Abstract
Purpose
To assess the feasibility, acceptability, and efficacy of a text message–based smoking cessation intervention in China.
Design
Randomized control trial with a 6-month follow-up assessment of smoking status.
Setting
Zhejiang, Heilongjiang, and Shaanxi provinces in China.
Subjects
8,000 adult smokers in China who use Nokia Life Tools and participated in Phase II (smoking education via text message) of the study.
Intervention
High Frequency Text Contact (HFTC) group received one to three messages daily containing smoking cessation advice, encouragement, and health education information. Low Frequency Text Contact (LFTC) group received one weekly message with smoking health effects information.
Measures
Our primary outcome was smoking status 0, 1, 3, and 6 months post-intervention. Secondary outcomes include participant perceptions of the HFTC intervention, and factors associated with smoking cessation among HFTC participants.
Analysis
Descriptive and chi-square analyses were conducted to assess smoking status and acceptability. Factors associated with quitting were assessed using multiple logistic regression analyses.
Results
Quit rates were high in both HFTC and LFTC groups (HFTC: 0 month 27.9%, 1 month 30.5%, 3 months 26.7%, 6 months 27.7%; LFTC: 0 month 26.7%, 1 month 30.4%, 3 months 28.1%, 6 months 27.7), with no significant difference between the two groups in an intent-to-treat analysis. Attitudes towards the HFTC intervention were largely positive.
Conclusion
Our findings suggest that a text message–based smoking cessation intervention can be successfully delivered in China and is acceptable to Chinese smokers, but further research is needed to assess the potential impact of this type of intervention.
Keywords: Smoking Cessation, Text Message Intervention Research, Health Education, Tobacco Control, mHealth, China, Behavior Change Intervention
Purpose
Cigarette smoking is a persistent health threat worldwide. With one-third of the world’s adult smokers, China’s population of 301 million adult smokers is a significant global public health concern, which must be urgently and comprehensively addressed.1, 2 Over half (52.9%), of the male adult population and 2.4% of adult females reported that they were smokers in 2010.3 Smoking is a major risk factor for many health problems such as cancers, cardiovascular disease, and respiratory disease–related deaths.4, 5 An estimated 673,000 adult deaths were attributed to tobacco smoking in 2005,4 and more recent estimates are as high as 1.2 million deaths.6 In 2008, in China, smoking-attributable health care costs amounted to at least US$6.2 billion.7 Quitting smoking can effectively reduce smokers’ risk of morbidity and mortality.5 Because of smoking’s impact on health and the economy, widespread cessation efforts are extremely important.
Reported percentages of people who intend to quit smoking are low in China compared with many other countries.8 In 2010, only 16.1% of adult smokers reported they intended to quit smoking within the next 12 months,1 and an estimated 36.4% reported they had attempted to quit in the previous 12 months.1 Lack of intent to quit smoking can be due to many factors including a low overall awareness of the risks of smoking on health. Only 5.2% of current smokers who responded to a 2006 International Tobacco Control (ITC) China Survey were aware of all the following health effects of smoking—stained teeth, lung cancer in smokers and non-smokers, emphysema, premature aging, cardiovascular diseases, stroke, and impotence.9 Participants in this same study who were more knowledgeable about the adverse health effects were more likely to intend to quit smoking, which illustrates the relevance and importance of increasing knowledge to motivate smoking cessation, as seen in other countries.10 Because efforts to increase public knowledge about the dangers of smoking have been limited and few smoking cessation resources are available in China, more programs to support cessation are urgently needed.8 In China, recent smoking policy changes, such as smoke-free public venues, may have increased motivation for smokers to quit, but access to smoking cessation programs and use of existing programs, such as quit lines and nicotine replacement therapy, are limited.8, 11
The feasibility and utility of using mobile phone text messaging to send health-related messages are now under study.12 Mobile phone services are widely accessible around the world. About 93% of the world’s population and 99% of China’s citizens have access to cellular networks.13 Estimates from 2011 indicate that worldwide there are 85.5 mobile phone subscriptions per 100 people, and in China there are 73.2 subscriptions per 100 people.13 Because of the widespread use of mobile phones, text messaging services could reach large numbers of people at a lower cost for both the organization sending the message and the people receiving it in comparison with the cost of other smoking cessation methods such as quitlines, behavioral counseling, and nicotine replacement therapy. A mobile phone–based intervention for smoking cessation could capitalize on the widespread use of mobile phones and text messaging in China to deliver information, motivation, and support to quit smoking in a low-cost manner, while reaching a large group of people at any time and in any location.
Text messaging has been incorporated into smoking cessation with mixed results, depending on the nature of the intervention and the size of the sample.14 A meta-analysis of 5 mobile phone interventions involving over 9,000 participants found that the text message intervention groups were 1.71 times more likely to be continuously abstinent at 6 months (95% confidence interval [CI] = 1.47–1.99) compared to the control groups.14 To date, the vast majority of text message intervention studies have been conducted in high-income countries. Conducting such studies in low- and middle-income, resource-limited countries is particularly important given the limited research in these countries and the great need for economical treatment approaches. To our knowledge, only one text message smoking cessation study has been conducted in China; this study suggested that a text message intervention could reduce the number of cigarettes smoked by adolescents ages 16–19.15
The purpose of this study is to test the feasibility of delivering a text message–based smoking cessation program to a large number of Chinese smokers and assess the program’s impact on smoking status between 0 and 6 months after the intervention. To our knowledge, this is the first large randomized controlled study using text messages for smoking cessation in China. In addition to evaluating feasibility, this study addressed the program’s acceptability among a sub-sample of participants.
