Abstract
Objective
Patients with major depressive disorder (MDD) and a comorbid personality disorder (PD) have been found to exhibit relatively poor outcomes in cognitive therapy (CT) and other treatments. Adaptations of CT focusing heavily on patients’ core beliefs have yielded promising findings in the treatment of PD. However, there have been no investigations that have specifically tested whether increased focus on maladaptive beliefs contributes to CT’s efficacy for these patients.
Method
CT technique use from an early CT session was assessed for 59 patients (33 without PD, 26 with PD – predominantly Cluster-C) who participated in a randomized controlled trial for moderate to severe MDD. Scores were calculated for directive CT techniques (CT-Concrete) and a set of belief-focused items (CT-Belief) as rated by the Collaborative Study Process Rating Scale. Robust regressions were conducted to estimate relations between scores on each of these measures and change in depressive and PD symptoms. A PD status by CT-Belief use interaction tested the hypothesis that therapist use of CT-Belief techniques would exhibit a stronger association with symptom change in the PD group relative to the non-PD group.
Results
As hypothesized, a significant interaction between PD status and use of CT-Belief techniques emerged in the prediction of depressive and PD symptom change. Among PD patients, higher early CT-Belief interventions were found to predict significantly greater improvement. CT-Belief use did not predict greater symptom change among those without PD.
Conclusions
Early focus on CT-Belief interventions may facilitate changes in depression and PD symptoms for patients with MDD-PD comorbidity.
Keywords: cognitive therapy, personality disorders, depression, psychotherapy process, adherence
Personality disorder (PD) diagnoses are a common co-morbidity among patients with a major depressive disorder (MDD), estimated at approximately 45% in a recent meta-analysis (Friborg et al., 2014). Cluster-C PD diagnoses (i.e., avoidant, dependent, and obsessive-compulsive; 30% combined prevalence) and borderline PD (14%) are especially common (Friborg et al., 2014).
PD co-morbidity predicts the persistence of depressive symptoms in naturalistic, longitudinal, treatment-seeking samples (Grilo et al., 2010), as well as decreased odds of treatment response in trials of psychotherapy, pharmacotherapy, and combined treatment (Newton-Howes et al., 2014). In a study of depressed patients with co-morbid PD whose depression improved with treatment, Markowitz et al. (2007) reported that those who no longer met PD criteria at the end of treatment experienced more stable improvements in functioning across a 2-year follow-up, compared to those whose PD status did not change.
Due to the potential impact of PD on treatment course, many psychotherapy approaches advocate a strong clinical focus on PD symptomatology when it is apparent (e.g., psychodynamic therapies; Caligor, Clarkin, & Kernberg, 2007; Summers & Barber, 2010). In their manual on cognitive therapy (CT) for patients with PD, Beck, Freeman, and Davis (2004) stress the importance of targeting PD symptoms themselves, even if amelioration of the patient’s acute, non-PD symptoms (e.g., depressive symptoms) is the initial goal of treatment. The authors argue that insofar as PD symptoms persist, even following the remission of non-PD symptoms, the patient is at risk of relapse. For example, a patient with a comorbid obsessive-compulsive PD whose depression symptoms have improved may continue to derive little satisfaction from events or circumstances that do not meet their unrealistically high standards. If the latter PD symptoms are not addressed, this interpretive style may place the patient at risk of a depression relapse.
Cognitive therapists purport that patients with a PD tend to hold maladaptive core beliefs whose content is specific to their specific PDs (Beck, Freeman, & Davis, 2004; Beck & Haigh, 2014). A patient with a paranoid PD might believe: “People will take advantage of me if I give them the chance” or “The world is a dangerous place and I have to be on guard at all times.” In CT, such core beliefs or schemas are assumed to underlie the maladaptive behaviors, interpersonal patterns, and negative emotions characteristic of PD patients (Beck et al., 2004). Adding support to the notion that maladaptive core beliefs underlie PDs, the Personality Beliefs Questionnaire (PBQ; Beck & Beck, 1991; Butler, Beck, & Cohen, 2007) has been shown to distinguish patients with versus those without a PD (Fournier, DeRubeis, & Beck, 2012; see Bhar, Beck, & Butler, 2012 for a review). The PBQ also can partially distinguish between specific PDs on the basis of endorsed beliefs (Fournier, DeRubeis, & Beck, 2012). Clinical recommendations by Beck advocate that, early on in treatment, CT clinicians should focus on identifying and beginning to adapt a given PD patient’s core beliefs, in an effort to promote lasting symptom relief and improvements in psychosocial functioning (Beck, Freeman, & Davis, 2004; Beck & Haigh, 2014).
Although the prescriptions in the clinical literature are relatively clear, there have been few attempts to test theoretically-supported models of PD treatment outside of that for borderline PD (for a BPD treatment review see Levy, Meehan, & Yeomans, 2012). Findings from three randomized trials provide evidence regarding the efficacy of Beck’s CT for PD in the treatment of Cluster-C PDs (Emmelkamp et al., 2006; Muran, Safran, Samstag, & Winston, 2005; Svartberg, Stiles, & Seltzer, 2004). For example, Svartberg and colleagues (2004) found substantial, stable reductions in PD symptomatology over the course of a 2-year follow-up in patients with mixed Cluster C diagnoses. In addition, schema-focused therapy (Young, Klosko & Weishaar, 2003) and manualized psychodynamic therapies (PDT) have been found to have efficacy in the treatment of Cluster-C diagnoses (Bamelis, Evers, Spinhoven, & Arntz, 2014; Barber, Muran, McCarthy, & Keefe, 2013; Leichsenring et al., 2015).
However, generally these trials have not targeted specific PDs and tend to compare two specialized, bona fide treatments (Wampold et al., 1997; cf. Budge et al., 2013) rather than use a control group (see Bamelis et al., 2014 for a notable exception), which is reflected in the fact that no treatment for a non-BPD PD currently meets APA Division 12 criteria to be an “evidence-based treatment.” One disadvantage to comparing specialized therapies head-to-head without an active control group or a dismantling design (e.g., that therapists cannot use a particular technique in one group but are encouraged to in the other) is that it is unclear to what extent techniques uniquely provided or emphasized by a given specialized therapy for PD (e.g., affect-focused PDT for Cluster-C patients; McCullough et al., 2003) are responsible for any observed change.
Even without the use of a dismantling study or an active control group, psychotherapy process research can provide unique insights into the relationship between patient outcomes and the use of particular therapeutic techniques thought to be crucial to the treatment of a PD. However, process research concerning CT and other psychotherapies for PD has typically not focused on questions of technique use in PD therapies. Instead, such research has focused on in-session processes involving, for example, therapist broad focus on affect (Ulvenes et al., 2012), changes in patient representations of self and other (Berggraf et al., 2014), gains in psychodynamic insight (Johansson et al., 2010; Kallestad et al., 2010), therapist competence in assigning homework (Ryum, Stiles, Svartberg, & McCullough, 2010), and the resolution of ruptures in the therapeutic alliance (Muran et al., 2009; Strauss et al., 2006).
For PDT specifically, however, a growing body of experimental research has investigated whether therapist use of transference interpretation tends to foster change for personality-disordered patients (Clarkin, Levy, Lenzenweger, & Kernberg, 2007; Johansson et al., 2010; Høglend et al., 2011; for a review see Høglend, 2014). By contrast, to date no study has tested whether particular CT techniques ostensibly emphasized in successful PD trials—specifically the identification and modification of core beliefs—may also be especially therapeutically beneficial for patients with a PD.
Objectives
The aim of this investigation is to examine, for the first time, the relation between CT techniques theorized to be core to the treatment of PD (i.e., identifying and adapting core beliefs), and symptom improvement among patients with and without a PD. Our primary hypothesis is that early focus on beliefs will predict subsequent symptom change among patients with – but not among those without – a PD co-morbidity. From a CT conceptualization, early focus on core beliefs may be particularly important for patients with a PD, as these beliefs are theorized to underlie and ultimately generate PD symptoms, as well as contribute to depressive symptoms (Beck, Freeman, & Davis, 2004). On the other hand, for patients without a PD comorbidity, the use of CT-Belief focused interventions at an early stage of therapy might be considered less appropriate, insofar as the etiology of their presenting symptoms are less strongly tied to underlying core beliefs (Fournier, DeRubeis, & Beck, 2012).
