ABSTRACT
Nipah virus (NiV) is a highly lethal paramyxovirus that recently emerged as a causative agent of febrile encephalitis and severe respiratory disease in humans. The ferret model has emerged as the preferred small-animal model with which to study NiV disease, but much is still unknown about the viral determinants of NiV pathogenesis, including the contribution of the C protein in ferrets. Additionally, studies have yet to examine the synergistic effects of the various P gene products on pathogenesis in animal models. Using recombinant NiVs (rNiVs), we examine the sole contribution of the NiV C protein and the combined contributions of the C and W proteins in the ferret model of NiV pathogenesis. We show that an rNiV void of C expression resulted in 100% mortality, though with limited respiratory disease, like our previously reported rNiV void of W expression; this finding is in stark contrast to the attenuated phenotype observed in previous hamster studies utilizing rNiVs void of C expression. We also observed that an rNiV void of both C and W expression resulted in limited respiratory disease; however, there was severe neurological disease leading to 60% mortality, and the surviving ferrets demonstrated sequelae similar to those for human survivors of NiV encephalitis.
IMPORTANCE Nipah virus (NiV) is a human pathogen capable of causing lethal respiratory and neurological disease. Many human survivors have long-lasting neurological impairment. Using a ferret model, this study demonstrated the roles of the NiV C and W proteins in pathogenesis, where lack of either the C or the W protein independently decreased the severity of clinical respiratory disease but did not decrease lethality. Abolishing both C and W expression, however, dramatically decreased the severity of respiratory disease and the level of destruction of splenic germinal centers. These ferrets still suffered severe neurological disease: 60% succumbed to disease, and the survivors experienced long-term neurological impairment, such as that seen in human survivors. This new ferret NiV C and W knockout model may allow, for the first time, the examination of interventions to prevent or mitigate the neurological damage and sequelae experienced by human survivors.
INTRODUCTION
Nipah virus (NiV), a lethal human pathogen, recently emerged in Southeast Asia. NiV belongs to the family Paramyxoviridae and causes acute respiratory disease and/or severe encephalitis with systemic vasculitis (1, 2). Outbreak case fatality rates can reach 92% (3, 4), and many of the surviving patients experience long-term neurological sequelae (5). A single NiV outbreak occurred in Malaysia and Singapore in 1998 to 1999 (6), whereas outbreaks occur almost annually in Bangladesh and northeastern India (7–12); an outbreak also occurred in the Philippines in 2014 (13). Little is known about NiV pathogenesis (14, 15), and the viral determinants that contribute to the pulmonary and encephalitic components of NiV-mediated disease have not yet been identified; however, we recently reported on the contributions of the V and W proteins in the ferret model of NiV disease (16).
Pteropus bats are the reservoir for NiV (17), with spillover into humans, pigs, dogs, cats, and other species (13, 18–20). Developed experimental animal models for NiV infection exist; the most commonly used animals include hamsters (21), ferrets (22), and African green monkeys (AGMs) (23). Due to size, cost, and ethical considerations, greater numbers of hamsters than of ferrets or AGMs can be employed in experiments. However, hamsters model NiV-mediated disease only in a dose-dependent manner; they develop meningoencephalitis (with a low dose) or respiratory disease (with a high dose) (24). The recently developed ferret model of NiV infection models all major aspects of NiV-mediated disease in humans regardless of the dose (2), including both respiratory disease and complex neurological disease, as well as systemic vasculitis (22, 25). Indeed, the ferret model has already proven very useful in deciphering the determinants of NiV pathogenesis (16).
The NiV P gene encodes four proteins; P, C, W, and V (26). The C protein utilizes alternative start codons shortly after the P start codon; the C open reading frame (ORF) is out of frame with P, and therefore, the C protein shares no homology with P (26). The V and W proteins are produced through mRNA editing by the viral polymerase (27, 28), resulting in P, W, and V proteins that share an N-terminal domain but contain unique C-terminal domains. The C, W, and V proteins are not known to interact with each other or with other NiV proteins, and they are not required for in vitro growth of NiV (29). The W protein localizes to the nucleus, at least in some cell types, whereas the C, V, and P proteins localize to the cytoplasm (30, 31).
Although the NiV V and W proteins have previously described roles in directly inhibiting type I interferon (IFN) induction and signaling (30, 32–37), the contribution of the NiV C protein has not been well defined. The NiV C protein appears to decrease viral RNA synthesis (26, 38, 39), thus indirectly inhibiting type I IFN induction. A recent report suggests that the C proteins of several paramyxoviruses, including NiV, inhibit the Toll-like receptor 7/9 (TLR7/9)-dependent induction of IFN-α by binding to inhibitor of κB kinase α (IKKα), thus inhibiting the phosphorylation of IFN regulatory factor 7 (IRF7) (40).
To investigate the role of the C protein in NiV infection, recombinant NiV (rNiV) mutants that do not express the C protein (Cko) have been examined in vitro (29, 39, 41, 42) and in the hamster model (29, 41). The in vivo studies with hamsters yielded differing results: the first study showed that an rNiV-Cko mutant was completely attenuated in hamsters, with 100% survival after challenge (29), while the second study, using similar rNiV-Cko mutants, demonstrated only partial attenuation, with 16.7% to 66.7% survival depending on the challenge dose (41).
To better understand the contribution of the NiV C protein to pathogenesis, we utilized reverse genetics to produce rNiV-Malaysia (rNiVM) mutants containing either a Cko mutation alone or both the Cko and Wko mutations. These rNiVM mutants were characterized in vitro, followed by studies in the ferret model. In contrast to the findings of studies with hamsters, our results suggest that the C protein plays only a minor role in the respiratory component of disease and no role in the neurological component of NiV disease in the ferret model, which is similar to the previously reported role of the W protein (16). We also determined that the C and W proteins have either the same or complementary targets, since rNiVM-CkoWko-infected ferrets had very little respiratory disease but still developed severe neurological disease with 60% mortality. Intriguingly, the surviving ferrets demonstrated sequelae similar to those for human survivors of NiV encephalitis.
MATERIALS AND METHODS
Cell lines.
BSR-T7/5 cells, a BHK-21 cell line stably expressing T7 RNA polymerase (43), were maintained in Dulbecco's modified Eagle medium (DMEM; Gibco, Carlsbad, CA) supplemented with 10% fetal bovine serum (FBS; Gibco), 100 U/ml penicillin, 100 g/ml streptomycin, and 0.5 mg/ml Geneticin (Gibco). Vero 76 cells (ATCC CRL-1587) were maintained in Eagle's minimum essential medium (EMEM) supplemented with 10% FBS, 100 U/ml penicillin (Gibco), and 100 g/ml streptomycin (Gibco). HEK 293T/17 cells (ATCC CRL-11268) and MFP cells (ATCC CRL-1656) were maintained in DMEM supplemented with 10% FBS, 100 U/ml penicillin, and 100 g/ml streptomycin.
Primary cells.
Human pulmonary microvascular endothelial cells (HPMECs; Lonza, Basel, Switzerland) were maintained in endothelial basal medium (EBM-2 MV; Lonza) supplemented with 5% FBS and proprietary concentrations of human epidermal growth factor, fibroblast growth factor, vascular endothelial growth factor, insulin-like growth factor, hydrocortisone, and gentamicin, all provided by Lonza. The medium was changed every 2 to 3 days, and cells were used up to passage 7.
Plasmid construction and generation of recombinant NiVs.
The NiV genomic sequence used to construct the rNiVs in this study was UMMC1 (GenBank accession no. AY029767), an isolate cultured from the cerebrospinal fluid of an encephalitic human patient in the initial outbreak in Malaysia. This NiVM genome was assembled into three segments, A (nucleotides [nt] 1 to 6780), B (nt 6780 to 10404), and C (nt 10404 to 18246), as described previously (42). These fragments could then be mutated, followed by assembly into full-length cDNA clones in pSL1180 cloning vectors containing T7 promoter and terminator sequences and a hepatitis delta virus ribozyme sequence. Three NiVM full-length cDNA clones (pFL-NiVM-Cko, pFL-NiVM-CkoWko, and pFL-NiVM-CkoVko) were constructed. An A segment containing the Cko mutations (T2429C, T2432C, and C2438A), which disrupt both possible start codons for the C open reading frame and introduce an early stop codon, was produced previously (42). Site-directed mutagenesis was performed by Mutagenex Inc. (Piscataway, NJ) to introduce the Wko (C3628T) or Vko (A3629T) mutation into an A segment containing the Cko mutations (see Fig. 1B); the Wko or Vko mutation introduced a stop codon shortly after the editing site in the W or V open reading frame, respectively, as described previously (16).
FIG 1.
rNiVM genome design. (A) (Top) Schematic of the rNiVM genome showing the location of each gene (N, P, M, F, G, and L). Open segments represent open reading frames, and shaded segments represent noncoding regions of the genome. (Bottom) Schematic of the P gene showing the location of the alternative start site for the C protein ORF and the location of the mRNA editing site, which allows for the production of the V and W proteins, as well as the P protein, from the P gene. (B) The start site and ORF for the C protein are shown in relation to the P/V/W start site and ORFs. Nucleotide changes (indicated by orange arrowheads and letters) were incorporated into the P gene to obliterate the C start codons and to introduce early stop codons into the C ORF. (C) Relationships of the unique C-terminal domains of P, V, and W to the mRNA editing site. Nucleotide changes (indicated by green and red arrowheads and letters) were incorporated into the P gene to introduce early stop codons into the V and W ORFs. Numbers flanking the nucleotide sequences indicate positive-sense antigenomic positions. (D) Western blot analysis of Vero cell lysates that were either mock infected or infected with rNiVM-wt, rNiVM-Cko, rNiVM-CkoWko, or rNiVM-CkoVko. NiV P-, V-, W-, and C-specific antibodies were used to detect the presence or absence of the respective proteins.
The pTM1-HA NiVM P helper plasmid was constructed as described previously (42); the P gene was tagged with hemagglutinin (HA) at the amino terminus and was subcloned into the pTM1 expression plasmid. The pTM1.W-NiVM N and pTM1.W-NiVM L helper plasmids were constructed previously (16) by amplifying the sequences for the N and L genes from the A and C segments, respectively, by PCR and were cloned into a pTM1.W expression vector.
rNiVM mutants were generated as described previously (16). Briefly, BSR-T7/5 cells were seeded in 6-well plates and were cotransfected with 3.5 μg of an NiVM full-length cDNA clone, 0.2 μg of pTM1-HA NiVM P, 0.75 μg of pTM1.W-NiVM N, and 0.4 μg of pTM1.W-NiVM L per well in Opti-MEM (Gibco) with Lipofectamine 2000 (Life Technologies) according to the manufacturer's protocol. At 72 h posttransfection, the medium and cells were collected and were passaged onto Vero cells. Cytopathic effect (CPE) was typically observed beginning between days 4 and 8 postinfection (p.i.). The medium was then collected and was passed on Vero cells for plaque purification of the virus. A small quantity (passage 1 [P1]) of the plaque-purified virus was then grown in Vero cells, followed by a larger quantity (P2) in Vero cells infected at a multiplicity of infection (MOI) of 0.01. At 48 h p.i., the virus-containing medium was harvested, clarified by low-speed centrifugation, aliquoted, and stored at −80°C. The presence of the mutations introduced was confirmed by sequencing of reverse transcription-PCR fragments amplified from virus RNA isolated from virus stocks with TRIzol LS reagent (Ambion, Carlsbad, CA). Virus titers were determined by standard plaque assays using 5% neutral red. All experiments using full-length clones or infectious rNiVM were performed using approved protocols in biosafety level 4 (BSL-4) containment at the Galveston National Laboratory (GNL) in Galveston, TX.
