Abstract
Purpose: To investigate the effects of non-drug interventions on the sleep quality of patients after mechanical cardiac valve implantation.
Methods: In this prospective, randomized, controlled trial, 64 patients scheduled for mechanical mitral valve replacement were recruited. Patients underwent cognitive behavioral therapy and wore noise cancelling earplugs and eye mask. Sleep quality was evaluated on the 4th after admission and the 5th days after operation. The primary outcome was the total sleep quality score differences between the 4th day after admission and the 5th day after operation.
Results: All patients had been suffering from poor sleep quality for a month before admission. There was no difference between both groups on the 4th day after admission. Overall sleep quality in the intervention group was better than in the control group on the 5th day after operation. The subjective sleep quality of the patients in each group was significantly lower on the 5th day after the operation than on the 4th day after admission (P <0.05).
Conclusion: Non-drug intervention could improve the sleep quality of patients after mechanical cardiac valve implantation and help the postoperative recovery of the patients. (Trial registration: ChiCTR-TRC-14004405, 21 March 2014.)
Keywords: non-drug intervention, mechanical valve, valve noise, sleep quality
Introduction
Cardiovascular diseases have become a dangerous threat to people’s life and the incidence rate is increasing all over the world. According to the statistics of the World Heart Association, the situation of prevention and management of cardiovascular diseases is very grim.1) Valve replacement is an effective method to treat heart valve disease.
Previous studies have shown that patients generally suffer from severe sleep disturbance after cardiac surgery.2) Sleep disturbance can impair the immunity of the body, prolong the mechanical ventilation duration, reduce cognitive functions, increase the risk of infections, and even aggravate the disease and increase the mortality.3,4) Previous studies reported that at least one third of the patients who undergo mechanical valve replacement are with severe stress from the continuous noise of the mechanical valve, which could further induce chronic stress and thus affect sleep quality.5) Some patients even have to undergo a second operation because the noise from the mechanical valve severely disturbs their sleep.6)
Clinically used sleep interventions include drug interventions and non-drug interventions. Many studies showed that hypnotics and sedatives could improve the sleep duration, but they can also change the sleep pattern, reduce the time of deep sleep and rapid-eye-movement sleep, and induce side effects.7,8) Postoperative thirst has been reported as a major reason that influences the sleep of the patients.9) Other studies also suggest that noise is the major cause that affects the sleep of the patients after operation.10) However, no study has been performed to investigate the effects of the noise from the mechanical valve on the sleep of the patients after valvular surgeries.
In this study, we investigated the factors that affect postoperative sleep quality after mechanical valve replacement, and we tried to improve the quality of sleep with a series of non-drug interventions including correcting the cognitive errors with cognitive behavioral therapy (CBT) and wearing noise canceling earplugs and eye masks.
Materials and Methods
Subjects
In this prospective, randomized controlled trial, sixty-four patients scheduled for mechanical mitral valve replacement at Fujian Medical University Union Hospital between March 2014 and August 2014 were recruited. The inclusion criteria were: (1) aged 18–65 years; (2) the patient or the family voluntarily accepted participation; (3) first-attempt mitral valve replacement; (4) the time between admission and scheduled operation was at least 5 days; (5) conscious; and (6) no hearing disorders. Exclusion criteria were: (1) confirmed obstructive sleep apnea syndrome (OSAS); (2) severe complications of the brain, liver, renal, or other major organs; or (3) recently taking somnifacient regularly. The present study was approved by the ethical committee of Fujian Medical University Union Hospital. Informed consent was obtained from each patient.
Study design and intervention
Participation in the study was terminated if a complication occurred, if disease aggravated, if the patient became unable to participate, or died. Data of these patients were not included in the final analysis. The 64 patients were randomized to the intervention and control groups (n = 32/group) at the first visit at the outpatient department using sequential sealed envelopes prepared using a random number table.