In previous investigations of CT for depression, greater adherence to symptom- or problem-focused “CT-Concrete” techniques (e.g., identifying and challenging specific negative automatic thoughts, use of thought records) has been associated with greater subsequent depressive symptom improvement (DeRubeis & Feely, 1990; Feely, DeRubeis, & Gelfand, 1999). Given the entrenched nature of dysfunctional beliefs underlying personality pathology, a focus on CT-Concrete techniques may be less effective for PD patients, relative to non-PD patients who may be better at reality-testing and perspective-taking (Fournier, DeRubeis, & Beck, 2012; cf. Semerari et al., 2014). Consequently, we further hypothesized that the effects of CT-Concrete techniques on symptom change would be moderated by PD status, such that a stronger relationship of CT-Concrete would be observed in patients without a PD, relative to patients with a PD.
Methods
Participants
Patients
The present study is a secondary analysis of patients randomized to the CT condition (N = 60) of a clinical trial that included patients with moderate to severe depression randomized between CT, antidepressants, and placebos (DeRubeis et al., 2005; Hollon et al., 2005). Local institutional review board (IRB) approval was obtained, and all patients provided written informed consent.
To be included in the trial, patients had to qualify for a current major depressive episode (MDE) as assessed by the Structured Clinical Interview for DSM-IV Diagnosis (Axis I; First et al., 1997), and score at least a 20 on the modified 17-item Hamilton Rating Scale for Depression (HRSD; Reimherr et al., 1998) at both a screening and baseline assessment, which were separated by at least 7 days. MDE diagnostic and HRSD severity criteria were established in the original trial to be consistent with the definition of “more severely depressed” set by the National Institute of Mental Health Treatment of Depression Collaborative Research Program (Elkin et al., 1989). Both the HRSD symptom ratings (ICC = 0.96) and MDE diagnoses (κ = 0.80) were reliably rated, and all diagnoses were confirmed by an experienced research psychiatrist. Exclusion criteria included any history of bipolar disorder, psychosis, substance abuse or dependence requiring treatment, and any Axis I disorder deemed primary over MDD. Patients diagnosed with schizotypal PD, borderline PD, or antisocial PD were also excluded from the trial, as these PDs were judged to require specialized and prolonged treatment specific to these conditions that could not take place in the course of this trial. Additional study details have been described in previous publications (DeRubeis et al., 2005; Hollon et al., 2005). One patient dropped out of the CT condition after the first session and was therefore excluded from analysis in this study, reducing the sample to n = 59.
Therapists
Four male and two female clinicians (three therapists at each site) served as cognitive therapists. Five of the therapists were licensed PhD psychologists, and one was a psychiatric nurse practitioner (MSN). Four of the therapists had extensive CT experience (7–21 years) prior to the initiation of the study. Two of the therapists started the study with 2 years of CT experience and received additional training from the Beck Institute for Cognitive Therapy during the trial. All therapists followed procedures outlined in standard texts of cognitive therapy for depression (Beck, Rush, Shaw, & Emery, 1979) and comorbid personality disorders (Beck, Freeman, & Davis, 2004). Guidelines called for 50-minute sessions to be held twice weekly for the first 4 weeks of treatment, once or twice weekly for the middle 8 weeks, and once weekly for the final 4 weeks.
At each site, therapists met together weekly for 90 minutes for supervision. Each site had a separate psychotherapy supervisor who had a high degree of experience in supervising CT for depression (≥15 years) and were each founding fellows of the Academy of Cognitive Therapy. Supervisors for each site consulted regularly with the other.
Outcome Indices
Beck Depression Inventory (BDI-II; Beck et al., 1996)
The BDI-II is a commonly-used 21-item self-report measure of depressive symptoms. Excellent psychometric properties are generally reported for the measure (Beck et al., 1996). The BDI-II was administered prior to each therapy session, and at every scheduled study assessment. Subsequent change was defined as the decrease (or increase) in the BDI-II score between two administrations: (1) just prior to the session in which therapist technique use was assessed; and (2) the Week 16 (termination) assessment. The BDI-II was used for the primary analysis over the Hamilton Rating Scale for Depression due to the BDI-II administration’s co-occurrence with process measurements. Information for patients who dropped out of treatment subsequent to Session 3 was retained using a last-observation carried forward method. 5 out of 26 (19.2%) of PD patients dropped out before treatment termination, compared to 4 out of 33 (12.1%) of non-PD patients.
Treatment Response on the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960)
The HRSD was assessed at intake, and treatment weeks 1–4, 6, 8, 10, 12, 14, and 16 (Hamilton, 1960). The dichotomous outcome of HRSD treatment response was analyzed, as per an a priori trial definition based on the 17-item HRSD scores (<citation masked>). In this trial, a clinical response was defined as completion of the 16-week acute treatment phase and either:
a week 16 HRSD score of 12 or lower and either a week 14 score of 14 or lower or a week 10 and 12 score of 12 or lower or;
a score of 12 or lower across weeks 12 to 16.
To be designated a clinical responder required multiple measurements of lower-severity HRSD scores to ensure stability of depression symptom relief. Criteria were developed as per absolute symptom level rather than percentage change such that no patient could be classified as a responder while concurrently having a relatively high end-state symptom burden (DeRubeis et al., 2005; Hollon et al., 2005). Although dichotomizing continuous variables can proffer biased estimates in regression (MacCallum, Zhang, Preacher, & Rucker 2002), we included the HRSD response outcome as a secondary analysis to provide an additional perspective on the clinical significance of any observed process relationship (i.e., are patients more likely to end up relatively non-depressed under certain circumstances?).
Structured Clinical Interview for Diagnosis of Axis-II Disorders (First et al., 1997)
Presence of a personality disorder was assessed at intake and treatment termination via the Structured Clinical Interview for the DSM-IV Personality Disorders (SCID-II; First et al., 1997). Twenty-six patients (44%) qualified for a comorbid PD, whereas thirty-three patients (56%) did not. The SCID-II is a commonly used structured diagnostic interview for the assessment of personality disorders as per DSM-IV criteria. Adequate to excellent inter-rater reliability on both diagnosis and number of criteria met is typically reported for trained users of the measure (Maffei et al., 1997; Lobbestael, Leurgans, & Arntz, 2011). Both the presence/absence of each PD and the number of criteria met for each PD were recorded. All diagnoses made by research assessors were confirmed by an experienced research psychiatrist.
Data from the SCID-II termination assessment were unavailable for four PD and four non-PD patients, leaving 51 patients with a termination SCID-II. Two late dropout PD patients attended a final assessment session, while the SCID-II was not available for one treatment completer PD patient who was an HRSD responder. Remaining missing SCID-II assessments were due to treatment dropout.
Process Measures
Collaborative Study Psychotherapy Rating Scale (CSPRS; Hollon et al., 1988)
The CSPRS (CSPRS; Hollon et al., 1988) is an observer-rated instrument initially developed to measure treatment integrity of cognitive therapy, interpersonal therapy, and psychiatric clinical management in the National Institute of Mental Health Treatment of Depression Collaborative Research Program (Elkin et al., 1989). In the current study, we employed the CSPRS’s CT scale, which assesses the degree to which therapists used specific CT techniques. The use of each technique was rated on a 7-point Likert scale ranging from 0 (technique not present in this session) to 6 (technique applied fully and comprehensively in session). Note that the CSPRS measures the extent or degree to which particular CT techniques were observed in-session, and is not a measure assessing the competence or skill with which these techniques were implemented (for a commonly used measure of CT competence, see Cognitive Therapy Scale; Young & Beck, 1988).
The CT-Concrete subscale consists of 10 items within the CT scale concerning directive, symptom-focused techniques in CT, such as assigning cognitive-behavioral homework, and identifying and addressing cognitive distortions and negative automatic thoughts (DeRubeis & Feeley, 1990). For the present inquiry we identified a CT-Belief subscale comprising four items that describe interventions that focus on identifying, assessing, and challenging patients’ core beliefs. These items were #58: “Did the therapist probe for beliefs related to a thought the client reported [so as] to explore the personal meaning associated with the client’s initial thought?”; #60: “Did the therapist explore with the client a general belief that underlies many of the client’s specific negative thoughts and beliefs?”; #65: “Did the therapist work with the client to determine what the realistic consequences would be if the client’s belief proved to be true?”; and #66: “Did the therapist guide the client to consider whether or not maintaining a specific belief is adaptive for the client (regardless of whether or not it is accurate)?”