Western blot analysis.
Western blot analysis was performed using polyclonal rabbit antisera against the unique C-terminal domains of the NiV P, W, and V proteins and against the NiV C protein. The antisera were produced by GenScript (Piscataway, NJ) as described previously (16). Briefly, 1.2 × 106 Vero cells/well were seeded in a 6-well plate and were infected with either wild-type rNiVM (rNiVM-wt), rNiVM-Cko, rNiVM-CkoWko, or rNiVM-CkoVko at an MOI of 0.01. The cells were harvested at 40 h p.i. in 1 ml of 2× Laemmli sample buffer (Bio-Rad, Hercules, CA) then heated to 95°C for 20 min. Samples were then run on a denaturing 8 to 16% SDS-PAGE gel (Bio-Rad). The proteins were transferred from the gel to polyvinylidene difluoride (PVDF) membranes and were blocked in TTBS (100 mM Tris-HCl [pH 7.5], 0.9% NaCl, 0.1% Tween 20) with 5% skim milk. PVDF membranes were incubated with polyclonal rabbit antisera against NiV P, W, V, and C diluted in TTBS with 5% milk (dilutions, 1:5,000 for P and 1:500 for V, W, or C) for 1 h at room temperature and were washed 4 times in TTBS. The membranes were then incubated with anti-rabbit IgG conjugated to horseradish peroxidase (HRP) (dilution, 1:5,000; Thermo Scientific, Waltham, MA) for 1 h at room temperature, washed 4 times in TTBS, incubated with ECL reagent (Promega) for 5 min, and imaged with a VersaDoc system (Bio-Rad).
Virus growth kinetics.
Overall, 1.2 × 106 Vero, 293T, or MPF cells per well were seeded in 6-well plates and were incubated at 37°C for 12 h with either regular medium or a medium containing 1,000 U/ml of Universal IFN-α (PBL Assay Science, Piscataway, NJ). The cells were then infected at an MOI of 0.01 with either rNiVM-wt, rNiVM-Wko, rNiVM-Vko, rNiVM-Cko, rNiVM-CkoWko, or rNiVM-CkoVko for 1 h, followed by the removal of the inoculum, 4 washes with PBS, and the addition of fresh medium. Supernatants were collected at 1, 6, 12, 24, 36, 48, and 72 h p.i., clarified by centrifugation, aliquoted, and stored at −80°C. All infections were performed in duplicate. The titers of samples were then determined on Vero cells using standard plaque assays. The limit of detection was 25 PFU/ml.
Similarly, 2.5 × 105 HPMECs per well were seeded in 24-well plates and were allowed to polarize for 48 h at 37°C, followed by incubation at 37°C for 12 h with either regular medium or a medium containing 1,000 U/ml of Universal IFN-α (PBL). The cells were then infected at an MOI of 0.01 with either rNiVM-wt, rNiVM-Cko, rNiVM-CkoWko, or rNiVM-CkoVko for 1 h, followed by removal of the inoculum, 4 washes, and the addition of fresh medium. Supernatants were collected at 1, 24, 48, and 72 h p.i., clarified by centrifugation, aliquoted, and stored at −80°C. Additional aliquots were stored for use in chemokine/cytokine analysis, described below. All infections were performed in duplicate. The titers of samples were then determined on Vero cells using standard plaque assays. The limit of detection was 25 PFU/ml.
Chemokine/cytokine analysis.
HPMECs were infected, and supernatants aliquoted and stored, as described above. Levels of 6Ckine/CCL21, B cell-attracting chemokine 1 (BCA-1)/CXCL13, cutaneous T cell-attracting chemokine (CTACK)/CCL27, ENA-78/CXCL5, eotaxin/CCL11, eotaxin-2/CCL24, eotaxin-3/CCL26, fractalkine/CX3CL1, GCP-2/CXCL6, granulocyte-macrophage colony-stimulating factor (GM-CSF), Gro-α/CXCL1, Gro-β/CXCL2, I-309/CCL1, IFN-γ, interleukin 1β (IL-1β), IL-2, IL-4, IL-6, IL-8/CXCL8, IL-10, IL-16, IFN-inducible protein 10 (IP-10)/CXCL10, IFN-inducible T cell alpha chemoattractant (I-TAC)/CXCL11, monocyte chemoattractant protein 1 (MCP-1)/CCL2, MCP-2/CCL8, MCP-3/CCL7, MCP-4/CCL13, macrophage-derived chemokine (MDC)/CCL22, macrophage migration inhibitory factor (MIF), monokine induced by IFN-γ (MIG)/CXCL9, macrophage inflammatory protein 1α (MIP-1α)/CCL3, MIP-1δ/CCL15, MIP-3α/CCL20, MIP-3β/CCL19, myeloid progenitor inhibitory factor 1 (MPIF-1)/CCL23, SCYB16/CXCL16, stromal cell-derived factor 1α and 1β (SDF-1α+β)/CXCL12, thymus- and activation-regulated chemokine (TARC)/CCL17, thymus-expressed chemokine (TECK)/CCL25, and tumor necrosis factor alpha (TNF-α) in supernatants from infected HPMECs were quantified. Briefly, gamma-irradiated supernatants were diluted 1:4, and 50 μl of each sample was quantified using a Bio-Plex Pro human chemokine 40-plex panel (Bio-Rad) according to the manufacturer's instructions. Infections and supernatant sample collection were performed in duplicate, and each sample was quantified in duplicate. Samples were assayed across at least a 100-bead region. Assays were performed on the Bio-Plex 200 machine, and the results were analyzed using Bio-Plex Manager software (version 6.1; Bio-Rad).
Levels of IFN-α or IFN-β were quantified using 25 μl of undiluted supernatant in a Human IFN-α (multisubtype) or Human IFN-β enzyme-linked immunosorbent assay (ELISA) kit, respectively (Thermo Scientific), according to the manufacturer's instructions. All samples were read for dilution endpoints at 405 nm on a Molecular Devices (Sunnyvale, CA) EMax microplate reader.
Statistics.
Conducting animal studies in BSL-4 containment severely restricts the number of animal subjects, the volume of biological samples that can be obtained, and the ability to repeat assays independently, thus limiting statistical analysis. Consequently, data are presented as means calculated from replicate samples, not replicate assays, and error bars represent the standard deviations across replicates.
Prism 5 software was used to calculate statistical significance throughout this study using the log rank (Mantel-Cox) test for Kaplan-Meier survival curves and analysis of variance (ANOVA) with Dunnett's multiple-comparison test for viral growth kinetics and chemokine/cytokine analysis.
Animals.
Animal studies were performed in BSL-4 biocontainment at the GNL at the University of Texas Medical Branch (UTMB) in Galveston, TX, and were approved by the UTMB Institutional Animal Care and Use Committee (IACUC). Animal research was conducted in compliance with the Animal Welfare Act and other Federal statutes and regulations relating to animals and experiments involving animals. The research adhered to the principles stated in the 8th edition of the Guide for the Care and Use of Laboratory Animals, National Research Council, 2011 (44). The facility where this research was conducted is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
Fifteen female 6- to 8-month-old ferrets (Mustela putorius furo) weighing 0.75 to 1.0 kg were housed in groups of 2 or 3 animals per virus cohort. Before infection, subjects were anesthetized with 5% isoflurane and had transponder chips (Bio Medic Data Systems, Seaford, DE) implanted subcutaneously for animal identification and temperature monitoring. For the challenge and procedures, animals were anesthetized with a ketamine-acepromazine-xylazine (KAX) cocktail and were inoculated intranasally (i.n.) with ∼5,000 PFU of rNiVM-wt, rNiVM-Cko, or rNiVM-CkoWko in 0.5 ml of 10% FBS–Hanks' balanced salt solution (HBSS; Gibco). Animals were anesthetized for clinical examination, respiration quality assessment, and blood collection on days 0, 3, 6, 15, and 35 p.i. or at the terminal endpoint. After challenge, animals were assessed daily for weight and temperature and were scored on a scale of 0 to 12 for clinical observations based on coat appearance, social behavior, and provoked behavior; animals scoring 9 or higher were euthanized per IACUC protocol.
rNiVM serum neutralization assays.
Fifty percent neutralization titers (PRNT50s) were determined using a conventional serum neutralization assay. Briefly, sera were serially diluted 2-fold and were incubated with ∼100 PFU of rNiVM-wt for 1 h at 37°C. Virus and antibodies were then added to individual wells of 6-well plates of confluent Vero cell monolayers in duplicate. Plates were stained with neutral red 2 days after infection, and plaques were counted 24 h after staining. The PRNT50 was determined as the serum dilution at which there was a 50% reduction in plaque counts from that in control wells.
Collection and processing of specimens from rNiVM-infected ferrets.
Blood was collected and was placed in MiniCollect EDTA tubes or serum tubes (Greiner Bio-One, Monroe, NC). Immediately following sampling, 100 μl of blood was added to 600 μl of AVL viral lysis buffer with carrier RNA (Qiagen) for RNA extraction. For tissue sample processing, approximately 100 mg of tissue was stored in 1 ml RNAlater (Qiagen) for 96 h to stabilize RNA. RNAlater was completely removed, and tissues were homogenized in 600 μl RLT buffer (Qiagen) in a 2-ml cryovial using a tissue lyser (Qiagen) and 1.4-mm ceramic beads (Precellys; Bertin Corp., Saint-Quentin-en-Yvelines Cedex, France). The tissues sampled included the right lung (upper, middle, and lower lobes), left lung (upper, middle, and lower lobes), liver, spleen, kidney, adrenal gland, pancreas, and brain (frontal cortex). All blood samples were inactivated in AVL viral lysis buffer with carrier RNA, and tissue samples were homogenized and inactivated in RLT buffer prior to removal from the BSL-4 laboratory. Subsequently, RNA was isolated from blood and swabs using the QIAamp viral RNA kit (Qiagen), and from tissues using the RNeasy minikit (Qiagen), according to the manufacturer's instructions supplied with each kit.
Hematology and serum biochemistry.
Blood was collected on days 0, 3, 6, 15, and 35 p.i. or at the terminal endpoint for all animals. Total white blood cell counts, white blood cell differentials, red blood cell counts, platelet counts, hematocrit values, total hemoglobin concentrations, mean cell volumes, mean corpuscular volumes, and mean corpuscular hemoglobin concentrations were analyzed for blood collected in MiniCollect EDTA tubes (Greiner Bio-One) using a Hemavet HV950FS instrument according to the manufacturer's instructions (Drew Scientific, Oxford, CT). Serum was centrifuged at 2,000 rpm for 10 min, and blood chemistry was analyzed using a VetScan classic analyzer and comprehensive diagnostic profile rotors measuring albumin (ALB), amylase, alanine aminotransferase (ALT), alkaline phosphatase (ALP), calcium, glucose, total protein, total bilirubin (TBIL), blood urea nitrogen (BUN), creatinine (CRE), phosphorus, sodium, and total protein (Abaxis, Union City, CA). All blood and serum samples were processed and analyzed immediately after collection.
Histopathology and IHC.