Methods
Design
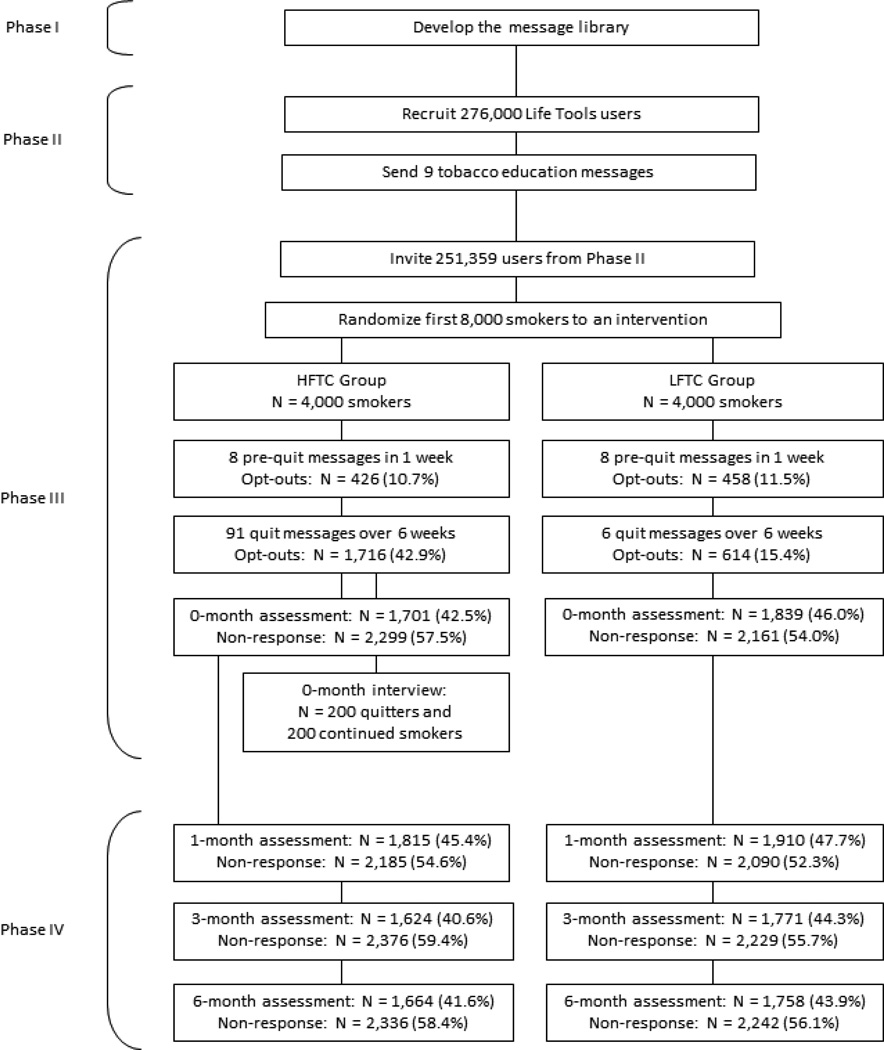
The study design was a two-arm randomized control trial of a 6-week smoking cessation intervention (described below) with a follow-up assessment of smoking status at the end of the intervention, and 1, 3, and 6 months after the smoking cessation intervention (Figure). The study was designed and implemented collaboratively by the National Cancer Institute (NCI), U.S. Centers for Disease Control and Prevention (U.S. CDC), China Centers for Disease Control (China CDC), China Center for Health Education, and Nokia (a multinational telecommunications corporation). Institutional Review Board approval was obtained for this study from the China CDC prior to the study.
Figure.
Smoking Cessation Text Message Study Framework
Text Message Library Development
Phase I of this project involved smoking cessation message testing and adaptation. The text messages used in the study came from a text message library created for the U.S. population. This text library was developed by smoking cessation experts at NCI, and was based on well-established cognitive–behavioral cessation approaches. The library was translated into Chinese, reviewed by Chinese health communication and tobacco cessation experts, and adapted to the Chinese context. Eight focus group interviews were conducted with smokers in rural and urban areas of three Chinese provinces to assess the acceptability of the cessation text message library. Focus group interviewees, most of whom were male (152 males, 13 females), were evenly distributed between rural and urban areas (82 and 83 interviewees, respectively) and among the three provinces (49 interviewees in Zhejiang, 60 in Heilongjiang, and 56 in Shaanxi). The focus groups assessed the quality of the messages, including whether the interviewees thought the messages were motivating, believable, and appropriately translated for the Chinese context. The messages were then modified based on focus group feedback to assure that they were culturally appropriate for a Chinese audience.