Early session tapes were rated using the CSPRS by five advanced undergraduate psychology majors at <institution masked>. A graduate student who led the project (<author masked>) and was not one of the raters provided 30 hours of training to each rater. Training included a review of both the rater manual (Hollon et al., 1988) and a CT manual (Beck, J.S., 1995). Members of the project team met weekly to rate a tape collectively in an effort to prevent rater drift. All session tapes were masked for patient identity (e.g., clinical comorbidities, treatment course) and were given a random number. Tapes were assigned to raters using a balanced incomplete block design (Fleiss, 1981) such that each rater was paired with each of the other 4 raters an equal number of times, and each rater rated no more than one session per therapist-patient dyad. Whenever session 3 was available (52 of the 59 cases) it served as the “early” session; otherwise the recording of session 2 (4 times) or 4 (3 times) was used.
Random effects ICCs were calculated using variance estimates from an REML mixed model in the R package “lme4” (Bates et al., 2014). The reliability model followed Shrout and Fleiss (1979)’s [2, 2] model for the case of scores pooled between two raters. Adequate reliability was estimated for both the Concrete (ICC = .76) and Belief (ICC = .70) subscales. CT-Concrete and CT-Belief were significantly correlated (r = 0.30, p = 0.023), reflecting a moderate degree of collinearity.
Statistical Analyses
All analyses were conducted using the R statistical programming language (version 3.0.1; R Core Team, 2014). The primary analysis examined change on the BDI-II subsequent to the process-measured session was modeled using linear regression. Two secondary analyses were conducted. The odds of a patient meeting HRSD treatment response criteria were modeled using logistic regression. We also tested a linear model in which the number of SCID-II PD criteria met in the post-treatment interview served as the dependent variable, with the number of PD criteria met at intake included as a covariate. Analyses of PD criteria included only those individuals for whom a termination SCID-II (n = 51) was available, whereas the two analyses of depression outcomes included all patients with a CSPRS measurement (n = 59).
All analyses were run using robust regressions (Huber & Ronchetti, 2009) as implemented in the R package “Robustbase” (v. 0.90-2; Rousseuw et al., 2014). Given the sample size (n = 59), robust regression was selected over standard regression for its superior properties of robustness against multivariate outliers and in cases of deviation from homoscedasticity. A robust regression: (1) retains full information on all observations in an initial estimate of parameters; (2) iteratively determines weights for each observation based on a particular estimator function from this initial estimate, such that points much farther from model predictions in the previous iteration are given lower weight; and (3) re-calculates final parameter estimates based on the final weighting when the values of the coefficients converge within a specified tolerance (Huber & Ronchetti, 2009).
In order to test models predicting continuous symptom change outcomes (i.e., BDI-II change, PD criteria), settings for the linear robust regressions were made as per Koller and Stahel (2011). Semi-partial correlation effect sizes (i.e., semi-pr) for parameters of interest were estimated. For dichotomous outcomes (i.e., HRSD response) robust generalized regressions were performed with a Huber function with parameters set as per Cantoni and Ronchetti (2001).
Covariates and predictors that were included across all analyses were: (1) the BDI-II score collected at the beginning of the rated session; (2) the difference in BDI-II score between intake and the rated session; and (3) the CT-Concrete and CT-Belief subscale totals, as main effects as well as interaction terms with PD co-morbidity status (PD vs. non-PD). The interaction between the CT-Belief subscale and PD status represents our main moderator of interest, testing whether a focus on beliefs is a stronger predictor of outcomes for patients with PD.
Results
Patient Characteristics
PDs represented in the sample
The average number of PD diagnoses among the 26 patients with at least one PD diagnosis was 1.69 PDs (SD = 0.88, median = 1, mode = 1). The majority of patients with a PD (16) had at least 1 Cluster-C disorder, the most common being obsessive-compulsive PD (9) and avoidant PD (8). Only three patients were diagnosed with a Cluster-A disorder (all paranoid PD), and only one patient met criteria for a Cluster-B disorder (narcissistic PD). Nine patients were diagnosed with Personality Disorder-Not Otherwise Specified (PD-NOS). The PD-NOS patients, on average, met 5.3 Cluster B criteria, 3.9 Cluster C criteria, and 2.1 Cluster A criteria. Additional PD criteria information for both PD and non-PD patients can be found in Table 1.
Table 1.
Personality Disorder Characteristics of CT Patients with and without Personality Disorder
| SCID-II PD Criteria Met | No PD (n=33) | PD (n=26) |
|---|---|---|
| Avoidant** | .70 (.92) | 2.35 (2.47) |
| Obsessive-Compulsive*** | 1.27 (1.07) | 3.04 (2.23) |
| Dependent* | .36 (.65) | 1.19 (1.67) |
| Borderline*** | .58 (.97) | 1.92 (1.29) |
| Narcissistic† | .48 (.94) | 1.08 (1.41) |
| Histrionic | .21 (.49) | .42 (.90) |
| Antisocial | .12 (.42) | .35 (.69) |
| Paranoid** | .39 (.61) | 1.50 (1.61) |
| Schizotypal | .21 (.60) | .38 (.64) |
| Schizoid | .18 (.73) | .27 (.53) |
| Cluster A* | .79 (1.56) | 2.15 (2.22) |
| Cluster B*** | 1.39 (1.78) | 3.77 (2.70) |
| Cluster C*** | 2.33 (1.71) | 6.58 (3.70) |
| Total Number of Criteria Met*** | 4.52 (3.94) | 12.50 (5.1) |
Note. All values reported as the group mean (standard deviation).
p <.10;
p <.05;
p <.01;
p <.001
Differences between PD and non-PD patients
PD patients did not differ at intake from non-PD patients on depressive symptom severity (see Table 2), but significant differences were observed on some clinical and demographic variables. Relative to non-PD patients, PD patients reported earlier ages of onset of depression (t[57] = −3.51, p <.001, d = 0.93), more prior episodes of depression (t[57] = 3.51, p <.001, d = 0.93), and higher scores on the Dysfunctional Attitudes Scale (t[57] = −2.25, p = 0.029, d = 0.57).
Table 2.
Characteristics of the CT Patient Sample per Personality Disorder Co-morbidity
| No PD (n=33) | PD (n=26) | |
|---|---|---|
| Age † | 42.4 (13.1) | 37.3 (8.7) |
| Gender (% Female) | 66.7% | 46.2% |
| Caucasian (% Yes) | 78.8% | 76.9% |
| Unemployed | 15.1% | 30.8% |
| Years of Education | 14.5 (2.8) | 14.5 (2.1) |
| IQ | 109.3 (13.1) | 109.8 (9.1) |
| Intake BDI-II | 30.8 (9.3) | 31.1 (8.0) |
| Intake HRSD | 23.4 (2.5) | 25.9 (4.2) |
| BDI-II at Session 3† | 22.2 (9.7) | 27.4 (10.3) |
| BDI-II Change Prior to Session 3† | 8.5 (11.1) | 3.7 (8.0) |
| Total BDI-II Change† | 20.6 (11.3) | 14.5 (12.5) |
| Age at Depression Onset*** | 28.8 (13.5) | 17.9 (9.3) |
| Number of Prior Episodes*** | 1.6 (1.4) | 3.3 (2.3) |
| Number of Prior Treatments | 1.6 (1.7) | 1.9 (2.0) |
| Chronic Depression (% Yes) | 36.4% | 53.8% |
| Recurrent Depression (% Yes) | 69.7% | 84.6% |
| Dysthymia (% Yes) | 24.2% | 23.1% |
| Intake HRSA | 17.9 (7.5) | 15.5 (5.8) |
| Intake Beck Hopelessness Scale† | 10.2 (5.3) | 12.6 (4.9) |
| Intake Dysfunctional Attitudes Scale* | 134.4 (35.5) | 158.6 (33.9) |
| Session 3 CT-Concrete | 22.5 (6.2) | 20.7 (5.6) |
| Session 3 CT-Belief | 2.2 (2.0) | 2.5 (2.2) |
Note. BDI-II = Beck Depression Inventory-II; HRSA = Hamilton Rating Scale for Anxiety; HRSD = Hamilton Rating Scale for Depression; All values reported as the group mean (standard deviation); All binary variables tested with an exact χ2 test
p <.10;
p <.05;
p <.001
Non-PD patients experienced greater symptomatic change (on the BDI-II) prior to Session 3, at the level of a non-significant trend (t[57] = 1.87, p = 0.067, d = 0.50, mean difference = 4.81), in addition to experiencing greater total BDI-II change (d = 0.52; see Table 2). Despite being nonsignificant (potentially due to the low power of comparison), these differences in early and total outcome were notably of a medium effect size (Cohen, 1992), and are consistent with the literature on the negative prognostic impact of having a personality disorder in depression treatment (Newton-Howes et al., 2014).
