Abstract
Objectives
Questionnaire-based research has shown that parents exert a powerful influence on and are profoundly influenced by living with a child with chronic pain. Examination of parents' pain narratives through an observational lens offers an alternative approach to understanding the complexity of pediatric chronic pain; however, the narratives of parents of youth with chronic pain have been largely overlooked. The present study aimed to characterize the vulnerability- and resilience-based aspects of the pain narratives of parents of youth with chronic pain.
Methods
Pain narratives of 46 parents were recorded during the baseline session as part of two clinical trials evaluating a behavioral intervention for parents of youth with chronic pain. The narratives were coded for aspects of pain-related vulnerability and resilience.
Results
Using exploratory cluster analysis, two styles of parents’ pain narratives were identified. Distress narratives were characterized by more negative affect and an exclusively unresolved orientation towards the child’s diagnosis of chronic pain whereas resilience narratives were characterized by positive affect and a predominantly resolved orientation towards the child’s diagnosis. Preliminary support for the validity of these clusters was provided through our finding of differences between clusters in parental pain catastrophizing about child pain (helplessness).
Discussion
Findings highlight the multidimensional nature of parents’ experience of their child’s pain problem. Clinical implications in terms of assessment and treatment are discussed.
Keywords: Narratives, pain, chronic pain, adolescents, children, parents
Parents are integral to an understanding of the experience of chronic pain in children and adolescents. Over the past decade, the field of pediatric pain has made great strides in developing quantitative measures to assess a range of parent cognitions, beliefs, and behaviors related to their child’s pain including fear of pain1, acceptance2, psychological flexibility3, 4, catastrophizing5, protective responses to child pain6 and the impact of parenting a child with chronic pain7. This has led to important advances in our understanding of the powerful influence of parents on the development and maintenance of pediatric chronic pain and disability, and the profound impact that parenting a child with pain can have on parents’ own emotional and behavioral functioning.
To date, the majority of studies in this area have been conducted using quantitative survey measures typically probing unidimensional aspects of parents’ emotional functioning and/or behavioral responses. Qualitative approaches and behavioral observation might offer unique, nuanced insights into the parenting experience that cannot be gleaned from questionnaire measures. Unlike questionnaire measures, parents’ pain narratives (i.e., their verbal accounts of the origin of their child’s pain problem and the impact it has had on their family) offer a fruitful opportunity to understand this complex experience. Narratives also more closely approximate the information provided to clinicians in real-world clinical encounters. However, to date, the pain narratives of parents of youth with chronic pain have been largely overlooked.
Narratives are considered a fundamental human cognitive activity involving memory, language, time, and our understanding of causal effects8. They are inherently communicative in nature and direct the listener’s attention. People tell stories to a listener for a purpose, and narratives are constructed and shaped as a result of this interaction8. Narratives convey meaning, interpretation, and expectancies: all factors that can shape the pain experience. In the broader field of medicine, “narrative competence” is considered an essential medical skill for physicians and involves recognizing, absorbing, interpreting, and being moved by stories of illness9. For pain management clinicians working with youth with chronic pain, a patient’s pain narrative is often the first source of information offered. In pediatric pain management clinics, parents are often involved in this telling, yet, their story of personal impact is not always elicited. Parents’ pain narratives may offer valuable insights that can be used by clinicians to build rapport, develop shared treatment goals, and guide clinical decision-making.
Parents’ pain narratives have only been previously examined in three qualitative studies. Jordan and colleagues10 conducted focus group interviews with parents to examine the impact that caring for an adolescent with chronic pain had on them. Narratives were primarily characterized by negative impact. Parents described feeling stuck in an unusual, developmentally immature pattern of parenting. They described that their expectations about their own and their child’s life had been violated, leaving them with a sense of loss, uncertainty, uncontrollability, and fear. Just as patients struggle to obtain legitimacy with respect to their diagnosis, parents themselves described searching for such legitimacy for their child. Similar themes of disempowerment and suffering were found in a qualitative examination of 9 parents of children and adolescents with chronic pain who were enrolled in a pain rehabilitation program11. Like the parents in the study by Jordan and colleagues, these parents described feeling a lack of control, disrupted or “disabled” parenting, fear, lack of support from broader community, and endless searching in an exasperating journey to find relief for their child’s pain. Nevertheless, parents also described a sense of empowerment emerging from the process of rehabilitation, indicating a degree of hopefulness among the more dominant themes of distress. The third, more recent qualitative study by Jordan and colleagues examined pain narratives of six fathers of adolescents with chronic pain12. Findings similarly revealed a largely negative impact on fathers characterized by disempowerment, helplessness, and struggling to balance competing roles; however, some fathers identified ways in which they renegotiated their relationships with their children in order to manage disruption caused by pain. Importantly, there were individual differences in the meaning fathers ascribed to their experience as well as their coping. Whereas some fathers reported a sense of loss about their weakened relationship with their child, other fathers described a more positive relationship as a result of the pain. For some, they described changes in their family experience of adversity evolving from grief and despair to resilience and closeness, highlighting the intra-individual change that can occur for parents over time. Examination of parent narratives in these studies revealed important insights into the parenting experience that could otherwise not be fully captured by questionnaire-based measures.
Broader narrative-based research would suggest that the content of parents’ pain narratives tells only half of the story. Beyond content, the affective context is integral to understanding pain narratives8. Missing from the pediatric pain literature is examination of both the content and affective tone of parents’ pain narratives. Moreover, recent research on resilience-based constructs and processes (acceptance, psychological flexibility, optimism) among parents of youth with chronic pain2, 4, 12, 13 emphasize the merit in examining themes pertaining to resilience in addition to emotional burden. Finally, pain narratives shared in a therapeutic context (i.e., with a psychologist, physician, or other provider in treatment) may reveal unique insights that are not offered in non-therapeutic contexts (e.g., focus groups, face-to-face interviews with a researcher).
Patient narratives have been categorized as falling into two general profiles: “chaos narratives” (stories of lives falling apart) and “restitution narratives” (stories of unexpectedly finding benefit in the face of illness and loss)14. Among adults with chronic pain, pain narrative profiles have been identified as involving stigma15 as well as survival16. Such characterization of the pain narratives of parents of children with chronic pain may expand understanding of such profiles.
Thus, the objective of the current study was to characterize parents’ pain narratives from the baseline phase of a parent psychological treatment for their child’s chronic pain. Specific aims were to: (a) examine both resilience-based (e.g., resolved orientation to diagnosis, optimism, benefit-finding, humor, positive affect) and vulnerability-based (e.g., unresolved orientation to diagnosis, threat/anxiety, stressful/potentially traumatic events, negative affect) aspects of the content and affect of parents’ pain narratives; and (b) explore profiles/styles of parents’ pain narratives based on both content and affect. We hypothesized that parents would express aspects of both vulnerability and resilience. We also hypothesized that there would be more than one narrative style and that narrative styles would be differentially characterized by features of vulnerability and resilience. Finally, our exploratory hypothesis was that parents’ catastrophic thinking about child pain, as a robust predictor parents’ negative emotional and behavioral responses to child pain1,5, would be more highly associated with features of vulnerability in the narratives in contrast to features of resilience.