The patients were hospitalized in two different zones of the Cardiac Surgery Department to minimize information exchange. The ward facilities, bed number, and natural environment of these two zones were comparable. All patients received conventional treatments and healthcare (conventional group). The patients in the intervention group received additional non-drug interventions including acousto-optic protective measures and CBT (non-drug intervention group). The interventions continued until the patient was discharged. In the conventional group, routine psychiatric care and environmental control were given. Drugs in the two groups complied with the applicable Chinese guidelines and little differences were observed. When patients suffered from intolerable pain, morphine hydrochloride was injected as per doctor’s prescriptions.
The Pittsburgh Sleep Quality Index (PSQI)11) was used to evaluate the sleep status of the patients for the past month on admission, and a subjective sleep quality assessment scale was used for the patients on the 4th day after admission (before the operation). The disease of the patients was generally stabilized on the 5th day after admission, and then subjective sleep quality assessment scale and sleep influencing factor questionnaire were used to collect the data.
Cognitive behavioral therapy
CBT has been approved by the National Institute of Mental Health (NIMH). CBT was considered the preferred choice for treating insomnia if it overcomes the limitations of insomnia treatment with drugs. The aims of CBT are to change the non-adaptive sleep habits, reduce autonomous or cognitive arousal, and conduct healthy sleep education.12) During this study, the investigators distributed educational materials to each patient, which included the general information about the disease, volume of noise from the mechanical valve, mechanisms involved in the noise generation, and the significance of the noise. In addition, the patients were also informed that the noise of the mechanical valve was generated when the heart was beating normally, which meant that the heart has restored normal functions after surgery. In this present study, we tried to identify the irrational beliefs that caused the insomnia through rational analysis and logic discrimination, and help them to replace the irrational beliefs with rational beliefs. Therefore, this study was designed to change the wrong beliefs and attitude of the patients that the noise from the mechanical valve will cause poor sleep, and help them tackle the emotional and behavioral issues against the noise.
Acousto-optic protective measures
Noise canceling earplugs and eye masks were distributed to each patient in the intervention group on the 4th day after admission (at which time no intervention had been performed for the patients). The patients were taught how to use the materials properly and were informed that these materials will help them to improve their sleep quality. The patients were asked to wear the earplugs and eye masks at 21:00–21:30 h every night, and not to remove them until the next morning. This was to allow the patients to get used to wearing these materials and start to establish time signals.
Evaluation tools and outcomes
The three sleep quality scales were all applied by a practitioner nurse. The team included three members. The team leader conducted a uniform training to the team members. Uniform normative terminologies and instructions were used in the scales. General characteristics of the patients were collected by questionnaires designed by the investigators. Demographic characteristics and clinical data of the patients including sex, age, education, smoking history, underlying disease, complications, cardiac function classification, surgical method, cardiopulmonary bypass time, mechanical ventilation time, intensive care unit (ICU) stay, and acute physiology and chronic health evaluation (APACHE II) score were collected.
A PSQI score11,13) of 7 was used as the cut-off value: PSQI ≤7 indicated good sleep quality, while PSQI >7 indicated poor sleep quality.14)
Subjective sleep quality assessment
The Verran and Snyder-Halpern (VSH)15) sleep scale was used for the subjective sleep quality assessment,16) and the results were compared between the two groups as well as before and after the interventions within the same group. The VSH contains eight items, namely mid-sleep awakenings, awaken time, sleep duration, satisfaction with sleep, sleep latency, satisfaction with sleep latency, sleep depth, and energy recovery after sleep. Visual scoring was used; in brief, a 10-cm line was divided evenly in 10 and was marked 0–10 (from left to right); 0 indicates no awakening, deep sleep, and rapid energy recovery after awaking, while 10 indicates frequent awakening during the whole night, awake almost all the night, no sleep time, and not satisfied with the sleep, hard to fall asleep, not satisfied with sleep latency, light sleep, and hard to recover energy after awaking. The scores were added up to obtain the overall VSH score, with the highest scores indicating poorer sleep quality.