Potential confounds between pre-treatment characteristics, technique use, and symptom change
We examined the relationships of nine variables that could represent confounds in analyses of technique use, inasmuch as they could predict both the course of symptom change and techniques used at the measured session (i.e., “3rd variable” confounds). These potential confounders could indicate trivial links by which any association between levels of technique use and outcome may be epiphenomenal, which could inform the need for additional statistical controls in the analyses. We selected nine such variables, including those that referred to the patient’s disease history (number of prior episodes; Gorwood et al., 2010; number of prior treatments; Rush et al., 2006), intake symptom levels (e.g., depression scores; Driessen, Cuijpers, Hollon, & Dekker, 2010; anxiety scores; Forand et al., 2011), PD criteria met at intake (Gorwood et al., 2010; Newton-Howes et al., 2014), and both change in BDI-II prior to the measured session (indicating early symptom trajectory) and the level of symptoms at the measured session.
Of the 18 correlations (9 variables, each with CT-Belief and CT-Concrete), none was significant and only one met the threshold for a non-significant trend (see Table 3). Thus, we included only BDI-II symptom levels at Session 3 and BDI-II change prior to the Session 3 as pre-specified method covariates across all analyses.
Table 3.
Pearson Correlations between Pre-Prediction Clinical Variables and Technique Ratings at Session 3
| CT-Concrete | CT-Belief | |
|---|---|---|
| Intake BDI-II | 0.07 | 0.11 |
| Intake HRSD | −0.23† | −0.19 |
| Intake HRSA | −0.15 | −0.04 |
| Intake Beck Hopelessness Scale | 0.09 | 0.03 |
| Change Prior to Session 3 | 0.05 | −0.03 |
| BDI-II at Session 3 | 0.01 | 0.11 |
| Total PD Criteria | 0.02 | 0.14 |
| Number of Prior Episodes | −0.10 | 0.08 |
| Number of Prior Treatments | −0.17 | −0.05 |
Note. BDI-II = Beck Depression Inventory-II; HRSA = Hamilton Rating Scale for Anxiety; HRSD = Hamilton Rating Scale for Depression; PD = Personality Disorder.
p <.10
Predicting Change in the BDI-II
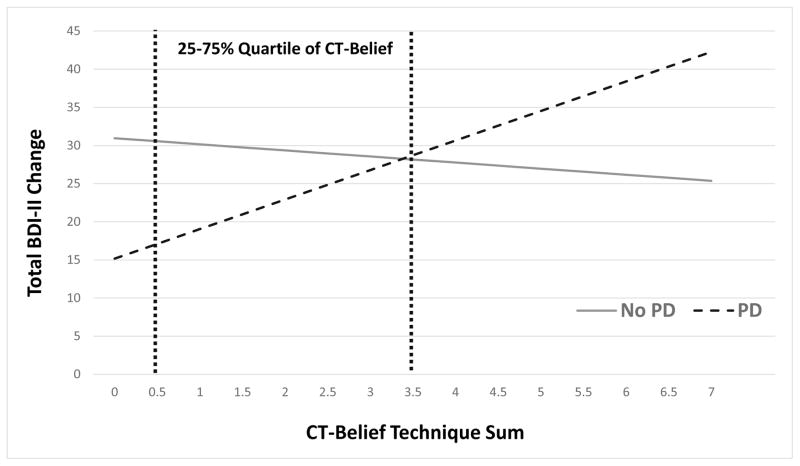
A significant interaction was found between CT-Belief techniques and PD co-morbidity, such that greater early use of CT-Belief techniques was predictive of more subsequent BDI-II change among patients with a PD than among those without a PD (B = 4.67 [95% CI: 2.88 to 6.47], SE = 0.89, t[51] = 5.22, p < .001, semi-pr = 0.46; see Figure 1 for estimated slopes; see Table 4). The simple slope of BDI-II change as a function of CT-Belief was significant in the PD co-morbid group such that higher CT-Belief predicted more subsequent change on the BDI-II (B = 3.87 [95% CI: 2.59 to 5.16], SE = 0.64, t[51] = 6.07, p < .001, semi-pr = 0.53). By contrast, the simple slope in the non-PD group was nonsignificant (B = −0.80 [95% CI: −2.04 to 0.45], SE = 0.62, t[51] = −1.29, p = 0.204, semi-pr = −0.11) suggesting that in this group there was no relationship between CT-Belief and subsequent symptom change.
Figure 1.
Estimated slopes of subsequent BDI-II change as a of personality disorder co-morbidity status and rated sum CT-Belief techniques at session 3. For these estimates, modelled variables that were not directly represented (prior change, BDI at session of measurement, CT-Concrete techniques) were set to the respective means for No PD and PD patients. Because PD patients’ average change on the BDI-II prior to session 3 was 3.7, whereas non-PD patients’ average change was 8.5, the respective averages were added to the modeled subsequent BDI-II change values so that the curves represent estimates of total BDI-II change, modeled for each group. Representations of the relations between CT-Belief and subsequent change were thus preserved, but the values on the ordinate include BDI-II change prior to session 3 across the full range of the abscissa.
Table 4.
Semi-Partial Correlations between Technique Ratings at Session 3 and either Subsequent BDI-II Change or Total PD Criteria Change
| Simple Slope (PD) | Simple Slope (No PD) | Interaction with PD | |
|---|---|---|---|
| BDI-II Change | |||
| CT-Belief | 0.53*** | −0.11 | 0.46*** |
| CT-Concrete | −0.04 | 0.26** | −0.20* |
| PD Criteria Change | |||
| CT-Belief | 0.29* | −0.16 | 0.33* |
| CT-Concrete | 0.25† (full sample) | 0.00 | |
Note. Positive semi-partial correlations indicate a positive relationship between increasing technique ratings and symptom improvement.
p <.10;
p <.05;
p <.01;
p <.001
In the same model, the test of the interaction of PD status and CT-Concrete was significant (B = −0.71 [95% CI: −1.35 to −0.08], SE = 0.32, t [51] = −2.26, p = 0.028, semi-pr = −0.20). Simple slope analyses by PD status revealed no association between CT-Concrete and subsequent change in the PD group (B = −0.12 [95% CI: −0.61 to 0.38], SE = 0.25, t[51] = −0.48, p = 0.64, semi-pr = −0.04), whereas in the non-PD group there was a significant, positive association (B = 0.60 [95% CI: 0.20 to 1.00], SE = 0.20, t[51] = 3.01, p = 0.004, semi-pr = 0.26).1,2
Predicting HRSD Treatment Response
Overall, 23 of 33 non-PD patients (69.7%) met criteria for an HRSD response, compared with 12 of 26 PD patients (46.2%). Among neither the HRSD responders nor the non-responders was a difference observed between PD and non-PD patients in average HRSD scores (means 6.8 and 6.3 for PD and non-PD responders; 18.5 and 17.0 for PD and non-PD non-responders). A test of the interaction of PD status by responder status on HRSD scores was non-significant (F[1, 55] = 0.12, p = 0.73).