Necropsies were performed on all subjects. Tissue samples of all major organs were collected for histopathologic and immunohistochemical (IHC) examination and were immersion-fixed in 10% neutral buffered formalin for at least 21 days in BSL-4 containment. Subsequently, formalin was changed; specimens were removed from BSL-4 containment, processed in BSL-2 containment by conventional methods, embedded in paraffin, and sectioned at a thickness of 5 μm as described previously (25). Briefly, for IHC, specific anti-NiV immunoreactivity was detected using a rabbit primary antibody against NiV N protein (kindly provided by Christopher Broder) at a 1:5,000 dilution for 30 min. The tissue sections were processed for immunohistochemistry using the Dako Autostainer (Dako, Carpinteria, CA). The secondary antibody used was biotinylated goat anti-rabbit IgG (Vector Laboratories, Burlingame, CA) at 1:200 for 30 min, followed by Dako LSAB2 (labeled streptavidin-biotin 2) conjugated to HRP for 15 min. Slides were developed with Dako DAB (diaminobenzidine) chromogen for 5 min and were counterstained with hematoxylin for 1 min. Nonimmune rabbit IgG was used as a negative staining control.
Detection of rNiVM loads.
RNA was isolated from blood or tissues and was analyzed by quantitative real-time PCR (qRT-PCR) using primers and a probe targeting the N gene and the intergenic region between N and P of NiV. The probe used here was 6-carboxyfluorescein (6FAM)–5′ CGT CAC ACA TCA GCT CTG ACG A 3′–6-carboxytetramethylrhodamine (TAMRA) (Life Technologies, Carlsbad, CA). This strategy using the intergenic region allows for genome and antigenome detection only, without detection of contaminating viral mRNA. rNiVM RNA was detected using the CFX96 detection system (Bio-Rad) in One-Step probe qRT-PCR kits (Qiagen) with the following cycle conditions: 50°C for 10 min, 95°C for 10 s, and 40 cycles of 95°C for 10 s and 59°C for 30 s. Threshold cycle (CT) values representing rNiV genomes were analyzed with CFX Manager software, and data are expressed as genome equivalents (GEq). To create the GEq standard, RNA was extracted from NiV challenge stocks and was quantified using a NanoDrop 2000 system (Thermo Scientific), and the number of NiV genomes was calculated using Avogadro's number and the molecular weight of the NiV genome. Virus titration was performed by plaque assays with Vero cells from all blood and tissue samples. Briefly, increasing 10-fold dilutions of the samples were adsorbed to Vero cell monolayers in duplicate wells (200 μl); the limit of detection was 25 PFU/ml.
RESULTS
rNiVM recovery and in vitro characterization.
rNiVM-wt, rNiVM-Wko, and rNiVM-Vko were recovered previously through reverse genetics (16), while rNiVM-Cko, rNiVM-CkoWko, and rNiVM-CkoVko mutants were successfully recovered in the present study using the same methods (Fig. 1A, B, and C). Western blot analysis of infected Vero cell lysates demonstrated that the C protein was not expressed by rNiVM-Cko; neither the C nor the W protein was expressed by rNiVM-CkoWko; and neither the C nor the V protein was expressed by rNiVM-CkoVko (Fig. 1D).
Multicycle growth kinetics were determined for each rNiVM mutant in Vero cells (Fig. 2A) and HEK 293T cells (Fig. 2B). The growth curves and peak titers were similar for the rNiVM-Cko, rNiVM-CkoWko, and rNiVM-CkoVko mutants, although rNiVM-CkoWko and rNiVM-CkoVko grew to slightly lower titers than rNiVM-Cko early in the time course. All mutants grew to significantly lower titers (1.0 to 1.5 log units) than rNiVM-wt. This finding is similar to results reported previously for other rNiVM mutants lacking C expression (29, 39, 41, 42). To investigate whether the C and W proteins were important for overcoming the innate immune response, multicycle growth kinetics were assessed in Vero (Fig. 2A) and HEK 293T (Fig. 2B) cells that had been stimulated with 1,000 U/ml of Universal IFN-α for 12 h prior to infection. The rNiVM-Cko and rNiVM-CkoWko mutants grew to similar titers, which were lower than those of rNiVM-wt; all three mutants grew to titers moderately lower (0.25 to 0.75 log unit) than those in cells that had not been pretreated with IFN-α. rNiVM-CkoVko grew to lower titers than rNiVM-Cko, as observed previously for rNiVM-Vko compared to rNiVM-wt (16). To determine if a lack of C expression led to lower titers in ferret cells, multicycle growth kinetics were also determined for each rNiVM mutant, including rNiVM-Wko and rNiVM-Vko, in MPF cells (Fig. 2C), and lack of C expression did lead to lower titers, although not as drastically as in Vero and 293T cells until 72 h p.i.
FIG 2.
In vitro growth kinetics of rNiVM in the Vero, 293T, and MPF cell lines. Shown are the growth kinetics in Vero (A), 293T (B), or MPF (C) cells that either were pretreated with IFN-α for 12 h (light colors) or were not pretreated (dark colors). Error bars show standard deviations. LOD, limit of detection (25 PFU/ml). ANOVA was carried out with Dunnett's multiple-comparison test (n = 4). *, P < 0.05; **, P < 0.01; ***, P < 0.001 for comparisons of data on the indicated bars.
rNiVM-infected primary human microvascular endothelial cells.
Endothelial cells in the lung are thought to be early targets for NiV infection (2); therefore, primary human lung microvascular endothelial cells were infected with the rNiVM mutants at a low MOI of 0.01 in order to determine the multicycle growth kinetics. No virus was detectable in supernatants from infected human pulmonary microvascular endothelial cells (HPMECs) with any mutant lacking C expression, a finding similar to those at most time points for the previously reported rNiVM-Vko mutant (16) either treated with 1,000 U/ml of Universal IFN-α prior to infection or not pretreated.
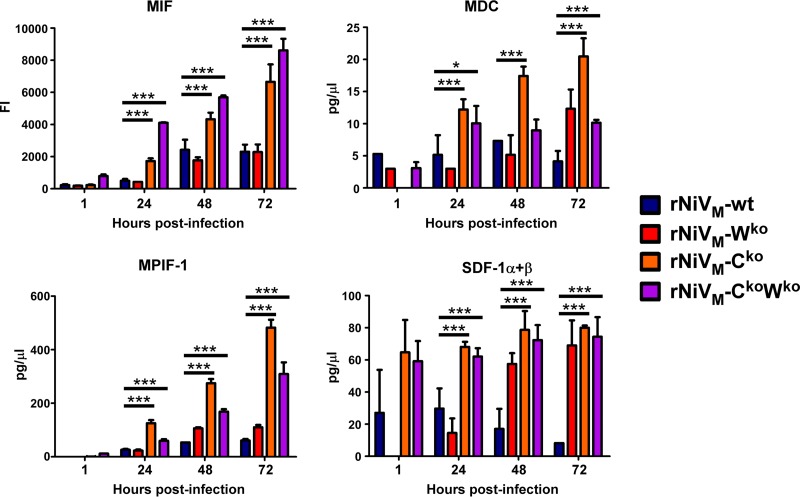
To examine the chemokine/cytokine response after initial target cell infection, supernatants from infected HPMECs were used to quantify the levels of 42 chemokines/cytokines by a Bio-Plex assay or ELISA. Overall, four chemokines in supernatants from mutant-infected cells exhibited levels elevated over the baseline and above those in supernatants from rNiVM-wt-infected cells (Fig. 3). These four chemokines, macrophage migration inhibitory factor (MIF), macrophage-derived chemokine (MDC), myeloid progenitor inhibitory factor 1 (MPIF-1), and stromal cell-derived factor 1 (SDF-1), are noted for their roles in recruiting macrophages, monocytes, dendritic cells, natural killer cells, and/or lymphocytes through chemotactic mechanisms (45).
FIG 3.
Selected chemokine/cytokine levels in supernatants of infected HPMECs. Inflammatory chemokine levels in HPMECs infected with rNiVM-wt (blue), rNiVM-Wko (red), rNiVM-Cko (orange), or rNiVM-CkoWko (purple) are shown. Error bars represent standard deviations. ANOVA was carried out with Dunnett's multiple-comparison test (n = 4). Asterisks indicate significant differences (*, P < 0.05; **, P < 0.01; ***, P < 0.001) from values for rNiVM-wt. FI, fluorescence intensity (in arbitrary units); MIF, macrophage migration inhibitory factor; MDC, macrophage-derived chemokine; MPIF-1, myeloid progenitor inhibitory factor 1; SDF-1, stromal cell-derived factor 1.
Clinical disease in ferrets infected with the Cko or CkoWko mutant.
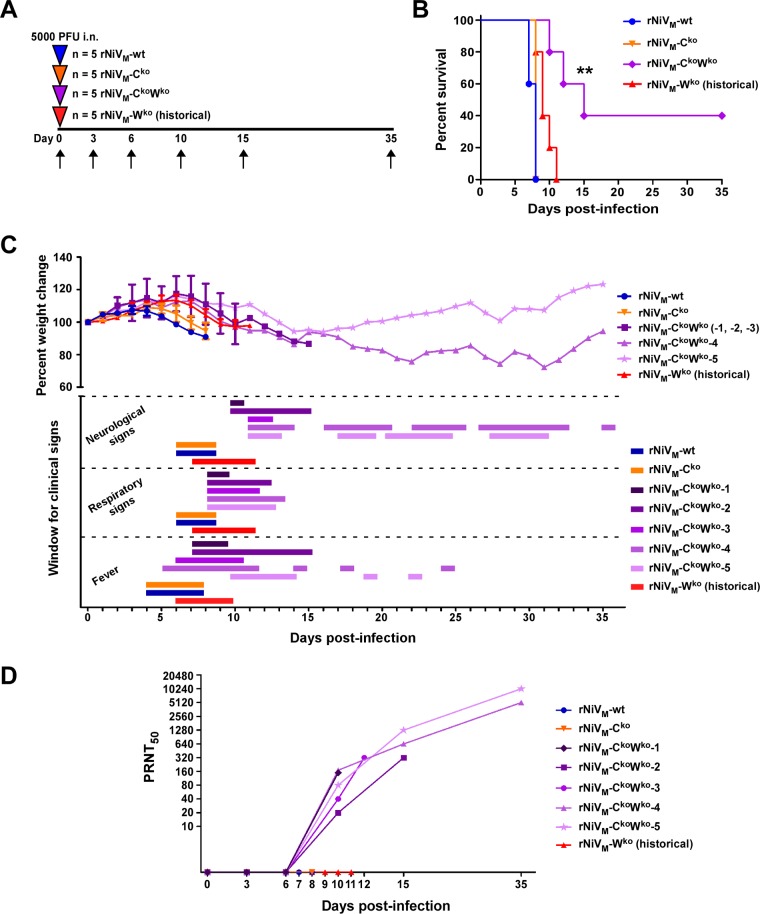
Three cohorts of 5 ferrets each were challenged intranasally (i.n.) with ∼5,000 PFU of rNiVM-wt, rNiVM-Cko, or rNiVM-CkoWko. After the challenge, animal weight, temperature, and clinical score were assessed daily, with blood drawn on days 3, 6, 10, and 15 and on terminal days (Fig. 4A).
FIG 4.
Clinical disease in ferrets after experimental infection with rNiVM. (A) Flow chart showing the day of infection (arrowheads) and days of samples collection (arrows). (B) Kaplan-Meier survival curve for ferrets infected with rNiVM-wt (blue circles), rNiVM-Cko (orange inverted triangles), rNiVM-CkoWko (purple diamonds), or rNiVM-Wko (red triangles). All data for rNiVM-Wko-infected animals (labeled “historical”) are from a previously published study (16). A log rank (Mantel-Cox) test was carried out (n, 5 for all rNiVM ferret cohorts). Asterisks indicate significant differences (**, P < 0.01) from the rNiVM-wt and rNiVM-Cko curves. (C) (Top) Changes in weight for animals from the rNiVM-wt (blue circles) or rNiVM-Cko (inverted orange triangles) cohort, rNiVM-CkoWko cohort animals 1, 2, and 3 (dark purple squares), rNiVM-CkoWko cohort animal 4 (medium purple triangles), rNiVM-CkoWko cohort animal 5 (light purple stars), and rNiVM-Wko cohort animals (red triangles). Error bars show standard deviations. (Bottom) Windows for neurological signs, respiratory signs, and fever. (D) Neutralizing antibody titers for ferret cohorts. Results for each animal in the rNiVM-CkoWko cohort are shown individually.
