Abstract
Introduction
Acromegaly is a rare disease with a large burden due its associated comorbidities and the life-long management required. Since the occurrence and severity of associated complications are related to length of exposure to the excess growth hormone seen in acromegaly, early diagnosis is imperative. The delay in diagnosis, however, can be long, and may be the result of a lack of disease awareness and screening programs. Since acromegaly is an uncommon disease, finding ways to increase recognition and diagnosis that would permit early detection in a logical and cost-effective manner could be a challenge.
Methods
We conducted a retrospective literature review for information relating to the screening and diagnosis of acromegaly using PubMed. The aim was to assess whether an acromegaly-screening program in Latin America (and elsewhere) would be both of use and be feasible.
Findings and conclusions
An earlier diagnosis allows earlier initiation of treatment, such as surgery and/or drugs, which leads to more successful disease management (biochemical control) and better outcomes. Since the delay in diagnosis can be long, we believe that clear opportunities exist for earlier (and increased) detection of acromegaly. This can be achieved by increasing disease awareness for earlier recognition of symptoms and by using targeted screening (rather than mass screening) programs.
Keywords: Acromegaly diagnosis, Acromegaly screening program, Latin America
Introduction
Acromegaly is a rare disease commonly caused by a pituitary adenoma, which overproduces growth hormone (GH) in a pulsatile manner, resulting in increased secretion of insulin-like growth factor 1 (IGF-1) [1–3]. It has an estimated prevalence of 40–70 per million in the general population [4, 5]. This, however, may be an underestimation with some reports of more than 100 cases per million [6]. Despite being a rare disease, the burden of acromegaly is largely due to its associated comorbidities and the life-long management required [4]. Untreated acromegaly is associated with increased morbidity and mortality [7], and the occurrence and severity of linked complications is related to the length of exposure to excess GH [8]. Furthermore, the duration of symptoms is directly associated with mortality due to the disease [9], which is significantly higher than the general population [10]. Unfortunately, there can be a very long delay between the appearance of initial symptoms and the diagnosis of acromegaly [9], and thus its prevalence may be underestimated. Delayed diagnosis is associated with poor quality of life and worse outcomes due to the more severe complications and harder-to-treat advanced disease at the time of diagnosis [11, 12]. As such, early diagnosis and treatment is of the utmost importance. An earlier diagnosis would allow for earlier initiation of appropriate treatment, which in turn would lead to more successful disease management and ultimately better outcomes. As there are clear unmet needs around the recognition and diagnosis of acromegaly, there are obvious opportunities for earlier and increased detection. However, since acromegaly is uncommon, it may be challenging to set strategies that will aid in the diagnosis and early detection in a realistic and cost-effective manner.
The rationale for screening for acromegaly
Diagnosis of acromegaly is based primarily on clinical manifestations and usually confirmed by measuring GH levels, although this can be tricky due to the pulsatile nature of GH production. IGF-1, on the other hand, is more stable throughout the day and has a good correlation to GH level [13]. The clinical manifestations depend on the levels of GH (and IGF-1), age, tumour size, and the delay in diagnosis. Since many of the symptoms of acromegaly are non-specific and similar to other more common diseases, diagnosis is often missed or delayed by 5–10 years from the onset of symptoms [7]. This delay is also partly due to the fact that the clinical effects of excess GH occur insidiously over time. This provides a major opportunity for earlier detection, although some centres have begun showing an earlier diagnosis due to incidental findings [31]. Treatment for acromegaly is effective, and biochemical control can restore life expectancy to normal, improve symptoms, and improve/reverse comorbidities, and can therefore drastically improve the quality of life of patients [14]. However, if the complications are long-standing, biochemical control does not always result in reversal [8]. Since the severity of complications increases with longer duration of untreated disease, and long-term complications may be harder to address through biochemical control, getting an early diagnosis and treatment is key to improving patient quality of life and long-term outcomes.
