Abstract
Background
Whereas stigma regarding mental health concerns exists, the evidence for stigma as a depression treatment barrier among patients in Veterans Affairs (VA) primary care (PC) is mixed.
Purpose
To test whether stigma, defined as depression label avoidance, predicted patients' preferences for depression treatment providers, patients' prospective engagement in depression care, and care quality.
Methods
We conducted cross-sectional and prospective analyses of existing data from 761 VA PC patients with probable major depression.
Results
Relative to low stigma patients, those with high stigma were less likely to prefer treatment from mental health specialists. In prospective controlled analyses, high stigma predicted lower likelihood of the following: taking medications for mood, treatment by mental health specialists, treatment for emotional concerns in PC, and appropriate depression care.
Conclusions
High stigma is associated with lower preferences for care from mental health specialists and confers risk for minimal depression treatment engagement.
Keywords: Depression, stigma, treatment preferences, treatment engagement, primary care, Veterans
Estimates suggest that 7% of the US adult population experiences a major depressive episode each year, and that nearly 1 in 3 persons will experience an episode in their lifetimes (1,2). Although effective treatments exist (3,4), many people with depression do not seek care (5), and only a minority of those who do receive appropriate care (6). Because depression is a leading cause of disability worldwide (7), improved understanding of depression care barriers is necessary to improve global health.
Though the US Surgeon General identified stigma as a primary reason that people avoid mental health care (8), many conceptions and types of mental health stigma exist. As described by Jones and Corrigan (9), these conceptions include public stigma, self-stigma, and label avoidance. Public stigma is understood as widely-held negative stereotypes regarding people with mental illness, while self-stigma represents the belief in these public stereotypes by a person with mental illness (9). Label avoidance stems from efforts to buffer the effects of public and self-stigma. In the case of label avoidance, fear of the psychiatric labels (e.g., depression) that confer stigma may lead people with mental health concerns to avoid the health care system and to reject diagnoses (9-13).
Stigma and depression care
The knowledge base regarding stigma and mental health care is growing rapidly, with existing work presenting considerable methodological variability and variability in operational definitions of stigma. As findings using different measures and methods accumulate, it can become difficult to ascertain when and how stigma impedes care seeking. Brohan and colleagues (14) reviewed the stigma literature spanning the years 1990-2009 and found that research more frequently examined perceived/public stigma than self-stigma. Self-report measurement of public stigma is exemplified by scales like The Perceived Devaluation and Discrimination Scale (15), a measure of respondents' beliefs regarding the general public's discriminatory behavior against and negative attitudes toward people with mental illness. Measures like the Self-Stigma of Mental Illness Scale (16) assess self-stigma by gauging the degree to which participants agree that mental illness stereotypes describe their own experiences. It is important to note that, despite its conceptual relevance for treatment engagement, Brohan et al.'s review did not reveal any studies of label avoidance.
Research based on hypothetical vignettes and surveys of attitudes, intention to seek treatment, and general concerns about depression care implicate stigma—defined in various ways—as a treatment barrier. For example, large proportions of the general public report that they would feel embarrassment or experience negative judgment if they were to discuss depression with care providers (17,18), and one in five worries that depression treatment might compromise work opportunities (18). A positive association between stigma and people's perceptions of their unmet mental health care needs also suggests that high stigma is related to perceived treatment inadequacy (19). In addition, high stigma has been linked to lower self-reported likelihood of seeking professional help for mental health concerns and depression (20-22). Finally, in vignette studies, people with depression who seek treatment are perceived more negatively than depressed persons who avoid it (23).
Although informative, most studies of attitudes and intent to seek care do not examine care behavior. As others have noted (22,24), relatively few studies examine stigma and care-seeking behavior specifically, and those that do so present mixed findings. Among college students, for example, there was no relationship between public stigma and help-seeking in those with probable depression and/or anxiety (24), but higher levels of self-stigma were associated with lower use of formal treatments (i.e., medication and/or psychotherapy) and mental health support from informal sources (i.e., friends, family, support groups, clergy) (25). Finally, naturalistic prospective investigations by Sirey and colleagues demonstrate that high stigma at the outset of depression treatment predicts lower adherence over time (26) and premature treatment dropout among older patients (27). Sirey and colleagues suggest that stigma hampers treatment and that poor adherence and early treatment dropout may result from patients' attempts to reject a devalued outgroup status (26).
Stigma and mental health care among Veterans
While some evidence suggests that stigma impedes mental health care, specific care barriers may exist in individual health care systems and stigma may function differently across patient populations. Because former and current military personnel differ from the general population in many ways, it is important to understand how they experience stigma and how it impacts their mental health care engagement. Moreover, the high prevalence of mental health concerns, like PTSD and depression, among Veterans (28) highlights the importance of understanding barriers to mental health care in this unique population.
Recent research indicates that the mental health care needs of military personnel and Veterans are only partially met (28,29). Stigma and logistical barriers represent significant separable deterrents to care, each with potential to confer suboptimal treatment engagement (30). Concerns regarding stigma are clearly evident among returning service members and Veterans (28,31,32) and range higher among those with significant mental health concerns than among those without them (28,33). Relative to admission of physical health problems, soldiers are more concerned that disclosing mental health concerns would negatively impact career opportunities, and that disclosure would lead peers to view them negatively (34).
The recent literature regarding stigma and mental health care among Veterans offers mixed findings, with some work suggesting that stigma inhibits care, and other work finding that it does not. For example, Veterans Affairs (VA) patients with PTSD who are not seeking mental health treatment described stigma as “slightly” to “moderately” problematic and rated it as a more salient care barrier than logistical or institutional barriers (35). Researchers have also documented links between stigma and lower self-reported intention to seek mental health care in other VA and military samples (36,37). Finally, a qualitative analysis suggested that treatment-seeking Veterans with PTSD believed that the public holds negative stereotypical beliefs about those with mental health concerns (38). These Veterans also feared that those with PTSD would be labeled “crazy” or held responsible by others for their mental health conditions, and many participants reported that stigma and fear of being labeled influenced their own treatment avoidance (38).
In contrast, other recent studies failed to observe treatment inhibiting effects for stigma. In a sample of returning soldiers, stigma did not predict psychotherapy use or use of medication (31). Similarly, Rosen and colleagues (39) found that stigma did not inhibit initiation of psychotherapy among Veterans with PTSD, and to the contrary, higher stigma predicted more intensive treatment among psychotherapy attendees. In a sample of National Guard service personnel and reservists, more strongly held negative beliefs about mental health care were associated with worse stigma and with decreased likelihood of counseling and medication use, but it was unclear whether stigma was related directly to treatment seeking (33).