Sample and Recruitment
All individuals in this study subscribed to Nokia Life Tools, a service providing more than 100 million users in five countries (China, India, Indonesia, Nigeria, and Kenya) with text message–based information on a variety of topics of their choosing.16 Nokia Life Tools software comes pre-installed on most Nokia phones and provides users with free basic subscriptions and content, with additional subscriptions available to purchase.
For Phase II, in April 2013, Life Tools users in both urban and rural areas of China’s Zhejiang, Heilongjiang, and Shaanxi provinces received a text message inviting them to join a free program to receive 1 week of text messages (nine messages total) about the health effects of smoking. The study accepted the first 276,000 individuals who opted into the program. Subject accrual for Phase II was completed in approximately 1 day, and 251,359 (91.1%) completed Phase II.
A text message was then sent to all 251,359 participants who completed Phase II to invite those who self-identified as adult smokers interested in quitting to join the next phase of the study and receive free smoking cessation messages. This recruitment text was sent the day after the last Phase II educational text message was sent; the first Phase III cessation text messages were sent 1 week after the Phase III recruitment text. There were no other exclusions for participation in the last two phases of the study. The first 8,000 participants who accepted this invitation were enrolled into Phases III and IV of the study. Subject accrual was completed in less than 1 hour. The Institutional Review Board waived the requirement for informed consent because it was determined that the intervention would be of minimal risk to participants. In addition, the recruitment and treatment delivered via text message made gathering informed consent or demographic information infeasible. Although demographic data were not collected from participants, Nokia records provided province and city residence of Phase III and IV participants: 2,768 participants in Zhejiang, 2,053 participants in Heilongjiang, and 3,179 participants in Shaanxi. Nokia consumer profiles also suggested that the vast majority of our sample would be above the age of 19. We selected a sample size that would give us sufficient power to detect modest differences between the groups while accounting for (1) the high rates of lost to follow-up that occur in mobile health research projects and (2) the wide range of quit rates seen in previous cessation intervention studies in China.17 Even assuming a quit rate as high as 37% in the control group at any time point, there would be a power of roughly 80% to detect a modest difference between the two groups with a significance level of alpha = 0.05. In addition, the trial’s large sample size will also inform potential efforts to further scale up the intervention if it is successful.
Intervention
Participants who opted into the Phase III smoking cessation trial were randomly assigned to the intervention or comparison group (n = 4,000 in each group). Participants were not aware of the separate intervention arms, and therefore did not know what group they were assigned to. On April 28, 2013, Phase III text messages began with a notification that the quit date would be 1 week later, plus 1 week of pre-quit-day messages sent to all participants (8 messages total). These pre-quit-day messages were designed to increase motivation to make a sustained attempt to quit smoking.
The High Frequency Text Contact (HFTC) treatment group received an additional 91 messages over the 6 weeks after May 5, 2013: 3 messages per day for weeks 1–2, 2 per day for weeks 3–5, and 1 per day for week 6. At the end of each text message, participants in both groups were offered the opportunity to cancel the service via text. The text messages sent to the HFTC group provided encouragement, practical advice to help maintain cessation, and information on health effects of smoking. The Low Frequency Text Contact (LFTC) comparison group received 1 text message a week, for a total of 6 text messages over the 6-week intervention period. Because only 6 text messages were being sent, LFTC participants did not receive the full range of text messages available to the HFTC group, and instead were sent a subset of text messages on smoking’s health effects. See Table 1 for examples of text messages sent to both the HFTC and LFTC groups.
Table 1.
Examples of text messages sent to HFTC and LFTC treatment groups (English translation)*
| HFTC Treatment Group | LFTC Treatment Group |
|---|---|
|
|
Please note that these messages were originally sent in Chinese. This table is intended to convey the sense of the messages rather than represent a literal translation, which would result in phrasing that is awkward in English.
The day after the 6-week intervention ended (June 16, 2013) all participants (including participants who opted out of the service during the intervention) received a text message asking them to report their smoking status via text message (see “Measures – Cessation Outcomes” for additional information).
Follow-Up Interview with Sub-Sample
During the week following the intervention (June 16–22, 2014), follow-up phone interviews were conducted with a sub-sample of participants in the HFTC group to assess demographic factors associated with smoking cessation and intervention satisfaction among those who received the HFTC intervention. Interviewers called HFTC participants who reported their smoking status at the end of the intervention, including participants who opted out during the intervention. If a participant did not answer, hung up, or otherwise did not complete the interview, the interviewer continued to call other participants until a total of 400 interviews were completed with participants who reported continuing to smoke (n = 200) or quitting (n = 200) at the end of the intervention. Seven of these interviewees were later excluded from analyses because they indicated they were not smokers at the beginning of the study, but rather were gathering information for another smoker. Interviewees who reported a different smoking status on the phone than they reported via text were categorized based on their verbal response. There was an 86.6% agreement between the self-reports via text and subsequent verbal reports. This resulted in a final sub-sample of 393 interviewees (180 quitters and 213 current smokers).