Patients typically visit a number of healthcare providers prior to diagnosis. The first manifestations and reasons for a medical visit, in most cases, are physiognomic alterations and growth of the acral parts [11, 15]. These are not common in patients without acromegaly, and can be evaluated using simple observations, such as a change in shoe and/or ring size [16]. Surprisingly, the features present at clinical diagnosis have not changed between 1981 and 2006, and so it is clear that acromegaly remains under diagnosed and under recognized [11]. Therefore, familiarization of physicians and nurses (and the general public) with these phenotypes may be one step towards increasing early detection and diagnosis. Increasing awareness of these typical early features may help to identify patients at risk, rather than addressing comorbidities, which usually appear later, are not always present, and are rarely seen in the absence of these phenotypes. Establishing screening programs for these at risk patients could make headway in diagnosing these patients earlier. It is important to note that patients present with many different types of comorbidities, including cardiovascular disease, diabetes, hypertension, sleep apnea, carpal tunnel syndrome, and goitre [17], meaning increased awareness across broad spectrum of specialties is required.
General principles for a successful screening program in acromegaly
In general, screening programs are used in a population to identify an unrecognized disease in individuals without signs or symptoms, and are designed to identify this disease earlier. When implementing a screening program, a number of key criteria need to be met for it to be worthwhile and effective. These key criteria are as follows: (1) the condition should be an important health problem; (2) there should be a treatment available for the condition; (3) facilities that allow diagnosis and treatment should be available; (4) there should be a “latent” stage of the disease; (5) there should be a test or examination currently available for the condition; (6) the test should be acceptable to the population; (7) the natural history of the disease should be adequately understood; (8) there should be an agreed policy on whom to treat; (9) the total cost of finding a case should be economically balanced in relation to medical expenditure as a whole; (10) screening should be a continuous process, and not a ‘once for all’ project [18].
There are two main types of screening for disease: mass screening and targeted screening [19]. The difference is that mass screening is offered to all, irrespective of risk, and targeted screening is offered only to those known to be at increased risk. Many screening programs exist in other disease areas with varying levels of success e.g., breast cancer [20, 21], colorectal cancer [22, 23], prostate cancer [24, 25], and cervical cancer [26]. In the context of a rare disease such as acromegaly, mass screening would be costly and unfeasible, whereas targeted screening may be more acceptable, especially when considering the cumulative costs of treating the increasing comorbidities associated with diagnosis delay. In order to implement this kind of program, (1) there needs to be a clear definition of which groups are at high risk, and (2) an increased awareness of this association among medical professionals (and the general public).
There are limitations of screening that would need to be considered for any program to be successful. These include the possibility of false positive or negative results, and potentially overdiagnosis [18]. There is also the risk of lead time and length time bias; lead time bias occurs when a test diagnoses the disease earlier, but there is no effect on the outcome of the disease, length time bias is when, for example, screening tends to detect slow-growing tumours that would not have caused death at all, or before other causes [18, 27]. The best way to overcome these limitations is to use a randomized controlled trial, which can be expensive and take time, but would provide the best information for evidence-based medicine. The aim of an acromegaly screening program would be to maximize the number of cases detected, while minimizing the number of people referred unnecessarily for further tests. Any screening program proposed would need to be introduced in a way that allows its quality to be measured and continuously improved. A possible starting point would be a pilot study in a chosen country before extending the program to other Latin American countries.
Some of the potential obstacles to implementing a new screening program in acromegaly are that physicians may require training and convincing to adopt new screening behaviors in their busy practice; many are not aware of the insidious nature of acromegaly or believe it is a serious, and irreversible disorder. Overcoming preconceptions about acromegaly could be a challenge, especially since many medical schools do not put a lot of focus on uncommon diseases. In addition support from health authorities and professional associations who currently do not push for screening would have to be gained. Funding, as with any screening program, would also be an important factor. Experience has shown that no screening test is perfect, and in order to implement a successful screening program in acromegaly, a number of key components should be considered. Exactly how these could be implemented is discussed below.
