |
Abbreviations: BMI, body mass index; BP, blood pressure; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; IQR, interquartile range; LDL, low-density lipoprotein; SD, standard deviation.
ANOVA or Kruskal Wallis test or chi-square test. P value of 0.05 or less was highlighted in bold.
Figure 1.
The Mediterranean diet score assessed by the mKIDMED index at baseline, 1-year follow-up, and 5-year follow-up visits. Low, median and high quality had a mKIDMED score of ≤3, 4–7 and ≥8, respectively.
Figure 2.
The distribution of the mKIDMED score at baseline, 1-year follow-up, and 5-year follow-up visits (P=0.23). From top to bottom: maximum, 95th percentile, 75th percentile, median, 25th percentile, 5th percentile and minimum. P value based on Kruskal Wallis test.
Figure 3.
The distribution of the individual level change in mKIDMED score between three visits (P=0.84). From top to bottom: maximum, 95th percentile, 75th percentile, median, 25th percentile, 5th percentile and minimum. P value based on Kruskal Wallis test.
Models of cross-sectional associations between Mediterranean diet score and glycemic control and CVD risk factors are displayed in Table 2. In the fully-adjusted Model 2, a two-point higher mKIDMED score was associated with 4.0 mg/dL lower TC (P=0.006), 3.4 mg/dL lower LDL-C (P=0.004), 3.9 mg/dL lower non-HDL-C (P=0.004), and 0.07 lower LDL-C/HDL-C ratio (P=0.02). Due to the log-transformation of HbA1c for modeling, the mean value of HbA1c (about 8.0%; data not shown) in the sample was used for interpreting the result. Specifically, for an individual with an HbA1c level of 7.5%, a two-point higher mKIDMED score was associated with 0.15% lower HbA1c (P=0.02). Mediterranean diet was not associated with log-triglycerides, apolipoprotein B, BMI z score or waist circumference.
Table 2.
Cross-sectional associations between the Mediterranean diet score and glycemic control and cardiovascular risk factors
| Partially adjusted Model 1a
|
Fully adjusted Model 2b
|
HbA1c as a mediator: Model 3c
|
BMI z score as a mediator: Model 4d
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| βe | SE | Pf | βe | SE | Pf | βe | SE | Pf | βe | SE | Pf | |
| Log HbA1c, % | −0.01 | 0.01 | 0.42 | −0.02 | 0.01 | 0.02 | −0.02 | 0.01 | 0.04 | |||
| Lipids | ||||||||||||
| Total Cholesterol, mg/dL | −3.59 | 1.33 | 0.007 | −4.04 | 1.46 | 0.006 | −3.17 | 1.40 | 0.02 | −3.71 | 1.47 | 0.01 |
| LDL Cholesterol, mg/dL | −3.11 | 1.08 | 0.004 | −3.39 | 1.19 | 0.004 | −2.80 | 1.16 | 0.02 | −3.16 | 1.20 | 0.008 |
| HDL Cholesterol, mg/dL | −0.26 | 0.46 | 0.58 | −0.18 | 0.51 | 0.73 | −0.02 | 0.50 | 0.97 | −0.04 | 0.50 | 0.94 |
| LDL/HDL ratio | −0.05 | 0.03 | 0.03 | −0.07 | 0.03 | 0.02 | −0.06 | 0.03 | 0.03 | −0.07 | 0.03 | 0.01 |
| Non-HDL cholesterol, mg/dL | −3.34 | 1.21 | 0.006 | −3.86 | 1.32 | 0.004 | −3.15 | 1.28 | 0.01 | −3.67 | 1.33 | 0.006 |
| Log triglycerides, mg/dL | −0.01 | 0.02 | 0.68 | −0.02 | 0.02 | 0.34 | −0.01 | 0.02 | 0.54 | −0.02 | 0.02 | 0.27 |
| Apolipoprotein B, mg/dL | −1.22 | 1.01 | 0.23 | −0.82 | 1.08 | 0.45 | −0.60 | 1.01 | 0.55 | −0.54 | 1.09 | 0.62 |
| BPg | ||||||||||||
| Systolic BP, mm Hg | ||||||||||||
| P for interaction | 0.04 | 0.03 | 0.03 | 0.02 | ||||||||
| Non-Hispanic white | 0.98 | 0.44 | 0.03 | 1.21 | 0.46 | 0.009 | 1.25 | 0.47 | 0.008 | 1.18 | 0.45 | 0.009 |
| Other | −0.91 | 0.81 | 0.26 | −0.83 | 0.87 | 0.34 | −0.90 | 0.88 | 0.30 | −1.07 | 0.85 | 0.21 |
| Diastolic BP, mm Hg | 0.14 | 0.37 | 0.72 | 0.57 | 0.40 | 0.16 | 0.59 | 0.42 | 0.16 | 0.53 | 0.40 | 0.19 |
| Obesity | ||||||||||||
| BMI z score | 0.02 | 0.04 | 0.56 | 0.05 | 0.04 | 0.22 | 0.06 | 0.04 | 0.19 | |||
| Waist circumference, cm | −0.10 | 0.43 | 0.83 | 0.20 | 0.46 | 0.67 | 0.33 | 0.48 | 0.50 | |||
Abbreviations: BMI, body mass index; BP, blood pressure; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SE, standard error.