Measures
Cessation Outcomes – Full Sample
The main outcome of interest was point prevalence of smoking cessation immediately following the intervention, as well as point prevalence during Phase IV of the study at 1, 3, and 6 months follow-up. Smoking status was based on past-7-day abstinence self-reported via text message. Participants were asked if they had “smoked cigarettes at all, even one puff, in the last 7 days” and were prompted to reply either “0” if they had not smoked, or “1” if they had smoked. Participants were also told they would receive a 10 RMB reimbursement (approximately $1.60 USD) to their mobile phone balance if they responded. This question was asked of all participants at all time points regardless of whether they opted out during the intervention or did not respond at any earlier follow-up point.
The name of each participant’s province was provided by Nokia. Nokia also reviewed system records to confirm that the delivered text messages during the intervention and the follow-up were received on participants’ mobile phones.
Outcomes from Phone Interviewees – Sub-sample
To assess the quality and utility of the numerous text messages in the HFTC intervention, interviewees were asked about their use and perceptions of the HFTC intervention. They were asked to confirm their current smoking status, then asked whether they received the text messages, how many they read, whether they were satisfied with the quantity of messages they received, whether the messages provided useful information, whether the messages encouraged them to quit, and if they would share these messages with other smokers. Demographic data on age, education, urban/rural residential status, marital status, and health status were also gathered during the phone interview.
Analysis
Descriptive statistics and chi-square analyses were completed to compare cessation rates between the intervention and control groups in the full sample at each follow-up point. The main analyses were based on the intent-to-treat principle, whereby individuals who opted out after randomization and those who did not respond to the smoking status prompt were considered to have continued smoking. This type of analysis is considered the most conservative and is the standard for smoking cessation studies.14 We also conducted less conservative analyses, excluding those who did not respond at the point of follow-up. Our ability to analyze continuous abstinence was hampered by the large amount of missing smoking status data for participants responding across all follow-up time points.
For the interviewee sub-sample, chi-square analyses were completed to assess relationships between smoking status, demographic variables (province, marital status, highest level of education attained, and age), and self-described health status. Simple logistic and multivariate logistic regression analyses were conducted to further describe the relationships between each variable and smoking status, and unadjusted and adjusted odds ratios are provided. The final multiple logistic regression model contained each of the demographic variables as well as health status. Descriptive data indicating the interviewees’ perceptions about the utility of the HFTC intervention are also provided.
All analyses were conducted using SPSS version 22.
Results
Data were collected and analyzed for 8,000 adults—4,000 in the HFTC intervention and 4,000 in the LFTC comparison group. In the intervention group, 426 respondents (10.7%) declined to receive messages before the quit date, and 458 respondents in the control group (11.5%) declined to receive these messages (see the Figure to see a flowchart for opt-out rates during the intervention and for follow-up smoking status response rates). By the end of the 6-week intervention, 1,716 HFTC participants (42.9%) and 614 LFTC participants (15.4%) had opted out of receiving additional messages (p<0.001).
Cessation Outcomes – Full Sample
The 7-day point prevalence cessation rates at the end of the intervention (0 month) and at follow-up (1, 3, and 6 months) are displayed in Table 2. Using the conservative intent-to-treat approach which considered all non-responders to be smokers, we observed high reported quit rates (between 26.7 and 30.5%) at all of the follow-up time points for both the HFTC and LFTC groups. The non-smoking point prevalence did not differ by treatment group for this approach. Excluding those who did not report their smoking status, we observe significantly greater 7-day point prevalence abstinence in the HFTC group compared to the LFTC group immediately after the intervention (66% vs. 58% for the HFTC and LFTC, respectively; p < 0.001); 1 month after the intervention (67% vs. 64% for the HFTC and LFTC, respectively; p = 0.027); and at 6 months (67% vs. 63% for the HFTC and LFTC, respectively; p = 0.032). Statistically significant differences were noted at each time point, but the magnitude of these differences is not clinically meaningful. These differences should also be interpreted cautiously given the high non-response rates in both the HFTC and LFTC groups during the study (0m = 55.8% of the full sample, 1m = 53.4%, 3m = 57.6%, 6m = 57.2%). The non-response rates did not differ significantly by treatment group. Additionally, response varied by participant: Those who did not respond at one time point may have responded at other time points (data not shown).
Table 2.