Method
Potentially eligible participants were identified by providers in two interdisciplinary chronic pain programs. Study staff screened participants for eligibility and obtained consent. Inclusion criteria were: (a) child was between 10 and 18 years of age; (b) child had pain occurring at least once a week for at least 3 months that interfered with daily functioning; and (c) parents could read and speak English. Exclusion criteria were: (a) child had another serious medical condition (e.g., arthritis, cancer); (b) parent did not currently live with the child; and (c) parent had a serious psychiatric comorbidity (e.g., active psychosis, suicidal ideation).
Procedure
Participants were enrolled in one of two psychological treatment studies evaluating a problem solving skills training (PSST) intervention for parents of children with chronic pain. Details about the intervention are described elsewhere17. Both studies received Institutional Review Board approval. One study recruited parents from outpatient pediatric pain clinics in the Pacific Northwest (n = 28), and the other study recruited parents from intensive pediatric pain rehabilitation programs in the Pacific Northwest and Midwestern United States (n = 18). Only participants randomized to the active treatment arm were included in the present study as they were the only parents who provided pain narratives. Parent pain narratives were elicited during the first session. Study interventionists were trained PhD-level psychologists with experience in pediatric pain management. The first session was identical across the two intervention studies and involved establishing rapport with parents by asking parents to tell the story of their child’s pain problem. All sessions were audio recorded.
Therapists used a non-directive style to ask the parent to tell his/her story of their child’s pain problem and specifically how it had affected him/her and his/her family. This was described in the manual as follows: “The therapist will use a non-directive style to ask the caregiver to tell her story of the child’s pain problem and specifically how it has affected the caregiver and family. Probes can be used to expand the caregiver’s focus to allow the therapist to understand all of the areas of impact on child functioning, parent functioning, and family functioning. For example, the instructor can ask the caregiver to comment about the following areas of potential impact (e.g., how has the pain problem affected….?): Child functioning (e.g., physical functioning, emotional functioning, sleep, school social/peer relationships); Parent functioning (social relationships, time, emotional impact); and Family functioning (conflict vs. harmony, finances, participation in important family activities).”
The majority of first sessions (89.4%) were completed in person with a therapist; however, some sessions (8.7%) were completed by phone. The first author (MN), a trained PSST therapist, listened to all audio recordings of these sessions and selected the start times that narratives occurred. End times were made standard at 15 minutes after the narrative began. This was to standardize time across narratives and approximate a realistic amount of time that a clinician could devote to eliciting and listening to a pain narrative in practice.
Parents completed baseline measures either by paper or online prior to the start of treatment. We did not include follow-up data in this particular paper because the follow-up data collection is still in progress and our study aims do not include examining treatment efficacy.
Measures
Demographics
Parents reported on their relationship to their child (i.e., biological mother, father), marital status, race, ethnicity, education, and socioeconomic status as well as their child’s age, sex, race, and ethnicity.
Pain Questionnaire
The pain questionnaire was administered to youth to describe details about their pain (frequency, intensity, duration) over the prior month. Average pain intensity was measured using an 11-point Numeric Rating Scale (0–10)18. Pain frequency was assessed using a Likert-type scale with six response options ranging from less than once a month to daily. Duration of the child’s pain problem was rated on a Likert-type scale with six response options ranging from less than three months to 5 years or more. This questionnaire has demonstrated adequate validity in children with chronic pain for rating pain intensity, frequency, and duration19.
Pain Catastrophizing Scale –Parent version (PCS-P)
The PCS-P is a 13-item self-report measure that assesses catastrophic thoughts and feelings that parents may have when their child experiences pain5. Items on the PCS-P are rated on a five-point Likert scale yielding a total score and three subscale scores: Rumination, Magnification, and Helplessness. Parents rate the extent to which they experience each thought or feeling when their child is in pain (e.g., “When my child is in pain, I feel I can’t go on like this much longer”). Lower scores indicate less Rumination, Magnification, or Helplessness about child pain. The PCS-P has been found to have good validity and reliability among parents of youth with chronic pain and is related to parent emotional distress (parenting stress, depression, anxiety) and child functional disability beyond child pain intensity5.
Bath Adolescent Pain Questionnaire (BAPQ)
The BAPQ is a 61-item self-report measure that assesses seven domains of adolescent functioning affected by pain: Social Functioning, Physical Functioning, Depression, General Anxiety, Pain-Specific Anxiety, Family Functioning, and Development20. Youth rate items on a five-point Likert scale ranging from never to always, yielding seven subscale scores. There is also a total score. Lower scores indicate less functional impairment. Research has shown that the BAPQ subscales have good internal consistency, construct validity, and temporal stability among samples of youth with chronic pain20. For the purposes of describing the sample in the present study, the subscales comprising the Daily Functioning Score (Physical and Social subscales) were used as the indicators of functional impairment.
Construction of the Pain Narrative Coding Scheme
The first and second authors (MN, SBE) developed the Pain Narrative Coding Scheme based on published recommendations for developing behavioral coding schemes for children and families with chronic medical conditions21 as well as broader pediatric literature on parents’ verbal interactions (affect and content) and their influence on psychological and functional outcomes22, 23. Moreover, behaviors of interest were informed by existing literature on parent distress in the context of chronic pain7, 10, 24 as well as factors implicated in the development of pain memories and parent-child narratives about pain25. A list of narrative codes is presented in Table 2.
Table 2.
Descriptive statistics for the parent pain narratives codes.
| Pain Narrative Code | Mean (SD) or Frequency (%) |
Possible Range |
Actual Range |
Percentile (Score) |
|---|---|---|---|---|
| Stressor count | 2.11 (1.72) | 0–32 | 0 – 7 | 25 (1); 50 (2); 75 (3) |
| Positive affect intensity | 2.80 (.75) | 1–5 | 2–5 | 25 (2); 50 (3); 75 (3) |
| Positive affect frequency | 2.72 (.69) | 1–5 | 2–4 | 25 (2); 50 (3); 75 (3) |
| Negative affect intensity | 3.15 (.82) | 1–5 | 2–5 | 25 (3); 50 (3); 75 (4) |
| Negative affect frequency | 3.02 (.75) | 1–5 | 2–4 | 25 (2); 50 (3); 75 (4) |
| Humor/Laughter | 2.93 (1.12) | 1–5 | 1–5 | 25(2); 50 (3); 75 (4) |
| Anger | 2.87 (.96) | 1–5 | 1–5 | 25 (2); 50 (3); 75 (3) |
| Threat/Anxiety | 3.09 (1.01) | 1–5 | 1–5 | 25(2); 50 (3); 75 (4) |
| Benefit finding/growth | 1.54 (.72) | 1–5 | 1–3 | 25(1); 50 (1); 75 (2) |
| Pessimism/Optimism | 3.15 (1.21) | 1–5 | 1–5 | 25 (2); 50 (3); 75 (4) |
| Diagnosis Orientation | ||||
| Resolved | 28 (60.9%) | |||
| Unresolved | 18 (39.1%) |
The Family Interaction Macro-coding System (FIMS26) was the primary coding scheme from which the current Pain Narrative Coding Scheme was based. The FIMS contains codes assessing interactional style, conflict, control, affect, problem solving, and family systems that are rated on five-point Likert scales. Behavioral descriptions of each code are provided in the coding manual (available from the first author upon request).