Blueprint for a screening program for acromegaly in Latin America
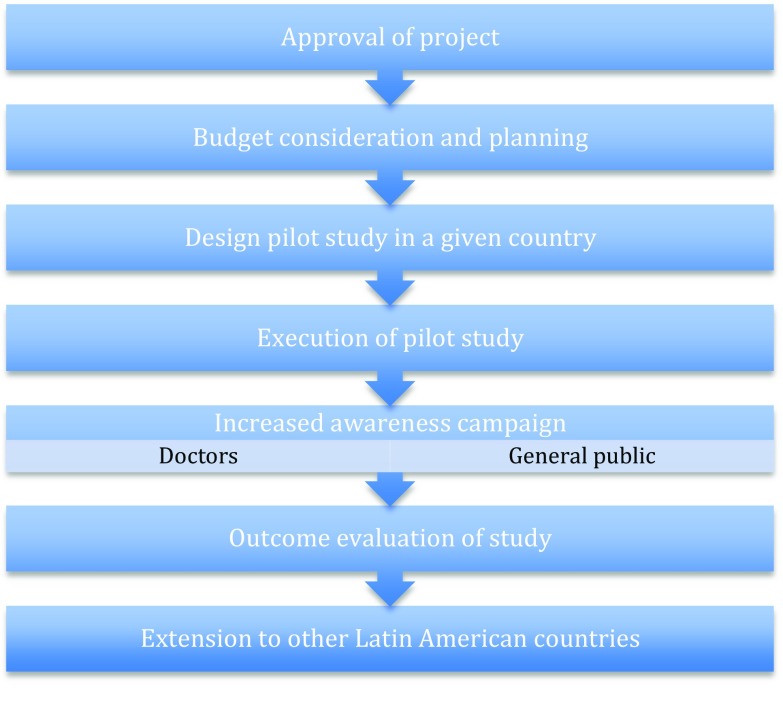
The successful implementation of a screening program for acromegaly in Latin America involves a number of key components (Fig. 1). First, there should be a plan to increase awareness of the early signs suggestive of acromegaly; this is important for doctors involved in primary care and other relevant specialties (cardiologists, diabetologists, dermatologists, rheumatologists, pulmonologists, gynecologists, odontologists, pediatricians). Second, doctors or physicians should be educated to look for acral changes in patients with sleep apnea, diabetes, insulin resistance, carpal tunnel syndrome, cardiac hypertrophy, and other common comorbidities. This education could occur via traditional courses, teleconferences, printed materials, and digital media. There should also be increased awareness of the early features of acromegaly among the general population. This would help patients ask the right questions, which in turn would help their physicians in an earlier diagnosis. The campaign should focus on simple key features such as increasing shoe and ring size, and this could occur via TV and/or radio interviews, articles in newspapers/magazines and web-based media. There may be an important role here for communications specialists, such as the Sociedad Argentina de Periodismo Médico (Argentina Society of Medical Journalism).
Fig. 1.
Key steps in the development of an acromegaly screening program in Latin America
The first practical steps in implementing the screening part of the program should include: the design of a simple detection program based on offering free IGF-1 measurements for patients with warning signs, and undertaking a pilot study (either single- or multi-center) of limited duration in a given country before extending the program to other Latin American countries with the support of pharmaceutical companies. There are a number of tools available that could help physicians with the screening process, for example a simple questionnaire evaluating the enlargement of extremities in adult patients seen at primary health care units [28]. Recently more novel approaches for early identification have been proposed; a study comparing diagnostic accuracy between physicians and a computer model showed that accuracy in the computer model was 86 %, whereas that of the physicians was only 26 % [29]. Similar results were seen in a recent study by Schneider et al. [30] where computer analysis again was more accurate than physicians. This type of model could aid in the early diagnosis in the proposed screening program.
Conclusions
Acromegaly is a rare disease with a large burden resulting from a lack of awareness, delayed diagnosis, and increasing comorbidities with time. A screening program for acromegaly would provide opportunities for earlier diagnosis and treatment. The most efficient strategy for detecting and diagnosing acromegaly would take the form of a targeted screening program (rather than mass screening). The two key components of this screening program would be (1) increasing awareness (among the public and doctors) of groups at risk, and (2) implementing a process of referral for further testing in those patients deemed to be at high risk. This type of targeted screening program appears to be feasible in Latin America and elsewhere. The program would first need to be evaluated for logistics and cost-effectiveness in a pilot study within a selected country, before extension to other Latin American countries. The earlier diagnosis and treatment that could be provided by the success of this type of screening program, could lead to improved outcomes and hopefully cost savings in the long-term due to fewer and less severe complications that tend to manifest over time in delayed diagnosis.
Acknowledgments
The Latin American Knowledge Network Initiative, including meetings and preparation of this supplement, was organized and funded by Ipsen. Medical writing support was provided by Dr. Catriona Paul on behalf of Arsenal-CDM Paris and funded by Ipsen. The authors were fully responsible for the concept and all content, were involved at all stages of manuscript development, and provided approval of the final version for submission.