All animals in the rNiVM-wt cohort succumbed to rNiVM-mediated disease on days 7 to 8 p.i. (Fig. 4B, blue) with fever, severe respiratory disease, and mild to moderate neurological signs (Table 1). Similarly, all animals in the rNiVM-Cko cohort succumbed to disease at different points on day 8 p.i. (Fig. 4B, orange) with fever, mild respiratory disease, and moderate neurological signs (Table 1). All animals in the rNiVM-CkoWko cohort developed fever, mild respiratory signs that resolved after a few days, and neurological signs. In three of these animals (rNiVM-CkoWko-1, -2, and -3), the neurological signs were very severe, including ataxia, myoclonus, seizures, and paralysis that progressed in a consistent manner. The other two animals in the rNiVM-CkoWko cohort (rNiVM-CkoWko-4 and -5) also developed motor deficits, including ataxia, myoclonus, and tremors, but did not suffer seizures or paralysis. Over the remainder of the study, the presence of these neurological signs undulated, with periods when the ferrets showed no motor deficits, gained weight, and had minimal clinical scores, followed by periods of renewed neurological signs, weight loss, higher clinical scores, and recurrent fever (Fig. 4C, purple; Table 1). These two animals both survived to day 35 of the study, although they still had neurological sequelae, including apparent visual deficits, aggressive behavioral change in one animal (rNiVM-CkoWko-4), and undulating periods of clinical signs. Clinical signs observed in animals from all cohorts included depression, lethargy, ocular and nasal discharge, sneezing, rales, ataxia, tremors, and myoclonus (Table 1).
TABLE 1.
Clinical disease in ferrets after experimental infection with rNiVM
| Ferret no. | Clinical outcome,a day p.i. | Respb | Neuroc | Hemd | Days p.i. on which fever occurred | Clinical disease |
|---|---|---|---|---|---|---|
| rNiVM-wt-3 | Suc., 8 | + | ++ | − | 5–6 | Thrombocytopenia (day 6), lymphopenia (day 6), hypoalbuminemia (day 6), hyperglycemia (day 6), depression (days 5–7), lethargy (days 5–7), inappetence (days 6–7), ocular and nasal discharge (days 6–7), ataxia (day 7), hindlimb myoclonus (day 7) |
| rNiVM-wt-4 | Suc., 7 | + | ++ | + | 4–6 | Thrombocytopenia (days 6–7), lymphopenia (days 6–7), hypoalbuminemia (days 6–7), >3-fold increase in BUN (day 7), hyperglycemia (day 7), depression (days 6–7), lethargy (days 5–7), inappetence (days 6–7), ocular and nasal discharge (days 6–7), nasal/oral frothing (day 7), facial edema (day 7), ataxia (days 6–7), myoclonus (day 7), violent tremors (day 7), hypothermia (day 7) |
| rNiVM-wt-5 | Suc., 8 | + | + | + | 4–7 | Thrombocytopenia (days 6, 8), lymphopenia (day 6), hypoalbuminemia (days 6, 8), >3-fold increase in BUN (day 8), depression (days 5–7), lethargy (days 5–7), inappetence (days 6–8), dehydration (day 8), rales (days 6–8), ocular, nasal, and oral discharge (day 6), ataxia (days 6–8), severe hypothermia (day 8) |
| rNiVM-wt-6 | Suc., 7 | + | ++ | − | 4–6 | Thrombocytopenia (days 6–7), hypoalbuminemia (day 7), hyperglycemia (day 7), depression (days 6–7), lethargy (days 6–7), inappetence (day 7), ocular and nasal discharge (days 6–7), myoclonus (day 7), ataxia (day 7) |
| rNiVM-wt-7 | Suc., 8 | + | + | + | 4–6 | Thrombocytopenia (days 6, 8), lymphopenia (day 8), hypoalbuminemia (days 6, 8), >3-fold increase in BUN (day 8), depression (days 6–8), lethargy (days 6–8), inappetence (days 7–8), sneezing (days 7–8), nasal discharge (days 6–8), rales (days 6–8), ataxia (days 7–8), obtundation (day 8), hypothermia (day 8), loss of >10% of body weight |
| rNiVM-Cko-1 | Suc., 8 | + | + | + | 5–7 | Thrombocytopenia (days 6, 8), lymphopenia (days 3, 6), hypoalbuminemia (day 8), hyperglycemia (day 8), depression (days 6–8), lethargy (days 6–8), sneezing (day 7), ataxia (day 8), hypothermia (day 8) |
| rNiVM-Cko-2 | Suc., 8 | + | ++ | − | 5–7 | Thrombocytopenia (days 6, 8), lymphopenia (days 6, 8), hypoalbuminemia (day 8), hyperglycemia (day 8), depression (days 6–8), lethargy (days 6–8), inappetence (days 7–8), sneezing (day 7), rales (day 7), ataxia (days 7–8), myoclonus (day 8) |
| rNiVM-Cko-3 | Suc., 8 | + | ++ | + | 4–7 | Thrombocytopenia (day 8), lymphopenia (days 6, 8), hypoalbuminemia (days 6, 8), >3-fold increase in BUN (day 8), hyperglycemia (day 8), depression (days 6–8), lethargy (days 6–8), sneezing (day 7), ocular and nasal discharge (days 7–8), myoclonus (day 8), hypothermia (day 8) |
| rNiVM-Cko-4 | Suc., 8 | + | ++ | + | 6–7 | Thrombocytopenia (day 6), lymphopenia (day 6), hypoalbuminemia (day 8), >3-fold increase in BUN (day 8), hyperglycemia (day 8), depression (days 6–8), lethargy (days 7–8), sneezing (days 7–8), nasal discharge (day 7), rales (day 8), severe ataxia (day 8), myoclonus (day 8) |
| rNiVM-Cko-5 | Suc., 8 | + | ++ | + | 5–6 | Thrombocytopenia (days 6, 8), lymphopenia (days 3, 6, 8), hypoalbuminemia (days 6, 8), >3-fold increase in BUN (day 8), depression (days 6–8), lethargy (days 7–8), sneezing (days 7–8), nasal discharge (day 7), myoclonus (day 8), hypothermia (day 8), loss of >10% of body weight |
| rNiVM-CkoWko-1 | Suc., 10 | + | +++ | − | 7–9 | Lymphopenia (days 6, 10), hyperglycemia (day 10), depression (days 8–10), lethargy (days 8–10), sneezing (days 8–9), nasal discharge (days 8–9), rales (day 9), progressive hindlimb myoclonus and paralysis (day 10), severe tremors (day 10), seizures (day 10), loss of >10% of body weight |
| rNiVM-CkoWko -2 | Suc., 15 | + | +++ | − | 7–15 | Thrombocytopenia (day 15), hypoalbuminemia (day 10), depression (days 8–15), lethargy (days 8–15), sneezing (days 8–12), ocular and nasal discharge (days 8–9, 11), rales (day 9), facial edema (days 10–11), dilated pupils (days 10–12), ataxia (days 14–15), progressive hindlimb/forelimb myoclonus and paralysis (days 13–15), facial myoclonus (day 15), seizures (day 15), loss of >10% of body weight |
| rNiVM-CkoWko -3 | Suc., 12 | + | +++ | − | 6–10 | Thrombocytopenia (day 12), hypoalbuminemia (day 12), >3-fold increase in BUN (day 12), hyperglycemia (day 12), depression (days 8–12), lethargy (days 9–12), sneezing (days 8–11), ocular and nasal discharge (days 8–11), dilated pupils (days 11–12), progressive hindlimb/forelimb myoclonus and paralysis (days 11–12), obtundation (day 12), severe hypothermia (day 12) |
| rNiVM-CkoWko -4 | S.E., 35 | + | ++ | − | 5–11e | Recurrent fever (days 14, 17, 24), thrombocytopenia (day 10), hypoalbuminemia (day 10), depression (days 10–35), lethargy (days 8–35), sneezing (days 8–13), ocular and nasal discharge (days 8–13), dilated pupils (days 11–13, 19, 30, 35), ataxia (days 22–28, 32–35), facial myoclonus (days 16–19), periodic quadrupedal tremors (days 20, 27–33, 35), aggressive behavioral change with vocalization and visual deficit (days 16–35), temporary loss of >15% of body weight (days 18–33) |
| rNiVM-CkoWko -5 | S.E., 35 | + | ++ | − | 10–14e | Recurrent fever (days 19, 22), depression (days 8–31), lethargy (days 8–31), sneezing (days 8–10), ocular and nasal discharge (days 8–12), dilated pupils (days 11–13, 17–18, 30–31), ataxia (days 21–25), facial myoclonus (days 19–20), hindlimb myoclonus (day 19), periodic quadrupedal tremors (days 22–25, 28–31), visual deficit (days 20–35) |
Suc., succumbed to rNiVM-mediated disease; S.E., euthanized at study endpoint.
Resp, respiratory involvement. Results are expressed as the absence (−) or presence (+) of increased respiratory effort and/or rate.
Neuro, neurologic involvement. Results are expressed as the absence (−) or presence of minor (+), moderate (++), or severe (+++) neurological signs.
Hem, hemorrhage (extensive periorbital, facial, and ventral neck edema with subcutaneous hemorrhages).
Fever recurred after the initial fever resolved; see “Clinical disease” column for details.
Clinical biochemistry and hematological analyses were performed on all blood samples. As the disease progressed, the findings for animals from all cohorts included thrombocytopenia, lymphopenia, hypoalbuminemia, >3-fold increases in blood urea nitrogen (BUN), and hyperglycemia. These were not observed as frequently, as consistently, or to the same degree for animals in the rNiVM-CkoWko cohort as for the other cohorts (Table 1).
Neutralizing antibody response.
To assess the humoral immune response, the amount of circulating neutralizing antibody was determined by a plaque reduction neutralization assay (PRNT). No significant neutralizing antibody was detected in any animals from the rNiVM-wt or rNiVM-Cko cohort, while detectable levels of neutralizing antibody were observed in all animals from the rNiVM-CkoWko cohort beginning at day 10 p.i. (Fig. 4D).
Gross pathology.
A necropsy was performed on each animal after it had succumbed to disease or at the study endpoint. Gross pathology revealed marked differences in the lung lesions among the three cohorts, with all animals (5/5) in the rNiVM-wt cohort displaying multifocal to coalescing hemorrhagic and necrotizing pneumonia (Fig. 5A). All animals (5/5) in the rNiVM-Cko cohort had multifocal pinpoint hemorrhagic and necrotizing pneumonia (Fig. 5B), though with considerably less severe gross lesions than those seen in the rNiVM-wt cohort. The rNiVM-CkoWko cohort showed inconsistent lesions; both survivors (2/2) showed no significant gross pulmonary lesions, and of the animals that succumbed to disease, one (rNiVM-CkoWko-3) showed significant multifocal to coalescing hemorrhagic and necrotizing pneumonia (1/3), while the others showed only a very few small points of hemorrhagic lesions (2/3) (Fig. 5C). The spleens of all animals in all three cohorts were enlarged and mottled, with multifocal white and dark red patches indicating splenomegaly and multifocal necrosis, respectively, although the spleens of the two survivors in the rNiVM-CkoWko cohort, when examined at the end of the study, were not as enlarged or mottled as those of the animals that succumbed. Some animals in the rNiVM-wt (2/5) and rNiVM-Cko (3/5) cohorts and one animal (1/5) in the rNiVM-CkoWko cohort (rNiVM-CkoWko-3) had mucosal hemorrhagic lesions in the urinary bladder.