A sound level meter (TM83, Teichman) was used to measure the valvular noise by qualified clinicians.
The primary outcome was total sleep quality score differences between the 4th day after admission and the 5th day after operation. Secondary outcomes were the scores of every item of sleep quality score differences.
Data collection
On the day of admission, the PSQI scale was used to for all patients. The VSH was used to evaluate the subjective sleep quality on the 4th day after admission, at which time no operation had been performed. The subjective sleep quality was evaluated again on the 5th day after operation, at which time the patients were stabilized. The investigators explained the objectives of the scale, how to answer the questions, and the unified instructions. Then the patients were asked to complete the questionnaires alone. The investigators were also responsible to identify any missing items as soon as possible, and ask the patients to complete the items immediately, to ensure the completeness and accuracy of the questionnaires, but without forcing the patients.
Statistical analysis
SPSS 17.0 (IBM, Armonk, NY, USA) was used for statistical analysis. The chi-square test was used to compare the categorical variables between the two groups. For the comparisons of continuous data, the independent sample t test was used if the data in the two groups were normally distributed and with equal variance. Two-sided P-values <0.05 were considered statistically significant.
Results
Patient’s characteristics
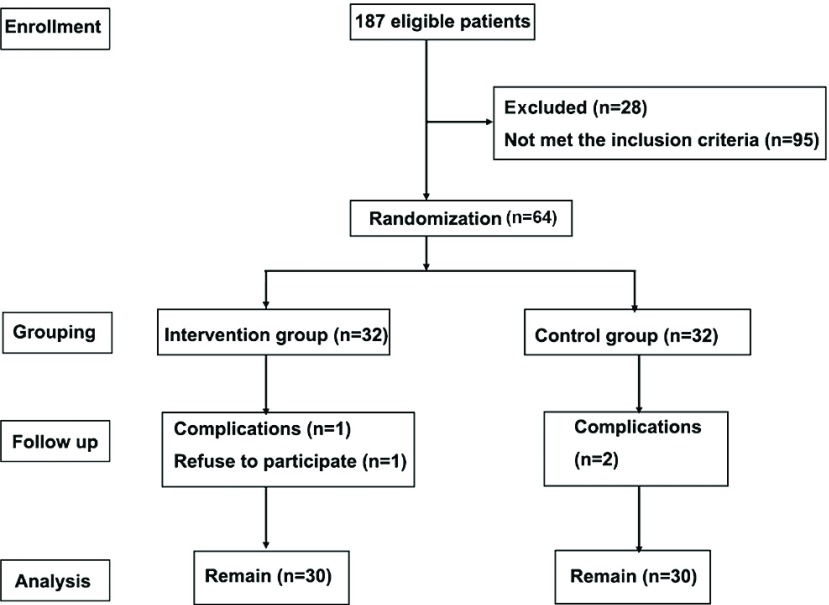
Two patients in the conventional group and one patient in the treatment group were withdrawn from the study. One patient in the intervention group refused to participate (total of 60 patients evenly divided in both groups) (Fig. 1).
Fig. 1.
Flowchart of the patients.
In the intervention group, there were 17 males and 15 females, and the mean age was 49.1 ± 11.4 years. In the conventional group, there were 14 males and 18 females, and the mean age was 48.6 ± 11.3 years. There were no significant differences between the two groups (P >0.05) (Table 1).
Table 1.