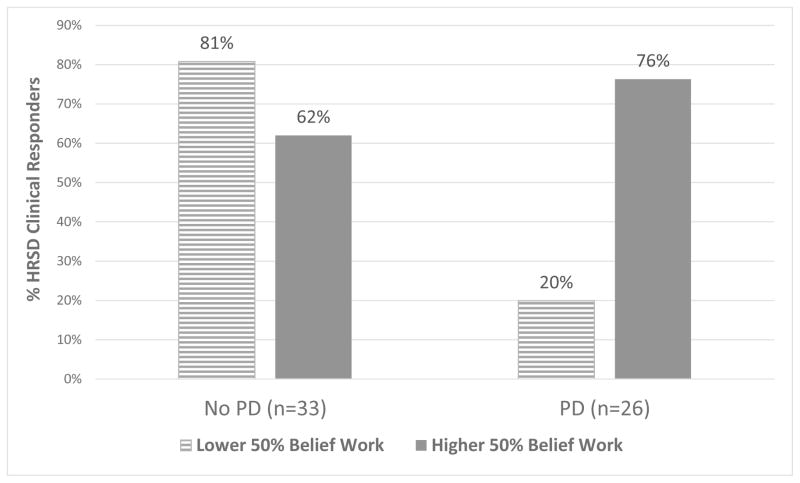
In a full model, the interaction of CT-Concrete and PD status in predicting meeting HRSD response was nonsignificant (p = 0.341), and was therefore not included in a reduced, final model. In this final model, there was a significant interaction between CT-Belief techniques and PD co-morbidity, such that greater use of CT-Belief techniques was more predictive of meeting clinical response criteria among patients with a PD (log odds = 2.28 [95% CI: 0.68 to 3.88], SE = 0.82, z = 2.79, p = 0.005; see Figure 2 for an illustration). There was a significant simple slope of CT-Belief techniques in the PD group such that increased levels of early belief work significantly predicted attaining a clinical response (log odds = 1.33 [95% CI: 0.24 to 2.42], SE = 0.55, z = 2.40, p = 0.016). Conversely, there was a significant simple slope in the non-PD co-morbid group such that increased CT-Belief work was associated with decreased odds of response (log odds = −0.95 [95% CI: −1.70 to −0.20], SE = 0.38, z = −2.49, p = 0.013). A main effect of CT-Concrete techniques was found, such that increasing levels of CT-Concrete techniques predicted higher odds of treatment response irrespective of PD status (log odds = 0.27 [95% CI: 0.06 to 0.46], SE = 0.10, z = 2.60, p = 0.009).
Figure 2.
Clinical response (percentages estimated by the model’s output) as a function of personality disorder co-morbidity and receiving CT-Belief techniques at session 3 in the lower 50% versus higher 50% of the CT-Belief distribution for the total sample. For these estimates, modelled variables that were not directly represented (prior change, BDI at session of measurement, CT-Concrete techniques) were set to the respective means for No PD and PD patients.
Predicting Change in PD Criteria
In a full model, the interaction of CT-Concrete and PD status was nonsignificant (p = 0.696). It was therefore not included in a final, reduced model.
In this final model, a significant interaction between CT-Belief and PD status indicated that CT-Belief was more strongly related to a reduction in PD criteria among PD patients, relative to non-PD patients (B = −1.31 [95% CI: −2.34 to −0.27], SE = 0.51, t[43] = −2.55, p = 0.015, semi-pr = 0.33). This was reflected by a significant simple slope in the PD group wherein higher CT-Belief scores predicted fewer end-state PD criteria (B = −0.85 [95% CI: −1.61 to −0.08], SE = 0.38, t[43] = −2.23, p = 0.031, semi-pr = 0.29), whereas the simple slope in the non-PD group was nonsignificant (B = 0.46 [95% CI: −0.25 to 1.17], SE = 0.35, t[43] = 1.31, p = 0.196, semi-pr = −0.16). In this model, a trend-level main effect of CT-Concrete techniques was also obtained; higher levels of CT-Concrete techniques predicted fewer PD criteria at termination among both PD and non-PD patients (B = −0.19 [95% CI: −0.41 to 0.02], SE = 0.11, t[43]= −1.81, p = 0.077, semi-pr = 0.25).3
Covariation of PD Change and Depression Change
12 out of 22 (54.5%) of PD patients with a termination SCID-II measurement qualified for any PD at treatment termination. Among the 22 PD-comorbid patients with a termination SCID-II, a strong connection was observed at termination between meeting the depression response criteria (on the HRSD) and no longer meeting criteria for any PDs (exact χ2[1] = 11.73, rφ = −0.73 [95% CI: −0.91 to −0.45], p = 0.002). Only 1 of the 11 PD-comorbid patients who met the HRSD response criteria was given a PD diagnosis at treatment termination. Moreover, only 2 of the 12 patients who no longer met full criteria for any PD diagnosis at termination were not also an HRSD responder. A large partial correlation was also observed between change in BDI-II score and change in PD criteria, controlling for intake symptom severity in each (pr = 0.68 [95% CI: 0.23 to 0.93], p = 0.001).
Discussion
This is the first study to examine the differential efficacy of cognitive therapy techniques for the treatment of depression in patients with and without a personality disorder. Results were consistent with a theory highlighting the therapeutic benefit of techniques focused on dysfunctional core beliefs for patients with personality disorders (Beck, Freeman, & Davis, 2004).
For patients with PD, higher early belief-focused cognitive work was associated with medium-to-large effect size improvements in symptoms as measured by the BDI-II and number of PD criteria endorsed, and was associated with higher odds of ending treatment with mild-severity HRSD symptoms at worst. That this pattern was either absent or opposite in direction among patients without a PD highlights the specificity of this relationship to those with personality pathology. The magnitude of the primary technique-outcome correlation of CT-Belief techniques for PD patients (semi-pr = 0.53) found in this sample was larger than that of all general CBT technique-outcome correlations reported in the only meta-analysis on this topic (Webb, DeRubeis, & Barber, 2010). To some extent, this may reflect a unique link between specific technique use (i.e., early belief focus in CT) and outcome among patients with a comorbid MDD-PD—that is to say, a detectable clinical benefit of matching treatment interventions to the particular needs of a distinctive patient population.
From one perspective, early focus on beliefs may be particularly efficacious for the PD subgroup because such a focus targets the core maladaptive schemas that characterize this patient population (Beck et al., 2001; Fournier, DeRubeis, & Beck, 2012). Modifying core beliefs may lead to long lasting cognitive, emotional, and behavioral change, as the patient perceives external situations as well as internal thoughts, feelings, and desires more flexibly and adaptively. On the other hand, it may be the case that less reactant patients may benefit more from early directive interventions, whereas more reactant patients such as those with PDs (Seibel & Dowd, 2001) may benefit more from non-directive interventions (Beutler et al., 2011). Under this hypothesis, CT-Concrete techniques probing the validity of thoughts and interpretations, if deployed early in treatment when working with PD patients, may be sometimes misperceived as personal criticism. By contrast, CT-Belief techniques engage patients in exploratory considerations of the nature, underlying meaning, and functionality of their general beliefs, which may be perceived by a PD patient as less directive than concrete cognitive work. To help resolve how focus on beliefs may be efficacious in treatment, trials of CT for PD should examine, via time-lagged mediational analyses, the extent to which change in beliefs appear to mediate change in PD symptomatology.
One reason for the consistency across analyses of change in mood and personality pathology is that amelioration in one domain tracked very closely remission in the other. With only three exceptions, PD patients either met response criteria on the HRSD and achieved remission on all PDs, or neither of these positive outcomes occurred. This is consistent with the perspective that for patients with PDs, reductions in PD symptoms often results in improvement in depressive symptoms (i.e., PD problems give rise to depression; depression subsides after PD problems begin to ameliorate; Gunderson et al., 2004). Alternatively, it could be that when problems with mood are addressed, personality pathology subsides (i.e., PD symptoms as primarily mood-reactant), or remains present but is no longer detectable (at least with present measures). On the other hand, recent longitudinal modeling of PD patients with and without comorbid MDD suggests that stability of most PD criteria may be less mood-dependent than has previously been thought (Morey et al., 2010). Repeated assessments of PD symptoms and symptoms of depression could help elucidate the directionality of the relationship between change in PD phenomenology and depression symptoms.
