BACKGROUND
Dual-energy X-ray absorptiometry (DXA) is a gold standard method for body composition measurement. It is a reliable and valid measure for clinical assessment of percent total body fat (%BF) in adult and pediatric populations.1 Due to the high cost and labor of DXA, alternative methods for accurately measuring body composition are needed. 2 Measures including neck circumference (NC), thigh circumference (TC), body adiposity index (BAI) and bioelectrical impedance analysis (Impedance) have been examined for the assessment of anthropometrics and body composition; however, limited studies have compared these measurements to DXA in overweight and obese pediatric populations.
As a basic anthropometric measure, NC is easy to implement in clinical practice. This measure is easily performed and is typically unaffected by clothing, respiratory movements, or satiety.3, 4 NC in children was found to be positively correlated with waist circumference, body mass index (BMI), height, and weight.3, 5-7 Studies in lean and overweight/obese pediatric populations have concluded that males have a greater NC when compared to females, which is also true of waist circumference and BMI across genders.6, 7 There are no studies to date comparing NC to %BF in children as assessed by DXA. Additional research is needed to assess the feasibility and reliability of NC in pediatric populations as a predictor of obesity and body fat distribution when compared against the gold standard.
TC is a noninvasive and simple measure that has been evaluated in the prediction of body fatness and disease risk.8 Recent studies have suggested that TC reflects body muscle mass, as well as peripheral subcutaneous fat in adult populations.9 A study of Danish men and women found that a low TC was associated with an increased risk of developing heart disease or premature death.10 Researchers in another study looking at White men and women concluded that a larger TC was associated with a lower risk of type 2 diabetes, although they noted that a protective effect was statistically significant only in women.11 While the mechanism is not yet known, one study proposed that this gender difference may be due to regional differences in adipocyte metabolism, which is more pronounced in women than in men.12 A study using magnetic resonance imaging (MRI) to measure body fat in White men and women concluded that when controlling for waist circumference, TC was positively correlated with total and abdominal subcutaneous adipose tissue and skeletal muscle, but negatively associated with visceral adipose tissue.13 The researchers hypothesized that the health protective effect of a larger TC is due to the increased deposition of lower-body and abdominal subcutaneous adipose tissue and skeletal muscle, a decreased accumulation of visceral adipose tissue, or both.13 While researchers have investigated the use of TC as a predictor of body fat distribution and disease risk in the adult population, studies specifically looking at this measurement as a useful alternative to DXA %BF in pediatric populations are warranted.
The BAI equation, which is a ratio of hip circumference to height, was developed in 2001 using a population of adult Mexican Americans ranging in BMI from underweight to morbidly obese.14 The equation was compared against DXA %BF and validated in a population of adult African Americans with BMIs ranging from normal weight to morbidly obese.14 Very few studies have assessed BAI in pediatric populations; however, it has been shown to overestimate male adiposity and underestimate female adiposity in adolescent populations.15 In White children (5-12 years), BAI was not predictive of %BF as measured by Impedance.16 In this younger population of children, a pediatric BAI (BAIp) was developed. However, BAIp was noted to be less useful on an individual scale for predicting %BF than on an epidemiologic scale. Further research is necessary to assess the use of BAIp in pediatric populations.
Impedance analysis is a common method utilized in research and clinical settings to analyze a subject’s body composition. The premise of this measure relies on the implication that fat free mass (FFM), due to its greater electrolyte content, is a better conductor of electrical current than fat mass.17 Impedance is a useful method for assessing body fatness because it is non-invasive and is associated with marginal cost and reasonable accuracy.18, 19 There are multiple equations that have been developed for use with Impedance; however, much of the initial research surrounding the development of these equations focused on lean adults. Deurenberg and colleagues and Schaefer and colleagues developed Impedance equations to estimate fat free mass in pediatric populations.20, 21 Later, Cleary and colleagues validated both equations against DXA in a sample of overweight and obese children aged 5-9. The %BF as determined by the Schaefer equation was the only result that did not significantly differ from DXA in this population.22 Additional research is needed to evaluate the validity of Impedance equations in obese adolescents.
Limited pediatric studies have assessed the validity of NC, TC, BAI, and Impedance compared to DXA. The aim of this study was to investigate more clinically feasible indices to assess body fatness in overweight and obese adolescents at risk for associated comorbidities.