References
- 1.Adelman DT, Liebert KJ, Nachtigall LB, Lamerson M, Bakker B. Acromegaly: the disease, its impact on patients, and managing the burden of long-term treatment. Int J Gen Med. 2013;6:31–38. doi: 10.2147/IJGM.S38594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melmed S. Acromegaly pathogenesis and treatment. J Clin Invest. 2009;119(11):3189–3202. doi: 10.1172/JCI39375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schneider HJ, Sievers C, Saller B, Wittchen HU, Stalla GK. High prevalence of biochemical acromegaly in primary care patients with elevated IGF-1 levels. Clin Endocrinol (Oxf) 2008;69(3):432–435. doi: 10.1111/j.1365-2265.2008.03221.x. [DOI] [PubMed] [Google Scholar]
- 4.Ben-Shlomo A, Sheppard MC, Stephens JM, Pulgar S, Melmed S. Clinical, quality of life, and economic value of acromegaly disease control. Pituitary. 2011;14(3):284–294. doi: 10.1007/s11102-011-0310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chanson P, Salenave S. Acromegaly. Orphanet J Rare Dis. 2008;3:17. doi: 10.1186/1750-1172-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chanson P, Salenave S, Kamenicky P, Cazabat L, Young J. Pituitary tumours: acromegaly. Best Pract Res Clin Endocrinol Metab. 2009;23(5):555–574. doi: 10.1016/j.beem.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Holdaway IM, Rajasoorya RC, Gamble GD. Factors influencing mortality in acromegaly. J Clin Endocrinol Metab. 2004;89(2):667–674. doi: 10.1210/jc.2003-031199. [DOI] [PubMed] [Google Scholar]
- 8.Colao A, Ferone D, Marzullo P, Lombardi G. Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev. 2004;25(1):102–152. doi: 10.1210/er.2002-0022. [DOI] [PubMed] [Google Scholar]
- 9.Rajasoorya C, Holdaway IM, Wrightson P, Scott DJ, Ibbertson HK. Determinants of clinical outcome and survival in acromegaly. Clin Endocrinol (Oxf) 1994;41(1):95–102. doi: 10.1111/j.1365-2265.1994.tb03789.x. [DOI] [PubMed] [Google Scholar]
- 10.Dekkers OM, Biermasz NR, Pereira AM, Romijn JA, Vandenbroucke JP. Mortality in acromegaly: a metaanalysis. J Clin Endocrinol Metab. 2008;93(1):61–67. doi: 10.1210/jc.2007-1191. [DOI] [PubMed] [Google Scholar]
- 11.Reid TJ, Post KD, Bruce JN, Nabi Kanibir M, Reyes-Vidal CM, Freda PU. Features at diagnosis of 324 patients with acromegaly did not change from 1981 to 2006: acromegaly remains under-recognized and under-diagnosed. Clin Endocrinol (Oxf) 2010;72(2):203–208. doi: 10.1111/j.1365-2265.2009.03626.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siegel S, Streetz-van der Werf C, Schott JS, Nolte K, Karges W, Kreitschmann-Andermahr I. Diagnostic delay is associated with psychosocial impairment in acromegaly. Pituitary. 2013;16(4):507–514. doi: 10.1007/s11102-012-0447-z. [DOI] [PubMed] [Google Scholar]
- 13.Barkan AL, Beitins IZ, Kelch RP. Plasma insulin-like growth factor-I/somatomedin-C in acromegaly: correlation with the degree of growth hormone hypersecretion. J Clin Endocrinol Metab. 1988;67(1):69–73. doi: 10.1210/jcem-67-1-69. [DOI] [PubMed] [Google Scholar]
- 14.Colao A, Auriemma RS, Pivonello R, Galdiero M, Lombardi G. Medical consequences of acromegaly: what are the effects of biochemical control? Rev Endocr Metab Disord. 2008;9(1):21–31. doi: 10.1007/s11154-007-9062-0. [DOI] [PubMed] [Google Scholar]
- 15.Ezzat S, Forster MJ, Berchtold P, Redelmeier DA, Boerlin V, Harris AG. Acromegaly. Clinical and biochemical features in 500 patients. Medicine (Baltim) 1994;73(5):233–240. doi: 10.1097/00005792-199409000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Melmed S. Medical progress: acromegaly. N Engl J Med. 2006;355(24):2558–2573. doi: 10.1056/NEJMra062453. [DOI] [PubMed] [Google Scholar]