7-day point prevalence abstinence at each follow-up point
| HFTC (n = 4,000) n (%) |
LFTC (n = 4,000) n (%) |
Significance | |
| Intent-to-Treat* | |||
| 0 month | 1,114 (27.9) | 1,069 (26.7) | χ2(1) = 1.276, p = 0.259 |
| 1 month | 1,218 (30.5) | 1,216 (30.4) | χ2(1) = 0.002, p = 0.961 |
| 3 months | 1,067 (26.7) | 1,123 (28.1) | χ2(1) = 1.972, p = 0.160 |
| 6 months | 1,108 (27.7) | 1,109 (27.7) | χ2(1) = 0.001, p = 0.980 |
| HFTC n quit/n total respondents (%) |
LFTC n quit/n total respondents (%) |
Significance | |
| Excluding Non-Response† | |||
| 0 month | 1,114/1,701 (65.5) | 1,069/1,839 (58.1) | χ2(1) = 20.257, p <0.001 |
| 1 month | 1,218/1,815 (67.1) | 1,216/1,910 (63.7) | χ2(1) = 4.870, p = 0.027 |
| 3 months | 1,067/1,624 (65.7) | 1,123/1,771 (63.4) | χ2(1) = 1.943, p = 0.163 |
| 6 months | 1,108/1,664 (66.6) | 1,109/1,758 (63.1) | χ2(1) = 4.599, p = 0.032 |
Participants with missing smoking status classified as “smoking”
Participants with missing smoking status were excluded from the results; p-values reflect differences detected by chi-square analyses between reported smokers and reported non-smokers by treatment status
Outcomes from Phone Interviewees – Sub-sample
Among the 393 HFTC participants included in the call sample, the overwhelming majority (96.4%) were male, and most reported living in an urban location (84.6%) and being married (72.0%). Approximately 43% were between 18 and 29 years of age; 25.7% were ages 30–39; 23.4% were 40–49; and 8% were age 50 and older (data not shown). When comparing the demographics of interviewees who opted out to those who received the full intervention, we did not detect any significant differences. In addition, we conducted chi-square analyses to determine if people who opted out of the intervention were less likely to answer the call and complete the interview than people who did not opt out of the intervention. We found that people who opted out of the intervention completed the phone interview at a rate very similar to that of people who completed the full intervention; the difference was not significant (χ2(1) = 0.416, p = 0.519).
Table 3 presents the demographic profile of the interviewees by smoking status at the time of the interview, as well as unadjusted and adjusted odds ratios of smoking. When adjusting for all of the presented covariates, smoking status did not vary significantly by province, participant age, highest level of education, or marital status (at p < 0.05). However, interviewees who reported being in good health [adjusted odds ratio (AOR) = 2.68, 95% confidence interval (CI) = 1.69–4.24] or poor/fair health (AOR = 7.42, 95% CI = 2.36–23.37) were more likely to report smoking than those who reported excellent or very good health. Additionally, interviewees from rural areas were 3 times more likely to report continued smoking compared to participants from urban areas (AOR = 3.07, 95% CI = 1.51–6.25). In the unadjusted analysis, interviewees who were 30–39 years old had marginally higher odds (p = 0.07) of smoking compared to those younger than 29, but these results no longer approached significance when data were adjusted for the other covariates in the model.
Table 3.
Demographics by smoking status, and odds of smoking at the time of the call for the call participants*
| Demographics | Odds Ratios | |||
|---|---|---|---|---|
| Abstinent Participants (n = 180) n (%) |
Smoking Participants (n = 213) n (%) |
Unadjusted odds ratio, 95% CI |
Adjusted odds ratio, 95% CI |
|
| Province | ||||
| Zhejiang | 56 (31.1) | 64 (30.0) | 1.00 | 1.00 |
| Shaanxi | 68 (37.8) | 72 (33.8) | 0.93 (0.57, 1.51) | 0.91 (0.53, 1.57) |
| Heilongjiang | 56 (31.1) | 77 (36.2) | 1.20 (0.73, 1.98) | 1.31 (0.76, 2.26) |
| Area† | ||||
| Urban | 163 (90.6) | 167 (78.4) | 1.00 | 1.00 |
| Rural | 15 (8.3) | 45 (21.1) | 2.93 (1.57, 5.46)# | 3.07 (1.51, 6.25)# |
| Age (years)‡ | ||||
| <29 | 84 (46.7) | 83 (39.0) | 1.00 | 1.00 |
| 30–39 | 39 (21.7) | 61 (28.6) | 1.58 (0.96, 2.62) | 1.37 (0.72, 2.62) |
| 40–49 | 40 (22.2) | 51 (23.9) | 1.29 (0.77, 2.16) | 1.03 (0.53, 2.01) |
| 50+ | 15 (8.3) | 16 (7.5) | 1.08 (0.50, 2.32) | 0.96 (0.38, 2.42) |
| Education§ | ||||
| Less than HS | 51 (28.3) | 77 (36.2) | 1.00 | 1.00 |
| HS Grad or More | 124 (68.9) | 131 (61.5) | 0.70 (0.46, 1.08) | 0.89 (0.54, 1.47) |
| Marital status‖ | ||||
| Married | 119 (66.1) | 154 (72.3) | 1.00 | 1.00 |
| Single | 54 (30.0) | 52 (24.4) | 0.74 (0.48, 1.17) | 0.88 (0.47,1.67) |
| Perceived health | ||||
| Excellent/Very Good | 91 (50.6) | 59 (27.7) | 1.00 | 1.00 |
| Good | 85 (47.2) | 131 (61.5) | 2.38 (1.55, 3.64)# | 2.68 (1.69, 4.24)# |
| Fair/Poor | 4 (2.2) | 23 (10.8) | 8.87 (2.92, 26.94)# | 7.42 (2.36, 23.37)# |
Percentages represent the percent of the total by column (180 non-smoking and 213 smoking participants). Percentages may not add up to 100% due to missing data. Unadjusted and adjusted odds ratios exclude missing values.
