Despite a growing number of new molecular targets, allogeneic hematopoietic cell transplantation remains the most relevant treatment for adverse risk AML.1 In order to balance a low therapy-related mortality with high anti-leukemic efficacy relying on the GvL effect, Schmid et al. introduced a sequential therapy approach consisting of cytoreductive chemotherapy with fludarabine, high-dose cytarabine and amsacrine (FLAMSA), followed by reduced-intensity conditioning (RIC) with 4-Gy TBI, high-dose cyclophosphamide and antithymocyte globulin, and prophylactic donor lymphocyte infusions if indicated. With this regimen, long-term remissions are achieved in up to 40% of patients with high-risk AML.2 Considering the current controversy about the clinical relevance of extramedullary disease (EMD)3, 4 and tumor burden as one of the strongest predictors for treatment outcome after hematopoietic stem cell transplantation (HSCT), we performed a retrospective analysis of high-risk AML patients treated with FLAMSA-RIC followed by HSCT with respect to the impact of medullary as well as EMD manifestations.
Eighty-four patients diagnosed with de novo AML (n=67) or secondary AML (n=17) treated at our institution between 2000 and 2012 were included. High-risk disease was defined as AML with high-risk cytogenetics,5 secondary AML, AML in second CR, primary induction failure and chemo-refractory relapse (Table 1). Disease staging before transplant included a lumbar puncture and the prophylactic administration of 12 mg of methotrexate in all patients. Outcome was analyzed with respect to overall survival (OS), cumulative incidence of death (CID) or cumulative incidence of relapse (CIR).
Table 1. Patient characteristics.
| Patient characteristics | Number (%) | Univariate analysis | Multivariate analysis |
|---|---|---|---|
| No. of patients | 84 (100) | ||
| Age (years) | P=0.886 | ||
| Median | 48.7 | ||
| >60 | 8 (9) | ||
| <60 | 76 (91) | ||
| Sex | P=0.538 | ||
| Male | 46 (55) | ||
| Female | 38 (45) | ||
| Diagnosis | P=0.786 | ||
| De novo AML | 67 (80) | ||
| sAML | 17 (20) | ||
| Cytogenetic risk (ELN) | P=0.125 | ||
| Favorable | 9 (11) | ||
| Intermediate I | 16 (19) | ||
| Intermediate II | 25 (30) | ||
| Adverse | 34 (40) | ||
| Stage at transplantation | P=0.005 | P=0.292 | |
| First CR | 13 (15) | ||
| Second CR | 12 (14) | ||
| Primary refractory | 31 (37) | ||
| Refractory relapse | 28 (34) | ||
| Extramedullary disease | 24 (29) | P<0.001 | P=0.981 |
| Time | |||
| Present at transplantation | 17 | P<0.001 | P=0.008 |
| Present at relapse after transplantation | 4 | ||
| Present at first relapse before transplantation | 1 | ||
| Only present at diagnosis | 1 | ||
| Localized | |||
| Chloroma | 7 (25) | ||
| Meningeosis | 16 (67) | ||
| Chloroma and meningeosis | 2 (8) | ||
| GvHD | |||
| cGvHD | 32 (38) | ||
| Skin | 21 (25) | ||
| Gastrointestinal | 11 (13) | ||
| aGvHD | 44 (52) | ||
| Skin | 19 (22) | ||
| Gastrointestinal | 25 (30) | ||
| Donor | P=0.984 | ||
| Family donor | 16 (19) | ||
| Unrelated donor | 56 (67) | ||
| Unrelated HLA-mismatch donor | 12 (14) | ||
| Prior transplantation | 5 | ||
| Allogeneic HSCT | 4 | ||
| Autologous HSCT | 1 | ||
| Cause of death | |||
| Leukemia related | 34 (57) | ||
| Non-leukemia mortality | 22 (37) | ||
| Unknown | 4 (6) | ||
Abbreviation: ELN, European Leukemia Network.
Bold entries represent P<0.05.
In 17 patients (20%), EMD was present at the time of HSCT; 10 CNS, 3 chloroma (1 skin, 1 axillary lymph nodes and 1 intraorbital) and 4 with multiple sites (1 CNS, skin and pleural effusion, 1 CNS and cervical lymph nodes, 1 lymph nodes and skin, and 1 CNS and skin). In seven patients, EMD persisted in spite of prior intrathecal (i.th.) therapy or i.th. therapy plus irradiation (two patients), in the remaining 10 patients EMD (7 CNS, 3 skin) was detected immediately before the initiation of the conditioning regimen so that no additional therapy directed toward the extramedullary manifestation was given.