Affect Codes
For the purpose of developing the Pain Narratives Coding Scheme, the following six FIMS affect codes were used: Intensity of Positive Affect Expression/Emotionality; Frequency of Positive Affect; Intensity of Negative Affect Expression/Emotionality; Frequency of Negative Affect; Humor and Laughter; and Anger. The operational definitions of these six affect codes were modified and refined to pertain to the affective quality of parent narratives that could be gleaned from audio as opposed to interaction gleaned from video (e.g., laughing and joking vs. laughing, joking, and smiling). In addition, specific guidance was included in the manual with respect to some response options regarding the frequency of a behavior that needed to be endorsed (e.g., “rarely” expresses humor or laughter was defined as exhibiting this behavior 1–2 times). Such modifications were made to improve reliability given the difficulty inherent in reliably rating macro-level codes27.
The following are direct quotations from parents that exemplify affect codes; however, tone of voice was an important cue that coders used when assigning levels on these codes.
Positive Affect
“We were lucky to get in as quickly as we did…I feel good that we caught it early enough.”
“I’m thrilled to be here!”
“She did a great job in all her classes. I applaud her in that.”
Negative Affect
“I was at wit’s end and didn’t know what to do and I was crying and upset.”
“I had a complete and total meltdown one day, in the office, prior to the end of tax seasons, I said I can’t do it…it was a lot.”
“I don’t know why I’m so tearful today [crying]… I talk about it all the time, but just all the sudden I feel like crying.”
“I’m just worried…I just don’t think it’s fair that a 10-year-old could have pain for the rest of her life [crying].”
Humor/Laughter
“Let’s see here…I have memory issues [laughs].”
“People keep asking [child] ‘How are you feeling?’… [child’s response was]‘Well, I’m going through puberty…I’m all over the place!’[laughs]”
Anger
“We just weren’t very happy with our care with [the pain doctor]…it’s like he didn’t even review his chart or the notes or anything. And he was pretty condescending and he was pretty sure it was something that she was doing.”
“I was very resentful to him [husband] and I didn’t want to do anything to help him.”
“We had a bad situation with the doctor on the telephone, he was rude and condescending and he told me that basically I was an overprotective mother…I have some frustration with that.”
Content Codes
In addition to the inclusion of affect codes, the following five content codes were used: Threat/Anxiety; Benefit-Finding/Growth; Pessimism/Optimism; Diagnosis Orientation (regarding diagnosis of chronic pain); and Potentially Traumatic/Stressful Events. Content was coded based on explicit statements made by the caregiver whereas affect codes took into account tone of voice as well as content. The Threat/Anxiety, Benefit-Finding/Growth, and Pessimism/Optimism codes were each rated on a five-point Likert scale. The Pessimism/Optimism code was based on the same code included in the Expressed Emotion Coding system28. Higher scores on the Pessimism/Optimism code reflected higher optimism and lower pessimism; lower scores on this code reflected lower optimism and higher pessimism. Operational definitions for the Threat/Anxiety code were informed by definitions of pain catastrophizing about child pain5 and general anxiety29 used in the literature. An operational definition for the Benefit-Finding/Growth code was informed by literature on benefit-finding in the context of childhood cancer and diabetes30, 31 and was developed to be specific to benefit derived from the experience of children’s chronic pain problems. Both the Threat/Anxiety and Benefit-Finding/Growth codes pertained to statements about the child, parent, family, or broader society. In addition, parents were rated as being Resolved or Unresolved in terms of their orientation towards their child’s diagnosis of chronic pain. This code was adapted from the Reaction to Diagnosis Interview coding system32, 33. A resolved orientation was characterized by expressing a change in feelings since the time of their child’s diagnosis; for example, by moving on from the trauma or disorganization that often occurs. Parents may express no longer searching for an alternative diagnosis. Conversely, an unresolved diagnosis was characterized by little change in thoughts/feelings since diagnosis or a preoccupation with their emotional response since that time (e.g., they may be preoccupied with why this happened). Parents may describe actively searching for a different diagnosis in the face of contradictory evidence, a belief that their child will grow out of chronic pain, or unrealistic expectations in the face of strong evidence to the contrary. Individuals may seem stuck in the past.
The following are direct quotations from parents that exemplify the aforementioned content codes:
Threat/anxiety
“I would be afraid…‘What if she falls?’…”
“She was just terrified.”
“My initial instinct was panic [about CRPS diagnosis]…I immediately went to worst-case scenario.”
Benefit finding
“The positive side of headaches is she’s had to let go of that a little bit…and say there are other things that are more important than that one thing [having a 4.0 grade point average].”
“I have chronic pain and fatigue…and I’m actually benefitting from a lot of the information [child] is getting [in pain rehab program]…It’s really going to be something we can work on together, so it’s kind of exciting.”
Pessimism/Optimism
“There was no relief, no hope, no nothing.”
“Once I found a support group and I found other parents whose kids have chronic illness, that totally changed it for me because then you realize, ‘Oh I’m not alone, these people know exactly what I’m talking about…so that was a lifesaver to find a group and that just did it for me, it turned me around…”
“As frustrating as it is for her, she does see the light at the end of the tunnel.”
“Hopefully…after yesterday I feel like she’ll get her function back”
Diagnosis orientation
“So they diagnosed him with CVS [cyclic vomiting syndrome], and that was the beginning of a very, very long journey.” [coded as resolved]
“They still didn’t do anything, they just send you home after a day, they didn’t even draw bloodwork…I worry that it’s not complex regional pain and that they’re not looking…maybe it is and maybe it isn’t. I don’t know.”[coded as unresolved]
Finally, coders counted the number of potentially traumatic or stressful events (PTEs) that parents referenced according to the events included in the 30-item Life Events Scale34 to provide a broad assessment of stressful life events that have been found to be salient correlates of post-traumatic stress symptoms in youth with medical illnesses35. Other items were added (i.e., transferring schools and child suicide attempts or self-harm) as potential PTEs that were described by parents in the pain narratives. PTEs were coded as being present or absent. It is important to note that traumatic events that were coded were only those events that were captured in the 15-minute narrative and therefore are not intended to reflect all traumatic events that parents may have experienced in their lifetime.
The lead researcher who developed the PSST intervention for parents of youth with chronic pain (TP) reviewed the coding scheme and her feedback was incorporated into subsequent revisions.
Implementation of Coding Scheme and Reliability
The coding scheme was intended to capture parent narratives for a fixed period of time (e.g., the first 15 minutes) during which the parent talked about their child’s chronic pain problem. As such, the coding scheme provides an assessment of the initial affective framing and content of the parent’s pain narrative prior to any therapeutic intervention.
Both the primary (SBE) and secondary (MN) coders were PhD-level clinical psychologists who were trained to deliver the PSST Intervention. The primary coder (SBE) was not a therapist of any of the parents included in this study in order to eliminate potential coding bias. Pilot testing of the coding scheme was completed on five audio recordings; additional refinements were made to the coding scheme (e.g., expanding operational definitions) and then the master codes were finalized. Disagreements were discussed between coders and consensus about all final codes was reached. Arbitration by a third party was not needed to reach consensus. Training continued until a certain level of reliability was reached (80%). Consistent with published recommendations21 the secondary coder (MN) coded an additional randomly selected subset of audio recordings (20%) to calculate reliability. Using all codes (with the exception of potentially traumatic or stressful event counts that led to very high estimates of reliability), the average intraclass correlation for these 9 observations was .86, indicating a high degree of agreement36.