FIG 5.
Gross pathology of lungs from rNiVM-infected ferrets. Images show representative gross pathology of lungs taken from ferrets infected with rNiVM-wt (A), rNiVM-Cko (B), or rNiVM-CkoWko (C). Multifocal to coalescing hemorrhage and necrosis of all lung lobes are seen in rNiVM-wt-infected ferrets (A), while much fewer and smaller hemorrhagic and necrotic foci are seen in rNiVM-Cko-infected ferrets (B), and very few, small, white or hemorrhagic foci are observed in rNiVM-CkoWko-infected ferrets (C).
Some ferrets in the rNiVM-wt cohort (2/5) had mild congestion of the meningeal blood vessels, while all ferrets (5/5) in the rNiVM-Cko cohort (Fig. 6A) and all ferrets in the rNiVM-CkoWko cohort that succumbed (3/3) (Fig. 6B) had marked congestion of the meningeal blood vessels. One of the survivors from the rNiVM-CkoWko cohort still had mild congestion of the meningeal blood vessels at the study endpoint, and the other survivor had poorly defined cerebral gyri and sulci, interpreted as edema, at the study endpoint (Fig. 6C). One ferret that succumbed to rNiVM-CkoWko infection also had blood pooled on the right lateral hemisphere, with a 1- to 2-mm-diameter raised focus within the neural parenchyma.
FIG 6.
Gross pathology of brains from rNiVM-infected ferrets. Images show representative gross pathology of brains taken from a ferret infected with rNiVM-Cko (A), a ferret that succumbed to infection with rNiVM-CkoWko (B), and a ferret that survived infection with rNiVM-CkoWko (C). Congestion of meningeal blood vessels was observed in ferrets infected with rNiVM-Cko (A) and in all ferrets infected with rNiVM-CkoWko (B) except for one of the survivors, which had poorly defined sulci and gyri of the brain, indicating that edema was still present at 35 days p.i. (C).
Histopathology and IHC.
Tissues were examined by hematoxylin-and-eosin (H&E) staining and by immunohistochemistry (IHC) using antibodies specific to the NiV N protein. Hepatic lesions for all animals in the rNiVM-wt (Fig. 7A) and rNiVM-Cko (Fig. 7E) cohorts included minimal to moderate hepatocellular degeneration/necrosis with minimal to mild vacuolar change, moderate congestion with occasional sinusoidal leukocytosis (neutrophilia), and moderate to severe periportal lymphoplasmacytic infiltrates. Strong immunolabeling for NiV antigen was present in all animals in the rNiVM-wt (Fig. 7B) and rNiVM-Cko (Fig. 7F) cohorts. Immunolabeling for NiV antigen was present in multifocal regions of the sinusoidal lining cells, a few scattered mononuclear cells within the sinusoids (Kupffer cells), the endothelia of medium- to large-caliber vessels, and scattered mononuclear inflammatory cells, which were largely centered near areas of necrosis. In the rNiVM-CkoWko cohort, no hepatocellular degeneration/necrosis was noted for any animals that succumbed to (Fig. 7I) or survived (Fig. 7M) infection; there was also no immunolabeling for NiV antigen in the livers of animals that succumbed to (Fig. 7J) or survived (Fig. 7N) infection.
FIG 7.
H&E and immunohistochemistry specimens of ferret liver and spleen. Shown are representative H&E-stained specimens (A, C, E, G, I, K, M, and O) and immunohistochemistry specimens labeled with a polyclonal rabbit antibody specific to NiV N protein (B, D, F, H, J, L, N, and P). Liver (A, B, E, F, I, J, M, and N) and spleen (C, D, G, H, K, L, O, and P) specimens were from representative ferrets infected with rNiVM-wt (A to D), rNiVM-Cko (E to H), or rNiVM-CkoWko (I to P) that succumbed to disease (I to L) or survived disease (M to P). White arrows indicate small areas of immunolabeling. Magnification, ×20.
Splenic lesions for all animals in the rNiVM-wt (Fig. 7C) and rNiVM-Cko (Fig. 7G) cohorts included moderate to marked diffuse depletion of lymphoid follicles, syncytial cell formation, hemorrhage, and fibrin deposition of the white pulp with accumulation of viable neutrophils, degenerative neutrophils, and cellular debris. Strong immunolabeling for NiV antigen was present in all animals in the rNiVM-wt (Fig. 7D) and rNiVM-Cko (Fig. 7H) cohorts. Immunolabeling for NiV was present in scattered mononuclear cells (largely centered on lymphoid follicles/germinal center remnants), syncytial cells, and scattered endothelial cells. The splenic architecture appeared mildly disturbed in spleens from the animals in the rNiVM-CkoWko cohort that succumbed, with lymphocytic proliferation and, in some of the animals (2/3), a few areas of minimal necrosis and germinal center disorganization (Fig. 7K) associated with the presence of minimal immunolabeling of the endothelium (Fig. 7L, white arrows). No splenic histopathologic lesions were noted in the survivors of the rNiVM-CkoWko cohort (Fig. 7O); splenic architecture appeared undisturbed; and no immunolabeling for NiV antigen was noted (Fig. 7P). Of note, the spleens from the rNiVM-Wko cohort described previously (16) looked very similar to those of the rNiVM-wt and rNiVM-Cko cohorts described here. These are all distinct from the phenotype observed for the rNiVM-CkoWko cohort.
Pulmonary lesions in all lung lobes of animals in the rNiVM-wt (Fig. 8A) cohort and, to a lesser extent, in those of all animals in the rNiVM-Cko (Fig. 8E) cohort included interstitial pneumonia with nodular inflammation and necrosis of the alveolar septae near the terminal bronchioles and occasional, small syncytial cell formation (Fig. 8A, inset) of endothelial and/or respiratory epithelial cells. Strong immunolabeling for NiV antigen was present in scattered mononuclear, endothelial, and respiratory epithelial cells in the rNiVM-wt (Fig. 8B) cohort. Strong immunolabeling was also observed in the rNiVM-Cko (Fig. 8F) cohort, although it was almost entirely localized to areas of nodular inflammation that appeared more discrete and smaller than in the rNiVM-wt cohort. More edema and hemorrhage were noted throughout the lung lobes from the rNiVM-wt cohort. Some of the animals (2/3) in the rNiVM-CkoWko cohort that succumbed (Fig. 8I) had rare areas of minimal interstitial pneumonia and very small inflammatory nodules with minimal or no immunolabeling for NiV antigen (Fig. 8J); in one of these animals, rNiVM-CkoWko-3, hemorrhage and edema were associated with these inflammatory nodules.
FIG 8.
H&E and immunohistochemistry specimens of ferret lung and brain. Representative H&E-stained specimens (A, C, E, G, I, K, M, and O) and immunohistochemistry specimens labeled with a polyclonal rabbit antibody specific to NiV N protein (B, D, F, H, J, L, N, and P) are shown. Lung (A, B, E, F, I, J, M, and N) and brain (C, D, G, H, K, L, O, and P) specimens were from representative ferrets infected with rNiVM-wt (A to D), rNiVM-Cko (E to H), or rNiVM-CkoWko (I to P) that succumbed to disease (I to L) or survived disease (M to P). The inset in panel A shows syncytial cell formation at a higher magnification (×60). Magnifications, ×10 (lung) and ×60 (brain).
No lesions were noted upon routine H&E staining of the brains of all animals in the rNiVM-wt (Fig. 8C), NiVM-Cko (Fig. 8G), and rNiVM-CkoWko (Fig. 8K and O) cohorts. However, strong immunolabeling for NiV antigen was present in the endothelia of small-caliber vessels within multiple sections of the brain (cerebrum, brainstem, choroid plexus, and meninges) in all animals of the rNiVM-wt (Fig. 8D) cohort. Congestion of vessels and hemorrhage were noted expanding the meninges in all animals in the rNiVM-Cko cohort and in those in the rNiVM-CkoWko cohort that succumbed. Some animals in the rNiVM-Cko cohort (Fig. 8H) and those in the rNiVM-CkoWko cohort that succumbed (Fig. 8L) had multifocal areas with strong immunolabeling for NiV antigen within the endothelium and neurons in the cerebrum, cerebellum/brainstem, and/or hippocampus, but those that survived did not (Fig. 8P). Although the blood-brain-barrier (BBB) consists of the entire interface of the neural parenchyma and the meninges and all blood vessels in the brain, the choroid plexus is known to be a more permissive region of the BBB. The choroid plexus showed labeling in mononuclear cells and some endothelial cells in some of the animals that succumbed from all three cohorts; however, no labeling in the neurons adjacent to the choroid plexus, which would have suggested an obvious breach of the BBB at the choroid plexus, was seen.
Viral loads.
To assess viral loads in animals, qRT-PCR was used to quantify the viral genomes present in blood (Fig. 9A). All animals in the rNiVM-wt and rNiVM-Cko cohorts had detectable levels of viral genome on day 6 p.i. which remained detectable until they succumbed to disease. Notably, only one animal in the rNiVM-CkoWko cohort (rNiVM-CkoWko-1) had detectable levels of viral genome in the blood; this was at day 10 p.i., the day on which this animal succumbed to disease.
FIG 9.
Viral loads in rNiVM-infected ferrets. (A and B) Viral loads in ferrets, expressed as genome equivalents per milliliter of blood (A) or per gram of tissue (B), were detected by qRT-PCR. (A) Asterisks indicate that rNiVM was successfully isolated from whole-blood samples. The dagger marks a sample for which neither virus isolation nor qPCR data were available. (B) Hashed blue and hashed orange bars represent the averages for all animals in the rNiVM-wt and rNiVM-Cko cohorts, respectively. Error bars show standard deviations. For hashed bars, a total of 10 samples (2 replicates from each of 5 animals) were used; for all other bars, 2 replicates were used. RU, right upper; RM, right middle; RL, right lower; LU, left upper; LM, left middle; LL, left lower. (C) Concentrations of rNiVM (expressed as PFU per gram) isolated from tissues of ferrets after necropsy.
Viral loads were also measured in 10% (wt/vol) tissue homogenates taken at necropsy; RNA was extracted, and the viral genomes were detected and quantified by qRT-PCR (Fig. 9B). High levels of viral genomes were detected in all tissues assayed for all animals in the rNiVM-wt and rNiVM-Cko cohorts. The three animals in the rNiVM-CkoWko cohort that succumbed to disease also had detectable levels of viral genome in all tissues, although these were lower (typically 1 to 5 log units lower) than those observed in the rNiVM-wt and rNiVM-Cko cohorts, and the levels in the animal that succumbed on day 15 p.i (rNiVM-CkoWko-2) were 1 to 2 log units lower than those in the two animals that succumbed on day 10 (rNiVM-CkoWko-1) or day 12 (rNiVM-CkoWko-3) p.i. Of the survivors, rNiVM-CkoWko-5 had no detectable levels of viral genome in any tissues, and rNiVM-CkoWko-4 had a low level of viral genome detectable in the spleen and a large amount detectable in the brain. Virus isolation was attempted from PCR-positive samples of the liver, spleen, kidney, and adrenal gland, and virus was isolated from all PCR-positive samples from animals in the rNiVM-wt and rNiVM-Ckocohorts, except for some of the liver samples from the rNiVM-Cko cohort; however, no virus was isolated from any samples from the rNiVM-CkoWko cohort (Fig. 9C).
