Abstract
Little is known about the style and quality of feeding and care provided in child day-care centres in slum areas. This study purposively sampled five day-care centres in Nairobi, Kenya, where anthropometric measurements were collected among 33 children aged 6–24 months. Mealtime interactions were further observed in 11 children from four centres, using a standardized data collection sheet. We recorded the child actions, such as mood, interest in food, distraction level, as well as caregiver actions, such as encouragement to eat, level of distraction and presence of neutral actions. Of the 33 children assessed, with a mean age of 15.9 ± 4.9 months, 14 (42%) were female. Undernutrition was found in 13 (39%) children with at least one Z score <−2 or oedema (2): height for age <−2 (11), weight for age <−2 (11), body mass index for age <−2 (4). Rates of undernutrition were highest (9 of 13; 69%) in children aged 18–24 months. Hand-washing before the meal was lacking in all centres. Caregivers were often distracted and rarely encouraged children to feed, with most children eating less than half of their served meal. Poor hygiene coupled with non-responsive care practices observed in the centres is a threat to child health, growth and development.
Keywords: early years, responsive feeding, hygiene practices, severe undernutrition, nursery, Kenya
INTRODUCTION
The quality of care provided to infants and young children is an important determinant of growth and development. To promote optimal growth, child care practices should be provided in a responsive manner, taking into account the child’s characteristics, needs and developmental level [1–4]. Caregivers should not only be able to allocate adequate time and resources to child care, but also interpret and respond to a child’s needs in an accurate timely manner [3, 5]. Responsive feeding behaviours such as persistence, physical help and verbalization during feeding enhance the level of caregiver and child interaction and the feeding experience and are associated with adequate dietary intake [2–5].
Over the years, research on infant feeding has shifted from food security and dietary diversity to the effect of feeding behaviour and stimulation on nutrition status [6]. It is now evident that successful infant and young child feeding not only depends on what the child is fed, but also the quality of interaction between the caregiver and child. Responsive feeding styles have been linked to fewer food refusals and good nutrition status [7–11]. Although informative, most of these studies are carried out in Asian countries. Little is known about child care practices in African countries.
In Kenya, despite a decreasing trend of the prevalence of undernutrition nationwide [12, 13], stunting levels still remain high, especially in urban slum areas [14, 15]. The steady growth in urban women joining the paid labour force has led to an increase in the number of day-care centres, as women seek alternative child care services [16–18]. Little is known about the quality of care provided in these day-care centres in urban slums and its impact on nutrition status.
Aims
This pilot study aimed to assess the nutritional status of the children enrolled in day-care centres in urban slums in Nairobi, Kenya, and describes child feeding and hygiene practices in these centres.
METHODOLOGY
Setting and study design
This pilot study was an exploratory cross-sectional survey in five day-care centres located in two urban slums in Nairobi: Mukuru kwa Njenga and Mukuru kwa Reuben. These slums have a combined population of around 1.5 million and are characterized by crowded semi-permanent housing, open sewage systems and poor access to water and sanitation facilities. The study targeted children aged 6–24 months in day-care centres and was conducted over a 6 week period (mid-June to July 2014).
Research approval
Ethical approval was granted by the University of Glasgow college ethics committee, UK and University of Nairobi/Kenyatta National Hospital ethics review committee. The study was approved by the National Council for Science, Technology and Innovation as well as the Nairobi county health office. Written consent was obtained from the day-care centre management and from one parent or guardian of the selected children.