Finally, some researchers have demonstrated that patient-based and/or illness characteristics might overshadow stigma's effects on treatment seeking. In separate prospective analyses, stigma failed to predict mental health service use beyond the effects attributable to personality (40), and PTSD and depressive severity predicted mental health service use initiation and retention, while stigma and other potential care barriers did not (41). These findings mirrored work from a non-military primary care sample, which found that the relationship between stigma and mental health service use was mediated by depressive severity (42).
In summary, data drawn from the general population and from former and current military service personnel suggest that negative attitudes regarding people with depression and other mental health concerns persist. Though stigma—defined differently across studies— demonstrates a link with self-reported intent to seek care, the role of stigma as an inhibitor of actual mental health service use is not entirely clear (e.g., 32). Further study is needed, and as leading stigma researchers have highlighted, there exists a particularly pressing need for studies that examine stigma and service use prospectively, while controlling for illness severity (10). Finally, nearly all existing studies have examined public and/or self-stigma, and while this work is informative, label avoidance, a stigma type with clear implications for treatment seeking (9), is less well studied. Existing qualitative studies link diagnostic label avoidance and mental health treatment seeking (38,43) and some propose label avoidance as a reason for poor treatment adherence (26,44), but to date no published studies have attempted to measure label avoidance explicitly and tested its relation to care seeking. Indeed, leading stigma researchers maintain that considerably less is known about label avoidance than other types of stigma and that label avoidance research is needed (9,45).
Current Study
In this study, we defined stigma as label avoidance and tested whether it hinders depression treatment in a sample of VA primary care patients with probable major depression. Our definition of stigma as label avoidance follows from the work of others (9,45) and aligns with Relational Frame Theory principles that describe how language (e.g., the term “depression” in the current study) establishes in- and out-groups and initiates stigma and prejudice (46,47). We tested specifically whether stigma demonstrated a concurrent association with openness to depression treatment from particular provider types at baseline and whether stigma predicted patients' depression treatment behavior and care quality seven months later. We expected high stigma at baseline to relate to lower openness to specialty mental health care (i.e., psychiatrists, psychologists/social workers). We also hypothesized that high baseline stigma would predict lower depression treatment engagement (e.g., use of medications for mood, visits to specialty mental health providers, etc.) and lower likelihood of appropriate depression care seven months later.
Methods
Sample and Setting
The study sample consisted of patients that participated in the Well-being among Veterans Enhancement Study (WAVES), a group randomized-controlled trial of depression collaborative care management. WAVES included patients with probable major depression from one of 10 VA PC clinics from five states (Florida, Ohio, South Dakota, Texas, and Wisconsin) spanning three VA administrative regions. Participating PC clinics employed between 4 and 13 PC providers and served between 3,900 and 13,000 patients annually (48,49). Because WAVES was designed to test practice level impacts of collaborative care management, seven practices implemented depression collaborative care management and three PC practices provided depression care as usual (48). Patients from all clinics participating in WAVES were included in the present study. Participants provided oral informed consent for study participation; Institutional Review Boards at participating VA facilities approved all WAVES procedures.
WAVES used visit-based sampling in order to recruit a sample that closely resembled the population of patients with major depression who are seen in practice. Patients were eligible for inclusion if they had attended one of the 10 study clinics within 12 months and had an upcoming PC visit scheduled. No exclusions were made on the basis of age, gender, race/ethnicity or health status. To generate the sample, research personnel at participating clinics provided contact information for eligible patients to a contracted survey research firm; the firm then mailed these patients a description of the study as well as preaddressed/postpaid postcards and a toll-free number for participants to use for study refusal. Ten days after mailing the invitation letters, interviewers from the survey research firm contacted patients and initiated study inclusion screening using computer-assisted telephone interviewing.
Using computer-assisted methods, trained interviewers initiated screening for major depressive episode symptomatology with 10,929 Veterans via the first two items (PHQ-2) (50) of the Patient Health Questionnaire-9 (PHQ-9), a self-report measure of depression (51). Roughly 20% of the screened patients achieved positive PHQ-2 screens. Of the 2,122 patients who agreed to complete the full PHQ-9, 1,313 (61.9%) had probable major depression and met the WAVES depression inclusion criterion. Ultimately, 761 patients (58.0% of eligible) experiencing a probable major depressive episode completed the full WAVES baseline assessment. Baseline assessments were conducted by telephone between 2003 and 2004. Follow-up assessments with 546 patients (71.7% of baseline) were conducted by trained interviewers using computer-assisted telephone interviewing at seven months. In addition, 506 participants (66% of baseline) consented to use of VA administrative healthcare utilization data; these data were merged with the WAVES baseline and 7-month surveys.
Measures
Depression
The PHQ-9 (51) is a depression measure designed for use in PC. Respondents indicated the 2-week frequency of each of the nine DSM-IV (52) symptoms of a major depressive episode using a scale ranging from 0 (“not at all”) to 3 (“nearly every day”). Total PHQ-9 scores range from 0-27; scores of 10 and greater have high sensitivity (.88) and specificity (.88) for Major Depressive Disorder (51). The PHQ-9 was used to determine WAVES eligibility (i.e., PHQ-9 ≥ 10). The measure's sum also provided an indicator of depressive severity, with higher scores denoting worse depression.
Stigma
The WAVES survey assessed depression label avoidance by asking participants about the degree to which they would accept a depression label from their physician. Using a Likert scale (1=“Strongly Agree” to 5=“Strongly Disagree”), participants indicated their degree of agreement with the statement: “If your doctor told you [that] you had depression, you would accept that.” Responses were dichotomized, with label avoidance and high stigma represented by responses of Disagree and Strongly Disagree and low stigma represented by all other responses. On this face valid indicator, therefore, patients with high stigma were identified as those who reported they would not accept a depression label.
Treatment provider preferences
Participants' preferences for depression treatment at baseline were assessed with the following question: “If you were depressed… and could choose who would help you with these problems, how likely would you be to choose each of the following providers?” Using a scale ranging from 1=“Very Likely” to 5=“Very Unlikely,” patients indicated their openness to treatment from a primary care physician, a psychiatrist, an other mental health specialist (i.e., psychologist, social worker, psychiatric nurse practitioner), and a spiritual counselor. Treatment preference variables were dichotomized, with Very Likely and Likely responses indicating preference for treatment from a particular provider type, and all other responses indicating non-preference.
