Abstract
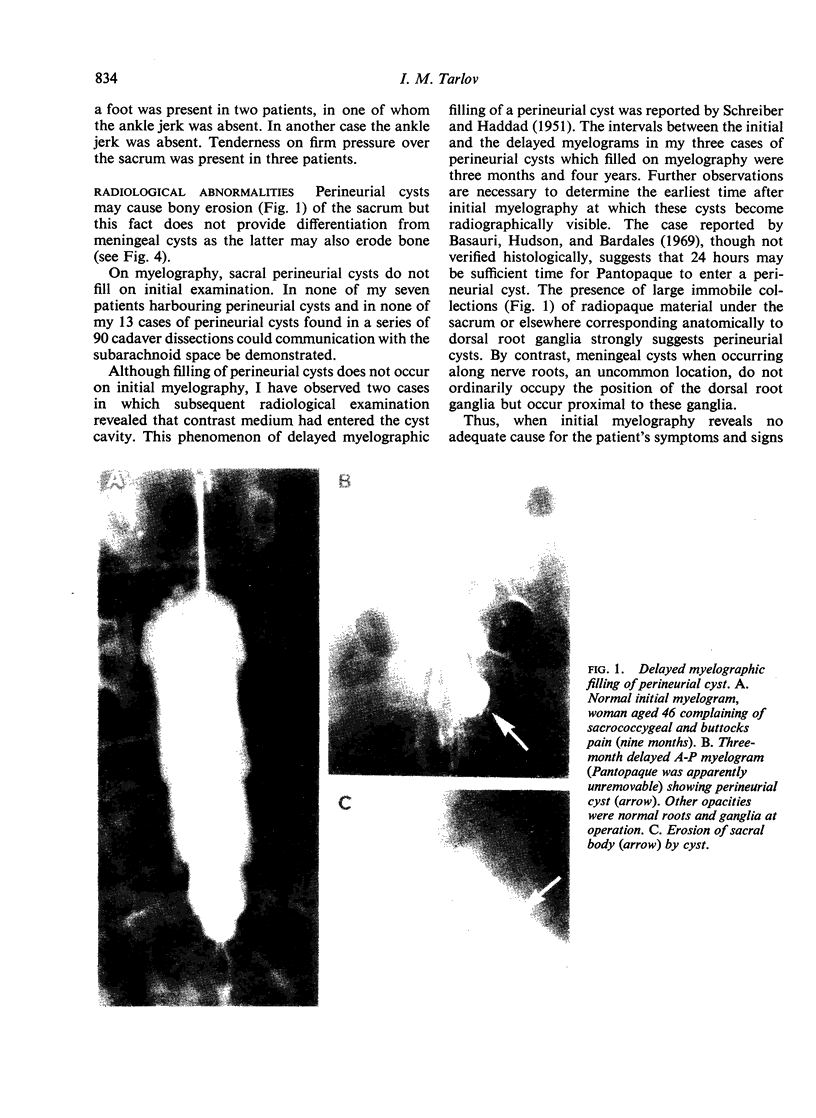
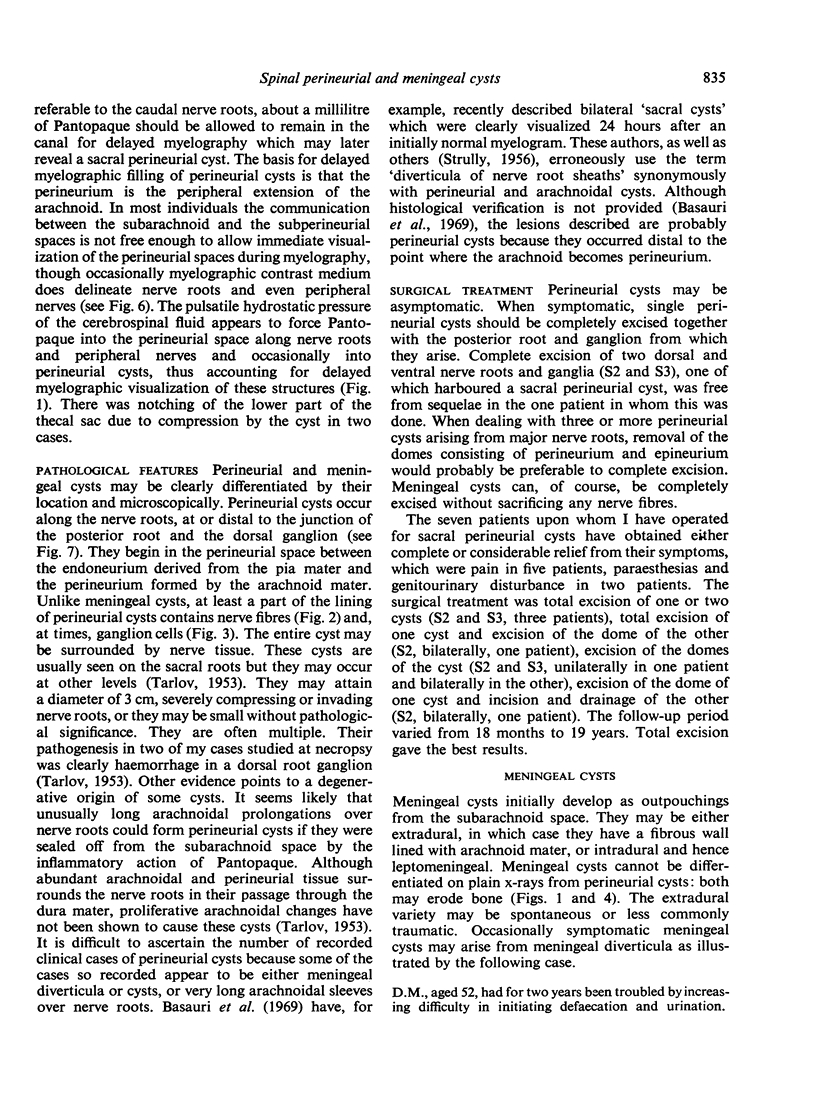
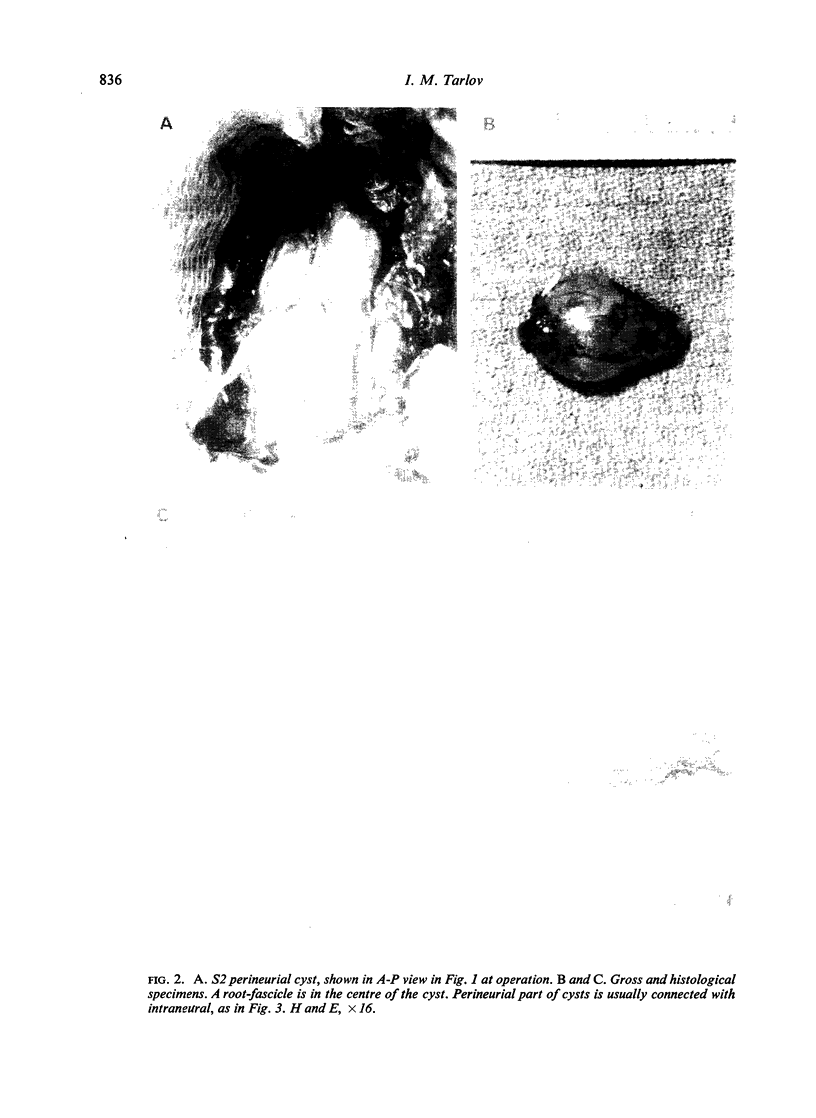
Perineurial cysts may be responsible for clinical symptoms and a cure effected by their removal. They do not fill on initial myelography but may fill with Pantopaque some time, days or weeks, after Pantopaque has been instilled into the subarachnoid space. Perineurial cysts arise at the site of the posterior root ganglion. The cyst wall is composed of neural tissue. When initial myelography fails to reveal an adequate cause for the patient's symptoms and signs referable to the caudal nerve roots, then about a millilitre of Pantopaque should be left in the canal for delayed myelography which may later reveal a sacral perineurial cyst or, occasionally, a meningeal cyst. Meningeal diverticula occur proximal to the posterior root ganglia and usually fill on initial myelography. They are in free communication with the subarachnoid space and are rarely in my experience responsible for clinical symptoms. Meningeal diverticula and meningeal cysts appear to represent a continuum. Pantopaque left in the subarachnoid space may convert a meningeal diverticulum into an expanding symptomatic meningeal cyst, as in the case described. Many cases described as perineurial cysts represent abnormally long arachnoidal prolongations over nerve roots or meningeal diverticula. In general, neither of the latter is of pathological significance. Perineurial, like meningeal cysts and diverticula, may be asymptomatic. They should be operated