Research procedures
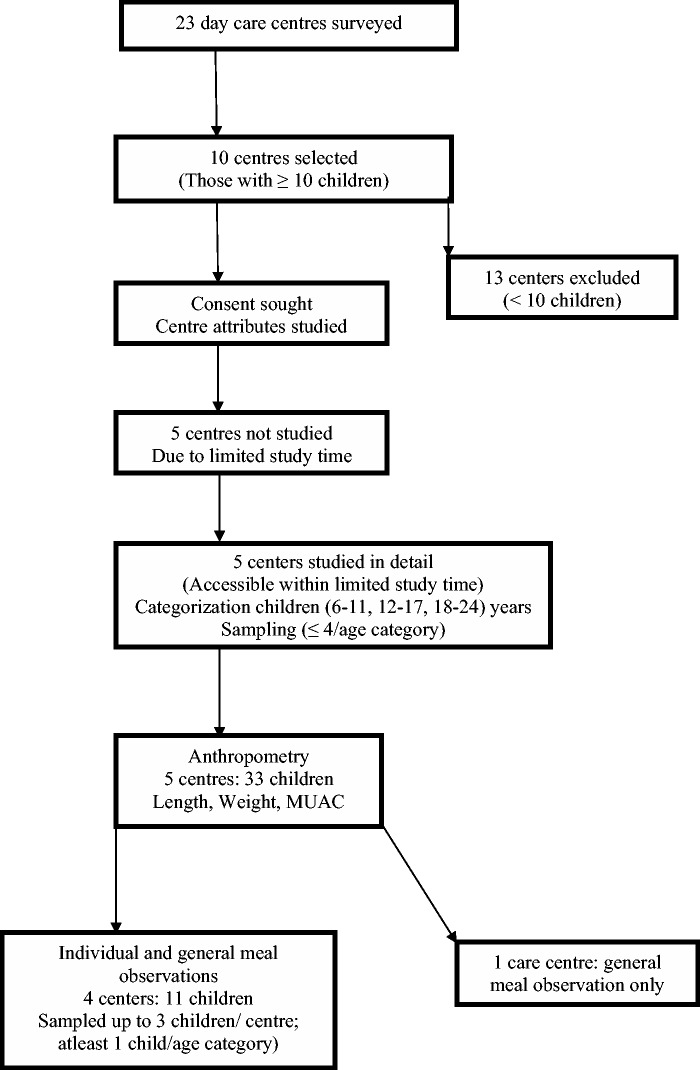
Initially, a survey of existing care centres both private and state owned was carried out in four slums, Mukuru kwa Reuben, Mukuru kwa Njenga, Mathare and Korogocho. From a list of 23 care centres that were identified, 10 of them with >10 enrolled children were selected for general surveying (Fig. 1). Information on centre characteristics such as ownership, construction, water supply, toilet facilities and child–caregiver ratio was collected in all 10 centres. Lunchtime meal and hygiene practices inclusive of hand-washing were observed in only five day-care centres in Mukuru kwa Njenga and Mukuru kwa Reuben, as these were conveniently located. Because the parents brought their children to the centres before dawn, information regarding consent was passed on to them through the caregivers. Signed consent forms were obtained from parents by caregivers and later handed to the researchers. This form also asked for each child’s age. Where this was not completed, as was the case in five children, the care staff reported an approximate age. Children were categorized into three age groups, 6–11, 12–17 and 18–24 months, and we aimed to take anthropometric measurements of up to four children in each age group for easy comparison. Where there were less than four children with consent per age group, all children in that group were studied. If this number was more, four children were selected at random by drawing lots.
Fig. 1.
Study flow chart.
Anthropometry
Weight, height and mid upper arm circumference (MUAC) measurements were taken by two researchers. Supine length was measured using the Rollametre measure mat (Raven Equipment Ltd Dunmow, U.K). The subject had to lie on this mat placed on a flat firm surface with all bulk clothes removed, head moved to Frankfort plane position and legs held down with gentle pressure. Three measurements were taken, and the mean of the closest two was then recorded. Weight was measured using an electronic balance (SECA 385 digital weighing scale III) with the child either nude or in a clean dry diaper. MUAC was measured using MUAC tapes (The United Nations Children's Fund). The tape was placed on the left arm at the midpoint between elbow and shoulder, and the circumference was measured to nearest 0.1 cm [19, 20]. A caregiver had to be present during the process of taking each child’s measurements.
Meal observations
Lunchtime meal observations were made for up to three children per centre, one from each age category, using a structured observation guide. This tool was designed using information from similar instruments [6, 21, 22] for a related pilot study that aimed at assessing child care practices in homes within urban Kenyan slums and peri-urban Lahore, Pakistan. The three children per centre were randomly selected by drawing lots. In the fifth centre, a general meal observation was made but not of individual children.