Data Analysis
To characterize parents’ pain narratives, descriptive analyses (frequencies, means, standard deviations, ranges, percentages, quartiles) were first conducted on the narrative codes. To provide validity on the coding scheme, bivariate correlations were computed between pain narrative codes to confirm that codes reflecting negative content and affect were positively related to each other and not vice versa. The one categorical narrative code (diagnosis orientation) was entered into a chi-square test to examine whether narrative codes differed as a function of whether parents were Resolved or Unresolved regarding their child’s diagnosis of chronic pain. Two-step cluster analysis was then used to characterize parents’ pain narrative profiles/styles. Two-step clustering (as opposed to k-means or hierarchical clustering alone) has the advantage of being able to accommodate both categorical (diagnosis orientation) and continuous narrative codes (all other narrative variables). Exploratory analyses were conducted to examine whether narrative typologies, which emerged from cluster analysis, were significantly different in terms of parents’ catastrophic thinking about child pain and adolescent pain-related functioning.
Results
Participants
Participants were 46 caregivers (41 mothers, 4 fathers, and 1 grandmother who was the legal guardian) of 46 children (11 boys; 35 girls) with chronic pain (Mage = 14.51, SD = 2.00, Range = 10–18 years). Parents predominantly self-identified as White. Approximately 74% of the sample was married and most had completed college or graduate school (70%). Overall, youth in the sample reported experiencing pain on a frequent basis (79.5% reporting daily pain in the past month) that was usually of high intensity (M = 6.59/10, SD = 1.53). See Table 1 for demographic information and pain characteristics of the sample.
Table 1.
Participant characteristics.
| Variable | Mean (SD) or Frequency (%) |
Mean (SD) or Frequency (%) |
Mean (SD) or Frequency (%) |
|---|---|---|---|
| Total Sample (n = 46) |
Distress Narratives (n = 26) |
Resilience Narratives (n = 20) |
|
| Parent age (years) | 46.17 (6.05) | 45.38 (5.36) | 47.20 (6.85) |
| Caregiver role | |||
| Mother | 41 (89.1%) | 24 (92.3%) | 17 (85.0%) |
| Father | 4 (8.7%) | 2 (7.7%) | 2 (10.0%) |
| Grandmother | 1 (2.2%) | 0 (0%) | 0 (0%) |
| Other | 0 (0%) | 0 (0%) | 1 (5.0%) |
| Caregiver race | |||
| White | 41 (89.1%) | 23 (88.5%) | 18 (90.0%) |
| Asian | 1 (2.2%) | 1 (3.8%) | 0 (0%) |
| American Indian/ Alaska native | 1 (2.2%) | 0 (0%) | 1 (5.0%) |
| Other | 7 (15.2%) | 2 (7.7%) | 1 (5.0%) |
| Marital Status | |||
| Married | 34 (73.9%) | 18 (69.2%) | 16 (80.0%) |
| Widowed | 1 (2.2%) | 0 (0%) | 1 (5.0%) |
| Divorced | 9 (19.6%) | 8 (30.8%) | 1 (5.0%) |
| Separated | 1 (2.2%) | 0 (0%) | 1 (5.0%) |
| Remarried | 1 (2.2%) | 0 (0%) | 1 (5.0%) |
| Parent Education | |||
| High School | 4 (8.7%) | 3 (11.5%) | 1 (5.0%) |
| Some college/vocational school | 9 (19.6%) | 6 (23.1%) | 3 (15.0%) |
| College | 24 (52.2%) | 11 (42.3%) | 13 (65.0%) |
| Graduate school | 9 (19.6%) | 6 (23.1%) | 3 (15.0%) |
| Child age | 14.51 (2.00) | 14.27 (2.01) | 14.83 (2.00) |
| Child gender | |||
| Male | 11 (23.9%) | 9 (34.6%) | 2 (10.0%) |
| Female | 35 (76.1%) | 17 (65.4%) | 18 (90.0%) |
| Child pain intensity (usual) | 6.59 (1.53) | 7.04 (1.46) | 6.05 (1.47) |
| Child pain frequency (past month) | |||
| Not at all | 1 (2.3%)* | 1 (4.2%)* | 0 (0.0%) |
| 1–3 times per month | 1 (2.3%) | 1 (4.2%) | 0 (0.0%) |
| 1 time per week | 3 (6.8%) | 3 (12.5%) | 0 (0.0%) |
| 2–3 times per week | 2 (4.5%) | 2 (8.3%) | 0 (0.0%) |
| 3–6 times per week | 2 (4.5%) | 1 (4.2%) | 1 (5.0%) |
| daily | 35 (79.5%) | 16 (66.7%) | 19 (95.0%) |
| Pain duration | |||
| < 3 months | 1 (2.3%) | 1 (4.2%) | 0 (0.0%) |
| 3–6 months | 12 (27.3%) | 6 (25.0%) | 6 (30.0%) |
| 1 year | 5 (11.4%) | 2 (8.3%) | 3 (15.0%) |
| 2 years | 9 (20.5%) | 5 (20.8%) | 4 (20.0%) |
| 3 years | 2 (4.5%) | 2 (8.3%) | 0 (0.0%) |
| 4 years | 3 (6.8%) | 1 (4.2%) | 2 (10.0%) |
| 5 years or more | 12 (27.3%) | 7 (29.2%) | 5 (25.0%) |
| Functional Disability | 26.83 (10.51) | 27.82 (12.84) | 25.75 (7.32) |
Note: During screening for eligibility, all youth had been evaluated in an interdisciplinary chronic pain clinic and reported experiencing pain that occurred at least once a week for at least 3 months that interfered with their daily functioning. Nevertheless, one adolescent self-reported experiencing no pain in the past month on the Pain Questionnaire.
Validity of Pain Narrative Coding Scheme
Descriptive statistics for all of the parent pain narrative codes are shown in Table 2. Bivariate correlations between parent pain narrative codes (Table 3) were conducted to confirm that positive and negative codes were correlated in the expected directions. As expected, many of the codes reflecting negative affect and content were positively related to each other and negatively related to codes reflecting positive and adaptive affect and content suggesting preliminary validity for the coding scheme.
Table 3.
Correlations between parent pain narrative codes.
|
N = 46 Variables |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Stressor Count | 1.00 | .22 | .18 | −.14 | .09 | .02 | .10 | −.07 | .04 | .04 |
| 2. Positive Affect Intensity | 1.00 | .71*** | −.24 | −.47** | .57*** | −.16 | −.10 | .33* | .55*** | |
| 3. Positive Affect Frequency | 1.00 | −.44** | −.68** | .55*** | −.16 | −.22 | .41** | .61*** | ||
| 4. Negative Affect Intensity | 1.00 | .73** | −.13 | .34* | .31* | −.18 | −.29* | |||
| 5. Negative Affect Frequency | 1.00 | −.37* | .38* | .26 | −.48** | −.60*** | ||||
| 6. Humor/ Laughter | 1.00 | .05 | −.15 | .24 | .19 | |||||
| 7. Anger | 1.00 | .13 | −.38* | −.27 | ||||||
| 8. Threat/ Anxiety | 1.00 | −.16 | −.23 | |||||||
| 9. Benefit finding/ Growth | 1.00 | .41** | ||||||||
| 10.Optimism/ Pessimism | 1.00 |
Note:
p < .05,
p < .01,
p < .001
Exploratory cluster analysis
An exploratory two-step cluster analysis was used to test if the number of narrative codes used could be reduced to create meaningful profiles of parents’ narratives. Profiles were based on the 11 parent pain narrative codes. The maximum number of clusters was set to 5, and data yielded a significant two-profile solution with adequate estimation (average silhouette score = .30). Generally a silhouette score of 0 indicates minimal distinction between clusters, whereas scores closer to 1 indicate more distinct clustering. Our silhouette coefficient fell in the adequate range, which reflects that the factors assessed in the parent narratives likely fell on a continuum rather than into purely discrete clusters.