Patient Recall of Provider behavior
At the seven-month follow-up, those participants who reported any PC visit in the previous six months were asked questions about their primary care provider's behavior. We inquired separately about whether the participants' primary care providers had asked about sadness or depression, thoughts about self-harm, or improvement in depression. We also assessed whether primary care providers had recommended counseling by another doctor, prescribed or refilled a medication for an emotional problem, and adjusted an existing medication for an emotional problem. Although it would have been helpful to know whether primary care providers had asked patients about their willingness to discuss depression or accept a prescription for emotional concerns, these questions were not included. All responses to the questions about patients' recall of primary care providers' behavior were dichotomous (“yes” v. “no”).
Care behavior/engagement at seven months
Several dichotomized variables from the self-report survey assessed participants' engagement in care at seven months. Respondents indicated whether they had taken medication and whether they had attended any outpatient visit (VA or non-VA) for an emotional problem. They also indicated whether they had had one or more visit (in-person or by telephone) with a specialty mental health provider. Those who reported specialist contact indicated separately whether they had seen a psychiatrist, a psychologist, or a social worker. Finally, as described elsewhere (48) we constructed an indicator of appropriate depression care at 7-month follow-up. Appropriate care was defined a current antidepressant medication and/or at least four visits in the previous 6 months with a mental health specialist.
A VA administrative database (i.e., the VA Outpatient Care file) provided additional information about care engagement at seven months. Two dichotomous variables indicated whether patients had received any individual or group visits in specialty mental health settings, and a separate count variable indicated the number of individual visits the patient had in the previous six months for specialty mental health care.
Data Analysis
Descriptive statistics illustrated demographic characteristics at baseline and seven month follow-up, provider preferences at baseline, treatment receipt/engagement, and provider behavior at seven months. Bivariate relationships between stigma and treatment preferences at baseline, treatment receipt/engagement at seven months, and provider behavior at seven months were examined using the χ2 test. The study's primary hypotheses regarding stigma's concurrent and prospective prediction of the outcomes (i.e., treatment preferences, treatment engagement and provider behavior) were tested with a series of covariate controlled multivariable logistic regression analyses. The regression models included age, gender, education (high school or less v. greater than high school), and depressive severity as covariates, as these variables demonstrated significant associations with stigma and/or care variables at baseline. Regression models were fit for the 11 preferences and care variables that demonstrated a significant relationship with stigma in the bivariate analyses. Alphas of ≤ .05 designated statistical significance.
Results
Demographic characteristics
Table 1 presents demographic characteristics of the 761 PC patients with probable major depression who composed the baseline sample. Participants' average age was 60.4 years (sd=11.9); 715 (94%) participants were male, and 646 (85%) were White/non-Hispanic. Roughly half of the sample (n=385) completed some education beyond high school, while just over 60% (n=457) of participants were married or living as married. Relatively few participants were employed part- or fulltime (17.1%). Most participants reported being in poor health, and only 149 (19.1%) described their health as “good” or better using a single item from the Health Status Questionnaire (53).
Table 1.
Demographic characteristics and depression treatment preferences at baseline, care behavior/engagement and provider behavior at 7 months for the entire sample and by high versus low stigma.
| Label Avoidance | p-value | ||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Overall | Low Stigma | High Stigma | |||||
| mean | SD | mean | SD | mean | SD | ||
| Demographic and health characteristics: baseline (n=761) | |||||||
| Age (years) | 60.3 | 11.9 | 59.8 | 11.7 | 66.6 | 12.0 | <.001 |
| Depression (PHQ-9 Sum) | 15.8 | 4.3 | 16.0 | 4.3 | 14.6 | 3.6 | <.05 |
| n | % | n | % | n | % | ||
| Gender (female) | 46 | 6.0 | 42 | 6.0 | 2 | 3.3 | 0.39 |
| Race/ethnicity (White, Non-Hispanic) | 630 | 82.8 | 578 | 83.3 | 51 | 86.4 | 0.53 |
| Education (high school or less) | 376 | 49.4 | 340 | 48.8 | 34 | 56.7 | 0.24 |
| General Health (Good or better) | 149 | 19.6 | 135 | 19.4 | 14 | 23.3 | 0.27 |
| Treatment preferences: baseline (n=761) | |||||||
| PC physician | 498 | 65.4 | 456 | 66.7 | 41 | 68.3 | 0.79 |
| Psychiatrist | 486 | 63.9 | 466 | 67.2 | 18 | 30.5 | <.001 |
| Another mental health specialist | 506 | 66.5 | 481 | 69.6 | 23 | 38.3 | <.001 |
| Spiritual Counselor/Clergy | 359 | 47.2 | 329 | 47.3 | 29 | 48.3 | 0.88 |
| Care behavior at 7 months (n=546) | |||||||
| At least one PC visit | 489 | 89.6 | 447 | 89.8 | 40 | 87.0 | 0.55 |
| Take medication for emotional problem | 353 | 64.7 | 343 | 68.6 | 10 | 21.7 | <.001 |
| Any PC visit for emotional health | 253 | 46.4 | 243 | 48.8 | 9 | 19.6 | <.001 |
| Any mental health provider visit | 295 | 54.4 | 287 | 57.9 | 8 | 17.4 | <.001 |
| Visit with psychiatrist | 210 | 73.2 | 207 | 73.3 | 3 | 42.9 | 0.07 |
| Visit with psychologist | 125 | 44.2 | 124 | 45.1 | 1 | 12.5 | 0.07 |
| Visit with social worker | 108 | 37.4 | 106 | 37.7 | 2 | 25.0 | 0.46 |
| Appropriate care (mental health specialist and/or meds) | 269 | 49.5 | 262 | 52.6 | 7 | 15.2 | <.001 |
| Care at 7 Months (administrative data) | |||||||
| Any mental health specialist individual visits | 251 | 46.5 | 246 | 49.8 | 5 | 10.9 | <.001 |
| Any mental health group visits | 51 | 9.5 | 50 | 10.1 | 1 | 2.2 | 0.08 |
| Provider behavior at 7 Months | |||||||
| Asked about sadness/depression | 280 | 58.0 | 261 | 58.8 | 19 | 48.7 | 0.22 |
| Asked about self-harm | 203 | 42.3 | 193 | 43.9 | 10 | 25.0 | 0.02 |
| Asked about depression improvement | 203 | 42.2 | 194 | 44.0 | 9 | 22.5 | 0.008 |
| Recommended counseling | 69 | 14.2 | 66 | 14.8 | 3 | 7.5 | 0.21 |
| Prescribed or refilled a medication for an emotional problem | 212 | 43.5 | 205 | 45.9 | 7 | 17.5 | .001 |
| Adjusted a medication for an emotional problem | 106 | 22.4 | 103 | 23.6 | 3 | 8.3 | .035 |
Baseline frequencies and bivariate comparisons
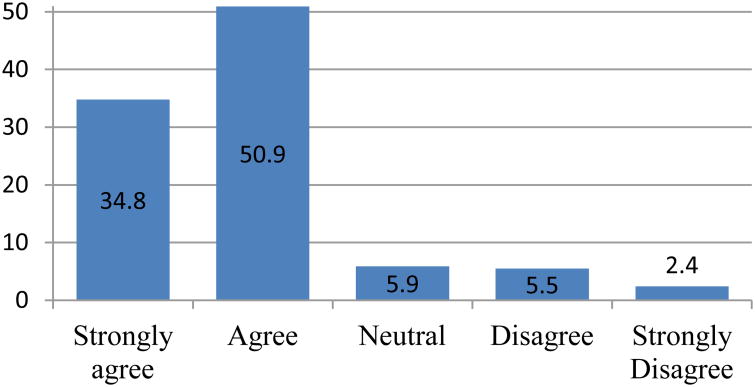
Figure 1 presents participants' responses to the depression label acceptability question. As presented in the figure, a minority of participants reported high stigma, stating that they would not accept a depression label from their doctors. Table 1 presents results of bivariate analyses that examined the relationships between stigma (dichotomized to high and low) and treatment preferences, treatment engagement and provider behavior variables. Considering demographic and health characteristics, low stigma participants were more depressed and nearly seven years younger on average than high stigma participants. As shown in Table 1, there were no additional significant health status or demographic differences between high and low stigma participants.