DISCUSSION
The role of the NiV C protein in viral pathogenesis has proved to be more enigmatic than those of the other P gene products. Our previous work demonstrated that the NiV V protein is a major determinant of pathogenesis in the ferret model and that the W protein contributes to the disease course, but not to the lethality, of NiV (16). To date, no studies have examined the role of the C protein in the ferret model; however, two studies have examined the contribution of the C protein in the hamster model (29, 41). Both studies demonstrated that rNiV mutants lacking C expression were attenuated in hamster infections. Together, they revealed that the C protein plays an important role in NiV pathogenesis in the hamster model and is responsible for suppressing inflammatory chemokines to the lungs that lead to necrosis and edema.
The results of our experiments show some distinct differences between rNiVM-Cko-infected ferrets and hamsters infected with similar rNiV mutants. Most notably, rNiVM-Cko was still 100% lethal in ferrets, with animals succumbing in the same time frame as rNiVM-wt-infected ferrets (Fig. 4B). Virus titers and genome levels in terminal blood and tissues did not differ substantially between the rNiVM-wt and rNiVM-Cko cohorts (Fig. 9). Also, like rNiVM-wt-infected ferrets, rNiVM-Cko-infected ferrets did not develop a neutralizing antibody response (Fig. 4D). The previous hamster study demonstrated that rNiVM-Cko-infected hamsters developed an antibody response by ELISA, but neutralization was not examined (41).
This is reminiscent of studies with related morbilliviruses, specifically measles virus (MeV) in the rhesus macaque model and canine distemper virus (CDV) in the ferret model. CDV is often used as a surrogate for studying MeV, since CDV causes a lethal, measles-like infection in ferrets, in contrast to the nonlethal model of MeV in rhesus macaques. Morbilliviruses produce V and C proteins from the P gene, although they do not produce a W protein. In the nonlethal rhesus macaque model of MeV infection, rMeV-Vko and -Cko mutants (46) were both attenuated compared to rMeV-wt. In the lethal ferret model of CDV infection, an rCDV-Vko mutant was attenuated in ferrets, causing only mild clinical disease; however, an rCDV-Cko mutant remained fully lethal (47).
One function of the MeV C protein is to promote the assembly and release of stable viral particles; large amounts of defective interfering viral genome RNA are formed in rMeV-Cko infection (48, 49), leading to lower titers of rMeV-Cko in vitro. This might also occur with rNiVM-Cko; certainly, lower titers are also observed for rNiVM-Cko in vitro, although what effect this might have in vivo is not yet clear. It is not clear if the morbillivirus C protein and the NiV C protein have the same targets, so we cannot say if there is a specific, common mechanism underlying the lesser role of the C protein in the ferret models of rCDV and rNiVM infection compared to those in the hamster model. It would therefore be of great interest to observe the effect of rNiVM-Cko infection in the AGM model of NiV disease. In an effort to determine if this effect was due to an intrinsic ability of the mutants to grow differently in ferret cells, we examined virus growth kinetics in AGM Vero cells, human 293T cells, and ferret brain MPF cells (Fig. 2). As in previous reports (29, 39, 41, 42), rNiV mutants containing the Cko mutation grew to lower titers than rNiVM-wt in Vero or 293T cells. We also observed this in MPF cells, although the difference was smaller in MPF cells at time points before 72 h p.i. Although rNiVM-Cko was still 100% lethal in ferrets, there were some minor differences in disease course and pathogenesis from the rNiVM-wt cohort, including a reduction in the severity of lesions in the lungs and accompanying respiratory signs, but the neurological signs were as severe as those of the rNiVM-wt cohort. This pattern was reminiscent of the rNiVM-Wko-infected ferret cohort described previously (16), but without the delayed time to death and the subsequent severe neurological signs.
Due to the observation that infection of ferrets with either rNiVM-Cko or rNiVM-Wko altered the disease course in similar ways while remaining 100% lethal, we were interested in examining the effects of rNiVM-CkoWko infection in order to further elucidate the roles of the C and W proteins. Surprisingly, the disease course was greatly altered in the rNiVM-CkoWko cohort, with only very mild respiratory signs, milder even than those for the rNiVM-Wko or rNiVM-Cko cohort. These signs quickly decreased and were completely resolved in some of the ferrets within a few days of onset (Fig. 5C; Table 1). Moderate neurological disease set in for all five ferrets and progressed to severe neurological disease in three of the ferrets, including tremors, myoclonus, seizures, and progressive paralysis. These three ferrets succumbed; they exhibited similar disease courses, beginning with paralysis of one hindlimb, followed by paralysis of the second hindlimb within 12 to 24 h and paralysis of one or both forelimbs within the next 24 h, leading to humane euthanasia. However, these animals survived significantly longer than those in the rNiVM-wt cohort (Fig. 4B).
The two survivors had similar clinical signs but never developed the progressive paralysis. Over time, the neurological signs diminished somewhat, and there were periods when no motor signs could be observed, but these would return a day or two later; this occurred multiple times in an undulating pattern. Although this study ended 35 days p.i., these sequelae are similar to the persistent gait disorders described for human survivors (1, 5, 50). The two surviving ferrets also exhibited dilated pupils and apparent visual deficits, possibly caused by oculomotor nerve palsy (cranial nerve III), which has been described as one of the neurological sequelae of some human survivors of NiV encephalitis (5). This lesion could be caused by direct viral infection, an inflammatory response, or increased intracranial pressure; both of these animals still had mild congestion and/or diffuse intracranial edema at the study endpoint.
One of the survivors, rNiVM-CkoWko-4, developed a stark behavioral change, shifting from a very calm and docile demeanor to extremely aggressive behavior. Similar persistent behavioral disturbances, including increased irritability and violent outbursts, have been reported frequently for human survivors of NiV encephalitis (5, 50).
The differences in gross pathology and histopathology among the three ferrets in the rNiVM-CkoWko cohort that succumbed and the ferrets in the rNiVM-wt, rNiVM-Cko, and previously reported rNiVM-Wko cohorts were striking (16). Two of the three rNiVM-CkoWko-infected ferrets had only a few, very small lesions and inflammatory nodules in the lungs associated with little or no NiV antigen (Fig. 5C and 7I and J), while the third had more gross hemorrhaging and serosanguineous fluid around the lung with larger hemorrhagic lesions, although these were still associated with only limited viral antigen. None of these three ferrets from the rNiVM-CkoWko cohort had necrosis of the splenic germinal centers, which was observed in ferrets in the rNiVM-wt, rNiVM-Cko (Fig. 7), and previously reported rNiVM-Wko cohorts, although the splenic architecture was altered in the three ferrets from the rNiVM-CkoWko cohort that succumbed, with occasional areas of necrosis. Because the splenic germinal centers remained intact in the rNiVM-CkoWko cohort, these ferrets were able to develop a neutralizing antibody response, unlike ferrets in the rNiVM-wt, rNiVM-Cko, and previously reported rNiVM-Wko cohorts. Although this antibody response may have played a role in the decreased amounts of NiV antigen, genome, and virus isolation in various organs (Fig. 9) and in the resolution of respiratory signs, it did not prevent the onset or progress of neurological signs. This observation has implications for the ability of therapeutics such as human monoclonal antibody m102.4 (51) to treat encephalitic cases of NiV infection.
These observations may shed some light on the mechanism of the neurological signs observed in NiV-mediated disease. From rabies virus, a distantly related human encephalitic virus in the order Mononegavirales, it is known that one of three possibilities can occur: (i) usually the BBB remains intact, leading to a lethal infection due to the absence of an immune response in the central nervous system (CNS) (52); (ii) rarely, immune effectors, including antibodies, transit the BBB and mediate a CNS immune response, leading to extensive immunopathology that contributes to the disease and clinical signs (52, 53); or (iii) very rarely, immune effectors transit the BBB and are able to clear the virus from the CNS without significant immunopathology (52). In this study, no signs of immunopathology in the CNS were detectable, and since the neurological signs persisted after the development of the neutralizing antibody response and viral antigen was detectable in the brains of the animals that succumbed, we can surmise that the virus was not cleared. Therefore, it is likely that the BBB remained largely intact in these animals and that NiV enters the CNS directly through the endothelium, through small disturbances in the BBB, or by hitchhiking on leukocytes (54), a scenario similar to that of human immunodeficiency virus (HIV) encephalitis (55), but without large-scale disruption of the BBB such as that seen in encephalitis due to several bacterial causes (56, 57).
It is also possible that small areas, possibly centered on areas of NiV-infected endothelium, may cause small breaches in the BBB, allowing limited entry of NiV without large-scale passage of inflammatory molecules or antibodies. This BBB gateway model has recently been suggested as a method for neuroinvasion by various viral agents (58, 59). This model suggests that nuclear factor κB (NF-κB) signaling through signal transducer and activator of transcription 3 (STAT3) is the key to opening this gate, and NF-κB interacts closely with the TLR/IKK/IRF pathways known to be affected by the NiV W and C proteins (36, 40). This may be one reason for the increased neurological signs observed in the rNiVM-Wko, rNiVM-CkoWko, and, to a lesser extent, rNiVM-Cko cohorts relative to the rNiVM-wt cohort, although delayed time to death may also have contributed in the rNiVM-Wko and rNiVM-CkoWko cohorts. Further studies are needed to better elucidate the mechanisms and timing of CNS invasion by NiV; the egress of NiV from infected kidney epithelial cells is predominantly from the apical side (60), but it is not known whether this holds true for brain endothelial cells. More-extensive, serial sacrifice studies could help identify the time course of NiV spread to various organs, including the CNS, and clarify what role the P gene products play in altering the time course of NiV spread through the various organs and to the CNS.
While our previous work identified the NiV V protein as the major determinant of virulence in the ferret model (16), it is noteworthy that rNiVM-CkoWko, which can still produce the V protein, is not 100% lethal, although all ferrets infected with rNiVM-CkoWko developed moderate to severe neurological disease with only limited respiratory disease. This suggests that the V protein is critical for infection in the initial target cells of the lung but is not sufficient to establish the severe respiratory component of NiV-mediated disease, because there is still CNS invasion and establishment of the neurological component of NiV-mediated disease. Further studies are needed to elucidate the initial target cells of NiV in vivo so as to ultimately define the roles that C, V, and W play in the establishment and progression of NiV infection.
In summary, the rNiVM ferret studies presented here and previously (16) demonstrate that, compared to the rNiVM-wt cohort, the rNiVM-Vko cohort had only very mild disease, with 100% surviving; the rNiVM-Wko cohort had decreased pulmonary disease, increased neurological disease, and a delayed time to death but 0% survival; the rNiVM-Cko cohort had decreased pulmonary disease but no change in the time to death and 0% survival; the rNiVM-CkoWko cohort had greatly decreased pulmonary disease but severe neurological disease, with 40% surviving. Although plasmid-based studies suggest that the W and C proteins inhibit various aspects of the innate immune viral recognition pathways (30, 36, 40), the current study demonstrates that neither the W nor the C protein plays a major role individually in NiV pathogenesis in the ferret model. The W and C proteins do appear to play complementary roles in the respiratory component of NiV-mediated disease but do not solely contribute to the lethality of NiV. These proteins are not necessary for neuroinvasion and may actually slow down or decrease the ability of NiV to invade the CNS. The C and W proteins likely either have a common target or have complementary targets or pathways in the host innate signaling response, leading to the progression of respiratory disease, since most rNiVM-CkoWko-infected ferrets had only mild respiratory signs and even fewer pulmonary pathological lesions than rNiVM-Wko- or rNiVM-Cko-infected ferrets but still had very severe, often fatal neurological disease. Alternatively, the decreased ability of the Cko rNiVM to form functional viral particles may serve as a complement to the mechanisms inhibited by the Wko mutation. These results are summarized in Fig. 10. Although it is likely that as yet unidentified targets and pathways are affected by the W and C proteins, one possibility for these complementary pathways might be the ability of the W protein to inhibit TLR3 signaling through IKKε and another unidentified target (36), while the C protein can inhibit TLR7/9 signaling through IKKα (40). Since the roles of C, V, and W have been examined in the ferret model, future work should focus on examining these innate pathways and other possible targets in the context of NiV infection through mutations in innate immune-modulating motifs, such as STAT1, STAT2, and MDA-5, for comparison with other paramyxoviruses (61, 62). Additionally, future work should focus on identifying the specific mechanisms of NiV neuroinvasion, and rNiVM-CkoWko should prove to be a useful tool for identifying these mechanisms.