Model 1 adjusted for age, sex, race, diabetes duration, parental education, family income, parental history of diabetes, clinical site.
Model 2, model 1 + physical activity, sedentary behavior, smoking, total calories, insulin regimen, daily insulin dose per kilogram.
Model 3, model 2 + HbA1c.
Model 4, model 2 + BMI z score.
β for 2 points increment in mKIDMED score.
P value of 0.05 or less was highlighted in bold.
Height was additionally adjusted for BP.
Effect modification by race/ethnicity was found for systolic BP (Model 2, P=0.03) at baseline. A two-point higher mKIDMED score was associated unexpectedly with 1.2 mm Hg higher systolic BP (P=0.009) among non-Hispanic white youth, while systolic BP was 0.8 mm Hg lower but not significant (P=0.34) among children with “other” race/ethnicity. Gender was not an effect modifier for any outcomes. No association was found for diastolic BP.
Results from longitudinal mixed models are shown in Table 3. Based on the fully-adjusted Model 2, a two-point increase in mKIDMED score was associated with 1.8 mg/dL lower TC (P=0.05), 1.6 mg/dL lower LDL-C (P=0.03), and 1.8 mg/dL lower non-HDL-C (P=0.03) than would otherwise have been expected. For an individual with an HbA1c of 7.5% at one visit, his/her HbA1c would be dropped to 7.43% (P=0.07) for a two-point increase in mKIDMED score at the next visit. No association was found between mKIDMED score and HDL-C, LDL-C/HDL-C ratio, log-triglycerides, BP, BMI z score or waist circumference.
Table 3.
Longitudinal mixed modeling results for associations of the Mediterranean diet score and glycemic control and cardiovascular risk factors
| Partially adjusted Model 1a
|
Fully adjusted Model 2b
|
HbA1c as a mediator: Model 3c
|
BMI z score as a mediator: Model 4d
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| βe | SE | Pf | βe | SE | Pf | βe | SE | Pf | βe | SE | Pf | |
| Log HbA1c, % | −0.01 | 0.01 | 0.34 | −0.01 | 0.01 | 0.07 | −0.01 | 0.01 | 0.12 | |||
| Lipids | ||||||||||||
| Total Cholesterol, mg/dL | −1.94 | 0.82 | 0.02 | −1.81 | 0.91 | 0.05 | −1.41 | 0.86 | 0.11 | −1.71 | 0.91 | 0.06 |
| LDL Cholesterol, mg/dL | −1.56 | 0.63 | 0.01 | −1.56 | 0.69 | 0.03 | −1.28 | 0.66 | 0.06 | −1.49 | 0.69 | 0.03 |
| HDL Cholesterol, mg/dL | −0.13 | 0.29 | 0.66 | −0.16 | 0.32 | 0.62 | −0.14 | 0.32 | 0.66 | −0.14 | 0.32 | 0.67 |
| LDL/HDL ratio | −0.02 | 0.02 | 0.14 | −0.02 | 0.02 | 0.18 | −0.02 | 0.02 | 0.33 | −0.02 | 0.02 | 0.18 |
| Non-HDL cholesterol, mg/dL | −1.92 | 0.75 | 0.01 | −1.81 | 0.83 | 0.03 | −1.37 | 0.78 | 0.08 | −1.71 | 0.83 | 0.04 |
| Log triglycerides, mg/dL | −0.01 | 0.01 | 0.28 | −0.01 | 0.01 | 0.58 | −0.0003 | 0.01 | 0.98 | −0.01 | 0.01 | 0.57 |
| BPg | ||||||||||||
| Systolic BP, mm Hg | 0.17 | 0.25 | 0.49 | 0.31 | 0.27 | 0.26 | 0.32 | 0.28 | 0.25 | 0.26 | 0.26 | 0.33 |
| Diastolic BP, mm Hg | 0.03 | 0.24 | 0.91 | 0.25 | 0.26 | 0.34 | 0.17 | 0.27 | 0.52 | 0.22 | 0.26 | 0.40 |
| Obesity | ||||||||||||
| BMI z score | −0.01 | 0.02 | 0.61 | 0.01 | 0.02 | 0.51 | 0.02 | 0.02 | 0.44 | |||
| Waist circumference, cm | −0.14 | 0.22 | 0.52 | 0.11 | 0.23 | 0.63 | 0.18 | 0.24 | 0.46 | |||
Abbreviations: BMI, body mass index; BP, blood pressure; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SE, standard error.