Comparison of the characteristics of the patients between the two groups
| Parameters | Variables | Control group | Intervention group | P-value |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Sex | Male | 14 (43.8) | 17 (53.1) | 0.453 |
| Female | 18 (56.2) | 15 (46.9) | ||
| Age (years) | 18–44 | 10 (31.2) | 10 (31.2) | 0.953 |
| 45–59 | 14 (43.8) | 13 (40.6) | ||
| 60–65 | 8 (25) | 9 (28.2) | ||
| Education | Primary school or lower | 9 (28.2) | 10 (31.2) | 0.736 |
| Middle school | 16 (50) | 13 (40.6) | ||
| College or higher | 7 (21.8) | 9 (28.2) | ||
| Smoking history | Yes | 11 (34.4) | 13 (40.6) | 0.606 |
| No | 21 (65.6) | 19 (59.4) | ||
| Underlying disease | Mitral stenosis | 21 (65.6) | 18 (56.2) | 0.442 |
| Mitral incompetence | 11 (34.4) | 14 (43.8) | ||
| Complication | Tricuspid incompetence | 6 (18.8) | 5 (15.6) | 0.966 |
| Atrial fibrillation | 10 (31.2) | 11 (34.4) | ||
| Hypertension | 9 (28.2) | 10 (31.2) | ||
| Diabetes | 7 (21.8) | 6 (18.8) | ||
| Cardiac function | Grade I | 6 (18.8) | 4 (12.5) | 0.665 |
| classification | Grade II | 19 (59.4) | 21 (65.6) | |
| Grade III | 7 (21.8) | 6 (18.8) | ||
| Grade IV | 0 (0) | 1 (3.1) | ||
| Cardiopulmonary | <30 | 7 (21.8) | 6 (18.8) | 0.875 |
| bypass time (min) | 30–90 | 19 (59.4) | 21 (65.6) | |
| >90 | 6 (18.8) | 5 (15.6) | ||
| ICU stay (h) | <24 | 15 (46.9) | 13 (40.6) | 0.725 |
| 24–48 | 14 (43.8) | 14 (43.8) | ||
| >48 | 3 (9.3) | 5 (15.6) | ||
| Mechanical ventilation | <12 | 6 (18.8) | 6 (18.8) | 0.895 |
| duration (h) | 12–24 | 24 (75) | 23 (71.9) | |
| >24 | 2 (6.2) | 3 (9.3) | ||
| APACHE II | ≤14 | 13 (40.6) | 11 (34.4) | 0.606 |
| >14 | 19 (59.4) | 21 (65.6) | ||
The valvular noises in the two groups are presented in Table 2. There was no significant difference between the two groups (P >0.05).
Table 2.
Noise from the mechanical mitral valve in the two groups (mean ± SD)
| Control group | Intervention group | P-value | ||
|---|---|---|---|---|
| N | 32 | 32 | ||
| GK valve | n | 13 | 14 | |
| Noise (dB) | 68.3 ± 8.9 | 69.7 ± 7.0 | 0.6627 | |
| SJM valve | n | 19 | 18 | |
| Noise (dB) | 69.9 ± 5.1 | 68.2 ± 6.3 | 0.6649 | |
GK valve: bileaflet mechanical cardiac valve; SJM valve: St. Jude mechanical cardiac valve; SD: standard deviation
Comparison of the sleep quality of the patients on admission
The scores of every item in the PSQI were not significantly different between the two groups (P >0.05). In addition, all the patients were with a PSQI score >7, suggesting that the patients in each group had a poor sleep quality in the month before admission (Table 3).
Table 3.