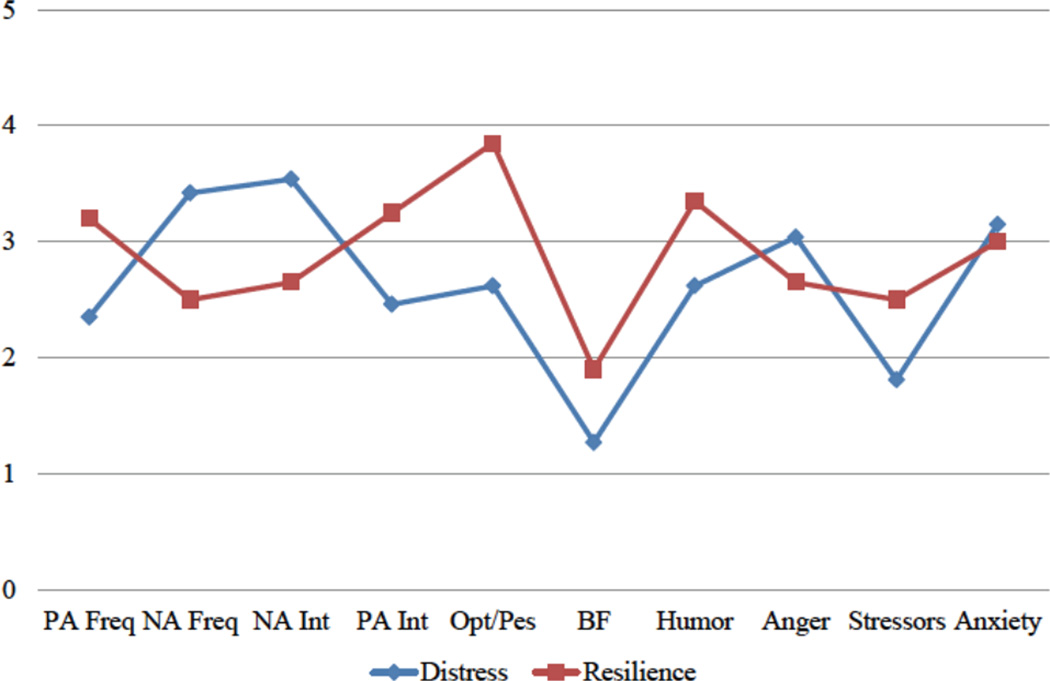
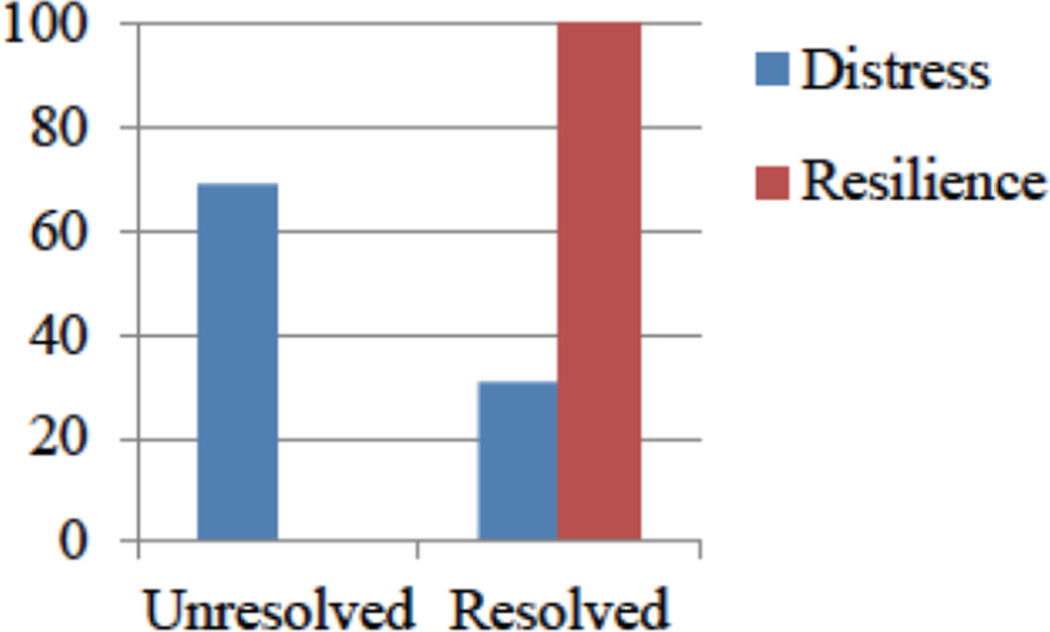
The narrative codes that were predictors of these profiles, from most to least contributory/meaningful, were: Diagnosis Orientation (Importance = 1.00); Positive Affect Frequency (Importance = .94); Negative Affect Frequency (Importance = .94); Negative Affect Intensity (Importance = .71); Positive Affect Intensity (Importance = .66); Pessimism/Optimism (Importance = .62); Benefit-Finding/Growth (Importance = .46); Humor/Laughter (Importance = .28); Anger (Importance = .13); PTEs total (Importance = .13); and Threat/Anxiety (Importance = .04). The distribution of the clusters was fairly even. The first cluster, labeled “Distress Narratives,” included 26 parents (56.5% of the sample). The second cluster, labeled “Resilience Narratives,” included 20 parents (43.5% of the sample). See Figures 1 and 2 for description and depiction of the pain narrative profiles.
Figure 1. Mean Narrative Codes across Parent Pain Narrative Profiles.
This figure depicts mean scores (plotted on the Y-axis) of each continuous narrative code (plotted on the X-axis). PA Freq: Positive Affect Frequency; NA Freq: Negative Affect Frequency; NA Int: Negative Affect Intensity; PA Int: Positive Affect Intensity; Opt/Pes: Optimism/Pessimism; BF: Benefit-Finding/Growth; Humor: Humor/Laughter; Stressors: Total Stressor Count; Anxiety: Threat/Anxiety.
Figure 2. Diagnosis Orientation Categorizations across Parent Pain Narrative Profiles.
This figure depicts the percentage of parents (Y-axis) categorized as being either unresolved or resolved regarding their child’s diagnosis (X-axis) across each narrative profile (Distress, Resilience). Distress narratives were told by parents who were exclusively unresolved regarding their child’s diagnosis of chronic pain whereas resilience narratives were predominantly told by parents categorized as resolved but also to a lesser extent by parents categorized as being unresolved about their child’s diagnosis.
Distress Narratives
Compared to the Resilience cluster, parents in the Distress cluster had narratives that were characterized by a higher frequency of unresolved diagnosis orientation (69.2% of this cluster; X2(1) = 22.75, p < .001), less frequent positive affect (t(44) = −5.26, p <.001), more frequent negative affect (t(44) = 5.26, p <.001), greater intensity of negative affect (t(44) = 4.32, p <.001), less intensity of positive affect (t(44) = −4.12, p <.001), more pessimism (t(44) = −3.94, p <.001), less benefit-finding (t(44) = −3.24, p <.01), and less humor/laughter (t(44) = −2.30, p <.05). Furthermore, while not significantly different, distress narratives had higher anxiety, more anger, and fewer stressors than the resilience narratives. Overall, these parent narratives were generally more negative in terms of affect and content, despite having fewer stressful life events overall.