Model 1 adjusted for age, sex, race, diabetes duration, parental education, family income, parental history of diabetes, clinical site.
Model 2, model 1 + physical activity, sedentary behavior, smoking, total calories, insulin regimen, daily insulin dose per kilogram.
Model 3, model 2 + HbA1c.
Model 4, model 2 + BMI z score.
β for 2 points increase in mKIDMED score between visits.
P value of 0.05 or less was highlighted in bold.
Height was additionally adjusted for BP.
HbA1c mediated about 20% of the associations for lipids both in cross-sectional (P=0.02) and longitudinal models (P=0.07). BMI z score attenuated ≤8% of the associations for lipids both in baseline and longitudinal models
DISCUSSION
Our study revealed that a very low percentage of youth adhered to a Mediterranean style diet in this large incident T1D cohort in the US. Higher Mediterranean diet score was cross-sectionally associated with lower HbA1c and improved lipid profile. Increased Mediterranean diet score across time was longitudinally associated with improved lipid profile and marginally improved HbA1c. Additionally, HbA1c mediated about 20% of the effect of a Mediterranean diet on lipids.
In SEARCH, beneficial associations between the Dietary Approaches to Stop Hypertension (DASH) diet and CVD risk factors and glycemic control were reported among T1D youth.14,22,23 A favorable association was found between the DASH diet and lipids only in cross-sectional analyses while, reported herein, a Mediterranean diet was inversely associated with lipids both cross-sectionally and longitudinally. Of note, the previous longitudinal analyses of the DASH diet had a markedly smaller sample.23 The DASH diet and Mediterranean diet were beneficial for HbA1c in both cross-sectional and longitudinal analyses.14,23 The DASH diet was inversely associated with hypertension,22 whereas such a beneficial effect on hypertension was not observed for a Mediterranean diet in our study. Although similar food groups comprise both dietary patterns, there are subtle differences that may explain disparate findings between two diets. The type of fats consumed is emphasized in the mKIDMED index and fast food consumption is scored into the mKIDMED index, but not the DASH diet score. Fruit and vegetable intake are emphasized to a greater extent in the mKIDMED index with a total of four scored items compared to two in the DASH diet score. The benefits of increased MUFA/SFA ratio,24 fruits and vegetables,25 and detrimental effect of fast foods,26 on CVD risk factors have been well documented.
We found significant inverse associations between a Mediterranean diet and TC, LDL-C and non-HDL-C in both cross-sectional and longitudinal models. The lipid-lowering effect of a Mediterranean diet on children was previously reported. In a 6-month prospective cohort study of 96 children with T1D following a structured dietitian training to a Mediterranean diet,27 the reduction of LDL-C and non-HDL-C for about 9 mg/dL was similar to our cross-sectional results, if the mKIDMED score was increased from a mean score of 3.6 to the lowest score of 8 in the high mKIDMED score category (Calculation details: The betas for LDL-C and non-HDL-C were −3.39 mg/dL and −3.86 mg/dL, respectively, which was based on an increase of mKIDMED score of 2 (Table 2). A 4.4 increase in mKIDMED score would be associated with 7.46 mg/dL lower LDL-C and 8.49 mg/dL lower non-HDL-C.). However, in a 12-month Mediterranean diet intervention on 36 pre-pubertal hypercholesterolemic children,28 the reduction of TC and LDL-C was about 25 mg/dL, much greater than the reduction in our study. Of note, the mean baseline TC level (260.6 versus 159 mg/dL) and LDL-C level (182.0 versus 93.3 mg/dL) were much higher among hypercholesterolemic children as compared to those in our study participants. We found that about 20% of the association with lipids was mediated by HbA1c in both cross-sectional and longitudinal models. It has been shown that, in youth with T1D, improved HbA1c over a two-year follow-up was associated with improved lipid profile.29 BMI z score was not a mediator in our data. There may be additional pathways linking a Mediterranean diet with lipids independent of HbA1c and weight.