Notably, in the PD patient sample investigated in this study, only 17% of those PD patients who met clinical response criteria by treatment termination relapsed over the course of a one-year follow-up, compared to 40% among non-PD patients who responded to CT, indicating that PD patients who responded to treatment tended to hold onto their therapeutic gains (Fournier et al., 2008). Regardless of the mechanism, the current study suggests that PD patients who attained and maintained a clinical depression response tended to be those who both received higher early CT-Belief technique focus and who dropped below the diagnostic threshold for their PD.
Conversely, the secondary hypothesis that early CT-Concrete focus would not be as strongly associated with change for PD patients was not supported, with mixed findings regarding the predictive validity of early CT-Concrete focus for this group. In particular, while there was no effect of CT-Concrete on subsequent BDI-II change for PD patients, main effects of CT-Concrete (i.e., collapsing across the PD and non-PD groups) emerged in the logistic analyses predicting HRSD treatment response and the analyses predicting end-state PD criteria. Given this ambiguous set of findings, future research should examine contexts wherein more concrete focus is helpful for PD patients within CT. For example, competence in assigning homework in Cluster C PD treatment has been associated with greater therapeutic change (Ryum, Stiles, Svartberg, & McCullough, 2010), suggesting a role for PD-tailored cognitive-behavioral homework.
Limitations
Several limitations of this study should be noted. First, sample size was relatively limited, with 59 patients in total, 26 of whom were diagnosed with one or more PDs. Nevertheless, the present study had sufficient ability to detect the hypothesized PD status by CT-Belief interaction.
Second, given the observational nature of this study, certain unmeasured third variables (e.g., patient interpersonal styles) may have driven our findings by predicting both early technique use and subsequent outcome. However, this pattern would need to be especially complex to explain the observed CT-Belief by PD status interaction (i.e., there must be different third variable confounds operating for PD and non-PD patients to account for the differential association between technique use and symptom change between groups).
Third, some personality disorders were excluded from the trial (antisocial, borderline, and schizotypal), or were under-represented (e.g., narcissistic). Nevertheless, Cluster B traits—particularly borderline—were well-represented in the trial, as were paranoid traits (see Table 1). Thus, the results as they stand relate primarily to depression patients with Cluster C disorders and PD-NOS with Cluster B & C features, who together comprised the vast majority of the PD cohort and indeed are among the most common PDs diagnosed in depression patients (Friborg et al., 2014). Patients with other personality disorder diagnoses may require different, specialized clinical techniques, such as teaching affect- and impulse-regulation, as well as interpersonal effectiveness, skills for BPD patients (Linehan, 1993), or work on building reality testing capacities among Cluster A patients (Grant et al., 2012).
Lastly, there is nothing in our data to indicate why therapists chose specific interventions for individual patients in the trial—for example why some therapist-patient dyads focused more on belief work. Patients with personality disorders tend to evoke particular emotionality and responsiveness in their therapists (i.e., countertransference; Betan, Heim, Zittel Conklin, & Westen, 2005; Colli, Tanzilli, Dimaggio, & Lingiardi, 2014), which may influence technique use. Future research should examine how therapists choose particular interventions for different subsets of patients, as we know there can be substantial variability across therapist-patient dyads in the focus on different CT techniques (Webb et al., 2013; Sasso et al., in press). Such research may help therapists find ways to focus more on the therapeutic techniques that may be the most appropriate for their patients.
Future Directions and Conclusions
An early focus on core beliefs may be specifically advantageous for patients with a PD diagnosis in CT for depression, supporting theoretical writings concerning the importance of targeting a PD patient’s maladaptive core beliefs (Beck, Freeman, & Davis, 2004). CT clinicians treating depression patients with co-morbid PD should consider beginning to identify and work with their patients’ core beliefs relatively early in treatment. This recommendation is consistent with current clinical manualization of CT for PD (Beck, Freeman, & Davis, 2004), and positive findings from controlled trials of CT for PD in which such a focus was prescribed and generally applied (e.g., Svartberg, Seltzer, & Stiles, 2004). Future research may seek to replicate these findings (e.g., as a process-outcome study or dismantling components trial as in Høglend et al., 2011), to assess other therapeutic conditions that may influence the impact of belief work (e.g. competence, the therapeutic alliance), and to determine mediators of change in PD related to technique use (e.g., decreases in PD-specific beliefs).
Patients with a personality disorder form a uniquely impaired and prevalent subpopulation among patients with unipolar mood disorders. Further investigations into treating depression within this patient population should pay greater attention to disease processes that might distinguish these patients in clinically meaningful ways from other mood-disordered individuals. Continued empirical research as to specialized technique and process may inform more effective treatment strategies for this vulnerable patient group.
Public Health Significance Statement.
In cognitive therapy for depression, early therapeutic focus on core beliefs may be especially beneficial in treating mood and PD symptoms for patients with co-morbid Cluster C PDs and PD-NOS with Cluster C and B features. CT clinicians treating this population may wish to attend to their patients’ core beliefs relatively early in treatment.
Acknowledgments
The CPT-II trial (DeRubeis et al., 2005) was supported by National Institute of Mental Health (NIMH) Grants MH50129 (R10) (to Robert J. DeRubeis) and MH55875 (R10) and MH01697 (K02) (to Steven D. Hollon)
Footnotes
As a check for the LOCF-intention to treat method, the above model was re-run using only patients completing the trial, which included 21 PD patients and 29 non-PD patients. The results of the completer analysis did not differ notably from the LOCF analysis, with the chief interaction of PD Status x CT-Belief remaining significant at p <.001.
PD and non-PD patients differed significantly on several pre-treatment characteristics (see Table 2). To verify that the observed pattern of findings was driven chiefly by PD co-morbidity rather than by these other characteristics, a series of models was run that tested whether subsequent BDI-II change could be accounted for by interactions between CT techniques and characteristics that distinguished the two groups at a level of p <.10 or lower. Number of prior episodes interacted with CT-Concrete such that patients with more prior episodes experienced less benefit from increasing concrete technique use (p = 0.026), and with CT-Belief such that patients with more episodes were associated with increasing benefit of belief technique use (p = 0.031). Age of depression onset interacted at the level of a non-significant trend with CT-Belief such that later ages of onset were related to less CT-Belief benefit (p = 0.062). When simultaneously modeling the prior episodes interactions with the main interactions of technique and PD-Status, the interactions between CT-Belief and PD status (p < .001) and between CT-Concrete and PD status interaction (p = 0.032) remained significant. By contrast, neither prior episode interaction was significant (ps > 0.21). These findings are consistent with the notion that these additional variables are tracking PD status in moderating the effects of technique use, rather than driving the pattern of findings per se.
During the review process for this article, one reviewer recommended that we analyze the change in SCID-II criteria as a count variable, as this index reflects the number of individual PD criteria that was met by the patient met. We believe that the linear analyses are ultimately preferable, given the dimensional psychometric properties of SCID-II criteria (e.g., Maffei et al., 1997), the distribution of change scores in the study (which can be provided upon request), and the greater interpretability of linear model coefficients and standardized effect sizes. Nonetheless, we also analyzed the PD criteria data using a negative binomial regression, using robustness weights derived from a robust poisson regression (Cantoni & Ronchetti, 2001). In this framework, the primary interaction of PD status with CT-Belief remained significant (p = 0.001), as did the simple slope of CT-Belief techniques in the PD subgroup (p = 0.008) and a main effect of CT-Concrete techniques (p = 0.027). The only shift from analyzing the data in a negative binomial framework is that a nonsignificant trend emerged in the simple slope of CT-Belief techniques in the non-PD subgroup (p = 0.058), such that higher CT-Belief techniques predicted meeting relatively more SCID-II criteria by termination. This was in the same direction when analyzed in a linear framework, but p was >.100.
