Abstract
Background
The association between perceived stress and atrial fibrillation (AF) remains unclear.
Purpose
To examine the association between perceived stress and AF.
Methods
A total of 25,530 participants (mean age: 65 ± 9.4 years; 54% women; 41% blacks) from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study were included in this analysis. Logistic regression was used to compute odds ratios (OR) and 95% confidence intervals (CI) for the association between the short version of the Cohen Perceived Stress Scale and AF.
Results
In a multivariable analysis adjusted for demographics, cardiovascular risk factors, and potential confounders, the prevalence of AF was found to increase with higher levels of perceived stress (none: OR=1.0, referent; low stress: OR=1.12, 95%CI=0.98, 1.27; moderate stress: OR=1.27, 95%CI=1.11, 1.47; high stress: OR=1.60, 95%CI=1.39, 1.84).
Conclusion
Increasing levels of perceived stress are associated with prevalent AF in REGARDS.
Keywords: stress, atrial fibrillation, epidemiology
Introduction
Increased levels of stress are associated with several cardiovascular outcomes. For example, elevated stress in women of lower occupational status is associated with a higher incidence of hypertension (1). Chronic stress also has been implicated in the development of diabetes, coronary heart disease (CHD), and stroke (2-4).
Atrial fibrillation (AF) shares several risk factors with the aforementioned cardiovascular outcomes. Potentially, psychological stress also increases one's risk for AF development. This is partially supported by previous reports showing that persons with AF have elevated levels of depression and anxiety (5-7). Additionally, data from the Framingham Offspring Study have implicated tension, anger, and hostility as risk factors for AF in males (8,9).
Due to the increased prevalence of adverse psychological outcomes reported in those with AF, a higher percentage of persons with AF possibly experience increased levels of perceived stress. It also is plausible that the relationship between perceived stress and AF varies by race due to the higher prevalence of CHD among black men and women compared with whites, and the known association between stress and CHD (10). Additionally, the association possibly varies by income since high levels of perceived stress are associated with a greater CHD risk in individuals with low but not high incomes (3).
The purpose of this analysis was to examine the cross-sectional association between perceived stress and AF in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study, a large biracial cohort of men and women. Such a finding would extend previous work regarding psychological distress and AF to perceived stress.
Methods
Study Population and Design
Details of REGARDS have been published previously (11). Briefly, this prospective cohort study was designed to identify causes of regional and racial disparities in stroke mortality. The study over sampled blacks and residents of the stroke belt (North Carolina, South Carolina, Georgia, Alabama, Mississippi, Tennessee, Arkansas, and Louisiana). This included participants from the stroke buckle (coastal plains of North Carolina, South Carolina and Georgia) as this region experiences a stroke mortality rate considerably higher than the rest of the United States (12). Between January 2003 and October 2007, a total of 30,239 participants were recruited from a commercially available list of residents using postal mailings and telephone interviews. Demographic information and medical histories were obtained by trained interviewers using a computer-assisted telephone interview (CATI) system. Additionally, a brief in-home physical examination was performed approximately 3 to 4 weeks after the telephone interview. During the in-home visit, trained staff collected medication information, blood and urine samples, blood pressure readings, and a resting electrocardiogram.
This analysis examined the cross-sectional association between perceived stress and AF. Of the 30,239 participants from the original REGARDS cohort, 56 were excluded for data anomalies. Participants were excluded if they were missing perceived stress data, AF data, or baseline covariates. A total of 25,530 study participants (mean age: 65 ± 9.4 years; 54% women; 41% blacks) were included in the final analysis.