Comparison of the PSQI scores on admission between the two groups (mean ± SD)
| Control group | Intervention group | P-value | |
|---|---|---|---|
| n | 30 | 30 | |
| Sleep quality | 1.79 ± 0.28 | 1.80 ± 0.13 | 0.8745 |
| Sleep latency | 1.65 ± 0.82 | 1.69 ± 0.67 | 0.4881 |
| Sleep duration | 1.92 ± 0.62 | 1.89 ± 0.76 | 0.3369 |
| Sleep efficiency | 1.78 ± 0.54 | 1.89 ± 0.23 | 0.131 |
| Sleep disturbances | 2.86 ± 0.47 | 2.78 ± 0.96 | 0.7984 |
| Daytime dysfunction | 1.75 ± 0.87 | 1.82 ± 0.19 | 0.1593 |
| Mean score | 7.68 ± 0.53 | 7.72 ± 0.28 | 0.716 |
PSQI: Pittsburgh Sleep Quality Index; SD: standard deviation
Comparison of the sleep quality on the 4th day after admission and 5th day after operation
There were no significant differences between the two groups for each of the eight items (namely mid-sleep awakenings, awaken time, sleep duration, satisfaction with sleep, sleep latency, satisfaction with sleep latency, sleep depth, and energy recovery) or in the total score (P >0.05). In contrast, the scores were significantly lower in the intervention group compared to the conventional group on the 5th day after operation (P <0.01). In addition, the scores of each item, as well as the total score, in each group were significantly lower in the intervention group compared to the conventional group on the 5th day after operation than on the 4th day after admission (P <0.05), but the decrease of the sleep quality in the intervention group was not as pronounced as in the conventional group (Table 4).
Table 4.
Comparison of the subjective sleep quality on the 4th day after admission and 5th day after operation between the two groups (mean ± SD)
| Items | 4th day after admission | 5th day after operation | ||
|---|---|---|---|---|
| Control group (n = 30) | Intervention group (n = 30) | Control group (n = 30) | Intervention group (n = 30) | |
| Mid-sleep awakenings | 3.90 ± 1.51 | 3.66 ± 1.18 | 6.07 ± 1.11## | 5.23 ± 1.01$$ |
| Awaken time | 3.40 ± 1.35 | 4.00 ± 1.20 | 6.43 ± 1.07## | 5.10 ± 1.16$$ |
| Sleep duration | 4.20 ± 1.39 | 4.80 ± 1.24 | 6.40 ± 1.07## | 5.70 ± 1.02$$ |
| Satisfaction with sleep | 3.83 ± 1.51 | 4.13 ± 1.38 | 6.10 ± 1.18## | 5.10 ± 1.16$$ |
| Sleep latency | 3.57 ± 1.07 | 3.73 ± 1.04 | 5.50 ± 1.01## | 4.83 ± 0.99$$ |
| Satisfaction with sleep latency | 3.10 ± 1.32 | 3.10 ± 1.03 | 5.60 ± 1.13## | 4.33 ± 0.92$$ |
| Sleep depth | 3.03 ± 1.26 | 3.47 ± 1.22 | 6.10 ± 0.76## | 5.23 ± 0.77$$ |
| Energy recovery after sleep | 3.07 ± 1.28 | 2.90 ± 1.10 | 6.10 ± 1.21## | 4.90 ± 0.76$$ |
| Total score | 27.27 ± 7.80 | 29.77 ± 5.28 | 45.33 ± 6.27## | 39.27 ± 4.19$$ |
##P <0.01; $$P <0.01; comparison of the scores between the 4th day after admission and the 5th day after operation within the intervention group. SD: standard deviation
Comparison of the subjective sleep quality scores between the 4th day after admission and the 5th day after operation
The score differences of each item and the total scores between the 4th day after admission and the 5th day after operation were calculated and compared between the two groups, and the results showed significant differences in seven items (except for mid-sleep awakenings) and the total score (P <0.05). The results showed that the increase of the scores in the intervention group was not as pronounced as in the conventional group, which means that the extent of the sleep quality decrease was smaller in the intervention group than in the control group, but no significant differences were found in the score differences of mid-sleep awakenings between the two groups (P >0.05). (Supplemental Table 1).