Figure 1.
Level of agreement with depression label.
Depression treatment preferences at baseline
Overall, relatively similar proportions of participants indicated openness to depression treatment from a PC physician, a psychiatrist, or another mental health specialist (i.e., psychologist, social worker). Just under half of participants noted preference for depression treatment from a spiritual counselor. Several significant differences in treatment preferences were observed for high versus low stigma. Consistent with hypotheses, high stigma was related to lower openness to depression care from specialty mental health providers. Specifically, relative to those with low stigma, significantly lower proportions of participants with high stigma reported openness to depression treatment from a psychiatrist or another mental health specialist. Stigma did not demonstrate significant bivariate relationships with preferences for depression treatment from a primary care provider or a spiritual provider/counselor.
Care receipt/engagement at seven month follow-up
Overall, nearly 90% of the sample reported at least one PC visit between baseline and follow-up. A substantial proportion of participants reported taking a medication for an emotional problem, and a little more than half reported a visit with a specialty mental health provider. For those who reported specialist care, the greatest proportion saw a psychiatrist; lower proportions reported care from a psychologist or a social worker. Approximately one-half of the participants with probable major depression received appropriate depression care at seven month follow-up. Finally, administrative data told a similar story at seven months, as 46.5% of participants had at least one individual visit in a specialty mental health clinic and 9.5% of participants had at least one group visit in specialty care.
Consistent with our hypotheses, stigma demonstrated significant bivariate associations with a number of care behavior/engagement variables at seven months. For example, when compared to those with low stigma, a significantly lower proportion of participants with high stigma at baseline reported taking a medication for an emotional problem, having any PC visit specifically addressing emotional health, and having any healthcare visit with a specialty mental health provider during the six months between baseline and follow-up. Similar differences were observed in the administrative data, with significantly lower proportions of high stigma participants attending any individual visit in a specialty mental health clinic at 7 months. Finally, 52.8% of low stigma participants received appropriate depression care at 7 months, while only 15.2% of high stigma participants received appropriate care.
Patient's reports of provider behavior at seven month follow-up
As noted above, most participants attended at least one PC visit between baseline and seven month follow-up. Among those who attended PC, most reported that their providers had asked about sadness or depression, while fewer noted that they were asked about suicide or depression improvement. A minority of participants noted that their providers recommended counseling with another provider. Considering medications, 43.5% of participants received a medication prescription or refill for an emotional problem, and 22.4% noted that their providers adjusted an existing medication.
Four significant differences, all in the hypothesized directions, were observed in the prospective bivariate analyses of the relations between stigma and patient-reported provider behavior. Specifically, compared to those with low stigma, lower proportions of participants who reported high stigma at baseline reported at seven months that their primary care providers had asked about suicide/self-harm or depression improvement. Similarly, as described by the patients, primary care providers for those with high stigma were significantly less likely than those treating low stigma participants to prescribe or refill a medication or to adjust a medication for an emotional problem.
Multivariable Logistic Regressions
Eleven controlled multivariable logistic regression models tested whether stigma predicted the baseline treatment preferences, seven month treatment engagement variables and seven month provider behavior variables for which significant relationships were observed in bivariate comparisons. To determine covariates for these models, we examined the relationship between stigma and demographic/illness characteristics, with stigma coded as a 5-point variable. Stigma was slightly higher for men relative to women [t (755) = 3.47, p < .001] and for participants with a high school education or less schooling relative to those who had completed some college education or more [t (755) = 2.36, p< .05]. Stigma was not significantly different for racial/ethnic minority participants and non-minority participants. All multivariable logistic regression models included participant age, gender, education, and baseline depression as covariates. Table 2 presents the results of these controlled logistic regressions.
Table 2.
Multivariable Logistic Regressions: Stigma as a concurrent predictor of care preferences and a prospective predictor of care behavior/engagement and provider behavior.
| Outcomes | Odds Ratio: Stigmaa,b | 95% CI | p-value |
|---|---|---|---|
| Provider preferences at baseline | |||
| Psychiatrist | 0.27 | 0.15-0.49 | <.001 |
| Other Mental Health Specialist | 0.31 | 0.18-0.54 | <.001 |
| Care behavior at 7 Months | |||
| Take medication for emotional problem | 0.19 | 0.09-0.40 | <.001 |
| Any outpatient PC for emotional health | 0.31 | 0.14-0.66 | .002 |
| Any mental health specialist visit past 6 months | 0.23 | 0.10-0.52 | <.001 |
| Appropriate care (mental health specialist and/or meds) | 0.24 | 0.10-0.55 | .001 |
| Care at 7 months (administrative data) | |||
| Any mental health specialist individual visits | 0.19 | 0.07-0.50 | .001 |
| Provider's behavior at 6 Months | |||
| Asked about self-harm | 0.51 | 0.24-1.08 | .080 |
| Asked about depression improvement | 0.39 | 0.18-0.86 | .019 |
| Prescribed or refilled a medication for an emotional problem | 0.28 | 0.12-0.66 | .003 |
| Adjusted a medication for an emotional problem | 0.34 | 0.10-1.15 | .083 |
Note.