Area of residence includes 390/393 participants. Those not represented did not disclose this information.
Participant age was included for 389/393 participants.
Highest level of education attained was provided by 383/393 participants.
Marital status includes 379/393 participants. Those not represented did not disclose their marital status.
p < 0.05
Interviewees were also asked questions about the utility of the program (Table 4). Over 80% of this sample of HFTC participants stated that the number of messages was “the right amount,” while 11.5% and 7.4% stated that there were too many or too few, respectively. The majority of interviewees responded that they read all the messages (80.7%). Interviewees responded positively to the content, with 93% stating that useful information was provided. Additionally, nearly 91% of interviewees reported that the information motivated them to quit, and 86% stated that they were likely to share the information with someone else. It is important to note that satisfaction was assessed among interviewees who had responded to the first smoking status assessment at 0 month, and does not represent those who did not respond at this time point.
Table 4.
Participant satisfaction immediately after the study among the call participants (n = 393)
| Questions | Total (%) |
|---|---|
| Number of messages read | |
| All | 317 (80.7) |
| Most/some | 71 (18.0) |
| Few/none | 5 (1.3) |
| Perception of the number of messages | |
| Not enough | 29 (7.4) |
| Too many | 45 (11.5) |
| Right amount | 319 (81.2) |
| Messages provided helpful information | 365 (92.9) |
| Messages motivated participant to quit smoking | 357 (90.8) |
| Would share messages with other smokers | 338 (86.0) |
Discussion
To our knowledge, this study is the first large randomized controlled trial of a text message–based smoking cessation program in China. This study has demonstrated that a text message–based smoking cessation intervention can be successfully delivered in China and may help increase cessation rates among China’s 300 million smokers. Although a non-active comparison group was not included in this study, the reported cessation rates across all follow-up points are quite high (26.7%–30.5%) compared to national cessation rates report from previous studies in China.3, 11 These quit rates were within the range of those found in other Chinese smoking cessation intervention studies involving a variety of treatments (8–51%).17–19 In addition, this project successfully translated and culturally adapted a U.S. smoking cessation text message library for a Chinese audience. This Chinese language library is now being disseminated to other emerging cessation programs within China.
Despite the high quit rates, the intent-to-treat analysis did not detect any difference in quit rates between the HFTC and LFTC groups. It is possible that the minimal level of information and support provided in the LFTC group was sufficient to prompt cessation among this sample of smokers who were already interested in quitting. Cessation support services are not widely available in China,8 and compared to developed/Western countries, awareness about the health risks of smoking is relatively low.9 The amount of information provided to both intervention groups may have been sufficient to encourage cessation among this population, who may be more motivated and easy to convince to quit than the average smoker in China, thus resulting in higher than expected quit rates in both intervention groups. Many participants in both groups were also seeking health information from Nokia Life Tools and therefore may have been more motivated to utilize and benefit from the intervention than the average smoker.
In contrast to the intent-to-treat analysis, our analyses excluding non-respondents found that people in the HFTC group were significantly more likely to quit smoking than those in the LFTC group at 0, 1, and 6 months follow-up. Although these findings are encouraging about the potential effectiveness of the HFTC intervention, this difference is not clinically significant and must be interpreted with caution given the high non-response and intervention opt-out rates. In view of the higher opt-out rate in the HFTC group compared with the LFTC group (42.9% and 15.4%, respectively), it is possible that the HFTC participants felt they were receiving too many text messages. This suggests that sending fewer cessation text messages may improve retention, but our subsequent findings revealed that most HFTC phone interviewees (81.2%) felt they received the right amount of texts. It is likely that the HFTC group had a higher opt-out rate in part because HFTC participants received more texts, each of which included a prompt offering the participants the opportunity to opt out. The high frequency of these texts prompting people to opt out of the intervention could have led to more opting out by HFTC than LFTC participants. Unfortunately, the number of unknowns makes it difficult to conclude that one intervention was more effective than the other. Future research should further assess the ideal number of smoking cessation messages to send to Chinese smokers to ensure that they receive adequate support without being overwhelmed by text messages.
Our analysis of the sub-sample of 393 interviewees receiving the HFTC intervention revealed two significant predictors of smoking cessation: location and perceived health status. Interviewees were more likely to continue smoking if they lived in rural rather than urban areas, or reported being in fair/poor or good health compared to excellent/very good health. Improvements in health can be seen even within a short time of smoking cessation, but it is not clear if the interviewees reported better health as a result of their quitting status. The few other studies that have assessed predictors of smoking cessation among Chinese current smokers have produced inconsistent results.11, 19, 20 Further research is needed to assess characteristics associated with cessation among Chinese smokers.
Overall results from the phone interview sub-sample show that the program received largely positive feedback, and the level of engagement was high. Most interviewees reported reading all of the text messages (80.7%), and only 11.5% thought they received too many texts. Most interviewees also said that the messages were helpful and that they would share the messages with other smokers. This high level of satisfaction suggests that other smokers in China would be willing to use and benefit from this program.