METHODS
Sample population
This cross-sectional study examined baseline data from a randomized clinical trial conducted at the National Institutes of Health (NIH) Clinical Center (clinicaltrials.gov identifier NCT00001723). The original trial was approved by the NIH National Institute of Child Health and Human Development Review Board and informed consent and assent were obtained from all subjects and their parents prior to study initiation. Subjects were male and female adolescents aged 12-17 years and weighing at least 60 kg. BMI-for-age was >95th percentile using National Health and Nutrition Examination Survey I criteria.23 Subjects also had at least one quantifiable, obesity-related comorbidity as determined during the screening admission. Subject race was self-identified as either Non-Hispanic White or African American with all four grandparents also self-identified as all White or all African American. The original sample size for this study was 174 subjects. Five subjects were excluded due to missing data for a final sample size of 169.
Measures of body composition
Height, weight, hip circumference, NC, and TC were collected at the baseline outpatient study visit. Standing height was measured in duplicate to the nearest tenth of a cm using a wall stadiometer with a fixed vertical backboard and an adjustable headpiece. Weight was measured in kg on a digital scale while subjects wore minimal clothing without shoes. All circumference measures were completed in duplicate to the nearest tenth of a cm using a stretch-less tape measure. NC was measured just inferior to the laryngeal prominence at the minimal circumference with the tape measure positioned perpendicular to the long axis of the neck.24 Hip circumference was measured at the maximal protuberance of the buttocks in the horizontal plane with the subject standing erect with feet together and weight distributed evenly across both feet.23 TC was measured at the midpoint of the right thigh (between the inguinal crease and the cephalid border of the patella) with the subject standing with right leg forward and weight placed on left leg.23, 24 All measurements were performed in the fasted state in the morning by one of two registered dietitians certified in body composition measurement in order to reduce measurement variability.
%BF was calculated from height and hip circumference measurements using the BAI equation previously developed in adults14 as well as the equation developed specifically for use in pediatrics (BAIp).16
Impedance measurement was taken post-void with the subject laying supine on a non-conductive surface. The subject’s right shoe and sock and any jewelry on the right wrist or ankle were removed. The subject was positioned with arms away from the body and legs apart. Electrodes were placed on the wrist and finger and the ankle and toe on the right side of the body per instrument manufacturer instructions25 and impedance was measured using a RJL Quantum II (RJL systems, Clinton Township, MI) impedance analyzer. Fat free mass was then calculated using two previously validated equations by Schaefer et al (ImpedanceS) and by Deurenberg et al (ImpedanceD).20, 21
Fat free mass was then converted into %BF for comparison with DXA using the equation %BF = [(weight (kg) − FFM)/weight (kg)] × 100.
On the same day that anthropometric measurements were taken by the dietitian, subjects underwent a DXA scan in hospital radiology. Body composition was measured using a Hologic QDR-4500A (Hologic Inc., Bedford, MA).
Statistical analyses
Descriptive statistics were expressed as percentages for categorical variables and mean and standard deviation for continuous variables (IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY). NC and TC were converted to z-scores using applicable reference standards.26, 27 Pearson correlations were used to compare the various body composition measurements to DXA %BF, and linear regression analyses were done to further compare NC and TC z-scores with DXA %BF. Since z-scores, which take into account age and sex, were used in the regression models, the only other variable that was included with the z-scores was race. Bland-Altman and regression analyses were used to assess agreement for BAI, BAIp, ImpedanceD and Impedances, the measures most highly correlated with DXA (Graphpad Prism, version 6.0, La Jolla, CA).
RESULTS
Mean age of the study participants (n=169) was 14.4 ± 1.4 years and mean BMI was 38.3 ± 5.9 kg/m2 (Table 1). The majority of the subjects were female (68%) and greater than half were African-American (57%).
Table 1. Mean and standard deviation (SD) for age and anthropometric measures of sample population.
| Mean (SD) | |
|---|---|
| Age (y) | 14.4 (1.4) |
| BMI (kg/m2) | 38.3 (5.9) |
| Neck circumference (cm) | 38.8 (3.2) |
| Thigh circumference (cm) | 69.7 (7.5) |
| Body fat from BAI (%) | 39.5 (6.2) |
| Body fat from BAIp (%) | 43.3 (7.5) |
| Body fat from ImpedanceD (%) | 62.5 (4.5) |
| Body fat from ImpedanceS (%) | 56.9 (5.2) |
| Body fat from DXA (%) | 46.8 (4.7) |
While we observed no association between NC z-score and DXA %BF in the sample, TC z-score was significantly associated with DXA %BF (Table 2). Multiple regression analyses controlled for race revealed TC z-score, but not NC z-score, as a significant predictor predictive of DXA %BF (Table 3).