FIG 10.
Model of the roles of the NiV C and W proteins in ferret pathogenesis. (A) rNiVM-wt spreads unhindered in early target lung endothelial cells, leading to extensive lung injury (Fig. 5A), followed by spread to the spleen, causing germinal center necrosis (Fig. 7C), leading to a lack of neutralizing antibody response (Fig. 4D). The virus also spreads to the endothelium of the brain (Fig. 8D), and mild to moderate neurological signs develop before the ferret succumbs to severe respiratory disease. (B) rNiVM-Cko shows sequestered viral spread in distinctive inflammatory nodules of the lung (Fig. 5B and 8F), thus causing milder respiratory signs. rNiVM-Cko is still able to spread to the spleen, causing germinal center necrosis (Fig. 7G) and leading to a lack of neutralizing antibody response (Fig. 4D). The virus also spreads to the brain endothelium and, possibly due to altered cytokine production leading to BBB permeability, to neurons as well (Fig. 8H), leading to severe neurological signs and causing the animals to succumb to neurological disease. (C) rNiVM-CkoWko is unable to spread efficiently or cause injury in the lungs (Fig. 5C), leading to only temporary, mild respiratory disease. Although there is limited spread to the spleen (Fig. 7L), splenic germinal centers remain intact (Fig. 7K), and a potent neutralizing antibody response develops (Fig. 4D). The virus spreads efficiently to the brain (Fig. 8L), leading to severe neurological disease with a 60% fatality rate, and the survivors develop neurological sequelae similar to those of human survivors.
While research for developing vaccines and therapeutics for NiV should continue, in an outbreak scenario many NiV-infected patients will need to be treated at various points in the disease process. Intensive supportive therapy, including mechanical ventilation, can be used to help patients survive the respiratory component of NiV infection. However, these patients often succumb to neurological disease or develop long-term sequelae. Various therapeutic options need to be examined to prevent lethal neurological disease and the development of long-term sequelae. Since intensive supportive care and mechanical ventilation of animals in a BSL-4 laboratory are not feasible, the fact that rNiVM-CkoWko-infected ferrets develop only limited respiratory disease while retaining the neurological component of NiV disease allows this model to potentially serve as a surrogate model for intensive supportive care in a BSL-4 scenario. The use of rNiVM-CkoWko in the ferret model can thus provide a platform for testing therapeutic interventions targeted at limiting neurological disease and sequelae.
ACKNOWLEDGMENTS
We thank Joan Geisbert and Courtney Williams for study support, the staff of the UTMB Animal Resources Center for animal care, and Kenneth Escobar, Kerry Graves, and Natalie Dobias for technical expertise in histology.
We declare that we have no competing interests.
This study was supported by the Department of Health and Human Services, National Institutes of Health, grants U19-AI082121 (to T.W.G.), U19-AI109945-01 (to C.F.B.), and UC7 AI094660 (for BSL-4 operations support of the Galveston National Laboratory).
B.A.S., C.F.B., T.W.G., and C.E.M. conceived and designed the in vitro work. B.A.S., T.W.G., and C.E.M. conceived and designed the ferret study. B.A.S. designed, cloned, recovered, characterized, and propagated the rNiV mutants used in this study. R.W.C. propagated the primary human endothelial cells, and B.A.S. and V.B. performed the remainder of the in vitro work. B.A.S., R.W.C., V.B., D.J.D, J.G., K.A.F., and C.E.M. performed infection studies, carried out clinical observations in the animal infection studies, and processed animal tissues and blood. B.A.S. and V.B. performed virus isolation, determined neutralizing antibody titers, and performed clinical pathology assays. K.A.F. provided veterinary pathology expertise and performed histologic and immunohistochemical analysis. K.N.A. performed qRT-PCR and the Bio-Plex procedure. B.A.S., R.W.C., K.A.F., V.B., K.N.A., C.F.B., T.W.G., and C.E.M. analyzed the data. B.A.S., C.F.B., T.W.G., and C.E.M. wrote the paper. All authors had access to all of the data and approved the final version of the paper. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the UTMB.
REFERENCES
- 1.Goh KJ, Tan CT, Chew NK, Tan PS, Kamarulzaman A, Sarji SA, Wong KT, Abdullah BJ, Chua KB, Lam SK. 2000. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N Engl J Med 342:1229–1235. doi: 10.1056/NEJM200004273421701. [DOI] [PubMed] [Google Scholar]
- 2.Wong KT, Shieh WJ, Kumar S, Norain K, Abdullah W, Guarner J, Goldsmith CS, Chua KB, Lam SK, Tan CT, Goh KJ, Chong HT, Jusoh R, Rollin PE, Ksiazek TG, Zaki SR. 2002. Nipah virus infection: pathology and pathogenesis of an emerging paramyxoviral zoonosis. Am J Pathol 161:2153–2167. doi: 10.1016/S0002-9440(10)64493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eaton BT, Broder CC, Middleton D, Wang LF. 2006. Hendra and Nipah viruses: different and dangerous. Nat Rev Microbiol 4:23–35. doi: 10.1038/nrmicro1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rockx B, Winegar R, Freiberg AN. 2012. Recent progress in henipavirus research: molecular biology, genetic diversity, animal models. Antiviral Res 95:135–149. doi: 10.1016/j.antiviral.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Sejvar JJ, Hossain J, Saha SK, Gurley ES, Banu S, Hamadani JD, Faiz MA, Siddiqui FM, Mohammad QD, Mollah AH, Uddin R, Alam R, Rahman R, Tan CT, Bellini W, Rota P, Breiman RF, Luby SP. 2007. Long-term neurological and functional outcome in Nipah virus infection. Ann Neurol 62:235–242. doi: 10.1002/ana.21178. [DOI] [PubMed] [Google Scholar]
- 6.Chua KB, Goh KJ, Wong KT, Kamarulzaman A, Tan PS, Ksiazek TG, Zaki SR, Paul G, Lam SK, Tan CT. 1999. Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. Lancet 354:1257–1259. doi: 10.1016/S0140-6736(99)04299-3. [DOI] [PubMed] [Google Scholar]
- 7.Arankalle VA, Bandyopadhyay BT, Ramdasi AY, Jadi R, Patil DR, Rahman M, Majumdar M, Banerjee PS, Hati AK, Goswami RP, Neogi DK, Mishra AC. 2011. Genomic characterization of Nipah virus, West Bengal, India. Emerg Infect Dis 17:907–909. doi: 10.3201/eid1705.100968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I, Niezgoda M, Rupprecht C, Bresee J, Breiman RF. 2004. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis 10:2082–2087. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, Ksiazek TG, Mishra A. 2006. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis 12:235–240. doi: 10.3201/eid1202.051247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harcourt BH, Lowe L, Tamin A, Liu X, Bankamp B, Bowden N, Rollin PE, Comer JA, Ksiazek TG, Hossain MJ, Gurley ES, Breiman RF, Bellini WJ, Rota PA. 2005. Genetic characterization of Nipah virus, Bangladesh, 2004. Emerg Infect Dis 11:1594–1597. doi: 10.3201/eid1110.050513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hossain MJ, Gurley ES, Montgomery JM, Bell M, Carroll DS, Hsu VP, Formenty P, Croisier A, Bertherat E, Faiz MA, Azad AK, Islam R, Molla MA, Ksiazek TG, Rota PA, Comer JA, Rollin PE, Luby SP, Breiman RF. 2008. Clinical presentation of Nipah virus infection in Bangladesh. Clin Infect Dis 46:977–984. doi: 10.1086/529147. [DOI] [PubMed] [Google Scholar]
- 12.Luby SP, Hossain MJ, Gurley ES, Ahmed BN, Banu S, Khan SU, Homaira N, Rota PA, Rollin PE, Comer JA, Kenah E, Ksiazek TG, Rahman M. 2009. Recurrent zoonotic transmission of Nipah virus into humans, Bangladesh, 2001–2007. Emerg Infect Dis 15:1229–1235. doi: 10.3201/eid1508.081237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ching PKG, de los Reyes VC, Sucaldito MN, Tayag E, Columna-Vingno AB, Malbas FF Jr, Bolo GC Jr, Sejvar JJ, Eagles D, Playford G, Dueger E, Kaku Y, Morikawa S, Kuroda M, Marsh GA, McCullough S, Foxwell AR. 2015. Outbreak of henipavirus infection, Philippines, 2014. Emerg Infect Dis doi: 10.3201/eid2102.141433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Georges-Courbot MC, Contamin H, Faure C, Loth P, Baize S, Leyssen P, Neyts J, Deubel V. 2006. Poly(I)-poly(C12U) but not ribavirin prevents death in a hamster model of Nipah virus infection. Antimicrob Agents Chemother 50:1768–1772. doi: 10.1128/AAC.50.5.1768-1772.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halpin K, Mungall BA. 2007. Recent progress in henipavirus research. Comp Immunol Microbiol Infect Dis 30:287–307. doi: 10.1016/j.cimid.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Satterfield BA, Cross RW, Fenton KA, Agans KN, Basler CF, Geisbert TW, Mire CE. 2015. The immunomodulating V and W proteins of Nipah virus determine disease course. Nat Commun 6:7483. doi: 10.1038/ncomms8483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Field H, Young P, Yob JM, Mills J, Hall L, Mackenzie J. 2001. The natural history of Hendra and Nipah viruses. Microbes Infect 3:307–314. doi: 10.1016/S1286-4579(01)01384-3. [DOI] [PubMed] [Google Scholar]
- 18.Ksiazek TG, Rota PA, Rollin PE. 2011. A review of Nipah and Hendra viruses with an historical aside. Virus Res 162:173–183. doi: 10.1016/j.virusres.2011.09.026. [DOI] [PubMed] [Google Scholar]
- 19.Weingartl HM, Berhane Y, Czub M. 2009. Animal models of henipavirus infection: a review. Vet J 181:211–220. doi: 10.1016/j.tvjl.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 20.Lo MK, Rota PA. 2008. The emergence of Nipah virus, a highly pathogenic paramyxovirus. J Clin Virol 43:396–400. doi: 10.1016/j.jcv.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Wong KT, Grosjean I, Brisson C, Blanquier B, Fevre-Montange M, Bernard A, Loth P, Georges-Courbot MC, Chevallier M, Akaoka H, Marianneau P, Lam SK, Wild TF, Deubel V. 2003. A golden hamster model for human acute Nipah virus infection. Am J Pathol 163:2127–2137. doi: 10.1016/S0002-9440(10)63569-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bossart KN, Zhu Z, Middleton D, Klippel J, Crameri G, Bingham J, McEachern JA, Green D, Hancock TJ, Chan YP, Hickey AC, Dimitrov DS, Wang LF, Broder CC. 2009. A neutralizing human monoclonal antibody protects against lethal disease in a new ferret model of acute Nipah virus infection. PLoS Pathog 5:e1000642. doi: 10.1371/journal.ppat.1000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geisbert TW, Daddario-DiCaprio KM, Hickey AC, Smith MA, Chan YP, Wang LF, Mattapallil JJ, Geisbert JB, Bossart KN, Broder CC. 2010. Development of an acute and highly pathogenic nonhuman primate model of Nipah virus infection. PLoS One 5:e10690. doi: 10.1371/journal.pone.0010690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rockx B, Brining D, Kramer J, Callison J, Ebihara H, Mansfield K, Feldmann H. 2011. Clinical outcome of henipavirus infection in hamsters is determined by the route and dose of infection. J Virol 85:7658–7671. doi: 10.1128/JVI.00473-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mire CE, Versteeg KM, Cross RW, Agans KN, Fenton KA, Whitt MA, Geisbert TW. 2013. Single injection recombinant vesicular stomatitis virus vaccines protect ferrets against lethal Nipah virus disease. Virol J 10:353. doi: 10.1186/1743-422X-10-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park MS, Shaw ML, Munoz-Jordan J, Cros JF, Nakaya T, Bouvier N, Palese P, Garcia-Sastre A, Basler CF. 2003. Newcastle disease virus (NDV)-based assay demonstrates interferon-antagonist activity for the NDV V protein and the Nipah virus V, W, and C proteins. J Virol 77:1501–1511. doi: 10.1128/JVI.77.2.1501-1511.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kulkarni S, Volchkova V, Basler CF, Palese P, Volchkov VE, Shaw ML. 2009. Nipah virus edits its P gene at high frequency to express the V and W proteins. J Virol 83:3982–3987. doi: 10.1128/JVI.02599-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lo MK, Harcourt BH, Mungall BA, Tamin A, Peeples ME, Bellini WJ, Rota PA. 2009. Determination of the henipavirus phosphoprotein gene mRNA editing frequencies and detection of the C, V and W proteins of Nipah virus in virus-infected cells. J Gen Virol 90:398–404. doi: 10.1099/vir.0.007294-0. [DOI] [PubMed] [Google Scholar]