Resilience Narratives
Compared to the Distress cluster, parents who fell in the Resilience cluster had narratives that were characterized by significantly higher frequency of resolved diagnosis orientation (100% of this cluster), more frequent positive affect, less frequent negative affect, lower intensity of negative affect, higher intensity of positive affect, more optimism, more benefit-finding, and more frequent use of humor/laughter (see above for specific statistics). There were not statistically significant differences between clusters on anger, stressors, and anxiety; however, resilience narratives had relatively less anger, a higher occurrence of stressful life events, and less anxiety. Resilience narratives generally demonstrated more positive affect and content, even though this group experienced more stressful life events on average.
Differences between clusters
T-tests (for continuous variables) and chi-square (for the categorical variable diagnosis orientation) analyses indicated that there were no significant differences in demographic variables between the Distress and Resilience narrative clusters. Table 1 includes details on demographics for each cluster.
Exploratory analysis of differences between clusters based on parents’ catastrophic thinking about child pain and adolescent pain-related functioning. We used independent samples t-tests to compare narrative clusters on parents’ tendency to catastrophize about their child’s pain (PCS-P), as this construct is a robust predictor parents’ negative emotional and behavioral responses to child pain1,5. As expected, parents in the Distress Narrative cluster reported significantly higher levels of helplessness than those in the Resilience Narrative cluster (MDistress = 17.77, SD = 5.38; MResilience = 14.55, SD = 4.75; t(44) = 2.15, p < .05). Clusters did not differ on the other PCS-P subscales (rumination, magnification, total). Results further indicated that there were no significant differences between the clusters on adolescent pain-related functioning.
Discussion
This is the first study to examine the pain narratives of parents of youth with chronic pain in a therapeutic context. In the first session of the psychological intervention, parents were asked to share their story of their child’s pain problem and the impact that it had on them and their families. Based on existing literature, a detailed coding system was developed to characterize vulnerability- and resilience-based aspects of the pain narratives. Results showed that parents’ pain narratives could be reliably coded using this system. We found that several aspects of narrative content and affect were expressed. Parents told varied and unique narratives, revealing a range of impact that their child’s pain experience had on them. Parents differed in the overall affective tone of the narrative, ranging from positive to negative. Although the overall number of potentially traumatic or stressful events was relatively low, a diverse range of events was endorsed including very serious, potentially traumatic events (e.g., suicide attempts and self-injurious behaviors, car accidents or other serious accidents, child abuse). Parents’ pain narratives also reflected resiliency. Indeed, some parents expressed optimism, humor, and even an ability to find benefit and growth in their journey through their child’s chronic pain experience.
Nearly 40% of parents were described as having an unresolved versus a resolved orientation towards their child’s diagnosis, meaning that they did not accept or “buy in” to the diagnosis, and/or that they were continuing to actively feel grief and/or anger about it. This distinction was critical in characterizing narrative profiles. Using exploratory cluster analysis, two styles of parents’ pain narratives were characterized that we labeled Distress Narratives and Resilience Narratives. Support for the preliminary validity of these clusters was found by relationships between Distress Narratives and higher levels of parental catastrophizing about child pain (helplessness) compared to Resilience Narratives. These two narrative profiles are also consistent with previous thematic classifications in literature on illness narratives (e.g., chaos versus restitution)14. Contrary to expectations, clusters did not differ based on children’s pain-related functioning. Future research employing larger samples is needed to examine relationships between narrative typologies and parent, child, and family functioning. In particular, inclusion of more resilience-based measures (as emphasized in a recent topical review on this topic37) will be important. A longitudinal perspective will provide particularly valuable information on how narrative typologies may predict changes in pain-related functioning over time.
Our findings offer a broad and rich perspective on parents’ experience of their child’s pain problem. Although well-researched constructs were incorporated into the coding scheme (pain catastrophizing), several new codes emerged as important in distinguishing between narrative profiles. Indeed, the most important codes for differentiating between clusters were those that have seldom been previously examined in pediatric chronic pain literature (e.g., diagnostic orientation, affective valence, optimism/pessimism, and benefit finding). Distress Narratives were characterized by more negative affect and frequent unresolved orientation towards the child’s diagnosis of chronic pain whereas Resilience Narratives were characterized by positive affect and an exclusively resolved orientation towards the child’s diagnosis. Based on these results, we argue that parental diagnostic orientation towards their child’s chronic pain should be examined in future research; indeed, interviews designed to specifically elicit narratives about diagnostic orientation, as has been done in other pediatric chronic illness literatures, may provide unique information.
Interestingly, resilience narratives included a greater number of potentially traumatic events than distress narratives. This is counter to what one might expect. While it is possible that life adversity may prepare families to deal with pediatric chronic pain, it could also be that parents who disclosed more traumatic events in the narrative had already effectively processed those events. Indeed, avoidance of discussing/processing traumatic events is likely linked to greater distress. Nevertheless, it is also likely that it is not necessarily the overall number of stressful events that predict distress but rather, it is the subjective impact of particular events on individuals that matter most. In other words, the impact of each single stressful event is not equivalent. Finally, therapists elicited a pain (as opposed to a trauma) narrative. Coding of traumatic events included only those events that were captured in the 15-minute narrative and were not intended to reflect all traumatic events that parents may have experienced in their lifetime.
In interpreting these findings, it is important to contextualize these pain narratives to time and place. All families had previously been evaluated in a multidisciplinary chronic pain clinic and had received feedback regarding their child’s diagnosis as well as education about chronic pain, and a tailored set of treatment recommendations. The fact that 40% of parents in this study were still conveying an unresolved orientation to their child’s diagnosis after having completed an evaluation in a specialty chronic pain clinic could have implications for the degree to which they can engage in treatment recommendations. If parents are still searching for answers or reassurance about their child’s pain diagnosis they may have lower readiness to make behavioral changes that are required for recovery. Future research should examine the extent to which pain narratives are predictive of treatment engagement and response to intervention. Given the current findings, assessment of parents’ orientation toward their child’s diagnosis of chronic pain is deserving of further research.
On the other hand, it is encouraging that a significant portion of the parents in this study (60%) were rated as being resolved with respect to their child’s diagnosis of chronic pain. The limited research on pain narratives of parents of youth with chronic pain involving mothers has emphasized the predominantly negative and burdensome experience of parenting10. Our findings paint a richer, more complex picture to include both benefit and burden. This is in line with recent qualitative research conducted with fathers of youth with chronic pain12. Optimism and benefit finding as resilience-based factors have been hypothesized to be protective leading to better coping with chronic pain13 and other pediatric chronic illnesses38. In addition to constructs such as parent acceptance and psychological flexibility, optimism and benefit finding warrant further consideration in pediatric pain research.
In the broader field of medicine, the role of illness narratives is appreciated as a powerful source of clinical information and integral to relationship building between patients and providers9. Narratives are dynamic and inherently unreliable as a result of being shaped by the interaction between narrator, listener, and context. This makes them difficult to empirically examine. For this study, the listeners were all PhD-level psychologists trained to use similar open-ended prompts and reflective responses, thereby largely precluding examination of the clinician side of the interaction. Nevertheless, each clinician’s tone and therapeutic style invariably influenced the parents’ comfort, style, and content of their pain narratives. This study did not examine the influence of pain narratives on therapist judgments or the role of therapist verbalizations on narrative construction. Future research should examine the reciprocal relationship between narrator and listener. Related to this, the role of therapist validation on pain narratives is unknown and may have important implications for treatment development39.