Table 2. Associations between body composition measures and DXA %BF (*p<0.001).
| All Subjects (n=169) | African American (n=97) | White (n=72) | Female (n=115) | Male (n=54) | |
|---|---|---|---|---|---|
| NC z-score | −0.049 | −0.162 | 0.079 | −0.038 | −0.065 |
| TC z-score | −0.413* | −0.418* | −0.495* | −0.513* | −0.264 |
| BAI | 0.578* | 0.519* | 0.712* | 0.625* | 0.504* |
| BAIp | 0.580* | 0.539* | 0.684* | 0.644* | 0.458* |
| ImpedanceD | 0.655* | 0.685* | 0.648* | 0.671* | 0.630* |
| ImpedanceS | 0.634* | 0.678* | 0.614* | 0.635* | 0.658* |
Table 3. Regression models examining the relationships between neck and thigh circumference z-scores and DXA %BF.
| R2 | β | p-value | |
|---|---|---|---|
| Model 1 | |||
| NC z-score | 0.002 | −0.160 | 0.518 |
| Race | 0.003 | 0.168 | 0.822 |
| Model 2 | |||
| TC z-score | 0.170 | −1.942 | 0.000 |
| Race | 0.203 | 1.854 | 0.010 |
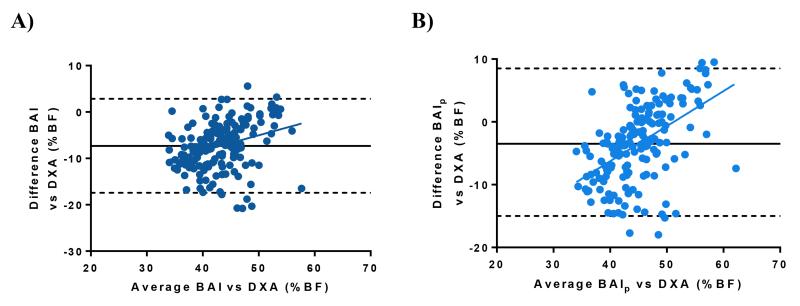
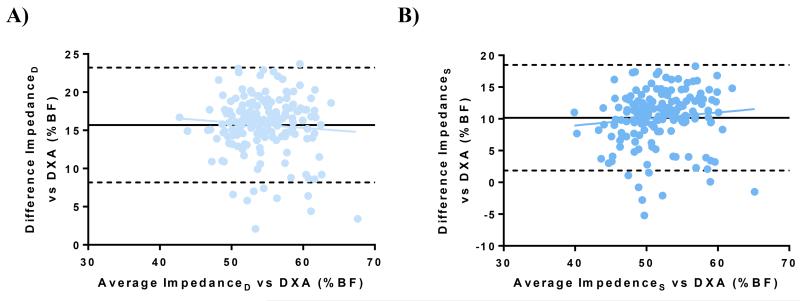
BAI and BAIp were positively correlated with DXA %BF across all subjects (r=0.578 and r=0.580 respectively, p<0.001) (Table 2). %BF calculated from ImpedanceD and ImpedanceS equations was also positively correlated with DXA %BF for all subjects (r=0.655, p<0.001 and r=0.634, p<0.0001 respectively) (Table 2). Bland-Altman analyses of %BF derived from BAI, BAIp, ImpedanceD and ImpedanceS compared to DXA %BF are shown in Figures 1 and 2. BAI underestimated %BF by −7.3% ± 5.2% as compared to DXA, however, a significant magnitude bias was present (r2=0.097, p<0.001) (Figure 1A). BAIp underestimated %BF by −3.5 ± 6.1% with significant magnitude bias (r2=0.250, p<0.001) (Figure 1B). ImpedanceD and ImpedanceS both overestimated %BF (15.7 ± 3.8% and 10.2 ± 4.2%, respectively), however, no magnitude bias was detected for Impedance measurements (r2=0.006, p=0.319 and r2=0.012, p=0.163 respectively) (Figures 2A and 2B).
Figure 1. Bland-Altman graphs of BAI (A) and BAIp (B) vs. DXA.
Figure 2. Bland-Altman graphs of ImpedanceD (A) and ImpedanceS (B) vs. DXA.