Analyses controlled for gender, age, education, and baseline depressive severity.
Additional analyses examined stigma as a predictor of the outcomes reported above with patients' reports of general health as an additional covariate. Controlling for perceived general health did not substantially affect odds ratios, confidence intervals, or p–values for stigma in association with any outcome.
After controlling for demographic characteristics and baseline depressive severity, participants with high stigma at baseline were considerably less likely than low stigma participants to indicate a baseline preference for depression treatment from specialty mental health providers, including psychiatrists and psychologists/social workers. Baseline stigma was also a significant prospective predictor of multiple indicators of care behavior/engagement at seven months. For example, as we hypothesized, participants with high stigma were about 80% less likely than low stigma participants to take medication for an emotional problem. High stigma patients were also about 70% less likely to have a PC visit specifically addressing emotional problems and 75% less likely than those with low stigma to report seeing an specialty mental health provider for care. Controlled analyses also indicated that high stigma at baseline predicted a significantly lower likelihood of appropriate depression care at seven months. Similar patterns were evident in the administrative data, as high stigma participants were 81% less likely than those with low stigma to attend an individual visit in a specialty mental health clinic in the six months between baseline and follow-up. Finally, among those who saw a primary care provider between baseline and follow-up, high stigma was associated with a substantially lower likelihood of a provider asking about depression improvement and prescribing or refilling a medication for an emotional problem.
Discussion
Nearly 8% of the present sample of older VA PC patients with probable major depression reported high stigma, which we defined as depression label avoidance. Our results indicated that high stigma in these patients is cause for concern. As hypothesized, stigma demonstrated significant associations with patients' self-reported openness to depression care from specialty mental health care providers, including psychiatrists and psychologists/social workers, and with self-report and administrative database indicators of depression care behavior and quality. These relationships, many of which remained significant after controlling for depressive severity and demographic covariates, all told a similar story: patients with high stigma were significantly less open to depression care from specialists than patients with low stigma, and high stigma patients were less likely to engage treatment specifically for emotional problems in both PC and specialty mental health settings.
The present findings expand the existing literature by demonstrating that label avoidance, an understudied aspect of stigma, contributes to poor depression care. Our findings are consistent with existing work that observes a negative relation between stigma and one's intent to seek mental health care (22) as well as findings that link beliefs in public stigma with likelihood of care seeking (20,36). In addition, our findings join the few existing studies that document a prospective relationship between stigma and poor depression treatment adherence (26), and premature treatment dropout (27). Our findings specifically resemble those of Sirey and colleagues (26,27) in that high stigma conferred significant risk for low likelihood of appropriate depression care. Finally, our findings regarding the relation between stigma and openness to depression care from specific care providers (PC v. specialty mental health) are consistent with existing speculation (23) that stigma leads some persons with depression to present for care in PC rather than specialty mental health clinics. To our knowledge, the present results that indicate no difference between high and low stigma patients in openness to PC provider care but significant differences in openness to specialty mental health providers offers some of the only evidence from patients that stigma might contribute to differential treatment preferences.
Considered as a whole, findings from the present study have implications for depression care and ongoing efforts of clinicians and health care systems to improve it. First, given that stigma predicts patients' care behavior prospectively, it is imperative that health care providers assess patients' levels of stigma and self-referent beliefs upon initial diagnosis of depression. Our findings suggest, for example, that care providers should examine whether or not patients accept their depression diagnoses, and then examine the beliefs behind label avoidance when it is present. When providers understand patients' stigma and the reasons behind label avoidance more fully, they have an opportunity to modify patients' beliefs and address concerns or misconceptions/myths about depression through psychoeducation (44). As others have observed, for example, simple educational messages regarding depression treatment impacts treatment adherence (54).
The Health Beliefs Model (55) asserts that treatment engagement stems in part from patients' beliefs and attitudes, including beliefs regarding the ‘costs’ and ‘benefits’ of care participation. Combined with Link's modified labeling theory of stigma (10-12), the Health Beliefs Model highlights treatment implications of the present findings regarding differential openness to care from particular provider types. Under the model, stigma could be considered a ‘cost’ of care engagement. Link and colleagues' (12) maintain that stigma is activated for someone when diagnosis identifies him as a member of a devalued ‘outgroup’ (e.g., the depressed). Among other effects, outgroup membership makes stereotypical or societal beliefs about people with depression personally relevant. As Sirey and colleagues suggested (26,27), avoidance of care altogether is one way for persons to avoid membership in a devalued outgroup and to circumvent negative effects of stigma. Following that reasoning, a patient who accepts a diagnosis and engages in care would experience negative effects of stigma, while one who avoids care--and the depression label--would not.
Instead of an ‘either-or’ proposition of engagement in versus outright avoidance of care, stigma may be activated to different degrees when depression care is provided in different treatment settings or by different types of providers. More specifically, for many patients PC-based depression care may confer lower levels of stigma than care provided in specialty mental health settings because depression management by a familiar PC provider in the normal scope of PC practice may normalize the depressive experience. On the other hand, suggesting specialty mental health care for depression may communicate that depression presents a complex problem that is beyond the scope of a general care setting. Returning to the understanding of stigma and the Health Beliefs Model, PC-based depression care may be less ‘costly’ for some patients because it less likely to activate stigma than care provided by specialty mental health clinicians. This possibility is consistent with reports in the literature of clinicians' beliefs that PC-based integrated care for mental health concerns confers lower stigma for patients than referral to specialty clinics (56). In the present study, high and low stigma patients did not differ in openness to depression care from a PC provider, but high stigma patients were less open to treatment from specialty mental health care providers. Although future study is needed to determine whether stigma is differentially activated by care in PC versus specialty mental health settings, one potential way to improve depression care for high stigma patients may be to redouble efforts, such as those aimed at Primary Care-Mental Health Integration (PC-MHI), which are underway within the VA and other systems (57). PC-MHI efforts like collaborative and co-located care and other approaches to integrated behavioral health, house depression care resources and related mental health expertise in PC settings. In addition to other aims, collaborative care models were designed in part to address stigma related to mental health care seeking (58). The present study's finding that patients with high stigma were amenable to depression care from primary care providers suggests that continued efforts in service of PC-MHI and integrated behavioral health might support improved care for people with high stigma. Consistent with Health Beliefs Model principles, high stigma patients may be more willing to engage PC-based depression care than specialty setting care because the former confers less cost to self-esteem.