Among the strengths of this study is that its sample was one of the largest of any smoking cessation text message study to date,14, 15, 21 including participants from rural and urban areas in three Chinese provinces. This intervention was also designed using health behavior change principles, and the messages were pre-tested and adapted to match the Chinese cultural context.
This study had several limitations. All data were collected via text message, and baseline data were not collected on variables such as smoking history, patterns of tobacco use, and demographic characteristics, which prevented a fuller understanding of how these factors may have affected quit rates. Relying on self-report via text also may have elicited biased responses about quit status, as well as their opinions on the HFTC intervention. As with many smoking cessation studies, self-reported quit rates tend to be higher than biologically verified quit rates.14, 22 The actual smoking abstinence rate is likely to have been lower than what was reported.
In addition to high opt-out rates, the low post-intervention response rates also hindered our ability to assess the impact of the intervention. This is a common limitation of automated mhealth and ehealth interventions, and previous research suggests that the most efficient way to counter this possibility is by making multiple attempts to personally call each participant who did not respond.23 Limited resources prevented us from pursuing this method of follow-up, but this should be considered in future research. Lastly, the two intervention groups differed in terms of number of text messages as well as in the breadth and depth of the content they received, which would have confounded the relationship between number of texts and content had our study detected a meaningful difference between the two intervention groups. Future studies should take this into account when identifying appropriate control groups. In the future, multi-arm trials that can manipulate more than one parameter would be helpful to assess what attributes increase the effectiveness of the intervention.
Despite these limitations, our study suggests that mobile phone cessation interventions can help fill the large gap in cessation support services in China.8 China has more than one-third of the world’s smokers2 and the cost of smoking is rising rapidly7; evidence-based text message cessation services may offer a cost-effective method of cessation support that capitalizes on existing mobile technology that is highly utilized in China.13 This study yielded overwhelmingly positive feedback about the intervention and high quit rates in both groups, which suggests that further study of a cessation text messaging intervention in China and other large, high-burden countries is warranted.
In conclusion, our study found that a text message–based cessation intervention is feasible to implement in China and may increase cessation rates. Users reported high levels of satisfaction and willingness to participate in the program and recommend the program to other smokers. Further research is needed both to assess more accurately the intervention’s impact on smoking cessation and to determine which intervention attributes are most effective in increasing long-term smoking abstinence.
SO WHAT- Implications for Health Promotion Practitioners and Researchers.
What is already known on this topic?
Research suggests that text message–based interventions could be effective in motivating or sustaining smoking cessation efforts. However, these efforts had not been tested on a large scale in China, where smoking rates are high, knowledge of the health effects of smoking is low, motivation to quit is low, and availability of cessation treatment is very limited.
What does this article add?
Findings show that a large-scale smoking cessation intervention utilizing text messages is feasible to implement in rural and urban areas in China, and may positively affect smoking cessation attempts.
What are the implications for health promotion practice or research?
This evidence-based smoking cessation message library for Chinese smokers shows great promise for increasing smoking cessation, but additional research is needed to further evaluate what attributes of text message interventions are effective at increasing smoking cessation rates in resource-limited countries. With more than 301 million smokers in China, this low-burden mhealth intervention has great potential to reduce smoking-related morbidity and mortality in China by educating, motivating, and supporting smokers who are interested in quitting.
Acknowledgments
This project has been funded in part with Federal funds from the National Cancer Institute, National Institutes of Health, U.S. Department of Health and Human Services, under Contract No. HHSN261201000043C.
Footnotes
Disclaimer
The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Cancer Institute.
There are no conflicts of interest to report.
References
- 1.World Health Organization. Geneva, Switzerland: WHO; 2010. [Accessed July 30, 2014]. Global Adult Tobacco Survey (GATS) fact sheet – China, 2010. http://www.who.int/tobacco/surveillance/en_tfi_china_gats_factsheet_2010.pdf. [Google Scholar]