The two researchers (I.M. and A.M.) positioned themselves in a non-intrusive location, made observations and filled out the observation guide during the meal. Data on care centre structure, attendance, caregiver to child ratio, hygiene practices such as hand-washing, meal duration, food served and its consistency and mode of feeding were collected. Some of the data not included herein—care centre structure, sanitation and food consistency—will be reported in the results following the main study. We also observed the child actions such as interest in food, mood and distraction level, as well as the caregiver actions such as encouragement to eat, level of distraction and the presence of neutral actions, e.g. silence during meals, or flat verbalizations, e.g. ‘eat your food'. These actions were observed at the start, 5 min into and at the end of the meal.
Data analysis
For analysis of the anthropometric data, WHO Anthro 2011 (v 3.2.2) software [23] was used to convert the measures into Z scores and identify children with underweight, stunting and wasting using the World Health Organization (WHO) cut-off points. Stunting was defined as a HAZ (height for age Z score) of <−2. Wasting was defined as a WHZ (weight for height Z score) of <−2. Underweight was defined a WAZ (weight for age Z score) of <−2. Qualitative data from child meal observations were coded before respective frequencies were determined. The complete data set was analysed using SPSS software (v 16.0).
RESULTS
Five privately owned day-care centres each consisting of a single room were studied. The care centres were semi-permanent structures with iron sheet walls and cemented floors and were poorly ventilated. Each of the five centres had a pit latrine, which was shared by other households. Water was purchased from a public tap and was stored in jerry cans. Attendance in these centres ranged from 10 to 30 children. On average, one caregiver attended 10 children.
Child characteristics and nutrition status
The study included 33 children with a mean age of 15.9 ± 4.9 months of which 14 (42%) were female. Nine children were in the 6–11 months age category, 11 in the 12–17 months and 13 in the 18–24 months category. An average of six children per centre were selected for anthropometry.
Undernutrition (acute and chronic malnutrition) was relatively common, as 13 of 33 (39%) children had at least one Z score <−2 or oedema. A third of the children (11 of 33) were stunted, a third (11 of 33) underweight and 4 of 33 (12%) wasted (Table 1). Bilateral pitting oedema was observed in two children aged between 18 and 24 months. This age group also had the highest overall prevalence of malnutrition, with 9 of the 13 children having one or more Z scores <−2.
Table 1.
Prevalence of undernutrition within the day-care centres (n = 33 children)
| Variable | Total (N) | Height for age SDS | Body mass index for age SDS | Weight for height | Weight for age SDS | MUAC for age SDS | Malnourisheda |
|---|---|---|---|---|---|---|---|
| Total mean Z score | 33 | −1.65 ± 1.58 | −0.39 ± 1.06 | −0.61 ± 1.02 | −1.19 ± 1.15 | −0.04 ± 1.1 | |
| Portion (%) with Z score <−2 | (11/33) 33% | (4/12) 12% | (4/12) 12% | (11/33) 33% | (2/33) 6% | (13/33) 39% | |
| Mean Z score (malnourished) | 13 | −3.16 ± 1.14 | −0.75 ± 1.17 | −1.21 ± 0.94 | −2.39 ± 0.43 | −0.95 ± 0.88 | |
| Undernutrition per category | |||||||
| 6–11 months | 9 | (1) 11% | (1) 11% | (1) 11% | (3) 33% | (1) 11% | (3) 33% |
| 12–17 months | 11 | (1) 9% | (1) 9% | (1) 9% | (1) 9% | 0 | (1) 9% |
| 18–24 months | 13 | (9) 69%b | (2) 15% | (2) 15% | (7) 54% | (1) 8% | (9) 69% |
SDS, Standard deviation score (Z-score).
aChildren were classified as undernourished if they had any Z score <−2 according to the 2006 WHO growth standards.
bTwo of these children also had severe acute malnutrition with oedema.
General meal observations
Lunch was served between noon and 2 pm, with meals lasting between 20 and 40 min. Apart from one care centre that had two caregivers, all centres had one caregiver attending to all the children during the meal. In one day-care centre, three mothers came to the centre during the lunchtime meal and fed their own children.