upon only if they produce progressive or disabling symptoms or signs clearly attributable to them. When myelography must be done, and this should be done only as a preliminary to a probable necessary operation, then patient effort should be made to remove the Pantopaque.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander E., Jr, Davis C. H., Jr Reduction and fusion of fracture of the odontoid process. J Neurosurg. 1969 Nov;31(5):580–582. doi: 10.3171/jns.1969.31.5.0580. [DOI] [PubMed] [Google Scholar]
- Bergland R. M. Congenital intraspinal extradural cyst. Report of three cases in one family. J Neurosurg. 1968 May;28(5):495–499. doi: 10.3171/jns.1968.28.5.0495. [DOI] [PubMed] [Google Scholar]
- DASTUR H. M. The radiological appearances of spinal extradural arachnoid cysts. J Neurol Neurosurg Psychiatry. 1963 Jun;26:231–235. doi: 10.1136/jnnp.26.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GORTVAI P. Extradural cysts of the spinal canal. J Neurol Neurosurg Psychiatry. 1963 Jun;26:223–230. doi: 10.1136/jnnp.26.3.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOFFMANN G. T. Cervical arachnoidal cyst. Report of a 6-year-old Negro male with recovery from quadriplegia. J Neurosurg. 1960 Mar;17:327–330. doi: 10.3171/jns.1960.17.2.0327. [DOI] [PubMed] [Google Scholar]
- HOLT S., YATES P. O. CERVICAL NERVE ROOT "CYSTS". Brain. 1964 Sep;87:481–490. doi: 10.1093/brain/87.3.481. [DOI] [PubMed] [Google Scholar]
- Kao C. C., Uihlein A., Bickel W. H., Soule E. H. Lumbar intraspinal extradural ganglion cyst. J Neurosurg. 1968 Aug;29(2):168–172. doi: 10.3171/jns.1968.29.2.0168. [DOI] [PubMed] [Google Scholar]