Discussion
Sleep disturbance can influence the immune, cardiovascular, and endocrine systems of the patients. It can also impair their cognitive functions and even induce delirium, which will in turn delay their recovery.2,16) Therefore, controlling these factors is important for improving the sleep quality and recovery of patients after valvular surgery. In this study, the PSQI scores of the patients in each group were higher than 7 before the operation, suggesting that all the patients scheduled for valve replacement were with poor sleep quality in the month before surgery. The major presentations of poor sleep quality included hard to fall asleep, easy to wake up during the night, dreaminess, and fatigue, which are supported by the findings of Redeker et al.2) The findings of this present study also showed that the subjective sleep quality of the patients was even poorer by the 5th day after valve surgery than on the 4th day after admission, which is also supported by previous findings.17)
In this study, 26 factors that could potentially influence the sleep quality of the patients were investigated on the 5th day after surgery. Valvular noise, worrying about the outcomes, and uncomfortable position were the three leading causes that influenced sleep quality. The noise from the mechanical valve was the first leading cause influencing the sleep quality after the operation. Several previous studies reported that noise was the major factor that influenced the sleep of the patients in the ICU;18) however, the noise they investigated was mainly environmental noise, while the effects of the noise from the cardiac valve itself was not reported. This present study focused on the effects of mechanical valves on the sleep quality of the patients after cardiac valve replacement, which was not investigated in previous studies. Noise in the 2–5 kHz frequencies is easily perceptible to humans.19) The noise from the valve can be heard by the patients and when heard for the first time, the patients are generally not aware whether the noise is associated with the disease, the valve, or the outcomes. Therefore, stress reactions are generally found in these patients. In this study, we found that the effects of the valvular noise on the sleep of the patients were more important than the worries about the outcomes and the pains. The wrong understandings of the working principle of the valves can be corrected by simple education.
Sleep interventions include drug and non-drug interventions. In this study, non-drug interventions including acousto-optic protective measures and CBT were performed, and the results showed that although the patients were with the same valve noise, the subjective sleep quality was significantly better in the intervention group than in the conventional group. In addition, the effects of the non-drug interventions on the sleep quality of the patients in the intervention group were more pronounced than in the conventional group. These findings suggest that performing non-drug interventions improved the sleep of the patients to a certain extent.
Several studies reported that noise cancelling earplugs and eye masks could improve the sleep quality of the patients in the ICU, but some patients cannot adapt to the use of earplugs or eye masks.20) In this present study, noise cancelling earplugs and eye masks were provided in addition to CBT. One patient in the intervention group withdrew from the study because he could not tolerate the earplugs. In this study, the patients were asked to use the earplugs and eye masks after the subjective sleep quality questionnaires were completed on the 4th day after admission in order to make the patients adapt to them, which helped tolerating the noise after the operation and improved sleep quality. In contrast, only conventional healthcare and health guidance were provided for the patients in the conventional group. Although the patients were also informed of the related knowledge, no intervention was provided, and thus the effectiveness was poor.
Conclusion
The findings of this study provide scientific evidence those non-drug interventions including CBT and acousto-optic protective measures (noise cancelling earplugs and eye masks) could effectively improve the sleep quality of the patients after mechanical valve implantation. Nevertheless, new mechanical valves producing less noise are now being commercialized. Therefore, these new valves should have a lower requirement for sleep drug therapy, and a non-drug approach should be able to overcome these noises.
Limitations
There are various limitations of this study:
This study only investigated sleep quality in patients after the selective implantation of a mechanical mitral valve.
The patients do not represent all the inpatients of the Department of Cardiac Surgery or even all hospitalized patients; there could be a selection bias.
The CBT and acousto-optic protective measures were defined in combination as the non-drug intervention.
No cost-effectiveness analysis has been made to determine if this intervention was less expensive than the lifetime use of sleep drugs. Future studies should look at this issue.
Disclosure Statement
The study was supported by Fujian Province Medical Innovation Fund Projects (No. 2012-CXB-17), National Key Subject Construction Project (No. 2011-1018), National Key Construction Projects of Clinical Nursing (No. 2013-544) and Countryside-Oriented Grassroots Promotion Projects (No. 2014011).
Conflict of Interests
The author declares that they have no conflict of interests.