The reduction of HbA1c by about 0.1–0.2% in youth with T1D was very similar between DASH and Mediterranean diets in SEARCH,14,23 which was smaller than that from a meta-analysis of randomized trials (0.47%, 95% confidence interval: 0.30–0.64%)30 and observational studies31 in adult type 2 patients. A 6-month structured dietitian training on T1D children to a Mediterranean diet improved HbA1c by about 0.2% in males, but not in females.27 Thus, a somewhat smaller effect on HbA1c was consistently observed in T1D children. The complex impact of macronutrients in the context of various dietary patterns on glycemic excursions post meal in T1D is not well understood.32 Thus, the full benefits of either the DASH or Mediterranean diet will not be realized until appropriate insulin dosing for these diets could be designed.
An unexpected positive association between a Mediterranean diet and systolic BP was identified using baseline data among non-Hispanic white youth, but not among youth with other racial/ethnic backgrounds. In children, evidence is scant and inconsistent regarding the association between a Mediterranean diet and BP.33,34 Two studies also found a positive association for systolic BP: Giannini et al.28 did not discuss this finding; the Leontio Lyceum Albuminuria (3L) Study34 hypothesized that obesity-related increase in systolic BP exceeds Mediterranean diet’s hemodynamically favorable effects in children. However, systolic BP still remained significant after accounting for BMI in the 3L study, as in our study. In adults, the BP-lowering effect of a Mediterranean diet9 was similar to the unrestricted-sodium DASH diet,35 but was less than the restricted-sodium DASH diet.36 None of the studies in children discussed considered the effect of dietary sodium on the association with BP, which may be one of main reasons for the inconsistent or unexpected findings. The SEARCH FFQ was not intended to assess sodium intake and did not include important sources of sodium in the diet (e.g., use of salt at the table).
The main strengths of our study were a large sample of T1D cases with follow-up data up to 5 years, inclusion of only incident cases to avoid confounding by factors associated with disease duration, extensive control of confounding and careful assessment of mediation and effect modification. Limitations should also be noted. First, although the SEARCH FFQ itself was validated,16 the original KIDMED index could not be exactly replicated. Thus, the derived mKIDMED score may not perfectly represent traditional Mediterranean dietary pattern. However, our approach to generate this score was consistent with that of other investigators.18,19 Second, some misclassification of the Mediterranean diet score was possible due to the assessment of dietary intake by a FFQ. However, it is unlikely that such misclassification would be differential as regard to the outcomes evaluated.14 Third, loss-to follow-up may have influenced our findings. However, participants who had one visit only were not different from those with one or two additional follow-up visits, in terms of age, gender, duration of diabetes, family history of diabetes, insulin dosage, smoking status, BMI z score and total daily dietary energy (Appendix Table 1). Fourth, only a small number of participants had high mKIDMED score, so we were unable to explore the threshold effect at high end of the mKIDMED score if such existed. Finally, we did not explicitly adjust for multiple comparisons. Given the large number of associations studied, we cannot ignore the possibility that some associations may be the result of type 1 error. The interpretation of these findings should consider both their theoretical grounding and results of the previous studies.23,27,28,34
In conclusion, higher Mediterranean diet score was associated with better glycemic control and lipid profile in youth with T1D. The effect of a Mediterranean diet on lipids was mediated in part through HbA1c. Randomized clinical trials are warranted to confirm the beneficial effects of a Mediterranean diet on glycemic control and lipids in T1D youth. Such trials need to carefully address issues related to insulin dosing and day-to-day glycemic control in the context of a Mediterranean diet, and need to address dietary sodium with respect to BP outcomes.
Supplementary Material
Acknowledgments
Sources of Support
Supported by research grants (R01 DK077949) from the NIH/National Institute of Diabetes and Digestive and Kidney Diseases, (PA numbers 00097, DP-05-069, and DP-10-001) from the CDC, and (DK056350) from the NIH, and supported by the Sanofi Global Scholars Program.