Contributor Information
John R. Keefe, University of Pennsylvania
Christian A. Webb, McLean Hospital/Harvard Medical School
Robert J. DeRubeis, University of Pennsylvania
References
- Bamelis LLM, Evers SMAA, Spinhoven P, Arntz A. Results of a multicenter randomized controlled trial of the clinical effectiveness of schema therapy for personality disorders. American Journal of Psychiatry. 2014;171:305–322. doi: 10.1176/appi.ajp.2013.12040518. [DOI] [PubMed] [Google Scholar]
- Barber JP, Muran JC, McCarthy KS, Keefe JR. Research on dynamic therapies. In: Lambert MJ, editor. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change. 6. Hoboken, NJ: Wiley & Sons; 2013. pp. 443–494. [Google Scholar]
- Bates D, Maechler M, Bolker B, Walker S, Christensen RHB, Singmann H. lme4: Linear mixed-effects models using Eigen and S4 (Version 1.1-5) 2014. [Google Scholar]
- Beck AT, Beck JS. The personality belief questionnaire. Bala Cynwyd, PA: The Beck Institute for Cognitive Therapy and Research; 1991. [Google Scholar]
- Beck AT, Freeman A, Davis DD. Cognitive therapy of personality disorders. 2. New York, NY: Guilford; 2004. [PubMed] [Google Scholar]
- Beck AT, Haigh EAP. Advances in cognitive theory and therapy: The generic cognitive model. Annual Review of Clinical Psychology. 2014;10:1–24. doi: 10.1146/annurev-clinpsy-032813-153734. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York, NY: Guilford; 1979. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the BDI-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck JS. Cognitive therapy: Basics and beyond. Guilford Press; New York, NY: 1995. [Google Scholar]
- Berggraf L, Ulvenes PG, Hoffart A, McCullough L, Wampold BE. Growth in sense of self and sense of others predicts reduction in interpersonal problems in short-term dynamic but not in cognitive therapy. Psychotherapy Research. 2014;24:456–469. doi: 10.1080/10503307.2013.840401. [DOI] [PubMed] [Google Scholar]
- Betan E, Heim AK, Zittel Conklin C, Westen D. Countertransference phenomena and personality pathology in clinical practice: An empirical investigation. American Journal of Psychiatry. 2005;162:890–898. doi: 10.1176/appi.ajp.162.5.890. [DOI] [PubMed] [Google Scholar]
- Beutler LE, Harwood TM, Michelson A, Song X, Holman J. Resistance/reactance level. Journal of Clinical Psychology. 2011;67:133–142. doi: 10.1002/jclp.20753. [DOI] [PubMed] [Google Scholar]
- Bhar SS, Beck AT, Butler AC. Beliefs and personality disorders: An overview of the personality beliefs questionnaire. Journal of Clinical Psychology. 2012;68:88–100. doi: 10.1002/jclp.20856. [DOI] [PubMed] [Google Scholar]
- Budge SL, Moore JT, Del Re AC, Wampold BE, Baardseth TP, Nienhuis JB. The effectiveness of evidence-based treatments for personality disorders when comparing treatment-as-usual and bona fide treatments. Clinical Psychology Review. 2013;33(8):1057–1066. doi: 10.1016/j.cpr.2013.08.003. [DOI] [PubMed] [Google Scholar]
- Butler AC, Beck AT, Cohen LH. The personality belief questionnaire-short form: Development and preliminary findings. Cognitive Therapy and Research. 2007;31:357–370. [Google Scholar]
- Caligor E, Kernberg OF, Clarkin JF. Handbook of dynamic psychotherapy for higher level personality pathology. Arlington, VA: American Psychiatric Publishing; 2007. [Google Scholar]
- Cantoni E, Ronchetti E. Robust inference for generalized linear models. Journal of the American Statistical Association. 2001;96:1022–1030. [Google Scholar]
- Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: A multiwave study. American Journal of Psychiatry. 2007;164:922–928. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Colli A, Tanzilli A, Dimaggio G, Lingiardi V. Patient personality and therapist response: An empirical investigation. American Journal of Psychiatry. 2014;171:102–108. doi: 10.1176/appi.ajp.2013.13020224. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Feeley M. Determinants of change in cognitive therapy for depression. Cognitive Therapy and Research. 1990;14(5):469–482. [Google Scholar]
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, ... Gallop R. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62:409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- Driessen E, Cuijpers P, Hollon SD, Dekker JJM. Does pretreatment severity moderate the efficacy of psychological treatments for adult outpatient depression? A meta-analysis. Journal of Consulting and Clinical Psychology. 2010;78:668–680. doi: 10.1037/a0020570. [DOI] [PubMed] [Google Scholar]
- Elkin I, Shea T, Watkins JT, Imber SD, Sotsky SM, Collins JF, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program: General effectiveness of treatments. Archives of General Psychiatry. 1989;46:971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- Emmelkamp PMG, Benner A, Kuipers A, Feiertag GA, Koster HC, van-Appeldoorn FJ. Comparison of brief dynamic and cognitive-behavioral therapies in avoidant personality disorder. British Journal of Psychiatry. 2006;189:60–64. doi: 10.1192/bjp.bp.105.012153. [DOI] [PubMed] [Google Scholar]
- Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(4):578–582. doi: 10.1037//0022-006x.67.4.578. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II) Washington, D.C: American Psychiatric Press; 1997. [Google Scholar]
- Fleiss JL. Balanced incomplete block design for inter-rater reliability studies. Applied Psychological Measurement. 1981;5:105–112. [Google Scholar]
- Forand NR, Gunthert KC, Cohen LH, Butler AC, Beck JS. Preliminary evidence that anxiety is associated with accelerated response in cognitive therapy for depression. Cognitive Therapy and Research. 2011;35:151–160. [Google Scholar]
- Fournier JC, DeRubeis RJ, Beck AT. Dysfunctional cognitions in personality pathology: The structure and validity of the personality belief questionnaire. Psychological Medicine. 2012;42:795–805. doi: 10.1017/S0033291711001711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Shelton RC, Gallop R, Amsterdam JD, Hollon SD. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. The British Journal of Psychiatry. 2008;192:124–129. doi: 10.1192/bjp.bp.107.037234. http://dx.doi.org/10.1192/bjp.bp.107.037234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friborg O, Martinsen EW, Martinussen M, Kaiser S, Overgard KT, Rosenvinge JH. Comorbidity of personality disorders in mood disorders: A meta-analytic review of 122 studies from 1988 to 2010. Journal of Affective Disorders. 2014;152–154:1–11. doi: 10.1016/j.jad.2013.08.023. [DOI] [PubMed] [Google Scholar]
- Gorwood P, Rouillon F, Even C, Falissard B, Corruble E, Moran P. Treatment response in major depression: Effects of personality dysfunction and prior depression. British Journal of Psychiatry. 2010;196:139–142. doi: 10.1192/bjp.bp.109.067058. [DOI] [PubMed] [Google Scholar]
- Grant PM, Huh GA, Perivoliotis D, Stolar NM, Beck AT. Randomized trial to evaluate the efficacy of cognitive therapy for low-functioning patients with schizophrenia. Archives of General Psychiatry. 2012;69(2):121–127. doi: 10.1001/archgenpsychiatry.2011.129. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Stout RL, Markowitz JC, Sanislow CA, Ansell EB, Skodol AE, et al. Personality disorders predict relapse after remission from an episode of major depressive disorder: A 6-year prospective study. Journal of Clinical Psychiatry. 2010;71:1629–1635. doi: 10.4088/JCP.08m04200gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG, Moery LC, Stout RL, Skodol AE, Shea MT, McGlashan TH, et al. Major depressive disorder and borderline personality disorder revisited: Longitudinal interactions. Journal of Clinical Psychiatry. 2004;65:1049–1056. doi: 10.4088/jcp.v65n0804. [DOI] [PubMed] [Google Scholar]
- Høglend P. Exploration of the patient-therapist relationship in psychotherapy. American Journal of Psychiatry. 2014;171:1056–1066. doi: 10.1176/appi.ajp.2014.14010121. [DOI] [PubMed] [Google Scholar]
- Høglend P, Dahl HS, Hersoug AG, Lorentzen S, Perry JC. Long-term effects of transference interpretations in dynamic therapy of personality disorders. European Psychiatry. 2011;26:419–424. doi: 10.1016/j.eurpsy.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Evans MD, Auerbach A, DeRubeis RJ, Elkin I, Lowrey A, et al. Development of a system for rating therapies for depression: Differentiating cognitive therapy, interpersonal psychotherapy, and clinical management pharmacotherapy. Vanderbilt University; 1988. Unpublished manuscript. [Google Scholar]