Meals were provided from home for over two-thirds (26 of 33) of the children. The rest either had their meals prepared by the caregiver (5 of 33), as was the case in one centre, or purchased (2 of 33) from street vendors. The meal often cost about £0.50 and composed of rice and bean soup, without visible beans. Although adequate for the children, the quality of food as well as the hygienic conditions around these kiosks was lacking. Majority of the children received their meals all at the same time, though younger children were served first in most centres. Most of the children were provided with their own plate of food and a spoon. Several were left to self-feed, with minimal supervision and assistance from the caregivers. Hence, younger children (6–17 months) consumed less than half of food offered, with some crying, playing with their food, looking at others or dozing off.
The use of flat verbalizations like ‘Eat your food' or threats such as ‘I will beat you if you do not eat' were common during meals. Children who were fed by a caregiver had a shorter mealtime than those who self-fed, as caregivers were rushing to attend to other children. Infants who shared food/plates seemed to be left yearning and crying for more, but the caregiver rarely served another food portion.
On the other hand, the three children who were fed by their mothers had their own plates, received encouragement and undistracted assistance to eat. Hence, they consumed more than half of the food offered without any observed flat verbalizations.
Poor hygiene practices were observed in all the centres. Caregivers washed neither their hands nor those of the children before feeding. Meals were served on plates placed on the dusty cemented floors. Although children were provided with spoons, the majority struggled using them and instead used their unwashed hands to eat. Others rubbed their spoons on the untidy floor and then resumed feeding using these dirty spoons.
Individual meal observations
These were done in 11 of the 33 recruited children, with the meal lasting about 30 min. Meals served were mainly (7 of 11) dry solids that consisted of either boiled rice, boiled green bananas or boiled potatoes. In cases where meals were served with either bean or meat stew, only the soup and not the pieces of beans and meat were served. Apart from legumes (mainly beans/peas), none of the meals served had other types of vegetables, particularly leafy vegetables. Six children between 12 and 17 months were fed by the caregiver, who simultaneously attended to other children, while five fed themselves. Two children (of 11) did not have their own plate, in which case the caregiver fed them out of a shared plate. Most children readily accepted the food and ate throughout the meal, but only four children ate more than half the food provided (more than half a fist), and only two were served more food when they had finished. All children were calm at the beginning of meal, but by the end of the meal, most were crying. The children became increasingly distracted and self-fed less as the meal progressed. The meal was terminated by the child in most (8 of 11) cases. Caregivers rarely encouraged children to eat throughout the meal and often shifted their attention to other children (Table 2).
Table 2.
Children and observed actions during mealtime (n = 11)
| Child’s actions | Beginning | Five minutes into meal | End |
|---|---|---|---|
| Interest in food | |||
| Interested | 10 (91%) | 8 (73%) | 6 (54%) |
| Distracted | 4 (37%) | 8 (73%) | 10 (91%) |
| Self-feeding | |||
| Not at all | 5 (46%) | 5 (46%) | 7 (63%) |
| Other child actions throughout meal | |||
| Served dry solids | 7 (63%) | ||
| Shared same plate | 2 (18%) | ||
| Ate less than half of food | 7 (63%) | ||
| Served more food | 2 (18%) | ||
| Ended feeding episode | 8 (73%) | ||
| Caregivers actions | |||
| Encourages child to eat most of the time | 3 (27%) | 3 (27%) | 2 (18%) |
| Distracted | 9 (82%) | 10 (91%) | 10 (91%) |
DISCUSSION
The present study was designed to assess feeding, hygiene practices and child nutritional status in urban slum day-care centres in Nairobi. This pilot study also aided in testing the observation tools to be used for the main study assessing child care practices in urban slum Kenyan homes and a peri-urban area in Lahore, Pakistan. A high prevalence of undernutrition was found as well as poor hygiene and non-responsive feeding practices.