The present study's prospective analyses regarding care engagement and care appropriateness provided evidence from multiple data sources that stigma impedes depression care. Although baseline stigma was unrelated to receipt of general medical care from a PC physician during the following six months, high stigma patients were substantially less likely than those with low stigma to report a PC visit that addressed emotional health specifically. In other words, high and low stigma patients with major depression were equally likely to interact with the health care system, but the interactions for high stigma patients with major depressive symptomatology were less likely to address their mental health concerns explicitly. High stigma patients were significantly less likely than those with low stigma to report medication use for an emotional problem and to report care for depression from a specialty mental health care provider at the seven-month follow-up. Patients with high stigma also differed from low stigma patients in terms of what they reported had happened in their most recent interactions with their PC providers. Consistent with the findings just described, patients with high stigma were less likely to report that their providers had asked them about suicidal thinking, for example. Additional evidence regarding the negative impact of stigma on care was found in the VA administrative data, where high stigma at baseline predicted a lower likelihood of any specialty mental health provider care during the following six months. Of greater potential concern, the patients who reported high stigma at baseline were less likely than low stigma patients to receive appropriate depression care during the following 6 months, using reports of antidepressant use and/or engagement with specialists.
The present findings suggesting that stigma impedes care join the growing body of work regarding stigma among military personnel and/or Veterans. Stigma related to mental health concerns clearly exists in these populations even though, as presented earlier, the evidence is mixed regarding stigma's function as a treatment barrier (28-32,35,38,40,41). The present study's definition of stigma as depression label avoidance contrasts with the various definitions of stigma employed by other researchers in VA and military samples. This difference is one possible reason for the findings we report here. As previously noted, our operational definition identified 8% of the present sample as having high stigma. The fact that we observed a negative effect of stigma on treatment among Veterans while others have not may be because our high-stigma definition identified a group with more severe concerns about stigma than those in prior studies. Regardless of the source of the differences in results, stigma as label avoidance is an understudied and important area of focus for clinicians who identify and treat patients with depression and for future research regarding barriers to mental health care. Indeed, although label avoidance is identified as a key component of stigma (9), minimal research documents its predictive relationship with care. Future research should specifically examine whether label avoidance is modifiable and whether modifications impact patients' care engagement and adherence. Along these lines, Dickstein and colleagues reported that a handful of studies indicate promise in acceptance-based and cognitive reappraisal interventions aimed at mental health self-stigma reduction among military personnel and Veterans (59). While we agree with Dickstein and colleagues' call for additional research of self-stigma reduction techniques, we also believe that future clinical and research efforts should target label avoidance. Finally, because we found that high stigma is associated with lower likelihood of specific care for emotional concerns in PC, PC providers who identify depression ought to talk explicitly with patients about stigma as a treatment barrier and to discuss potential ways to manage it.
Though our results are informative, limitations of the present study should be kept in mind. First, as we have noted above, studies of label avoidance are underrepresented in the broader stigma literature. Unlike other stigma types, questionnaires of label avoidance with known psychometric properties do not presently exist. We used a single item regarding depression diagnosis acceptance as our measure of label avoidance, and though this is consistent with theoretical models of stigma and prejudice (46,47), our single item may not fully capture the label avoidance construct. In addition, although our measure appears at face value to be a reasonable reflection of label avoidance, we cannot say with certainty that not accepting a depression diagnosis is the same as avoiding a depression label. As with any research that examines understudied issues, this potential limitation confers an opportunity. Future research efforts can and should focus on development of measures of label avoidance and should examine these measures' psychometric characteristics. These measures could then be used to qualify and quantify the relationships between the label avoidance type of stigma and those stigma types about which more is known.
Second, the present sample comprised VA PC attendees, most of whom were older, White men, with multiple physical health concerns. Additionally, the visit-based sampling procedure identified participants for study inclusion with the PHQ-9, a measure that demonstrates good sensitivity and specificity for major depressive episode but does not provide a definitive depression diagnosis (51,60). Therefore, though all patients were experiencing significant major depressive symptomatology, some may not have met full diagnostic criteria for a major depressive episode. In addition, because the recruitment strategy most likely resulted in a sample characterized by particularly poor health (61), generalization to non-VA samples and samples in better health ought to be done with great care. Notwithstanding these limitations, the present study identified depression using the same tool (i.e., PHQ-9) that characterizes system-wide depression screening within VA (62) and other health care systems (e.g., 63). Thus, the patients who composed the present sample are likely to resemble the clinical characteristics and care needs of similarly-aged Veterans with depression in VA care and other patients who present with similar circumstances.
A final limitation stems from the survey methodology that assessed participants' attitudes about and experiences with care. Specifically, patients' self-report of care may not have reflected actual care with absolute precision, and patients' recall of their providers' behavior may not have resembled exactly what happened during their healthcare encounter. Though we had some confirmation of depression care behavior from a subsample of participants via VA administrative data, the questions regarding care in the self-report survey and the indicators of care from the administrative databases were not identical. Nonetheless, the consistent pattern in results across the self-report and administrative data sources increases confidence that our findings accurately reflected patients' engagement in care. The computer-assisted telephone interviewing method of data collection also included several techniques to increase the validity of the participants' self-reports. In the assessment of medication use, for example, participants were encouraged to read prescription information from the labels on their medication bottles, and more than 80% of patients did so.
In conclusion, our data presented provide evidence that a high level of stigma, defined as depression label avoidance, may contribute to patients' greater openness to care from PC providers over mental health specialists. Further, our results confirm that high stigma predicts a lower likelihood of care specifically for emotional concerns and appropriate depression care over time. Ultimately, high stigma functions as a depression care barrier among VA PC attendees and this finding confirms the importance of system redesign efforts that integrate care for mental health conditions like depression in PC settings. Finally, the present findings suggest that understanding reasons behind depression label avoidance may allow providers to modify patients' treatment relevant beliefs and improve depression treatment engagement and adherence. As others have reported, depression outcomes may improve with targeted psychoeducation (64). In addition, early treatment discussions about stigma may help clarify for patients that depression is common, that treatment works (65), and that patients are not to blame for causing it (66).
Acknowledgments
This project was funded by the Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) Service and the VA Quality Enhancement Research Initiative (QUERI) (Project nos. MHI 99-375, MNT 01-027, MHQ 10-06). The authors acknowledge the contributions of the study participants who made this work possible. A portion of this work was presented at the 35th Annual Meeting and Scientific Sessions of the Society of Behavioral Medicine, Philadelphia, PA.
Footnotes
NOTE: The views expressed here are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs, the United States Government, and the authors' other institutions. The authors report no competing interests.