DISCUSSION
The purpose of this study was to identify a simpler, less expensive measure than DXA for assessing body fatness in overweight and obese adolescents. An alternative measure to DXA is needed in this population because measurement with DXA is expensive, immovable, and delivers a small dose of radiation. The alternative measurements examined in this study were less labor-intensive and more cost-effective, as equipment such as stadiometers, scales, tape measures and impedance analyzers were used.
As a non-invasive anthropometric measure, NC has been identified as a possible alternative to DXA as it has been shown to be well correlated with BMI and chronic disease in pediatrics.3, 5-7. However, the present study found no correlation between NC z-score and DXA %BF. This may be due to the exclusion of individuals with an underweight or normal BMI. In our obese pediatric population, the range of NC measures may not vary enough across subjects to show an association with DXA %BF. Also, the mean NC in the given population (38.8 cm) was greater than suggested cut-off values for elevated BMI identified in previous studies (27.4-31.3 cm in boys; 26.3-31.4 cm in girls).6 It is possible that an equation using height and/or weight with NC would result in an association with DXA %BF, therefore, further investigation is warranted to develop such an equation. At this time, NC cannot be recommended as an alternative measure to DXA in obese adolescents.
Previous studies have investigated the use of TC as a practical measure to predict body fat distribution and disease risk in adults. This study was the first to examine TC z-score as a possible alternative to DXA in the prediction of %BF in pediatrics as previous research on this association has only been done in adults.12, 28 In our study, TC z-score was negatively associated with DXA %BF only in females and was predictive of %BF in regression equations when race was taken into account. Since TC needs to be adjusted for age, sex and race when using it in research, this may not be as simple to use to estimate %BF as other measures being examined. Therefore, in contrast to others who have examined this measure in association with disease risk or in adult populations, we do not feel that this measurement should be recommended to use in place of DXA for prediction of %BF in obese adolescents without further exploration.
In this study, both BAI and BAIp were significantly correlated with DXA %BF. The BAI correlation is in line with results by Dias et al. in which BAI was significantly correlated with DXA %BF in Brazilian males and females aged 13-16 with BMIs classified as normal, overweight or obese28; however, our study looked at White and African American adolescents of a broader age range (12-17). Additionally, Dias et al. only looked at the BAI measure; the present study is the first study to date comparing pediatric measures of %BF from BAIp with %BF from DXA. In the current study, BAIp had better agreement with DXA %BF than did BAI; the difference between DXA and BAIp was −3.5 ± 6.1%. However, BAI and BAIp both showed significant magnitude bias, indicating that both measures become increasingly less accurate compared to DXA as body fat increases. This agrees with results by Wickel, who found that agreement between %BF from skinfolds and from BAI showed magnitude bias for both genders of adolescents.15 The bias observed in our study suggests that neither BAI nor BAIp is an accurate predictor of %BF for all ranges of %BF in this pediatric population. Therefore, BAI and BAIp are not recommended as simpler alternatives to DXA for measuring pediatric body adiposity.
ImpedanceS and ImpedanceD were both positively correlated with DXA %BF for all subjects in this study. Both impedance measures systematically over-estimated %BF compared to DXA (15.7 ± 3.8% for ImpedenaceD and 10.2 ± 4.2% for ImpedanceS). However, given the limited magnitude bias and easily correctible systematic over-estimation, our data suggests that ImpedanceS may be an easier and less expensive alternative to DXA in assessing body fatness in obese adolescents. Our results are consistent with those of Cleary et al. who also demonstrated significant correlations between ImpedanceD and ImpedanceS when compared to DXA %BF in overweight and obese children aged 5-9 years.22 While both equations over-estimated %BF compared to DXA, Cleary concluded that ImpedanceS provided the most accurate estimate of %BF due to limited bias. Future studies should evaluate this systematic overestimation to develop more accurate Impedance equations for obese pediatric participants.
A major strength of this study was the use of DXA, considered by many to be the gold standard measurement of body composition, as a comparison tool to identify a simpler, less costly measure of body fatness in an obese pediatric population. To date, there are a limited number of validation studies using DXA as a reference measure for body fatness in children; more common validation measures include skinfolds, waist circumference, and various methods of bioelectrical impedance analysis.15, 16, 28 Lastly, in order to reduce variability, all of the measurements were performed by two dietitians certified biannually to perform these measurements.