This study, in addition to the work of Jordan and colleagues10, 12 as well as Gaughan et al.11, offers novel insights into the incredibly complex experience of parenting a child with chronic pain. Indeed, many parents expressed aspects of both distress and resilience when describing their pain journeys. This growing area of research provides a richer account of the observable behaviors and affect that can be gleaned from parents’ language about their children’s pain problem. Unlike previous qualitative and observational research, this study emphasizes the importance of attending to and assessing the emotional context of narratives, parents’ orientation to their child’s diagnosis, and resilience-based aspects within the narratives. We argue that narratives are not only worth listening to; they should be listened to. Clinically, parents can be offered the opportunity to share their story of their child’s pain problem and importantly, the impact that the pain has had on them. This study assessed the first 15 minutes of the pain narrative to better approximate a realistic amount of time that clinicians would be able to devote to an interaction in the real world. In a relatively short amount of time, listening to a parent’s pain narrative can yield valuable clinical information that may not be revealed by checklists and questionnaires. Nevertheless, there are aspects of some parents’ narratives that were likely missed and that could have altered the categorizations presented herein.
In light of mounting research showing the powerful role of parent psychological functioning on children’s own functioning, it is becoming increasingly clear that parents’ own interpretations of the child’s pain experience should be understood and harnessed. The role of narratives as a primary target for intervention has been long recognized in the field of clinical psychology (e.g., narrative therapy40). Changing the pain narrative holds promise for changing the pain experience. Although these clinical implications are beyond the scope of the present study, this area is deserving of future research.
Despite several key strengths, this study was not without limitations. Parents’ pain narratives were shared in the first session of a research study examining the efficacy of parent psychological treatment to reduce distress. Narratives were told prior to receiving the treatment rationale and framework at one point in time. Therefore, it is unknown how the content and affect of the pain narrative might change over the course of treatment. Such evolution in meaning and experience has been previously described in qualitative research with fathers of youth with chronic pain12. Related to this, this study sample was primarily comprised of mothers; pain narratives of fathers might differ from those of mothers and warrant further consideration in research. In addition, given that narratives were told to psychologists in the context of a research study, it is possible that these narratives differ from the narratives that would be shared in interdisciplinary pain clinics. Study therapists were not providers connected with the child’s pain team, and parents were told that the information that they shared would be kept confidential. Furthermore, parents shared their narratives in the absence of their child; these narratives may be different than shared family pain narratives. Future research is needed to examine the co-construction of narratives. Some families likely have a shared family pain narrative that has been well rehearsed whereas other families may have very different recollections of the pain journey among individual family members. Given the potential importance of parents’ and children’s memories for painful experiences on subsequent pain and coping25, 41, 42, this is an intriguing area for future inquiry. Finally, given that parents chose to complete a psychological treatment, it is possible that their diagnostic orientation was skewed towards being resolved and there may be a larger proportion of parents in chronic pain clinics with an unresolved orientation. Nevertheless, it is also possible that parents who are resolved regarding their child’s diagnosis are less distressed and therefore do not perceive a need to complete an intervention designed to reduce parental distress.
The process of parents accepting the diagnosis of their child’s pain problem is likely just that, a process that unfolds and changes over time. Identifying resistant or unresolved families may offer insights into how to intervene differently (e.g., by using approaches that aim to increase their motivation and readiness to engage in behavior change). If parents do not “buy in” or accept their child’s diagnosis, our current interventions for pediatric chronic pain that promote functioning despite pain may not appear logical to parents and may in fact appear harmful. Importantly, conceptualization of pain is related to outcomes43. Listening for such resistance and conceptualizations during clinical encounters could have implications for how clinicians talk to families about diagnosis and treatment. However, it is also possible that diagnosis “resolution” may not be related to motivation for behavior change but may rather simply happen with the passage of time, with a different temporal course for different families. The longitudinal course of pain narratives is not known. Future work should examine pain narratives over the course of treatment as well as their role in treatment response. It could be that the telling of the pain story for some families is therapeutic in and of itself.
In conclusion, this study examined the pain narratives of parents of youth with chronic pain shared during the first session of a psychological intervention study. Adding to previous literature, findings reveal a richer, more varied account of the parenting experience that is characterized by benefit and burden. These findings emphasize the merit in eliciting and attending to parents’ stories of their journey of living with their child with chronic pain. We believe that the narrative typologies revealed in this study could offer important assessment information to clinicians about parents’ readiness to change and “buy-in” to treatment for chronic pain. It may also provide clinicians information about the particular aspects of the narrative that might be most helpful to listen and respond to (e.g., diagnostic orientation, affective tone). Future research is needed to examine the utility of this pain narrative classification in relationship to child, parent, and family functioning as well as in understanding response to intervention.
Supplementary Material
Acknowledgments
Disclosure of Funding: At the time that this research was conducted, Dr. Noel was funded by a Post-PhD Fellowship Award from the Canadian Institutes of Health Research. She was a trainee member of Pain in Child Health, a Strategic Training Initiative in Health Research of the Canadian Institutes of Health Research. Funding for this research was provided by Eunice Kennedy Shriver National Institute of Child Health and Human Development award to Dr. Palermo (1R21HD065180-02) and a Seattle Children’s Research Institute Center for Child Health, Behavior and Development Small Grant and Stimulus Fund awarded to Dr. Law.