Perceived Stress
Perceived stress was measured using a short version of the Cohen Perceived Stress Scale (PSS) (13). The PSS measures the degree to which participants feel they are unable to control important aspects of their life, their confidence to handle personal problems, how often they are unable to cope with all the things they needed to do, and how often their difficulties were overwhelming over the month prior to administration of the survey. The PSS is scored using a 5-point scale (0=never, 1=almost never, 2=sometimes, 3=fairly often, 4=very often), with final scores ranging from 0 to 16. Because of the skewed distribution of the PSS score and lack of defined cut-points, PSS was categorized by quartiles to examine its association with AF across increasing levels of perceived stress (none: PSS=0; low stress: 1 ≤PSS ≤3; moderate stress: 4≤ PSS ≤5; high stress: PSS >5) (3). We also examined the association between PSS and AF as a continuous variable per 1-unit increase in the PSS.
Atrial Fibrillation
AF was identified at baseline by the study-scheduled electrocardiogram and also from a self-reported history of a physician diagnosis during the CATI surveys. The electrocardiograms were read and coded at a central reading center by analysts who were blind to other REGARDS data (Epidemiologial Cardiology Research Center, Wake Forest School of Medicine, Winston-Salem, NC, USA). Self-reported AF was defined as an affirmative response to the following question: “Has a physician or a health professional ever told you that you had atrial fibrillation? (14)”
Covariates
Participant characteristics collected during the initial REGARDS in-home visit were used in this analysis. Age, sex, race, income, education, alcohol use, exercise habits, and smoking status were self-reported. Annual household income was dichotomized at <$35,000 or ≥$35,000 based on prior work showing the relationship between perceived stress and CHD possibly varies by income (3). Education was categorized into “high school or less,” or “some college or more.” Alcohol use was classified by the number of drinks per week reported by study participants using the following criteria: none, moderate (1 to 2 drinks/day for men and 1 drink/day for women), and heavy (>2 drinks/day for men and >1 drink/day for women). Exercise was classified as none, 1 to 3 times per week, and 4 or more times per week. The presence of depressive symptoms was defined as a score of 4 or more on the 4-item Center for Epidemiologic Studies Depression Scale (15,16). Smoking was defined as ever (e.g., current and former) or never smoker. Fasting blood samples were obtained and assayed for total cholesterol, high-density lipoprotein (HDL) cholesterol, and glucose. Diabetes was defined as a fasting glucose level ≥126 mg/dL (or a non-fasting glucose, ≥200 mg/dL among those failing to fast) or self-reported diabetes medication use. The use of aspirin, antihypertensive medications, and lipid-lowering medications was defined by the self-reported current use of these medications during the CATI surveys. Body mass index was computed as the weight in kilograms divided by the square of the height in meters. After the participant rested for 5 minutes in a seated position, blood pressure was measured using a sphygmomanometer. Two values were obtained following a standardized protocol and averaged. Using baseline electrocardiogram data, left ventricular hypertrophy was defined by the Sokolow-Lyon Criteria (17). Cardiovascular disease was defined as a history of CHD or stroke. CHD was confirmed by self-reported history of myocardial infarction, coronary artery bypass grafting, coronary angioplasty or stenting, or if evidence of prior myocardial infarction was present on the baseline electrocardiogram. Prior stroke was ascertained by participant self-reported history.
Statistics
Categorical variables were reported as frequency and percentage while continuous variables were reported as mean ± standard deviation. Statistical significance for categorical variables was tested using the chi-square method and the Kruskal-Wallis procedure for continuous variables. Logistic regression was used to compute odds ratios (OR) and 95% confidence intervals (CI) for the association between perceived stress and AF. Multivariable models were constructed as follows: Model 1 adjusted for age, sex, race, education, income, and geographic region; Model 2 included Model 1 covariates with the addition of systolic blood pressure, HDL cholesterol, total cholesterol, body mass index, smoking, diabetes, exercise, alcohol consumption, depression, antihypertensive medications, lipid-lowering therapies, left ventricular hypertrophy, and prior cardiovascular disease. Several sensitivity analyses were performed between perceived stress and AF using high stress (PSS >5). Due to the known association between blood pressure and stress, a sensitivity analysis was performed with adjustment for pulse pressure. Additionally, subgroup analyses were performed to evaluate effect modification by age (dichotomized at 65 years), sex (male vs. female), race (black vs. white), income (<$35,000 vs. ≥$35,000), and education (“high school or less” vs. “some college or more”) using a stratification technique and comparing models with and without interaction terms. Statistical significance for all comparisons including interactions was defined as p <0.05. SAS Version 9.3 (Cary, NC) was used for all analyses.