Footnotes
AUTHOR CONTRIBUTIONS
VWZ, APL and EJM-D designed research; VWZ and APL conducted research; VWZ and JLC analyzed data; VWZ wrote the paper; EJM-D had primary responsibility for final content. All authors read and approved the final manuscript, and contributed to the revision of the manuscript critically for important intellectual content.
CONFLICT OF INTEREST
VWZ received financial support from the Sanofi Global Scholars Program. All other authors declare no conflict of interest.
References
- 1.Dahl-Jorgensen K, Larsen JR, Hanssen KF. Atherosclerosis in childhood and adolescent type 1 diabetes: early disease, early treatment? Diabetologia. 2005;48:1445–1453. doi: 10.1007/s00125-005-1832-1. [DOI] [PubMed] [Google Scholar]
- 2.de Ferranti SD, de Boer IH, Fonseca V, Fox CS, Golden SH, Lavie CJ, et al. Type 1 diabetes mellitus and cardiovascular disease: a scientific statement from the American Heart Association and American Diabetes Association. Circulation. 2014;130:1110–1130. doi: 10.1161/CIR.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 3.Petitti DB, Klingensmith GJ, Bell RA, Andrews JS, Dabelea D, Imperatore G, et al. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr. 2009;155:668–72.e1. doi: 10.1016/j.jpeds.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10:293–302. doi: 10.1038/nrendo.2014.29. [DOI] [PubMed] [Google Scholar]
- 5.Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673–1686. doi: 10.1161/CIRCULATIONAHA.110.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K American Heart Association. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107:1562–1566. doi: 10.1161/01.cir.0000061521.15730.6e. [DOI] [PubMed] [Google Scholar]
- 7.Mikkila V, Rasanen L, Laaksonen MM, Juonala M, Viikari J, Pietinen P, et al. Long-term dietary patterns and carotid artery intima media thickness: the Cardiovascular Risk in Young Finns Study. Br J Nutr. 2009;102:1507–1512. doi: 10.1017/S000711450999064X. [DOI] [PubMed] [Google Scholar]
- 8.Serra-Majem L, Roman B, Estruch R. Scientific evidence of interventions using the Mediterranean diet: a systematic review. Nutr Rev. 2006;64:S27–47. doi: 10.1111/j.1753-4887.2006.tb00232.x. [DOI] [PubMed] [Google Scholar]
- 9.Estruch R, Martinez-Gonzalez MA, Corella D, Salas-Salvado J, Ruiz-Gutierrez V, Covas MI, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145:1–11. doi: 10.7326/0003-4819-145-1-200607040-00004. [DOI] [PubMed] [Google Scholar]
- 10.Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359:229–241. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 11.Estruch R, Ros E, Salas-Salvadó J, Covas M, Corella D, Arós F, et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 12.SEARCH Study Group. SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials. 2004;25:458–471. doi: 10.1016/j.cct.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 14.Liese AD, Bortsov A, Gunther AL, Dabelea D, Reynolds K, Standiford DA, et al. Association of DASH diet with cardiovascular risk factors in youth with diabetes mellitus: the SEARCH for Diabetes in Youth study. Circulation. 2011;123:1410–1417. doi: 10.1161/CIRCULATIONAHA.110.955922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayer-Davis EJ, Nichols M, Liese AD, Bell RA, Dabelea DM, Johansen JM, et al. Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J Am Diet Assoc. 2006;106:689–697. doi: 10.1016/j.jada.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Liese AD, Crandell JL, Tooze JA, Fangman MT, Couch SC, Merchant AT, et al. Relative validity and reliability of an FFQ in youth with type 1 diabetes. Public Health Nutr. 2014:1–10. doi: 10.1017/S1368980014000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Serra-Majem L, Ribas L, Ngo J, Ortega RM, Garcia A, Perez-Rodrigo C, et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004;7:931–935. doi: 10.1079/phn2004556. [DOI] [PubMed] [Google Scholar]
- 18.Fung TT, McCullough ML, Newby PK, Manson JE, Meigs JB, Rifai N, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82:163–173. doi: 10.1093/ajcn.82.1.163. [DOI] [PubMed] [Google Scholar]