Statement of Conflict of Interest: All authors of this manuscript declare that they have no conflicts of interest.
Statement of Adherence to Ethical Standards: The research described in this manuscript was conducted in accord with ethical principles for the treatment of human subjects. All study procedures were approved by the Institutional Review Boards of the participating study sites and the primary study administrative site.
References
- 1.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Meth Psych Res. 2012;21:169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatr. 2005;62:409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- 4.Dimidjian S, Hollon SD, Dobson KS, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- 5.Wang PS, Angermeyer M, Borges G, et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007;6:177–185. [PMC free article] [PubMed] [Google Scholar]
- 6.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States. Arch Gen Psychiatr. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Depression: A global health concern. [Accessibility verified July 31, 2014]; Available at http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf?ua=1.
- 8.U.S. Department of Health and Human Services. Mental health: A report of the Surgeon General. Washington, DC: Author; 1999. [Google Scholar]
- 9.Jones N, Corrigan PW. Understanding Stigma. In: Corrigan PW, editor. The Stigma of Disease and Disability: Understanding Causes and Overcoming Injustices. Washington, DC: American Psychological Association; 2014. pp. 9–34. [Google Scholar]
- 10.Corrigan PW. How stigma interferes with mental health care. Am Psychol. 2004;59:614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- 11.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 12.Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. Am Sociol Rev. 1989;54:400–423. [Google Scholar]
- 13.Luoma JB, Nobles RH, Drake CE, et al. Self-stigma in substance abuse: development of a new measure. J Psychopathol Behav. 2013;35:223–234. doi: 10.1007/s10862-012-9323-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brohan E, Slade M, Clement S, Thornicroft G. Experiences of mental illness stigma, prejudice and discrimination: a review of measures. BMC Health Serv Res. 2010;10:80. doi: 10.1186/1472-6963-10-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Link BG. Understanding labeling effects in the area of mental disorders: an assessment of the effect of expectations of rejection. Am J Community Psychol. 1987;11:261–273. [Google Scholar]
- 16.Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25:875–884. [Google Scholar]
- 17.Priest RG, Vize C, Roberts A, Roberts M, Tylee A. Lay people's attitudes to treatment of depression: Results of opinion poll for Defeat Depression Campaign just before its launch. Brit Med J. 1996;313:858–859. doi: 10.1136/bmj.313.7061.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simon GE, Fleck M, Lucas R, Bushnell DM. Prevalence and predictors of depression treatment in an international primary care study. Am J Psychiat. 2004;161:1626–1634. doi: 10.1176/appi.ajp.161.9.1626. [DOI] [PubMed] [Google Scholar]
- 19.Roeleffs C, Sherbourne C, Unutzer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. Gen Hosp Psychiat. 2003;25:311–315. doi: 10.1016/s0163-8343(03)00066-5. [DOI] [PubMed] [Google Scholar]
- 20.Cooper AE, Corrigan PW, Watson AC. Mental illness stigma and care-seeking. J Nerv Ment Dis. 2003;191:339–341. doi: 10.1097/01.NMD.0000066157.47101.22. [DOI] [PubMed] [Google Scholar]
- 21.Rost K, Zhang M, Fortney J, Smith J, Coyne J, Smith GR. Persistently poor outcomes of undetected major depression in primary care. Gen Hosp Psychiat. 1998;20:12–20. doi: 10.1016/s0163-8343(97)00095-9. [DOI] [PubMed] [Google Scholar]
- 22.Schomerus G, Matschinger H, Angermeyer MC. The stigma of psychiatric treatment and help-seeking intentions for depression. Eur Arch Psy Clin N. 2009;259:298–306. doi: 10.1007/s00406-009-0870-y. [DOI] [PubMed] [Google Scholar]
- 23.Ben-Porath DD. Stigmatization of individuals who receive psychotherapy: An interaction between help-seeking behavior and the presence of depression. J Soc Clin Psychol. 2002;21:400–413. [Google Scholar]
- 24.Golberstein E, Eisenberg D, Gollust SE. Perceived stigma and mental health care seeking. Psychiatr Serv. 2008;59:392–399. doi: 10.1176/ps.2008.59.4.392. [DOI] [PubMed] [Google Scholar]
- 25.Eisenberg D, Downs MF, Golberstein E, Zivin K. Stigma and help seeking for mental health among college students. Med Care Res Rev. 2009;66:522–541. doi: 10.1177/1077558709335173. [DOI] [PubMed] [Google Scholar]
- 26.Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001a;52:1615–1620. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- 27.Sirey JA, Bruce ML, Alexopoulos GS, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiat. 2001b;158:479–481. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]
- 28.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. NEJM. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 29.Zinzow HH, Britt TW, McFadden AC, Burnette CM, Gillispie S. Connecting active duty and returning veterans to mental health treatment: Interventions and treatment adaptations that may reduce barriers to care. Clin Psychol Rev. 2012;32:741–753. doi: 10.1016/j.cpr.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Britt TW, Greene-Shortridge TM, Brink S, et al. Perceived stigma and barriers to care for psychological treatment: Implications for reactions to stressors in different contexts. J Soc Clin Psychol. 2008;27:317–335. [Google Scholar]
- 31.Kehle SM, Polusny MA, Murdoch M, et al. Early mental health treatment-seeking among U.S. National Guard soldiers deployed to Iraq. J Trauma Stress. 2010;23:33–40. doi: 10.1002/jts.20480. [DOI] [PubMed] [Google Scholar]
- 32.Vogt D. Mental health-related beliefs as a barrier to service use for military personnel and Veterans: A review. Psychiatr Serv. 2011;62:135–142. doi: 10.1176/ps.62.2.pss6202_0135. [DOI] [PubMed] [Google Scholar]
- 33.Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Perceived stigma and barriers to mental health care utilization among OEF-OIF Veterans. Psychiatr Serv. 2009;60:1118–1122. doi: 10.1176/ps.2009.60.8.1118. [DOI] [PubMed] [Google Scholar]
- 34.Britt TW. The stigma of psychological problems in a work environment: Evidence from the screening of service members returning from Bosnia. J Appl Soc Psychol. 2000;30:1599–1618. [Google Scholar]