Results
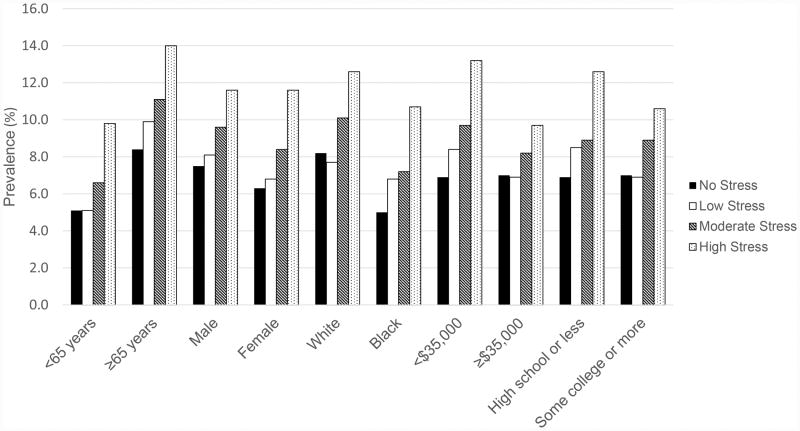
A total of 6,501 (25%), 8,616 (34%), 4,978 (20%), and 5,435 (21%) participants were categorized as having no stress, low stress, moderate stress, and high stress, respectively. Baseline characteristics for study participants stratified by PSS are shown in Table 1. AF was prevalent in 2,162 (8.5%) participants. The prevalence of AF increased with higher levels of perceived stress (none: 7.0%; low stress: 7.4%; moderate stress: 8.9%; high stress: 11.6%; Cochran-Armitage p-trend <0.0001). The prevalence of AF by age, sex, race, income, and education is shown in Figure 1.
Table 1. Baseline Characteristics (N=25,530).
| Characteristic | Entire Cohort (N=25,530) |
No Stress PSS=0 (n=6,501) |
Low Stress 1≤ PSS ≤3 (n=8,616) |
Moderate Stress 4≤ PSS ≤5 (n=4,978) |
High Stress PSS > 5 (n=5,435) |
P-value* |
|---|---|---|---|---|---|---|
| Age, mean (SD), years | 65 (9.4) | 66 (8.8) | 65 (9.3) | 65 (9.6) | 64 (9.9) | <0.0001 |
| Male (%) | 11,670 (46) | 3,657 (56) | 4,020 (47) | 2,146 (43) | 1,847 (34) | <0.0001 |
| Black (%) | 10,373 (41) | 2,607 (40) | 2,859 (33) | 2,147 (43) | 2,760 (51) | <0.0001 |
| Region | ||||||
| Stroke buckle (%) | 5,367 (21) | 1,308 (20) | 1,747 (20) | 1,084 (22) | 1,228 (23) | |
| Stroke belt (%) | 8,824 (35) | 2,215 (34) | 2,893 (34) | 1,732 (35) | 1,984 (37) | |
| Non-belt (%) | 11,339 (44) | 2,978 (46) | 3,976 (46) | 2,162 (43) | 2,223 (41) | <0.0001 |
| Education, high school or less (%) | 9,693 (38) | 2,312 (36) | 2,683 (31) | 2,021 (41) | 2,677 (49) | <0.0001 |
| Annual income, <$35,000 (%) | 10,674 (42) | 2,458 (38) | 2,985 (35) | 2,252 (45) | 2,979 (55) | <0.0001 |
| Body mass index, mean (SD), kg/m2 | 29 (6.1) | 29 (5.6) | 29 (6.0) | 29 (6.3) | 30 (6.8) | <0.0001 |
| Alcohol consumption | ||||||
| Heavy (%) | 991 (4.0) | 307 (4.7) | 352 (4.1) | 163 (3.3) | 169 (3.1) | |
| Moderate (%) | 8,469 (33) | 2,200 (34) | 3,146 (37) | 1,598 (32) | 1,525 (28) | |
| None (%) | 16,070 (63) | 3,994 (61) | 5,118 (59) | 3,217 (65) | 3,741 (69) | <0.0001 |
| Exercise | ||||||
| 4 or more times per week (%) | 7,509 (29) | 2,254 (35) | 2,625 (30) | 1,380 (28) | 1,250 (23) | |
| 1 to 3 times per week (%) | 9,161 (36) | 2,235 (34) | 3,239 (38) | 1,861 (37) | 1,826 (34) | |