- 19.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 20.Chatterjee R, Yeh HC, Shafi T, Anderson C, Pankow JS, Miller ER, et al. Serum potassium and the racial disparity in diabetes risk: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Clin Nutr. 2011;93:1087–1091. doi: 10.3945/ajcn.110.007286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singer JD. Using SAS PROC MIXED to Fit Multilevel Models, Hierarchical Models, and Individual Growth Models. J Educ Behav Stat. 1998;23:323–355. [Google Scholar]
- 22.Gunther AL, Liese AD, Bell RA, Dabelea D, Lawrence JM, Rodriguez BL, et al. Association between the dietary approaches to hypertension diet and hypertension in youth with diabetes mellitus. Hypertension. 2009;53:6–12. doi: 10.1161/HYPERTENSIONAHA.108.116665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnes TL, Crandell JL, Bell RA, Mayer-Davis EJ, Dabelea D, Liese AD. Change in DASH diet score and cardiovascular risk factors in youth with type 1 and type 2 diabetes mellitus: The SEARCH for Diabetes in Youth Study. Nutr Diabetes. 2013;3:e91. doi: 10.1038/nutd.2013.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baggio G, Pagnan A, Muraca M, Martini S, Opportuno A, Bonanome A, et al. Olive-oil-enriched diet: effect on serum lipoprotein levels and biliary cholesterol saturation. Am J Clin Nutr. 1988;47:960–964. doi: 10.1093/ajcn/47.6.960. [DOI] [PubMed] [Google Scholar]
- 25.Djousse L, Arnett DK, Coon H, Province MA, Moore LL, Ellison RC. Fruit and vegetable consumption and LDL cholesterol: the National Heart, Lung, and Blood Institute Family Heart Study. Am J Clin Nutr. 2004;79:213–217. doi: 10.1093/ajcn/79.2.213. [DOI] [PubMed] [Google Scholar]
- 26.Duffey KJ, Gordon-Larsen P, Steffen LM, Jacobs DR, Jr, Popkin BM. Regular consumption from fast food establishments relative to other restaurants is differentially associated with metabolic outcomes in young adults. J Nutr. 2009;139:2113–2118. doi: 10.3945/jn.109.109520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cadario F, Prodam F, Pasqualicchio S, Bellone S, Bonsignori I, Demarchi I, et al. Lipid profile and nutritional intake in children and adolescents with Type 1 diabetes improve after a structured dietician training to a Mediterranean-style diet. J Endocrinol Invest. 2012;35:160–168. doi: 10.3275/7755. [DOI] [PubMed] [Google Scholar]
- 28.Giannini C, Diesse L, D’Adamo E, Chiavaroli V, de Giorgis T, Di Iorio C, et al. Influence of the Mediterranean diet on carotid intima-media thickness in hypercholesterolaemic children: a 12-month intervention study. Nutr Metab Cardiovasc Dis. 2014;24:75–82. doi: 10.1016/j.numecd.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 29.Maahs DM, Dabelea D, D’Agostino RB, Jr, Andrews JS, Shah AS, Crimmins N, et al. Glucose control predicts 2-year change in lipid profile in youth with type 1 diabetes. J Pediatr. 2013;162:101–7.e1. doi: 10.1016/j.jpeds.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013;97:505–516. doi: 10.3945/ajcn.112.042457. [DOI] [PubMed] [Google Scholar]
- 31.Esposito K, Maiorino MI, Di Palo C, Giugliano D Campanian Postprandial Hyperglycemia Study Group. Adherence to a Mediterranean diet and glycaemic control in Type 2 diabetes mellitus. Diabet Med. 2009;26:900–907. doi: 10.1111/j.1464-5491.2009.02798.x. [DOI] [PubMed] [Google Scholar]
- 32.Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2013;36:3821–3842. doi: 10.2337/dc13-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lazarou C, Panagiotakos DB, Matalas AL. Lifestyle factors are determinants of children’s blood pressure levels: the CYKIDS study. J Hum Hypertens. 2009;23:456–463. doi: 10.1038/jhh.2008.151. [DOI] [PubMed] [Google Scholar]
- 34.Mazaraki A, Tsioufis C, Dimitriadis K, Tsiachris D, Stefanadi E, Zampelas A, et al. Adherence to the Mediterranean diet and albuminuria levels in Greek adolescents: data from the Leontio Lyceum ALbuminuria (3L study) Eur J Clin Nutr. 2011;65:219–225. doi: 10.1038/ejcn.2010.244. [DOI] [PubMed] [Google Scholar]
- 35.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 36.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.