All patients with EMD at HSCT also presented with active bone marrow disease (Table 1). After HSCT, 8 of 13 patients with CNS involvement (two died during HSCT, one had intracerebral bleeding during HSCT) received i.th. therapy with either 12 mg methotrexate or 40 mg cytarabine or 50 mg liposomal cytarabine ranging from 1 to 5 administrations.
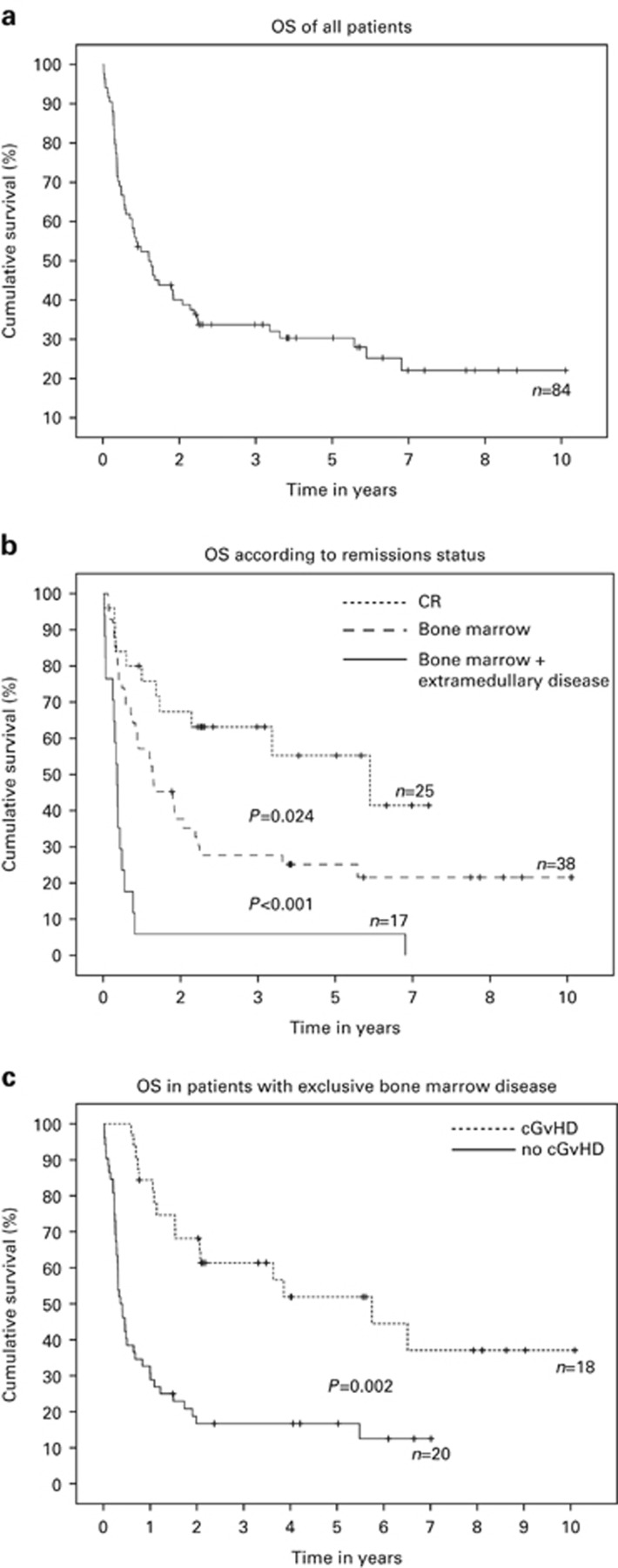
The median OS after HSCT was 12.1 months (confidence interval (CI) 95% range, 6.4–17.6 months) with survival rates at 1, 2 and 4 years of 51%, 35% and 24% respectively, which is in line with previous publications6 (Figure 1a). There was no significant difference in OS (Table 1), CIR and CID (data not shown) according to sex, age, donor type, de novo AML or sAML and cytogenetics. The hematopoietic CR rate of refractory (including primary refractory and refractory relapse) patients after HSCT was 81% (four patients died during HSCT, seven showed persistent bone marrow disease). Six of seven patients who presented with persistent bone marrow disease had exclusive bone marrow disease before HSCT with no extramedullary involvement.
Figure 1.
(a) Overall survival (OS) of all analyzed patients. (b) OS according to remission status. (c) OS of patients who developed cGvHD with bone marrow disease but no extramedullary disease.