| None (%) | 8,860 (35) | 2,012 (31) | 2,752 (32) | 1,737 (35) | 2,359 (43) | <0.0001 |
| Ever smoker (%) | 13,922 (55) | 3,691 (57) | 4,567 (53) | 2,659 (53) | 3,005 (55) | <0.0001 |
| Depression (%) | 2,738 (11) | 152 (2.3) | 366 (4.3) | 461 (9.3) | 1,759 (32) | <0.0001 |
| Diabetes (%) | 5,345 (21) | 1,322 (20) | 1,543 (18) | 1,093 (22) | 1,387 (26) | <0.0001 |
| Systolic blood pressure, mean (SD), mm Hg | 127 (17) | 128 (16) | 126 (16) | 127 (17) | 128 (18) | <0.0001 |
| Diastolic blood pressure, mean (SD), mm Hg | 76 (9.7) | 77 (9.4) | 76 (9.4) | 76 (9.7) | 77 (10) | <0.0001 |
| Pulse pressure, mean (SD), mm Hg | 51 (13) | 52 (13) | 50 (13) | 51 (14) | 51 (14) | <0.0001 |
| Total cholesterol, mean (SD), mg/dL | 192 (40) | 190 (40) | 192 (39) | 191 (39) | 194 (42) | <0.0001 |
| HDL cholesterol, mean (SD), mg/dL | 52 (16) | 51 (16) | 52 (16) | 52 (16) | 52 (16) | <0.0001 |
| Aspirin use (%) | 11,144 (44) | 2,982 (46) | 3,763 (44) | 2,082 (42) | 2,317 (43) | <0.0001 |
| Antihypertensive medication use (%) | 13,578 (53) | 3,449 (53) | 4,269 (50) | 2,643 (53) | 3,217 (59) | <0.0001 |
| Lipid-lowering medication use (%) | 8,591 (34) | 2,176 (33) | 2,789 (32) | 1,730 (35) | 1,896 (35) | 0.0050 |
| Left ventricular hypertrophy (%) | 2,526 (9.9) | 658 (10) | 757 (8.8) | 483 (9.7) | 628 (12) | <0.0001 |
| Cardiovascular disease (%) | 5,484 (21) | 1,389 (21) | 1,613 (19) | 1,119 (22) | 1,363 (25) | <0.0001 |
Statistical significance for categorical variables tested using the chi-square method and for continuous variables the Kruskal-Wallis procedure was used.
HDL, high-density lipoprotein; PSS, perceived stress scale; SD, standard deviation.
Figure 1. Prevalence of Atrial Fibrillation by Age, Sex, Race, Income, and Education.
In an unadjusted analysis, the prevalence of AF was found to increase with higher levels of perceived stress (none: OR=1.0, referent; low stress: 1.07, 95%CI=0.94, 1.21; moderate stress: OR=1.30, 95%CI=1.14, 1.50; high stress: OR=1.76, 95%CI=1.55, 1.99). Similar results were obtained in the unadjusted analysis per 1-unit increase in the PSS (OR=1.08, 95%CI=1.06, 1.09). After adjustment for demographics, cardiovascular risk factors, and potential confounders, increasing levels of perceived stress were significantly associated with AF when examined as a categorical and continuous variable (Table 2).