- Hollon SD, DeRubeis RJ, Shelton RC, Amsterdam JD, Salomon RM, O’Reardon JP, ... Gallop R. Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Archives of General Psychiatry. 2005;62:417–422. doi: 10.1001/archpsyc.62.4.417. [DOI] [PubMed] [Google Scholar]
- Huber PJ, Ronchetti EM. Robust statistics. 2. Hoboken, NJ: Wiley; 2009. [Google Scholar]
- Johansson P, Høglend P, Ulberg R, Amlo S, Marble A, Bøgwald KP, et al. The mediating role of insight for long-term improvements in psychodynamic therapy. Journal of Consulting and Clinical Psychology. 2010;78:438–448. doi: 10.1037/a0019245. [DOI] [PubMed] [Google Scholar]
- Kallestad H, Valen J, McCullough L, Svartberg M, Høglend P, Stiles TC. The relationship between insight gained during therapy and long-term outcome in short-term dynamic psychotherapy and cognitive therapy for cluster C personality disorders. Psychotherapy Research. 2010;20:526–534. doi: 10.1080/10503307.2010.492807. [DOI] [PubMed] [Google Scholar]
- Koller M, Stahel W. Sharpening Wald-type inference in robust regression for small samples. Computational Statistics & Data Analysis. 2011;55:2504–2515. [Google Scholar]
- Leichsenring F, Luyten P, Hilsenroth MJ, Abbass A, Barber JP, Keefe JR, et al. Psychodynamic therapy meets evidence-based medicine: A systematic review using updated criteria. The Lancet Psychiatry. 2015;2:648–660. doi: 10.1016/S2215-0366(15)00155-8. [DOI] [PubMed] [Google Scholar]
- Levy KN, Meehan KB, Yeomans FE. An update and overview of the empirical evidence for transference-focused psychotherapy and other psychotherapies for borderline personality disorder. In: Levy RA, Ablon JS, Kächele H, editors. Psychodynamic psychotherapy research: Evidence-based practice and practice-based evidence. New York, NY: Springer; 2012. pp. 139–167. [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. 1. New York, NY: Guilford Press; 1993. [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clinical Psychology & Psychotherapy. 2010;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Luborsky L. Principles of psychoanalytic psychotherapy: A manual for supportive-expressive treatment. New York, NY: Basic Books; 1984. [Google Scholar]
- MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychological Methods. 2002;7(1):19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
- Maffei C, Fossati A, Agostoni I, Barraco A, Bagnato M, Deborah D, et al. Interrater reliability and internal consistency of the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II), version 2.0. Journal of Personality Disorders. 1997;11:279–284. doi: 10.1521/pedi.1997.11.3.279. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Skodol AE, Petkova E, Cheng J, Sanislow CA, Grilo CM, Gunderson JG, McGlashan TH. Longitudinal effects of personality disorders on psychosocial functioning of patients with major depressive disorder. Journal of Clinical Psychiatry. 2007;68:186–193. doi: 10.4088/jcp.v68n0202. [DOI] [PubMed] [Google Scholar]
- Morey LC, Shea MT, Markowitz JC, Stout RL, Hopwood CJ, Gunderson JG, et al. State effects of major depression on the assessment of personality and personality disorder. American Journal of Psychiatry. 2010;167:528–535. doi: 10.1176/appi.ajp.2009.09071023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muran JC, Safran JD, Gorman BS, Samstag LW, Eubanks-Carter C, Winston A. The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psychotherapies for personality disorders. Psychotherapy: Theory, Research, Practice, Training. 2009;46:233–248. doi: 10.1037/a0016085. [DOI] [PubMed] [Google Scholar]
- Muran JC, Safran JD, Samstag LW, Winston A. Evaluating an alliance-focused treatment for personality disorders. Psychotherapy: Theory, Research, Practice, Training. 2005;42:532–545. [Google Scholar]
- Newton-Howes G, Tyrer P, Johnson T, Mulder R, Kool S, Dekker J, et al. Influence of personality on the outcome of treatment in depression: Systematic review and meta-analysis. Journal of Personality Disorders. 2014;28:577–593. doi: 10.1521/pedi_2013_27_070. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing (Version 3.0.1) Vienna, Austria: R Foundation for Statistical Computing; 2014. [Google Scholar]
- Reimherr FW, Amsterdam JD, Quitkin FM, Rosenbaum JF, Fava M, Zajecka J, et al. Optimal length of continuation therapy in depression: A prospective assessment during long-term fluoxetine treatment. American Journal of Psychiatry. 1998;155:1247–1253. doi: 10.1176/ajp.155.9.1247. [DOI] [PubMed] [Google Scholar]
- Rousseeuw P, Croux C, Todorov V, Ruckstuhl A, Salibian-Barrera M, Verbeke T, et al. robustbase (Version 0.90-2) 2014. [Google Scholar]
- Rush JA, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. American Journal of Psychiatry. 2006;163:1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- Ryum T, Stiles TC, Svartberg M, McCullough L. The effects of therapist competence in assigning homework in cognitive therapy with cluster C personality disorders: Results from a randomized controlled trial. Cognitive and Behavioral Practice. 2010;17:283–289. [Google Scholar]
- Sasso KE, Strunk DR, Braun JD, DeRubeis RJ, Brotman MA. A reexamination of process-outcome relations in cognitive therapy for depression: Disaggregating within-patient and between-patient effects. Psychotherapy Research. doi: 10.1080/10503307.2015.1026423. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seibel CA, Dowd ET. Personality characteristics associated with psychological reactance. Journal of Clinical Psychology. 2001;57:963–969. doi: 10.1002/jclp.1062. [DOI] [PubMed] [Google Scholar]
- Semerari A, Colle L, Pellecchia G, Buccione I, Carcione A, Dimaggio G, et al. Metacognitive dysfunctions in personality disorders: Correlations with disorder severity and personality styles. Journal of Personality Disorders. 2014;28:751–766. doi: 10.1521/pedi_2014_28_137. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;2:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Strauss JL, Hayes AM, Johnson SL, Newman CF, Brown GK, Barber JP, et al. Early alliance, alliance ruptures, and symptom change in a nonrandomized trial of cognitive therapy for avoidant and obsessive-compulsive personality disorders. Journal of Consulting and Clinical Psychology. 2006;74:337–345. doi: 10.1037/0022-006X.74.2.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers RF, Barber JP. Psychodynamic therapy: A guide to evidence-based practice. New York, NY: Guilford; 2010. [Google Scholar]
- Svartberg M, Stiles TC, Seltzer MH. Randomized, controlled trial of the effectiveness of short-term dynamic psychotherapy and cognitive therapy for Cluster C personality disorders. American Journal of Psychiatry. 2004;161:810–817. doi: 10.1176/appi.ajp.161.5.810. [DOI] [PubMed] [Google Scholar]
- Ulvenes PG, Berggraf L, Hoffart A, Stiles TC, Svartberg M, McCullough L, et al. Different processes for different therapies: therapist actions, therapeutic bond, and outcome. Psychotherapy. 2012;49:291–302. doi: 10.1037/a0027895. [DOI] [PubMed] [Google Scholar]
- Wampold BE, Mondin GW, Moody M, Stich F, Benson K, Ahn K. A meta-analysis of outcome studies comparing bona fide psychotherapies: Empirically, “all must have prizes”. Psychological Bulletin. 1997;122(3):203–215. [Google Scholar]
- Webb CA, DeRubeis RJ, Barber JP. Therapist adherence/competence and treatment outcome: A meta-analysis. Journal of Consulting and Clinical Psychology. 2010;78:200–211. doi: 10.1037/a0018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC. Convergence and divergence in the delivery of cognitive therapy in two randomized clinical trials. Behaviour Research and Therapy. 2013;51:493–498. doi: 10.1016/j.brat.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young JE, Beck AT. Revision of the cognitive therapy scale. Philadelphia, PA: Department of Psychology, University of Pennsylvania; 1988. [Google Scholar]
- Young JE, Klosko JS, Weishaar ME. Schema therapy: A practitioner’s guide. New York, NY: Guilford; 2003. [Google Scholar]