CID for patients in CR (n=25) and no-CR (n=59) before transplant after 12 months was 25% and 59%, respectively; whereas CIR was 19% and 60%, respectively. Patients transplanted in CR had a 2-year OS rate of 63% in comparison with 24% for refractory patients (Figure 1b). With regard to tumor load, in a multivariable analysis the strongest predictive factor for inferior prognosis was absence of CR at the time of HSCT with concurrent EMD (P=0.008; HR 0.31; CI 95%: 0.131–0.732). Due to the small number of patients, no differences were seen in location of the EMD site.
The median OS of these patients was 3.6 months in comparison with patients with exclusively active bone marrow disease with a median OS of 13 months (P<0.0001) (Figure 1b). With regard to GvHD, cGvHD positively modulated relapse-free survival (P<0.001) for all patients who were alive at day +100 (Figure 1c). However, in a subgroup analysis this was not seen for patients with extramedullary and concurrent bone marrow disease at HSCT.
FLAMSA-RIC followed by allogeneic HSCT offers acceptable OS rates for high-risk AML patients without concurrent active bone marrow and EMD. This confirms prior studies that did not specifically evaluate the impact of EMD.6, 7 In the retrospective analysis by Goyal et al.4 no impact of pre-transplant EMD was observed with regard to outcome. However, patients with active medullary disease and EMD were excluded from the multivariate analysis due to their dismal outcome. Here, we made a similar observation that concurrent EMD is highly associated with a negative outcome in AML patients and that FLAMSA-RIC followed by HSCT is not effective in this patient group. The study by Bommer et al. exclusively focused on AML patients with CNS involvement underlining an adverse outcome in this patient group despite intrathecal blast clearance.3 In our cohort of patients with residual disease, we could demonstrate a strong GvL effect associated with cGvHD but again this applied only to the subgroup without extramedullary involvement. There are several potential reasons for the lack of an effective GvL, such as the higher tumor load at transplant or the poor accessibility of extramedullary sites to alloreactive lymphocytes.8, 9
Taken together, our data suggest that allogeneic HSCT as currently performed is futile in this subgroup of patients. Unfortunately, only insufficient data is available to evaluate a potential beneficial effect of an earlier diagnosis of extramedullary involvement by routine lumbar puncture and/or PET-CT and systematic treatment of extramedullary manifestations.
Acknowledgments
FK was supported by grants from Deutsche Krebshilfe grant 109420 (Max-Eder program); fellowship 2010/04 by the European Hematology Association; and by the Deutsche Forschungsgemeinschaft (grant D.3955 (SFB 1074)).
The authors declare no conflict of interest.
References
- Schlenk RF. Post-remission therapy for acute myeloid leukemia. Haematologica 2014; 99: 1663–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol 2005; 23: 5675–5687. [DOI] [PubMed] [Google Scholar]
- Bommer M, von Harsdorf S, Dohner H, Bunjes D, Ringhoffer M. Neoplastic meningitis in patients with acute myeloid leukemia scheduled for allogeneic hematopoietic stem cell transplantation. Haematologica 2010; 95: 1969–1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal SD, Zhang MJ, Wang HL, Akpek G, Copelan EA, Freytes C et al. Allogeneic hematopoietic cell transplant for AML: no impact of pre-transplant extramedullary disease on outcome. Bone Marrow Transplant 2015; 50: 1057–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 2010; 115: 453–474. [DOI] [PubMed] [Google Scholar]
- Schmid C, Schleuning M, Schwerdtfeger R, Hertenstein B, Mischak-Weissinger E, Bunjes D et al. Long-term survival in refractory acute myeloid leukemia after sequential treatment with chemotherapy and reduced-intensity conditioning for allogeneic stem cell transplantation. Blood 2006; 108: 1092–1099. [DOI] [PubMed] [Google Scholar]
- Schmid C, Schleuning M, Hentrich M, Markl GE, Gerbitz A, Tischer J et al. High antileukemic efficacy of an intermediate intensity conditioning regimen for allogeneic stem cell transplantation in patients with high-risk acute myeloid leukemia in first complete remission. Bone Marrow Transplant 2008; 41: 721–727. [DOI] [PubMed] [Google Scholar]
- Yoshihara S, Ando T, Ogawa H. Extramedullary relapse of acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation: an easily overlooked but significant pattern of relapse. Biol Blood Marrow Transplant 2012; 18: 1800–1807. [DOI] [PubMed] [Google Scholar]
- Au WY, Kwong YL, Lie AK, Ma SK, Liang R. Extra-medullary relapse of leukemia following allogeneic bone marrow transplantation. Hematol Oncol 1999; 17: 45–52. [DOI] [PubMed] [Google Scholar]