The 33% prevalence of stunting was similar to the 35–37% reported by other studies among children <5 years in Kenya [12, 24], while the prevalence of wasting of 12% was higher than the 7% reported at the national level [12]. The prevalence of underweight in this study (33%) was double the previously reported (16%) prevalence among children <5 years [12]. Nonetheless, it was similar to that reported in poor rural areas where hygiene conditions may reflect those in slums [25] and to the 33% that was observed among children <2 years in a peri-urban slum in Southern India [26]. Nine of 13 children in the 18–24 age category reported the highest number of malnourished cases as similarly reported in a study among children aged 5 years in western Kenya [25]. Although the high prevalence of underweight and stunting in this category could have resulted from overestimation of age in cases where records were missing, there was no overall difference in results when the five children with approximated ages were excluded. Undernutrition remained at 11 of 28 (39%), 7 of 11 (70%) malnourished in the 18–24 age category, with overall prevalence of stunting and underweight at 9 of 28 (32%) and 7 of 28 (25%), respectively.
This study also showed the prevalence of poor hygiene practices characterized by the absence of hand-washing before food handling in the day-care centres. Similar findings were reported among Kenyan households [27]. This increases the risk of transmission of diarrhoeal diseases associated with poor appetite, reduced food intake and low nutrition status [25, 28, 29]. Hand-washing with soap has been shown to significantly reduce the prevalence of diarrhoea in low-income communities [30]. It is likely that water for care centre use was limited by low income, resulting in a rationed quantity of water purchases. Nonetheless, there is a need to double efforts in promoting hand-washing, particularly before food handling and feeding.
In this study, because majority of the children carried food from home, parents played a key role in determining what the children consumed, as in the home [31, 32]. The foods offered to the children were carbohydrate based, lacked animal source protein and leafy vegetables as previously been reported in other studies carried out in developing countries [33, 34]. A study conducted among Kenyan households [32] showed that some parents considered certain food items expensive, while others claim that children are not able to consume them.
Apart from the few cases where the mothers came to feed their children during lunchtime, non-responsive feeding practices characterized by absence of encouragement during feeding were observed in the care centres. This resulted in 7 of the 11 observed children losing interest in food and consuming less than half of food offered. This could be partly because of the low caregiver–child ratio (1:10), which made it hard for the caregiver to adequately attend to all children. Still, it is possible that these children had poor appetite or lacked the skills and coordination necessary for self-feeding. Similar high rates of non-responsive feeding were also reported in Nicaragua as well as in a study done in Ethiopia, where caregivers were reported to encourage feeding in only 40% of eating events [35–36]. To effect a successful feeding event, the caregiver ought to closely supervise the child’s self-feeding episode and where need be, assist a child to feed [37].
Apart from the poor care practices in the day-care centres, several other factors away from the care centre may also have contributed to the poor nutrition status. Factors related to poverty such as inadequate intake of nutritious food, inadequate breast feeding, low birth weight and presence of parasitic and infectious diseases are well-documented, predisposing children in slum settlements to undernutrition [38–40]. Data collected on all these factors may provide a deeper insight into the source of problem and guide future interventions.
This study is the first to assess feeding and care practices in day-care centres in Kenyan urban slums. It was particularly strengthened by direct observation with a systematic observation schedule. However, because of time limitation, only five centres were studied, which may not be representative. In addition to the small sample sizes used, the observation schedule had not been previously tested in this setting. Also, only one meal was observed and hence may not reflect the usual feeding practices. More data collection days could have reduced day-to-day variability and given a comprehensive view of dietary intake and patterns. The invasive nature of the observations might have resulted in change in subjects’ behaviour and hence systematic bias in the data collected [41]. The approximation of child ages by the caregivers may also have biased the results of this study.
CONCLUSION
Although day-care centres provide alternative care to children on behalf of working parents, overcrowding, poor hygiene and low staff levels are a potential threat to child health, growth and development. There is therefore a need for interventions to improve hygiene, feeding practices and thus child nutritional status in these slum settings. Because such interventions require resources, these care centres would greatly benefit from funding and collaboration with government agencies and non-government organizations. In addition, close supervision of care centre activities should ensure efficient operation and adherence to set standards.
ACKNOWLEDGEMENTS
Special thanks go out to the caregivers, mothers and children involved in the study, without whose help this work may not have been possible.
FUNDING
This study was made possible with funding from the University of Glasgow and the Commonwealth Scholarship Commission, which funded the studies in Glasgow of author I.M.