- 35.Ouimette P, Vogt D, Wade M, et al. Perceived barriers to care among Veterans Health Administration patients with posttraumatic stress disorder. Psychol Serv. 2011;8:212–223. [Google Scholar]
- 36.Blais RK, Renshaw KD. Stigma and demographic correlates of help-seeking intentions in returning service members. J Trauma Stress. 2013;26:77–85. doi: 10.1002/jts.21772. [DOI] [PubMed] [Google Scholar]
- 37.Brown MC, Creel AH, Engel CC, Herrell RK, Hoge CW. Factors associated with interest in receiving help for mental health problems in combat veterans returning from deployment to Iraq. J Nerv Ment Dis. 2011;199:797–801. doi: 10.1097/NMD.0b013e31822fc9bf. [DOI] [PubMed] [Google Scholar]
- 38.Mittal D, Drummond KL, Blevins D, Curran G, Corrigan P, Sullivan G. Stigma associated with PTSD: Perceptions of treatment seeking combat Veterans. Psychiatr Rehabil J. 2013;36:86–92. doi: 10.1037/h0094976. [DOI] [PubMed] [Google Scholar]
- 39.Rosen CS, Greenbaum MA, Fitt JE, Laffaye C, Norris VA, Kimerling R. Stigma, help-seeking attitudes, and use of psychotherapy in Veterans with diagnoses of posttraumatic stress disorder. J Nerv Ment Dis. 2011;199:879–885. doi: 10.1097/NMD.0b013e3182349ea5. [DOI] [PubMed] [Google Scholar]
- 40.Arbisi PA, Rusch L, Polusny MA, Thuras P, Erbes CR. Does cynicism play a role in failure to obtain needed care? Mental health service utilization among returning U.S. National Guard soldiers. Psychol Assessment. 2013;25:991–996. doi: 10.1037/a0032225. [DOI] [PubMed] [Google Scholar]
- 41.Harpaz-Rotem I, Rosenheck RA, Pietrzak RH, Southwick SM. Determinants of prospective engagement in mental health treatment among symptomatic Iraq/Afghanistan Veterans. J Nerv Ment Dis. 2014;202:97–104. doi: 10.1097/NMD.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 42.Menke R, Flynn H. Relationships between stigma, depression, and treatment in White and African American primary care patients. J Nerv Ment Dis. 2009;197:407–411. doi: 10.1097/NMD.0b013e3181a6162e. [DOI] [PubMed] [Google Scholar]
- 43.Howe L, Tickle A, Brown I. ‘Schizophrenia is a dirty word’: service users' experiences of receiving a diagnosis of schizophrenia. Psychiatr Bull. 2014;38:154–158. doi: 10.1192/pb.bp.113.045179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Corrigan PW, Bink AB. How does stigma impede adherence and self-determination? In: Corrigan PW, editor. Person-Centered Care for Mental Illness: The Evolution of Adherence and Self-Determination. Washington, DC: American Psychological Association; 2015. pp. 53–80. [Google Scholar]
- 45.Corrigan PW, Wassel A. Understanding and influencing the stigma of mental illness. Journal of Psychosocial Nursing. 2008;46:42–48. doi: 10.3928/02793695-20080101-04. [DOI] [PubMed] [Google Scholar]
- 46.Hayes SC, Niccolls R, Masuda A, Rye AK. Prejudice, terrorism, and behavior therapy. Cogn Behav Pract. 2002;9:296–301. [Google Scholar]
- 47.Masuda A, Hill ML, Morgan J, Cohen LL. A psychological flexibility-based intervention for modulating the impact of stigma and prejudice: a descriptive review of empirical evidence. Psychology, Society & Education. 2012;4:211–223. [Google Scholar]
- 48.Chaney EF, Rubenstein LV, Liu CF, et al. Implementing collaborative care for depression treatment in primary care: a cluster randomized evaluation of a quality improvement practice redesign. Implement Sci. 2011;6:121. doi: 10.1186/1748-5908-6-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yano EM, Chaney EF, Campbell DG, et al. Yield of depression screening in routine primary care practice. J Gen Intern Med. 2012;27:331–338. doi: 10.1007/s11606-011-1904-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Author. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 53.Kazis LE, Ren XS, Lee A, et al. Health status in VA patients: results from the Veterans Health Study. Am J Med Qual. 1999;14:28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 54.Brown C, Battista DR, Sereika SS, Bruehlman R, Dunbar-Jacob J, Thase ME. How can you improve antidepressant adherence? J Fam Practice. 2007;56:356–363. [PubMed] [Google Scholar]
- 55.Rosenstock IM. The health belief model: Explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 1990. pp. 39–62. [Google Scholar]
- 56.Gallo JJ, Zubritsky C, Maxwell J, et al. Primary care clinicians evaluate integrated and referral models of behavioral health care for older adults: Results from a multisite effectiveness trial (PRISM-D) Ann Fam Med. 2004;2:305–309. doi: 10.1370/afm.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pomerantz AS, Sayers SL. Primary care-mental health integration in healthcare in the Department of Veterans Affairs. Fam Syst Health. 2010;28:78–82. doi: 10.1037/a0020341. [DOI] [PubMed] [Google Scholar]
- 58.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 59.Dickstein BD, Vogt DS, Handa S, Litz BT. Targetting self-stigma in returning military personnel and Veterans: A review of intervention strategies. Mil Psychol. 2010;22:224–236. [Google Scholar]
- 60.Wittkampf K, van Ravesteijn H, Baas K, et al. The accuracy of Patient Health Questionnaire-9 in detecting depression and measuring depression severity in high-risk groups in primary care. Gen Hosp Psychiat. 2009;31:451–459. doi: 10.1016/j.genhosppsych.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 61.Lee ML, Yano EM, Wang M, Simon B, Rubenstein LV. What patient population does visit-based sampling in primary care settings represent? Med Care. 2002;40:761–770. doi: 10.1097/00005650-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 62.Kirchner JE, Curran GM, Aikens J. Datapoints: detecting depression in VA primary care clinics. Psychiatr Serv. 2004;55:350. doi: 10.1176/appi.ps.55.4.350. [DOI] [PubMed] [Google Scholar]
- 63.Simon, GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64:1195–1202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.deSouza Tursi MF, von Werne Baes C, deBarros C, Ribiero F, deCarvalho Tofoli SM, Jurena MF. Effectiveness of psychoeducation for depression: A systematic review. Aust NZ J Psychiat. 2013;47:1019–1031. doi: 10.1177/0004867413491154. [DOI] [PubMed] [Google Scholar]
- 65.Kriston L, von Wolff A, Holzel L. Effectiveness of psychotherapeutic, pharmacological, and combined treatments for chronic depression: a systematic review. BMC Psychiatry. 2010;10:95. doi: 10.1186/1471-244X-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hinshaw SP, Cicchetti D, Toth SL. Mark of Shame: Stigma of Mental Illness and an Agenda for Change. Cary, NC: Oxford University Press; 2006. [Google Scholar]