Table 2. Association between Perceived Stress and Atrial Fibrillation (N=25,530).
| AF Cases | Model 1* OR (95%CI) | P-value | Model 2† OR (95%CI) | P-value | |
|---|---|---|---|---|---|
| No Stress (PSS=0) | 452/6,501 | 1.0 | - | 1.0 | - |
| Low Stress (1≤ PSS ≤3) | 638/8,616 | 1.12 (0.99, 1.27) | 0.086 | 1.12 (0.98, 1.27) | 0.094 |
| Moderate Stress (4≤ PSS ≤5) | 442/4,978 | 1.35 (1.18, 1.55) | <0.0001 | 1.27 (1.11, 1.47) | 0.0007 |
| High Stress (PSS > 5) | 630/5,435 | 1.93 (1.70, 2.20) | <0.0001 | 1.60 (1.39, 1.84) | <0.0001 |
| PSS per 1-unit increase | 2,162/25,530 | 1.09 (1.08, 1.11) | <0.0001 | 1.06 (1.05, 1.09) | <0.0001 |
Adjusted for age, sex, race, education, income, and geographic region.
Adjusted for Model 1 covariates with the addition of systolic blood pressure, HDL cholesterol, total cholesterol, body mass index, smoking, diabetes, exercise, alcohol consumption, depression, antihypertensive medications, lipid-lowering therapies, left ventricular hypertrophy, and prior cardiovascular disease.
CI, confidence interval; HDL, high-density lipoprotein; OR, odds ratio; PSS, perceived stress scale.
High perceived stress remained significantly associated with AF (OR=1.55, 95%CI=1.39, 1.71) when pulse pressure was included in the fully adjusted model. Additionally, the results remained similar when stratified by age, sex, race, income, and education (Table 3). However, a trend was observed for income with the association between perceived stress and AF being stronger for those with income <$35,000 (OR=1.48, 95%CI=1.28, 1.73) compared with participants with incomes ≥$35,000 (OR=1.34, 95%CI=1.13, 1.58) (p-interaction=0.064) (Table 3). When we examined the association by income with PSS as a continuous variable, the association was stronger for those with incomes <$35,000 (OR=1.07, 95%CI=1.05, 1.10) compared with ≥$35,000 (OR=1.05, 95%CI=1.03, 1.08) (p-interaction=0.022).
Table 3. Subgroup Analysis (N=25,530)*.
| AF Cases | Model 1† OR (95%CI) | P-value | Model 2‡ OR (95%CI) | P-value | Interactionδ P-value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| <65 years | 848/12,962 | 1.66 (1.43, 1.93) | <0.0001 | 1.37 (1.15, 1.62) | 0.0003 | 0.28 |
| ≥65 years | 1,314/12,568 | 1.68 (1.46, 1.93) | <0.0001 | 1.45 (1.25, 1.68) | <0.0001 | |
| Sex | ||||||
| Female | 1,145/13,860 | 1.71 (1.50, 1.95) | <0.0001 | 1.41 (1.23, 1.63) | <0.0001 | 0.22 |
| Male | 1,017/11,670 | 1.65 (1.40, 1.94) | <0.0001 | 1.42 (1.19, 1.70) | 0.0001 | |
| Race | ||||||
| Black | 774/10,373 | 1.68 (1.44, 1.97) | <0.0001 | 1.34 (1.13, 1.59) | 0.0008 | 0.49 |
| White | 1,388/15,157 | 1.70 (1.49, 1.95) | <0.0001 | 1.48 (1.28, 1.71) | <0.0001 | |
| Income | ||||||
| <$35,000 | 1,033/10,674 | 1.80 (1.57, 2.06) | <0.0001 | 1.48 (1.28, 1.73) | <0.0001 | 0.064 |
| ≥$35,000 | 1,129/14,856 | 1.53 (1.31, 1.79) | <0.0001 | 1.34 (1.13, 1.58) | 0.0006 | |
| Education | ||||||
| High school or less | 904/9,693 | 1.74 (1.50, 2.02) | <0.0001 | 1.38 (1.18, 1.63) | <0.0001 | 0.33 |
| Some college or more | 1,258/15,837 | 1.63 (1.41, 1.87) | <0.0001 | 1.43 (1.23, 1.66) | <0.0001 |
ORs are presented for high stress (PSS >5).