REFERENCES
- 1.Dewey KG, Brown KH. Update on technical issues concerning complementary feeding of young children in developing countries and implications for intervention programs. Food Nutr Bull 2003;24:5–28. [DOI] [PubMed] [Google Scholar]
- 2.Engle PL, Menon P, Haddad L. Care and nutrition: concepts and measurement. World Dev 1999;27:1309–37. [Google Scholar]
- 3.Engle PL, Riccuiti H. Psychosocial aspects of care and nutrition. Food Nutr Bull 1995;16:356–77. [Google Scholar]
- 4.UNICEF. Strategy for improved nutrition of children and women in developing countries. Indian J Pediatr 1991;58:13–24. [DOI] [PubMed] [Google Scholar]
- 5.Eshel N, Daelmans B, de Mello MC, Martines J. Responsive parenting: interventions and outcomes. Bull World Health Organ 2006;84:991–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pelto GH, Levitt E, Thairu L. Improving feeding practices: current patterns, common constraints, and the design of interventions. Food Nutr Bull 2003;24:45–82. [DOI] [PubMed] [Google Scholar]
- 7.Aboud FE, Shafique S, Akhter S. A responsive feeding intervention increases children's self-feeding and maternal responsiveness but not weight gain. J Nutr 2009;139:1738–43. [DOI] [PubMed] [Google Scholar]
- 8.Dearden KA, Hilton S, Bentley ME, et al. Caregiver verbal encouragement increases food acceptance among Vietnamese toddlers. J Nutr 2009;139:1387–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ha PB, Bentley ME, Pachon H, et al. Caregiver styles of feeding and child acceptance of food in rural Viet Nam. Food Nutr Bull 2002;23(Suppl. 4):95–100. [PubMed] [Google Scholar]
- 10.Nti CA, Lartey A. Influence of care practices on nutritional status of Ghanaian children. Nutr Res Pract 2008;2:93–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oni GA, Brown KH, Bentley ME, et al. Feeding practices and prevalence of hand ‐ feeding of infants and young children in Kwara State, Nigeria. Ecol Food Nutr 1991;25:209–19. [Google Scholar]
- 12.Masibo PK, Makoka D. Trends and determinants of undernutrition among young Kenyan children: Kenya Demographic and Health Survey: 1993, 1998, 2003 and 2008–2009. Public Health Nutr 2012;15:1715–27. [DOI] [PubMed] [Google Scholar]
- 13.UNICEF. Evaluation of integrated management of acute malnutrition (IMAM) Kenya. Country case study. United Nations Children's fund, New York, 2012. http://www.unicef.org/evaldatabase/files/Kenya_CMAM_formatted_final.pdf (20 October 2014, date last accessed) [Google Scholar]
- 14.Abuya BA, Ciera J, Kimani-Murage E. Effect of mother's education on child's nutritional status in the slums of Nairobi. BMC Pediatr 2012;12:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olack B, Burke H, Cosmas L, et al. Nutritional status of under-five children living in an informal urban settlement in Nairobi, Kenya. J Health Popul Nutr 2011;29:357–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suda CA. Gender disparities in the kenyan labor market: implications for poverty reduction. Nordic J Afr Stud 2002;11:301–21. [Google Scholar]
- 17.Mbugua TJ. Early childhood care and education in Kenya. Child Educ 2004;80:191. [Google Scholar]
- 18.Kola P. Initiative to enhance pre-primary learning. Daily Nation, 20th August 2001. [Google Scholar]
- 19.UNICEF. Upper mid arm circumference. 2014. http://www.unicef.org/supply/files/Mid_Upper_Arm_Circumference_Measuring_Tapes.pdf (20 October 2014, date last accessed) [Google Scholar]
- 20.National Health Service, NHS. Policy and Procedure for Weighing and Measuring Infants and Children. Royal Hospital for Sick Children, 2007. http://www.clinicalguidelines.scot.nhs.uk/Dietetics/Weighing%20%20Measuring%20Policy%20YOR-DIET-002May07.pdf (15 October 2015, date last accessed). [Google Scholar]