References
- 1.Simons LE, Smith A, Kaczynski K, et al. Living in fear of your child's pain: the parent fear of pain questionnaire. Pain. 2015;156(4):694–702. doi: 10.1097/j.pain.0000000000000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith AM, Sieberg CB, Odell S, et al. Living Life with My Child's Pain: The Parent Pain Acceptance Questionnaire (PPAQ) Clin J Pain. 2014 doi: 10.1097/AJP.0000000000000140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCracken LM, Gauntlett-Gilbert J. Role of psychological flexibility in parents of adolescents with chronic pain: development of a measure and preliminary correlation analyses. Pain. 2011;152(4):780–785. doi: 10.1016/j.pain.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Wallace DP, McCracken LM, Weiss KE, et al. The role of parent psychological flexibility in relation to adolescent chronic pain: further instrument development. J Pain. 2015;16(3):235–246. doi: 10.1016/j.jpain.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Goubert L, Eccleston C, Vervoort T, et al. Parental catastrophizing about their child's pain. The parent version of the Pain Catastrophizing Scale (PCS-P): a preliminary validation. Pain. 2006;123(3):254–263. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 6.Van Slyke DA, Walker LS. Mothers' responses to children's pain. Clin J Pain. 2006;22(4):387–391. doi: 10.1097/01.ajp.0000205257.80044.01. [DOI] [PubMed] [Google Scholar]
- 7.Jordan A, Eccleston C, McCracken LM, et al. The Bath Adolescent Pain--Parental Impact Questionnaire (BAP-PIQ): development and preliminary psychometric evaluation of an instrument to assess the impact of parenting an adolescent with chronic pain. Pain. 2008;137(3):478–487. doi: 10.1016/j.pain.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Morris DB. Narrative and pain: Towards an integrative model. In: Moore RJ, editor. Handbook of Pain and Palliative Care: Biobehavioral Approaches for the Life Course. New York: Springer; 2013. pp. 733–751. [Google Scholar]
- 9.Charon R. Narrative medicine: honoring the stories of illness. New York: Oxford University Press; 2006. [Google Scholar]
- 10.Jordan AL, Eccleston C, Osborn M. Being a parent of the adolescent with complex chronic pain: an interpretative phenomenological analysis. Eur J Pain. 2007;11(1):49–56. doi: 10.1016/j.ejpain.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Gaughan V, Logan D, Sethna N, et al. Parents' Perspective of Their Journey Caring for a Child with Chronic Neuropathic Pain. Pain Manag Nurs. 2014;15(1):246–257. doi: 10.1016/j.pmn.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Jordan A, Crabtree A, Eccleston C. 'You have to be a jack of all trades': Fathers parenting their adolescent with chronic pain. J Health Psychol. 2015 doi: 10.1177/1359105315580461. [DOI] [PubMed] [Google Scholar]
- 13.Cousins LA, Cohen LL, Venable C. Risk and Resilience in Pediatric Chronic Pain: Exploring the Protective Role of Optimism. J Pediatr Psychol. 2014 doi: 10.1093/jpepsy/jsu094. [DOI] [PubMed] [Google Scholar]
- 14.Frank AW. The wounded storyteller: Body, illness, and ethics. Chicago: University of Chicago Press; 1995. [Google Scholar]
- 15.Goldberg DS. Job and the stigmatization of chronic pain. Perspect Biol Med. 2010;53(3):425–438. doi: 10.1353/pbm.0.0166. [DOI] [PubMed] [Google Scholar]
- 16.Markovic M, Manderson L, Warren N. Endurance and contest: women's narratives of endometriosis. Health (London) 2008;12(3):349–367. doi: 10.1177/1363459308090053. [DOI] [PubMed] [Google Scholar]
- 17.Palermo TM, Law EF, Essner B, et al. Adaptation of Problem-Solving Skills Training (PSST) for Parent Caregivers of Youth with Chronic Pain. Clinical practice in pediatric psychology. 2014;2(3):212–223. doi: 10.1037/cpp0000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.von Baeyer CL, Spagrud LJ, McCormick JC, et al. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children's self-reports of pain intensity. Pain. 2009;143(3):223–227. doi: 10.1016/j.pain.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Palermo TM, Valenzuela D, Stork PP. A randomized trial of electronic versus paper pain diaries in children: impact on compliance, accuracy, and acceptability. Pain. 2004;107(3):213–219. doi: 10.1016/j.pain.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Eccleston C, Jordan A, McCracken LM, et al. The Bath Adolescent Pain Questionnaire (BAPQ): development and preliminary psychometric evaluation of an instrument to assess the impact of chronic pain on adolescents. Pain. 2005;118(1–2):263–270. doi: 10.1016/j.pain.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 21.Chorney JM, McMurtry CM, Chambers CT, et al. Developing and modifying behavioral coding schemes in pediatric psychology: a practical guide. J Pediatr Psychol. 2015;40(1):154–164. doi: 10.1093/jpepsy/jsu099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaugars AS, Zebracki K, Kichler JC, et al. Use of the Family Interaction Macro-coding System with families of adolescents: psychometric properties among pediatric and healthy populations. J Pediatr Psychol. 2011;36(5):539–551. doi: 10.1093/jpepsy/jsq106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray CB, Amaro CM, Devine KAP. Observed macro- and micro-level parenting behaviors during preadolescent family interactions as predictors of adjustment in emerging adults with and without spina bifida. J Pediatr Psychol. 2015;40(1):18–32. doi: 10.1093/jpepsy/jsu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palermo TM, Eccleston C. Parents of children and adolescents with chronic pain. Pain. 2009;146(1–2):15–17. doi: 10.1016/j.pain.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noel M, Chambers CT, Petter M, et al. Pain is not over when the needle ends: a review and preliminary model of acute pain memory development in childhood. Pain Manag. 2012;2(5):487–497. doi: 10.2217/pmt.12.41. [DOI] [PubMed] [Google Scholar]
- 26.Holmbeck GN, Zebracki K, Johnson SZ, et al. Parent-child interaction macro-coding manual. 2007 [Google Scholar]
- 27.Margolin G, Oliver PH, Gordis EB, et al. The nuts and bolts of behavioral observation of marital and family interaction. Clin Child Fam Psychol Rev. 1998;1(4):195–213. doi: 10.1023/a:1022608117322. [DOI] [PubMed] [Google Scholar]
- 28.Holmbeck GN. Expressed emotion coding handbook. 2002 [Google Scholar]
- 29.Barlow D. Anxiety and its disorders: the nature and treatment of anxiety and panic (second edition) New York: Guilford Press; 2002. [Google Scholar]
- 30.Phipps S, Long AM, Ogden J. Benefit Finding Scale for Children: preliminary findings from a childhood cancer population. J Pediatr Psychol. 2007;32(10):1264–1271. doi: 10.1093/jpepsy/jsl052. [DOI] [PubMed] [Google Scholar]
- 31.Tran V, Wiebe DJ, Fortenberry KT, et al. Benefit finding, affective reactions to diabetes stress, and diabetes management among early adolescents. Health Psychol. 2011;30(2):212–219. doi: 10.1037/a0022378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pianta RC, Marvin RS, Britner PA, et al. Mothers' resolution of their children's diagnosis: organized patterns of caregiving representations. Infant Mental Health Journal. 1996;17(3):239–256. [Google Scholar]
- 33.Popp JM, Robinson JL, Britner PA, et al. Parent adaptation and family functioning in relation to narratives of children with chronic illness. J Pediatr Nurs. 2014;29(1):58–64. doi: 10.1016/j.pedn.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Phipps S, Klosky JL, Long A, et al. Postpe stress and psychological growth in children with cancer: has the traumatic impact of cancer been overestimated? J Clin Oncol. 2014;32(7):641–646. doi: 10.1200/JCO.2013.49.8212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Currier JM, Jobe-Shields LE, Phipps S. Stressful life events and posttraumatic stress symptoms in children with cancer. J Trauma Stress. 2009;22(1):28–35. doi: 10.1002/jts.20382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berk RA. Generalizability of behavioral observations: a clarification of interobserver agreement and interobserver reliability. Am J Ment Defic. 1979;83(5):460–472. [PubMed] [Google Scholar]
- 37.Cousins LA, Kalapurakkel S, Cohen LL, et al. Topical review: Resilience resources and mechanisms in pediatric chronic pain. J Pediatr Psychol. 2015;40(9):840–845. doi: 10.1093/jpepsy/jsv037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lindwall JJ, Russell K, Huang Q, et al. Adjustment in parents of children undergoing stem cell transplantation. Biol Blood Marrow Transplant. 2014;20(4):543–548. doi: 10.1016/j.bbmt.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain. 2015;156(2):215–219. doi: 10.1097/01.j.pain.0000460301.18207.c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.White M, Epson D. Narrative means to therapeutic ends. New York: Norton; 1990. [Google Scholar]
- 41.Noel M, Chambers CT, McGrath PJ, et al. The influence of children's pain memories on subsequent pain experience. Pain. 2012;153(8):1563–1572. doi: 10.1016/j.pain.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 42.Noel M, Rabbitts JA, Tai GG, et al. Remembering pain after surgery: a longitudinal examination of the role of pain catastrophizing in children's and parents' recall. Pain. 2015;156(5):800–808. doi: 10.1097/j.pain.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gallagher L, McAuley J, Moseley GL. A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. Clin J Pain. 2013;29(1):20–25. doi: 10.1097/AJP.0b013e3182465cf7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.