Adjusted for age, sex, race, education, income, and geographic region.
Adjusted for Model 1 covariates with the addition of systolic blood pressure, HDL cholesterol, total cholesterol, body mass index, smoking, diabetes, exercise, alcohol consumption, depression, antihypertensive medications, lipid-lowering therapies, left ventricular hypertrophy, and prior cardiovascular disease.
Interactions tested using Model 2.
CI, confidence interval; HDL, high-density lipoprotein; OR, odds ratio; PSS, perceived stress scale.
Discussion
In this analysis from REGARDS, an increasing prevalence of AF was observed with higher levels of perceived stress. The results were consistent when stratified by age, sex, race, and educational attainment. A trend was observed for the relationship between high levels of perceived stress and AF by income, with the association being stronger for those with lower compared with higher incomes. Additionally, when we examined the association between perceived stress and AF by income as a continuous variable, the association was significantly stronger for those with low compared with high incomes. In aggregate, our results suggest that AF is associated with higher levels of perceived stress and the association varies by income.
The majority of studies that have examined the relationship between psychological distress and AF have focused on persons with known AF and its influence on mental health and quality of life. An examination of 70 patients with AF has shown that the predominant affective response after a diagnosis of AF is anxiety (5). A case-control study of 101 AF patients and 97 hypertensive patients in sinus rhythm showed that persons with AF have elevated levels of depression and anxiety which negatively impact quality of life (6). Additionally, a study of 93 patients has shown that reduced quality of life in AF patients possibly is related to depression in women but not men (7). Depressive symptoms also have been associated with an increased recurrence of AF after electrical cardioversion to normal sinus rhythm (18). Only data from the Framingham Offspring study have shown that increased levels of tension, anxiety, anger, and hostility precede the development of AF in men but not women (8,9).
The aforementioned studies provide evidence that persons with AF experience increased levels of psychological distress that are mainly limited to anxiety and depression. Additionally, several aspects of psychological distress (e.g., tension, anxiety, anger, and hostility) possibly precede AF development. Our data provide further evidence that persons who have AF also have higher levels of psychological distress but extend these constructs to perceived stress. Furthermore, the current study was not limited to clinic- or hospital-based populations as we used data from REGARDS, a large biracial cohort of men and women (5-7,18). We also were able to examine the relationship between perceived stress and AF by several factors that likely influenced the relationship between stress and AF (e.g., sex, income, and education). Similar to a prior report from REGARDS that showed high perceived stress was associated with incident CHD and all-cause mortality among low- but not high-income participants, we observed a similar association between perceived stress and AF (3).
Elevated levels of stress have been implicated in the development of several cardiovascular outcomes (e.g., hypertension, diabetes, CHD, and stroke) (1-4). Possible explanations for these associations are dysfunctional regulation of glucocorticoid secretion, pathological alterations in cardiac autonomic tone, and an increased risk of unhealthful behaviors that accompany persons with high levels of stress (19). Although it has been suggested that psychological distress precedes AF development, we were unable to determine the temporal relationship between perceived stress and AF due to the cross-sectional nature of this study. Our data show that persons who have AF are more likely to report elevated levels of perceived stress and further research is needed to determine if perceived stress increases one's risk for AF development. Possibly, persons with AF who have poor rate control (e.g., rapid ventricular response) are more likely to experience palpitations which are perceived as stressful. Additionally, our data provide evidence that the association between perceived stress and AF differs by income, a marker for socioeconomic status. Low income is associated with the development of psychological distress and the relationship between perceived stress and cardiovascular outcomes varies by income (3,20). Therefore, it is plausible that persons with low incomes have poor coping mechanisms and limited social support which predispose to the development of cardiovascular diseases. However, further studies are needed to clarify the complex pathways between income, perceived stress, and outcomes such as AF. Black participants also were more likely to report higher levels of perceived stress compared with whites, but the association between perceived stress and AF did not vary by race (p-interaction=0.49). This likely is explained by the decreased prevalence of AF in blacks compared with whites that is related to a lower susceptibility to develop AF despite higher reported levels of perceived stress (21). Furthermore, depressive symptoms were observed to increase with higher levels of perceived stress, potentially implicating depression as a mediating factor between perceived stress and AF. This is supported by prior studies that have shown increased levels of depression exist in persons with AF (7).