- 2.Feng G, Jiang Y, Li Q, et al. Individual-level factors associated with intentions to quit smoking among adult smokers in six cities of China: findings from the ITC China Survey. Tob Control. 2010;19(suppl 2):i6–i11. doi: 10.1136/tc.2010.037093. PMCID: PMC2976002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qian J, Cai M, Gao J, Tang S, Xu L, Critchley JA. Trends in smoking and quitting in China from 1993 to 2003: National Health Service Survey data. Bull World Health Organ. 2010;88:769–776. doi: 10.2471/BLT.09.064709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gu D, Kelly TN, Wu X, et al. Mortality attributable to smoking in China. N Engl J Med. 2009;360(2):150–159. doi: 10.1056/NEJMsa0802902. [DOI] [PubMed] [Google Scholar]
- 5.He Y, Jiang B, Li LS, et al. Changes in smoking behavior and subsequent mortality risk during a 35-year follow-up of a cohort in Xi’an, China. Am J Epidemiol. 2014;179(9):1060–1070. doi: 10.1093/aje/kwu011. [published online ahead of print March 27, 2014]. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J, Ou J-X, Bai C-X. Tobacco smoking in China: prevalence, disease burden, challenges and future strategies. Respirology. 2011;16(8):1165–1172. doi: 10.1111/j.1440-1843.2011.02062.x. [DOI] [PubMed] [Google Scholar]
- 7.Yang L, Sung HY, Mao Z, Hu TW, Rao K. Economic costs attributable to smoking in China: update and an 8-year comparison, 2000–2008. Tob Control. 2011;20(4):266–272. doi: 10.1136/tc.2010.042028. [published online ahead of print February 21, 2011]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ITC Project and Office of Tobacco Control, China CDC. ITC China Project Report: Findings from the Wave 1 to 3 Surveys (2006–2009) Waterloo, Ontario, Canada: University of Waterloo; Beijing, China: Office of Tobacco Control, Chinese Center for Disease Control and Prevention; Beijing, China: China Modern Economic Publishing House; 2012. [Google Scholar]
- 9.Yang J, Hammond D, Driezen P, Fong GT, Jiang Y. Health knowledge and perception of risks among Chinese smokers and non-smokers: findings from the Wave 1 ITC China Survey. Tob Control. 2010;19(suppl 2):i18–i23. doi: 10.1136/tc.2009.029710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Antismoking messages and intention to quit—17 countries, 2008–2011. MMWR Morb Mortal Wkly Rep. 2013;62(21):417–422. [PMC free article] [PubMed] [Google Scholar]
- 11.Yang J, Hammond D, Driezen P, et al. The use of cessation assistance among smokers from China: findings from the ITC China Survey. BMC Public Health. 2011;11(1):75. doi: 10.1186/1471-2458-11-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Global Observatory for eHealth Series, vol. 3L. Geneva, Switzerland: WHO; 2011. [Accessed July 30, 2014]. mHealth: New Horizons for Health Through Mobile Technologies: Second Global Survey on eHealth. http://www.who.int/goe/publications/goe_mhealth_web.pdf. [Google Scholar]
- 13.World Bank. The Little Data Book on Information and Communication Technology 2013. Washington, DC: World Bank, International Bank for Reconstruction and Development; 2013. [Accessed July 30, 2014]. https://openknowledge.worldbank.org/bitstream/handle/10986/14453/9780821398166.pdf?sequence=2. [Google Scholar]
- 14.Whittaker R, McRobbie H, Bullen C, Borland R, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD006611. doi: 10.1002/14651858.CD006611.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Shi H-J, Jiang X-X, Yu C-Y, Zhang Y. Use of mobile phone text messaging to deliver an individualized smoking behaviour intervention in Chinese adolescents. J Telemed Telecare. 2013;19(5):282–287. doi: 10.1177/1357633X13495489. [published online ahead of print July 9, 2013]. [DOI] [PubMed] [Google Scholar]
- 16.Sen S. Nokia: news you can use. Nokia connects through an SMS-based information service. [Accessed July 30, 2014];Business Today. http://businesstoday.intoday.in/story/innovation-nokia-connects-through-sms-based-information-service/1/195887.html. Published July 7, 2013. [Google Scholar]
- 17.Kim SS, Chen W, Kolodziej M, Wang X, Wang VJ, Ziedonis D. A systematic review of smoking cessation intervention studies in China. Nicotine Tob Res. 2012;14(8):891–899. doi: 10.1093/ntr/ntr289. [DOI] [PubMed] [Google Scholar]
- 18.Sheng LX, Tang YL, Jiang ZN, et al. Sustained-release bupropion for smoking cessation in a Chinese sample: a double-blind, placebo-controlled, randomized trial. Nicotine Tob Res. 2013;15(2):320–325. doi: 10.1093/ntr/nts124. [published online ahead of print May 21, 2012]. [DOI] [PubMed] [Google Scholar]
- 19.Zheng P, Guo F, Chen Y, Fu Y, Ye T, Fu H. A randomized controlled trial of group intervention based on social cognitive theory for smoking cessation in China. J Epidemiol. 2007;17(5):147–155. doi: 10.2188/jea.17.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun H-Q, Guo S, Chen D-F, et al. Family support and employment as predictors of smoking cessation success: a randomized, double-blind, placebo-controlled trial of nicotine sublingual tablets in Chinese smokers. Am J Drug Alcohol Abuse. 2009;35(3):183–188. doi: 10.1080/00952990902839794. [DOI] [PubMed] [Google Scholar]
- 21.Kong G, Ells DM, Camenga DR, Krishnan-Sarin S. Text messaging-based smoking cessation intervention: a narrative review. Addict Behav. 2014;39(5):907–917. doi: 10.1016/j.addbeh.2013.11.024. [published online ahead of print December 4, 2013]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Connor Gorber S, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res. 2009;11(1):12–24. doi: 10.1093/ntr/ntn010. [published online ahead of print January 27, 2009]. [DOI] [PubMed] [Google Scholar]
- 23.Geraghty AW, Torres LD, Leykin Y, Perez-Stable EJ, Munoz RF. Understanding attrition from international Internet health interventions: a step towards global ehealth. Health Promot Int. 2013;28(3):442–452. doi: 10.1093/heapro/das029. [published online ahead of print July 10, 2012]. [DOI] [PMC free article] [PubMed] [Google Scholar]