- 29.Yoneda M, Guillaume V, Sato H, Fujita K, Georges-Courbot MC, Ikeda F, Omi M, Muto-Terao Y, Wild TF, Kai C. 2010. The nonstructural proteins of Nipah virus play a key role in pathogenicity in experimentally infected animals. PLoS One 5:e12709. doi: 10.1371/journal.pone.0012709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaw ML, Garcia-Sastre A, Palese P, Basler CF. 2004. Nipah virus V and W proteins have a common STAT1-binding domain yet inhibit STAT1 activation from the cytoplasmic and nuclear compartments, respectively. J Virol 78:5633–5641. doi: 10.1128/JVI.78.11.5633-5641.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lo MK, Miller D, Aljofan M, Mungall BA, Rollin PE, Bellini WJ, Rota PA. 2010. Characterization of the antiviral and inflammatory responses against Nipah virus in endothelial cells and neurons. Virology 404:78–88. doi: 10.1016/j.virol.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 32.Childs K, Stock N, Ross C, Andrejeva J, Hilton L, Skinner M, Randall R, Goodbourn S. 2007. mda-5, but not RIG-I, is a common target for paramyxovirus V proteins. Virology 359:190–200. doi: 10.1016/j.virol.2006.09.023. [DOI] [PubMed] [Google Scholar]
- 33.Childs K, Randall R, Goodbourn S. 2012. Paramyxovirus V proteins interact with the RNA helicase LGP2 to inhibit RIG-I-dependent interferon induction. J Virol 86:3411–3421. doi: 10.1128/JVI.06405-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis ME, Wang MK, Rennick LJ, Full F, Gableske S, Mesman AW, Gringhuis SI, Geijtenbeek TBH, Duprex WP, Gack MU. 2014. Antagonism of the phosphatase PP1 by the measles virus V protein is required for innate immune escape of MDA5. Cell Host Microbe 16:19–30. doi: 10.1016/j.chom.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rodriguez JJ, Parisien JP, Horvath CM. 2002. Nipah virus V protein evades alpha and gamma interferons by preventing STAT1 and STAT2 activation and nuclear accumulation. J Virol 76:11476–11483. doi: 10.1128/JVI.76.22.11476-11483.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shaw ML, Cardenas WB, Zamarin D, Palese P, Basler CF. 2005. Nuclear localization of the Nipah virus W protein allows for inhibition of both virus- and Toll-like receptor 3-triggered signaling pathways. J Virol 79:6078–6088. doi: 10.1128/JVI.79.10.6078-6088.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basler CF. 2012. Nipah and Hendra virus interactions with the innate immune system. Curr Top Microbiol Immunol 359:123–152. doi: 10.1007/82_2012_209. [DOI] [PubMed] [Google Scholar]
- 38.Lo MK, Søgaard TM, Karlin DG. 2014. Evolution and structural organization of the C proteins of Paramyxovirinae. PLoS One 9:e90003. doi: 10.1371/journal.pone.0090003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lo MK, Peeples ME, Bellini WJ, Nichol ST, Rota PA, Spiropoulou CF. 2012. Distinct and overlapping roles of Nipah virus P gene products in modulating the human endothelial cell antiviral response. PLoS One 7:e47790. doi: 10.1371/journal.pone.0047790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yamaguchi M, Kitagawa Y, Zhou M, Itoh M, Gotoh B. 2014. An anti-interferon activity shared by paramyxovirus C proteins: inhibition of Toll-like receptor 7/9-dependent alpha interferon induction. FEBS Lett 588:28–34. doi: 10.1016/j.febslet.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 41.Mathieu C, Guillaume V, Volchkova VA, Pohl C, Jacquot F, Looi RY, Wong KT, Legras-Lachuer C, Volchkov VE, Lachuer J, Horvat B. 2012. Nonstructural Nipah virus C protein regulates both the early host proinflammatory response and viral virulence. J Virol 86:10766–10775. doi: 10.1128/JVI.01203-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ciancanelli MJ, Volchkova VA, Shaw ML, Volchkov VE, Basler CF. 2009. Nipah virus sequesters inactive STAT1 in the nucleus via a P gene-encoded mechanism. J Virol 83:7828–7841. doi: 10.1128/JVI.02610-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buchholz UJ, Finke S, Conzelmann KK. 1999. Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J Virol 73:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Research Council. 2011. Guide for the care and use of laboratory animals, 8th ed National Academies Press, Washington, DC. [Google Scholar]
- 45.Takeshita Y, Ransohoff RM. 2012. Inflammatory cell trafficking across the blood-brain barrier: chemokine regulation and in vitro models. Immunol Rev 248:228–239. doi: 10.1111/j.1600-065X.2012.01127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Devaux P, Hodge G, McChesney MB, Cattaneo R. 2008. Attenuation of V- or C-defective measles viruses: infection control by the inflammatory and interferon responses of rhesus monkeys. J Virol 82:5359–5367. doi: 10.1128/JVI.00169-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.von Messling V, Svitek N, Cattaneo R. 2006. Receptor (SLAM [CD150]) recognition and the V protein sustain swift lymphocyte-based invasion of mucosal tissue and lymphatic organs by a morbillivirus. J Virol 80:6084–6092. doi: 10.1128/JVI.00357-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pfaller CK, Mastorakos GM, Matchett WE, Ma X, Samuel CE, Cattaneo R. 2015. Measles virus defective interfering RNAs are generated frequently and early in the absence of C protein and can be destabilized by adenosine deaminase acting on RNA-1-like hypermutations. J Virol 89:7735–7747. doi: 10.1128/JVI.01017-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Devaux P, Cattaneo R. 2004. Measles virus phosphoprotein gene products: conformational flexibility of the P/V protein amino-terminal domain and C protein infectivity factor function. J Virol 78:11632–11640. doi: 10.1128/JVI.78.21.11632-11640.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ng BY, Lim CC, Yeoh A, Lee WL. 2004. Neuropsychiatric sequelae of Nipah virus encephalitis. J Neuropsychiatry Clin Neurosci 16:500–504. doi: 10.1176/jnp.16.4.500. [DOI] [PubMed] [Google Scholar]
- 51.Geisbert TW, Mire CE, Geisbert JB, Chan YP, Agans KN, Feldmann F, Fenton KA, Zhu Z, Dimitrov DS, Scott DP, Bossart KN, Feldmann H, Broder CC. 2014. Therapeutic treatment of Nipah virus infection in nonhuman primates with a neutralizing human monoclonal antibody. Sci Transl Med 6:242ra82. doi: 10.1126/scitranslmed.3008929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hooper DC, Phares TW, Fabis MJ, Roy A. 2009. The production of antibody by invading B cells is required for the clearance of rabies virus from the central nervous system. PLoS Negl Trop Dis 3:e535. doi: 10.1371/journal.pntd.0000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Murphy FA. 1977. Rabies pathogenesis. Arch Virol 54:279–297. doi: 10.1007/BF01314774. [DOI] [PubMed] [Google Scholar]
- 54.Mathieu C, Pohl C, Szecsi J, Trajkovic-Bodennec S, Devergnas S, Raoul H, Cosset FL, Gerlier D, Wild TF, Horvat B. 2011. Nipah virus uses leukocytes for efficient dissemination within a host. J Virol 85:7863–7871. doi: 10.1128/JVI.00549-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ivey NS, MacLean AG, Lackner AA. 2009. Acquired immunodeficiency syndrome and the blood-brain barrier. J Neurovirol 15:111–122. doi: 10.1080/13550280902769764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tunkel AR, Rosser SW, Hansen EJ, Scheld WM. 1991. Blood-brain barrier alterations in bacterial meningitis: development of an in vitro model and observations on the effects of lipopolysaccharide. In Vitro Cell Dev Biol 27A:113–120. [DOI] [PubMed] [Google Scholar]
- 57.Bermpohl D, Halle A, Freyer D, Dagand E, Braun JS, Bechmann I, Schroder NW, Weber JR. 2005. Bacterial programmed cell death of cerebral endothelial cells involves dual death pathways. J Clin Invest 115:1607–1615. doi: 10.1172/JCI23223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barkhordarian A, Thames AD, Du AM, Jan AL, Nahcivan M, Nguyen MT, Sama N, Chiappelli F. 2015. Viral immune surveillance: toward a TH17/TH9 gate to the central nervous system. Bioinformation 11:47–54. doi: 10.6026/97320630011047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kamimura D, Yamada M, Harada M, Sabharwal L, Meng J, Bando H, Ogura H, Atsumi T, Arima Y, Murakami M. 2013. The gateway theory: bridging neural and immune interactions in the CNS. Front Neurosci 7:204. doi: 10.3389/fnins.2013.00204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lamp B, Dietzel E, Kolesnikova L, Sauerhering L, Erbar S, Weingartl H, Maisner A. 2013. Nipah virus entry and egress from polarized epithelial cells. J Virol 87:3143–3154. doi: 10.1128/JVI.02696-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Devaux P, Hudacek AW, Hodge G, Reyes-Del Valle J, McChesney MB, Cattaneo R. 2011. A recombinant measles virus unable to antagonize STAT1 function cannot control inflammation and is attenuated in rhesus monkeys. J Virol 85:348–356. doi: 10.1128/JVI.00802-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Svitek N, Gerhauser I, Goncalves C, Grabski E, Doring M, Kalinke U, Anderson DE, Cattaneo R, von Messling V. 2014. Morbillivirus control of the interferon response: relevance of STAT2 and mda5 but not STAT1 for canine distemper virus virulence in ferrets. J Virol 88:2941–2950. doi: 10.1128/JVI.03076-13. [DOI] [PMC free article] [PubMed] [Google Scholar]