- 17.Mestron A, Webb SM, Astorga R, Benito P, Catala M, Gaztambide S, Gomez JM, Halperin I, Lucas-Morante T, Moreno B, Obiols G, de Pablos P, Paramo C, Pico A, Torres E, Varela C, Vazquez JA, Zamora J, Albareda M, Gilabert M. Epidemiology, clinical characteristics, outcome, morbidity and mortality in acromegaly based on the Spanish Acromegaly Registry (Registro Espanol de Acromegalia, REA) Eur J Endocrinol. 2004;151(4):439–446. doi: 10.1530/eje.0.1510439. [DOI] [PubMed] [Google Scholar]
- 18.Raffe AE, Gray M. Screening: evidence and practice. Oxford: Oxford University Press; 2007. [Google Scholar]
- 19.Wilson JM, Jungner YG. Principles and practice of mass screening for disease. Bol Oficina Sanit Panam. 1968;65(4):281–393. [PubMed] [Google Scholar]
- 20.Colbert JA, Adler JN. Clinical decisions. Mammography screening–polling results. N Engl J Med. 2013;368(9):e12. doi: 10.1056/NEJMclde1301407. [DOI] [PubMed] [Google Scholar]
- 21.Kalager M, Adami HO, Bretthauer M, Tamimi RM. Overdiagnosis of invasive breast cancer due to mammography screening: results from the Norwegian screening program. Ann Intern Med. 2012;156(7):491–499. doi: 10.7326/0003-4819-156-7-201204030-00005. [DOI] [PubMed] [Google Scholar]
- 22.Shaukat A, Church TR. Colorectal-cancer incidence and mortality after screening. N Engl J Med. 2013;369(24):2355. doi: 10.1056/NEJMc1313116. [DOI] [PubMed] [Google Scholar]
- 23.Shaukat A, Mongin SJ, Geisser MS, Lederle FA, Bond JH, Mandel JS, Church TR. Long-term mortality after screening for colorectal cancer. N Engl J Med. 2013;369(12):1106–1114. doi: 10.1056/NEJMoa1300720. [DOI] [PubMed] [Google Scholar]
- 24.Esserman L, Shieh Y, Thompson I. Rethinking screening for breast cancer and prostate cancer. JAMA. 2009;302(15):1685–1692. doi: 10.1001/jama.2009.1498. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman RM. Clinical practice. Screening for prostate cancer. N Engl J Med. 2011;365(21):2013–2019. doi: 10.1056/NEJMcp1103642. [DOI] [PubMed] [Google Scholar]
- 26.Eddy DM. Screening for cervical cancer. Ann Intern Med. 1990;113(3):214–226. doi: 10.7326/0003-4819-113-3-214. [DOI] [PubMed] [Google Scholar]
- 27.Petrie A, Sabin C. Medical statistics at a glance. Hoboken: Blackwell Science; 2000. [Google Scholar]
- 28.Rosario PW, Calsolari MR. Screening for acromegaly by application of a simple questionnaire evaluating the enlargement of extremities in adult patients seen at primary health care units. Pituitary. 2012;15(2):179–183. doi: 10.1007/s11102-011-0302-7. [DOI] [PubMed] [Google Scholar]
- 29.Miller RE, Learned-Miller EG, Trainer P, Paisley A, Blanz V. Early diagnosis of acromegaly: computers vs clinicians. Clin Endocrinol (Oxf) 2011;75(2):226–231. doi: 10.1111/j.1365-2265.2011.04020.x. [DOI] [PubMed] [Google Scholar]
- 30.Schneider HJ, Kosilek RP, Gunther M, Roemmler J, Stalla GK, Sievers C, Reincke M, Schopohl J, Wurtz RP. A novel approach to the detection of acromegaly: accuracy of diagnosis by automatic face classification. J Clin Endocrinol Metab. 2011;96(7):2074–2080. doi: 10.1210/jc.2011-0237. [DOI] [PubMed] [Google Scholar]
- 31.Nachtigall L, Delgado A, Swearingen B, Lee H, Zerikly R, Klibanski A. Changing patterns in diagnosis and therapy of acromegaly over two decades. J Clin Endocrinol Metab. 2008;93(6):2035–2041. doi: 10.1210/jc.2007-2149. [DOI] [PubMed] [Google Scholar]