The current study has several implications regarding the care for those with AF. AF is a common arrhythmia encountered in clinical practice and its prevalence is projected to double by the year 2050 (21). The projected increases in the prevalence of AF are largely attributed to the expected growth in individuals over 65 years of age (21-23). Additionally, a significant burden will be placed on the healthcare system as persons over 65 years of age with AF are frequently hospitalized (24). Therefore, interventions that reduce stress in AF patients may have important implications in improving outcomes related to AF care. For example, those with AF have an increased risk of incident myocardial infarction and due to the known association between stress and CHD development, stress potentially is a mediating factor (3,25-27). Furthermore, if stress increases the risk for AF development, targeted preventions aimed to reduce stress in at-risk populations (e.g. >65 years of age) possibly are beneficial.
Our results should be interpreted in the context of several limitations. Certain characteristics were self-reported and subjected our analysis to recall and misclassification biases (e.g. exercise habits, smoking). This also included our classification of perceived stress as it was measured by survey. We classified perceived stress using a short version of the Cohen PSS, and the relationship between perceived stress and AF possibly varies with other scales. AF was ascertained at baseline by participant history and from electrocardiogram data. Potentially, non-permanent cases of AF were missed due to the intermittent nature of paroxysmal and persistent cases. Additionally, although we adjusted for several potential confounders, residual confounding remains a possibility. Furthermore, the cross-sectional design of this study prevented the determination of the temporal relationship between perceived stress and AF.
In conclusion, we have shown that increasing levels of perceived stress are associated with prevalent AF in REGARDS, and this association possibly varies by income. Potentially, targeted interventions aimed at reducing stress in those with AF and among persons who are high risk for developing this arrhythmia are beneficial. Further research is needed to confirm our findings and to explore the underlying mechanisms for the observed association.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Funding: This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health.
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest.
Ethics Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants included in the study.
References
- 1.Wiernik E, Nabi H, Pannier B, et al. Perceived stress, sex and occupational status interact to increase the risk of future high blood pressure: the IPC cohort study. J Hypertens. 2014;32(10):1979–1986. doi: 10.1097/HJH.0000000000000288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallo LC, Roesch SC, Fortmann AL, et al. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Psychosom Med. 2014;76(6):468–475. doi: 10.1097/PSY.0000000000000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Redmond N, Richman J, Gamboa CM, et al. Perceived stress is associated with incident coronary heart disease and all-cause mortality in low- but not high-income participants in the Reasons for Geographic And Racial Differences in Stroke study. J Am Heart Assoc. 2013;2(6):e000447. doi: 10.1161/JAHA.113.000447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henderson KM, Clark CJ, Lewis TT, et al. Psychosocial distress and stroke risk in older adults. Stroke. 2013;44(2):367–372. doi: 10.1161/STROKEAHA.112.679159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lane DA, Langman CM, Lip GY, Nouwen A. Illness perceptions, affective response, and health-related quality of life in patients with atrial fibrillation. J Psychosom Res. 2009;66(3):203–210. doi: 10.1016/j.jpsychores.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Thrall G, Lip GY, Carroll D, Lane D. Depression, anxiety, and quality of life in patients with atrial fibrillation. Chest. 2007;132(4):1259–1264. doi: 10.1378/chest.07-0036. [DOI] [PubMed] [Google Scholar]