- MASON M. S., RAAF J. Complications of pantopaque myelography. Case report and review. J Neurosurg. 1962 Apr;19:302–311. doi: 10.3171/jns.1962.19.4.0302. [DOI] [PubMed] [Google Scholar]
- Miller P. R., Elder F. W., Jr Meningeal pseudocysts (meningocele spurius) following laminectomy. Report of ten cases. J Bone Joint Surg Am. 1968 Mar;50(2):268–276. doi: 10.2106/00004623-196850020-00005. [DOI] [PubMed] [Google Scholar]
- NUGENT G. R., ODOM G. L., WOODHALL B. Spinal extradural cysts. Neurology. 1959 Jun;9(6):397–406. doi: 10.1212/wnl.9.6.397. [DOI] [PubMed] [Google Scholar]
- SCHREIBER F., HADDAD B. Lumbar and sacral cysts causing pain. J Neurosurg. 1951 Sep;8(5):504–509. doi: 10.3171/jns.1951.8.5.0504. [DOI] [PubMed] [Google Scholar]
- STRULLY K. J. Meningeal diverticula of sacral nerve roots (perineurial cysts). J Am Med Assoc. 1956 Jul 21;161(12):1147–1152. doi: 10.1001/jama.1956.02970120029009. [DOI] [PubMed] [Google Scholar]
- SVIEN H. J., THELEN E. P., KEITH H. M. Intraspinal tumors in children. J Am Med Assoc. 1954 Jul 10;155(11):959–961. doi: 10.1001/jama.1954.03690290009003. [DOI] [PubMed] [Google Scholar]
- TARLOV I. M., DAY R. Myelography to help localize traction lesions of the brachial plexus. Am J Surg. 1954 Aug;88(2):266–271. doi: 10.1016/s0002-9610(54)90510-3. [DOI] [PubMed] [Google Scholar]
- TENG P., RUDNER N. Multiple arachnoid diverticula. Arch Neurol. 1960 Mar;2:348–356. doi: 10.1001/archneur.1960.03840090112015. [DOI] [PubMed] [Google Scholar]