References
- 1).Ford ES. Trends in predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol 2013; 61: 2249-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Redeker NS, Ruggiero J, Hedges C. Patterns and predictors of sleep pattern disturbance after cardiac surgery. Res Nurs Health 2004; 27: 217-24. [DOI] [PubMed] [Google Scholar]
- 3).Orwelius L, Nordlund A, Nordlund P, et al. Prevalence of sleep disturbances and long-term reduced health-related quality of life after critical care: a prospective multicenter cohort study. Crit Care 2008; 12: R97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Cooper AB, Thornley KS, Young GB, et al. Sleep in critically ill patients requiring mechanical ventilation. Chest 2000; 117: 809-18. [DOI] [PubMed] [Google Scholar]
- 5).Dobie DJ, Kivlahan DR, Maynard C, et al. Screening for post-traumatic stress disorder in female Veteran’s Affairs patients: validation of the PTSD checklist. Gen Hosp Psychiatry 2002; 24: 367-74. [DOI] [PubMed] [Google Scholar]
- 6).Bucerius J, Gummert JF, Borger MA, et al. Predictors of delirium after cardiac surgery delirium: effect of beating-heart (off-pump) surgery. J Thorac Cardiovasc Surg 2004; 127: 57-64. [DOI] [PubMed] [Google Scholar]
- 7).Achermann P, Borbely AA. Dynamics of EEG slow wave activity during physiological sleep and after administration of benzodiazepine hypnotics. Hum Neurobiol 1987; 6: 203-10. [PubMed] [Google Scholar]
- 8).Borbely AA, Mattmann P, Loepfe M, et al. Effect of benzodiazepine hypnotics on all-night sleep EEG spectra. Hum Neurobiol 1985; 4: 189-94. [PubMed] [Google Scholar]
- 9).Hu RF, Jiang XY, Zeng YM, et al. Effects of earplugs and eye masks on nocturnal sleep, melatonin and cortisol in a simulated intensive care unit environment. Crit Care 2010; 14: R66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Meyer TJ, Eveloff SE, Bauer MS, et al. Adverse environmental conditions in the respiratory and medical ICU settings. Chest 1994; 105: 1211-6. [DOI] [PubMed] [Google Scholar]
- 11).Wang XD, Wang XL, Ma H. Rating scales for mental health. Chinese Ment Health J 1999: 375-8. [Google Scholar]
- 12).Pigeon WR. Treatment of adult insomnia with cognitive-behavioral therapy. J Clin Psychol 2010; 66: 1148-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193-213. [DOI] [PubMed] [Google Scholar]
- 14).Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med 2008; 4: 563-71. [PMC free article] [PubMed] [Google Scholar]
- 15).He HX, Fu LQ, Wang P. Attribution analysis on sleep quality and influencing factors of cardiac surgical patients in intensive care unit. Mod Prev Med 2012; 723-4. [Google Scholar]
- 16).Richardson SJ. A comparison of tools for the assessment of sleep pattern disturbance in critically ill adults. Dimens Crit Care Nurs 1997; 16: 226-39; quiz 240-2. [DOI] [PubMed] [Google Scholar]
- 17).Edell-Gustafsson UM, Hetta JE, Aren GB, et al. Measurement of sleep and quality of life before and after coronary artery bypass grafting: a pilot study. Int J Nurs Pract 1997; 3: 239-46. [DOI] [PubMed] [Google Scholar]
- 18).Aaron JN, Carlisle CC, Carskadon MA, et al. Environmental noise as a cause of sleep disruption in an intermediate respiratory care unit. Sleep 1996; 19: 707-10. [DOI] [PubMed] [Google Scholar]
- 19).Nishi K, Eishi K, Shibata Y, et al. Influence of prosthetic heart valve sound on a patient’s quality of life. Ann Thorac Cardiovasc Surg 2010; 16: 410-6. [PubMed] [Google Scholar]
- 20).Friese RS. Sleep and recovery from critical illness and injury: a review of theory, current practice, and future directions. Crit Care Med 2008; 36: 697-705. [DOI] [PubMed] [Google Scholar]