Limitations of this study include over-representation of females and inclusion of only White and African American races in the study population. However, findings suggest ImpedanceS could be a useful measurement, which should be examined further in larger samples including subjects of varying ethnicities. Additionally, this study sample only included obese adolescents. As such, generalizations to pediatric populations with a wider range in weight status are difficult. Finally, this study does not evaluate data trends over time when comparing different measurements. Therefore, it is not possible to make a conclusive validation of ImpedanceS as an alternative to DXA.
Given the pediatric obesity epidemic and its associated morbidities, more research is needed to develop an inexpensive, efficient, and accurate measure of body composition for clinical and research use. Of the measures reported in this study, ImpedanceS may be the simplest and most accurate predictor of %BF in obese adolescents when compared to DXA %BF. However, further validation studies are warranted to explore ImpedanceS as an alternative to DXA in pediatric populations.
Acknowledgements
This research was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development ZIAHD-00641 (to J. Yanovski) with supplemental funding from the National Institute on Minority Health and Health Disparities and the Division of Nutrition Research Coordination, NIH.
Abbreviations
- DXA
Dual Energy X-Ray Absorptiometry
- %BF
percent body fat
- NC
neck circumference
- TC
thigh circumference
- BAI
body adiposity index
- BAIp
pediatric body adiposity index
- FFM
fat-free mass
Footnotes
Disclaimer: Dr. Yanovski is a Commissioned Officer in the U.S. Public Health Service. The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the U.S. Public Health Service.
REFERENCES
- 1.Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am. J. Clin. Nutr. 2002;75:978–985. doi: 10.1093/ajcn/75.6.978. [DOI] [PubMed] [Google Scholar]
- 2.Van Der Ploeg GE, Withers RT, Laforgia J. Percent body fat via DEXA: comparison with a four-compartment model. J Appl Physiol (1985) 2003;94:499–506. doi: 10.1152/japplphysiol.00436.2002. [DOI] [PubMed] [Google Scholar]
- 3.Hatipoglu N, Mazicioglu MM, Kurtoglu S, Kendirci M. Neck circumference: an additional tool of screening overweight and obesity in childhood. Eur. J. Pediatr. 2010;169:733–739. doi: 10.1007/s00431-009-1104-z. [DOI] [PubMed] [Google Scholar]
- 4.Kurtoglu S, Hatipoglu N, Mazicioglu MM, Kondolot M. Neck circumference as a novel parameter to determine metabolic risk factors in obese children. Eur. J. Clin. Invest. 2012;42:623–630. doi: 10.1111/j.1365-2362.2011.02627.x. [DOI] [PubMed] [Google Scholar]
- 5.Guo X, Li Y, Sun G, et al. Prehypertension in children and adolescents: association with body weight and neck circumference. Intern. Med. 2012;51:23–27. doi: 10.2169/internalmedicine.51.6347. [DOI] [PubMed] [Google Scholar]
- 6.Lou DH, Yin FZ, Wang R, Ma CM, Liu XL, Lu Q. Neck circumference is an accurate and simple index for evaluating overweight and obesity in Han children. Ann. Hum. Biol. 2012;39:161–165. doi: 10.3109/03014460.2012.660990. [DOI] [PubMed] [Google Scholar]
- 7.Nafiu OO, Burke C, Lee J, Voepel-Lewis T, Malviya S, Tremper KK. Neck circumference as a screening measure for identifying children with high body mass index. Pediatrics. 2010;126:e306–310. doi: 10.1542/peds.2010-0242. [DOI] [PubMed] [Google Scholar]
- 8.Jung KJ, Kimm H, Yun JE, Jee SH. Thigh circumference and diabetes: obesity as a potential effect modifier. J. Epidemiol. 2013;23:329–336. doi: 10.2188/jea.JE20120174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park JS, Cho MH, Ahn CW, Kim KR, Huh KB. The association of insulin resistance and carotid atherosclerosis with thigh and calf circumference in patients with type 2 diabetes. Cardiovasc Diabetol. 2012;11:62. doi: 10.1186/1475-2840-11-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heitmann BL, Frederiksen P. Thigh circumference and risk of heart disease and premature death: prospective cohort study. BMJ. 2009;339:b3292. doi: 10.1136/bmj.b3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Snijder MB, Dekker JM, Visser M, et al. Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn Study. Am. J. Clin. Nutr. 2003;77:1192–1197. doi: 10.1093/ajcn/77.5.1192. [DOI] [PubMed] [Google Scholar]