- 21.Flax VL, Makinen S, Ashorn U, et al. Responsive feeding and child interest in food vary when rural Malawian children are fed lipid-based nutrient supplements or local complementary food. Matern Child Nutr 2013;9:369–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore AC, Akhter S, Aboud FE. Responsive complementary feeding in rural Bangladesh. Soc Sci Med 2006;62:1917–30. [DOI] [PubMed] [Google Scholar]
- 23.WHO. WHO Anthro (version 3.2.2, January 2011) and macros 2011. 2015. http://www.who.int/childgrowth/software/en/. [Google Scholar]
- 24.Gewa CA, Yandell N. Undernutrition among Kenyan children: contribution of child, maternal and household factors. Public Health Nutr 2012;15:1029–38. [DOI] [PubMed] [Google Scholar]
- 25.Bloss E, Wainaina F, Bailey RC. Prevalence and predictors of underweight, stunting, and wasting among children aged 5 and under in western Kenya. J Trop Pediatr 2004;50:260–70. [DOI] [PubMed] [Google Scholar]
- 26.Sarkar R, Sivarathinaswamy P, Thangaraj B, et al. Burden of childhood diseases and malnutrition in a semi-urban slum in southern India. BMC Public Health 2013;13:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmidt WP, Aunger R, Coombes Y, et al. Determinants of handwashing practices in Kenya: the role of media exposure, poverty and infrastructure. Trop Med Int Health 2009;14:1534–41. [DOI] [PubMed] [Google Scholar]
- 28.Kimani-Murage EW, Ngindu AM. Quality of water the slum dwellers use: the case of a Kenyan slum. J Urban Health 2007;84:829–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taddei JA, Cannon MJ, Warner L, et al. Nutritional gains of underprivileged children attending a day care center in S.Paulo City, Brazil: a nine month follow-up study. Rev Bras Epidemiol 2000;3:29–37. [Google Scholar]
- 30.Ejemot RI, Ehiri JE, Meremikwu MM, Critchley JA. Hand washing for preventing diarrhoea. Cochrane Database Syst Rev 2008:CD004265. [DOI] [PubMed] [Google Scholar]
- 31.Kamau-Thuita F, Omwega AM, Muita JW. Child care practices and nutritional status of children aged 0-2 years in Thika, Kenya. East Afr Med J 2002;79:524–9. [DOI] [PubMed] [Google Scholar]
- 32.Macharia CW, Kogi-Makau W, Muroki NM. Dietary intake, feeding and care practices of children in Kathonzweni division, Makueni District, Kenya. East Afr Med J 2004;81:402–7. [DOI] [PubMed] [Google Scholar]
- 33.Bwibo NO, Neumann CG. The need for animal source foods by Kenyan children. J Nutr 2003;133(11 Suppl. 2):3936S–40S. [DOI] [PubMed] [Google Scholar]
- 34.Michaelsen KF, Hoppe C, Roos N, et al. Choice of foods and ingredients for moderately malnourished children 6 months to 5 years of age. Food Nutr Bull 2009;30(Suppl. 3):S343–404. [DOI] [PubMed] [Google Scholar]
- 35.Engle PL, Zeitlin M. Active feeding behavior compensates for low interest in food among young Nicaraguan children. J Nutr 1996;126:1808–16. [DOI] [PubMed] [Google Scholar]
- 36.Wondafrash M, Amsalu T, Woldie M. Feeding styles of caregivers of children 6-23 months of age in Derashe special district, Southern Ethiopia. BMC Public Health 2012;12:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Engle PL. Infant feeding styles: barriers and opportunities for good nutrition in India. Nutr Rev 2002;60:S109–14 [DOI] [PubMed] [Google Scholar]
- 38.Calder PC, Jackson AA. Undernutrition, infection and immune function. Nutr Res Rev 2000;13:3–29. [DOI] [PubMed] [Google Scholar]
- 39.Ghosh S, Shah D. Nutritional problems in urban slum children. Indian Pediatr 2004;41:682–96. [PubMed] [Google Scholar]
- 40.Kimani-Murage EW, Madise NJ, Fotso JC, et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health 2011;11:396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gittelsohn J, Shankar A, West K, et al. Estimating reactivity in direct observation studies of health behaviors. Hum Organ 1997;56:182–9. [Google Scholar]