- 7.Ong L, Irvine J, Nolan R, et al. Gender differences and quality of life in atrial fibrillation: the mediating role of depression. J Psychosom Res. 2006;61(6):769–774. doi: 10.1016/j.jpsychores.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Eaker ED, Sullivan LM, Kelly-Hayes M, D'Agostino RB, Sr, Benjamin EJ. Anger and hostility predict the development of atrial fibrillation in men in the Framingham Offspring Study. Circulation. 2004;109(10):1267–1271. doi: 10.1161/01.CIR.0000118535.15205.8F. [DOI] [PubMed] [Google Scholar]
- 9.Eaker ED, Sullivan LM, Kelly-Hayes M, D'Agostino RB, Sr, Benjamin EJ. Tension and anxiety and the prediction of the 10-year incidence of coronary heart disease, atrial fibrillation, and total mortality: the Framingham Offspring Study. Psychosom Med. 2005;67(5):692–696. doi: 10.1097/01.psy.0000174050.87193.96. [DOI] [PubMed] [Google Scholar]
- 10.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 12.Howard G, Anderson R, Johnson NJ, Sorlie P, Russell G, Howard VJ. Evaluation of social status as a contributing factor to the stroke belt region of the United States. Stroke. 1997;28(5):936–940. doi: 10.1161/01.str.28.5.936. [DOI] [PubMed] [Google Scholar]
- 13.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 14.Soliman EZ, Howard G, Meschia JF, et al. Self-reported atrial fibrillation and risk of stroke in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2011;42(10):2950–2953. doi: 10.1161/STROKEAHA.111.621367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fava GA, Pilowsky I, Pierfederici A, Bernardi M, Pathak D. Depressive symptoms and abnormal illness behavior in general hospital patients. Gen Hosp Psychiatry. 1982;4(3):171–178. doi: 10.1016/0163-8343(82)90053-6. [DOI] [PubMed] [Google Scholar]
- 16.Bowling CB, Booth JN, 3rd, Safford MM, et al. Nondisease-specific problems and all-cause mortality in the REasons for Geographic and Racial Differences in Stroke study. J Am Geriatr Soc. 2013;61(5):739–746. doi: 10.1111/jgs.12214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J. 1949;37(2):161–186. doi: 10.1016/0002-8703(49)90562-1. [DOI] [PubMed] [Google Scholar]
- 18.Lange HW, Herrmann-Lingen C. Depressive symptoms predict recurrence of atrial fibrillation after cardioversion. J Psychosom Res. 2007;63(5):509–513. doi: 10.1016/j.jpsychores.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 19.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 20.Orpana HM, Lemyre L, Gravel R. Income and psychological distress: the role of the social environment. Health Rep. 2009;20(1):21–28. [PubMed] [Google Scholar]
- 21.Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 22.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odden MC, Coxson PG, Moran A, Lightwood JM, Goldman L, Bibbins-Domingo K. The impact of the aging population on coronary heart disease in the United States. Am J Med. 2011;124(9):827–833. doi: 10.1016/j.amjmed.2011.04.010. e825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naccarelli GV, Johnston SS, Dalal M, Lin J, Patel PP. Rates and implications for hospitalization of patients >/=65 years of age with atrial fibrillation/flutter. Am J Cardiol. 2012;109(4):543–549. doi: 10.1016/j.amjcard.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 25.Soliman EZ, Safford MM, Muntner P, et al. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med. 2014;174(1):107–114. doi: 10.1001/jamainternmed.2013.11912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Neal WT, Sangal K, Zhang ZM, Soliman EZ. Atrial fibrillation and incident myocardial infarction in the elderly. Clin Cardiol. 2014;37(12):750–755. doi: 10.1002/clc.22339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soliman EZ, Lopez F, O'Neal WT, et al. Atrial Fibrillation and Risk of ST-Segment Elevation versus Non-ST Segment Elevation Myocardial Infarction: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2015;131(21):1843–50. doi: 10.1161/CIRCULATIONAHA.114.014145. [DOI] [PMC free article] [PubMed] [Google Scholar]