- 12.Rebuffe-Scrive M, Enk L, Crona N, et al. Fat cell metabolism in different regions in women. Effect of menstrual cycle, pregnancy, and lactation. J. Clin. Invest. 1985;75:1973–1976. doi: 10.1172/JCI111914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuk JL, Janiszewski PM, Ross R. Body mass index and hip and thigh circumferences are negatively associated with visceral adipose tissue after control for waist circumference. Am. J. Clin. Nutr. 2007;85:1540–1544. doi: 10.1093/ajcn/85.6.1540. [DOI] [PubMed] [Google Scholar]
- 14.Bergman RN, Stefanovski D, Buchanan TA, et al. A better index of body adiposity. Obesity (Silver Spring) 2011;19:1083–1089. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wickel EE. Evaluating the utility of the body adiposity index in adolescent boys and girls. J. Sci. Med. Sport. 2014;17:434–438. doi: 10.1016/j.jsams.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Aarbaoui TE, Samouda H, Zitouni D, et al. Does the body adiposity index (BAI) apply to paediatric populations? Ann Hum Biol. 2013;40(45):451–458. doi: 10.3109/03014460.2013.802011. [DOI] [PubMed] [Google Scholar]
- 17.Okasora K, Takaya R, Tokuda M, et al. Comparison of bioelectrical impedance analysis and dual energy X-ray absorptiometry for assessment of body composition in children. Pediatr. Int. 1999;41:121–125. doi: 10.1046/j.1442-200x.1999.4121048.x. [DOI] [PubMed] [Google Scholar]
- 18.Eisenmann JC, Heelan KA, Welk GJ. Assessing body composition among 3- to 8-year-old children: anthropometry, BIA, and DXA. Obes. Res. 2004;12:1633–1640. doi: 10.1038/oby.2004.203. [DOI] [PubMed] [Google Scholar]
- 19.Lazzer S, Bedogni G, Agosti F, De Col A, Mornati D, Sartorio A. Comparison of dual-energy X-ray absorptiometry, air displacement plethysmography and bioelectrical impedance analysis for the assessment of body composition in severely obese Caucasian children and adolescents. Br. J. Nutr. 2008;100:918–924. doi: 10.1017/S0007114508922558. [DOI] [PubMed] [Google Scholar]
- 20.Deurenberg P, Kusters CS, Smit HE. Assessment of body composition by bioelectrical impedance in children and young adults is strongly age-dependent. Eur. J. Clin. Nutr. 1990;44:261–268. [PubMed] [Google Scholar]
- 21.Schaefer F, Georgi M, Zieger A, Scharer K. Usefulness of bioelectric impedance and skinfold measurements in predicting fat-free mass derived from total body potassium in children. Pediatr. Res. 1994;35:617–624. [PubMed] [Google Scholar]
- 22.Cleary J, Daniells S, Okely AD, Batterham M, Nicholls J. Predictive validity of four bioelectrical impedance equations in determining percent fat mass in overweight and obese children. J. Am. Diet. Assoc. 2008;108:136–139. doi: 10.1016/j.jada.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Centers For Disease Control. National Health and Nutrition Examination Survey (NHANES) Anthropometry Procedures Manual. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf2007.
- 24.Lohman TGRAFMR . Anthropometric standardization reference manual. Human Kinetics Books; Champaign, IL: 1988. [Google Scholar]
- 25.RJL Systems How Electrodes are Placed on the Hand and Foot. 2014 http://www.rjlsystems.com/documentation/how-electrodes-are-placed-on-the-hand-and-foot/ [Google Scholar]
- 26.Katz SL, Vaccani JP, Clarke J, Hoey L, Colley RC, Barrowman NJ. Creation of a reference dataset of neck sizes in children: standardizing a potential new tool for prediction of obesity-associated diseases? BMC Pediatr. 2014;14:159. doi: 10.1186/1471-2431-14-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frisancho AR. Anthropometric Standards: An Interactive Nutritional Reference of Body Size and Body Composition for Children and Adults. The University of Michigan Press; United States of America: 2008. [Google Scholar]
- 28.Dias IB, Panazzolo DG, Marques MF, et al. Relationships between emerging cardiovascular risk factors, z-BMI, waist circumference and body adiposity index (BAI) on adolescents. Clin. Endocrinol. (Oxf.) 2013;79:667–674. doi: 10.1111/cen.12195. [DOI] [PubMed] [Google Scholar]