Abstract
Background
Salmonella brain abscess associated with brain tumor is rare. Only 11 cases have been reported to date. Here we report a case of brain abscess caused by Salmonella entericaserovarEnteritidis mimicking post-surgical meningitis in a patient with glioblastoma multiforme.
Case presentation
A 60-year-old Algerian woman was admitted through an emergency department for a 4-day history of headache, nausea and vomiting, and behavioral disorders. Surgery for cerebral tumor excision was performed and histopathological analysis revealed glioblastoma multiforme. On the seventh day post-surgery, she presented a sudden neurological deterioration with a meningeal syndrome, confusion, and fever of 39.8°C. Her cerebrospinal fluid sample and blood cultures were positive for S. enterica Enteritidis. She was treated with ceftriaxone and ciprofloxacin. On the 17th day post-surgery, she presented a new neurological disorder and purulent discharge from the surgical wound. Brain computed tomography revealed a large cerebral abscess located at the operative site. Surgical drainage of the abscess was performed and microbial cultures of surgical deep samples were positive for the same S. enterica Enteritidis isolate. She recovered and was discharged 6 weeks after admission.
Conclusions
In this case report, a brain abscess was initially diagnosed as Salmonella post-surgical meningitis before the imaging diagnosis of the brain abscess. The diagnosis of brain abscess should be considered in all cases of non-typhoidal Salmonella meningitis after surgery for brain tumor. Surgical brain abscess drainage followed by prolonged antibiotic treatment remains a major therapeutic option.
Keywords: Brain abscess, Glioblastoma, Post-surgery meningitis, Salmonella, Salmonella enterica, MALDI-TOF, Bacteria, Infection, Human
Background
Salmonella species are mainly known as common agents of gastroenteritis worldwide. Invasive Salmonella infections have been reported due to their potential to cause focal suppurative complications in urinary tract infection, osteoarticular infection and liver abscess [1]. Central nervous system Salmonella infection is rare and occurs primarily in young children [2] and immunocompromised adults, including human immunodeficiency virus (HIV) infection and co-infected patients [3] and chronic granulomatous disease [4]. Here, we report a case of brain abscess caused by S. enterica subspecies (subsp.) entericaserovar Enteritidis mimicking post-surgical meningitis in a patient with glioblastoma multiforme. We also review cases of Salmonella brain abscess in patients with cerebral tumors.
Case presentation
In September 2015, a 60-year-old Algerian woman was seen in the emergency department in Marseille, France for a 4-day history of headache, nausea and vomiting, and behavioral disorders. She had an unremarkable medical history apart from obesity (body mass index at 30.9 kg/m2). Brain magnetic resonance imaging (MRI) revealed a single 40×35 mm tumor in her right mesial temporal region and a mass effect compression of her right lateral ventricle with transtentorial herniation (Fig. 1). She was transferred to our neurosurgery department, where levetiracetam and methylprednisolone led to neurological improvement. At that time, her leukocyte count was elevated at 22×109/L (neutrophil count was 21×109/L, lymphocytes were decreased at 0.47×109/L, and her platelet count was 291×109/L). Surgery for tumor removal was performed on day 5 of her admission. A histological examination revealed glioblastoma multiforme (Fig. 2). No bacteria were seen on histological analysis.
Fig. 1.
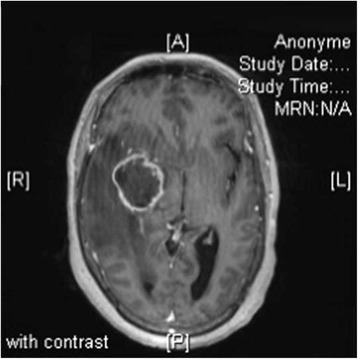
Brain magnetic resonance imaging revealed a single 40×35 mm tumor in the right mesial temporal region and a mass effect compression of the right lateral ventricle with transtentorial herniation
Fig. 2.
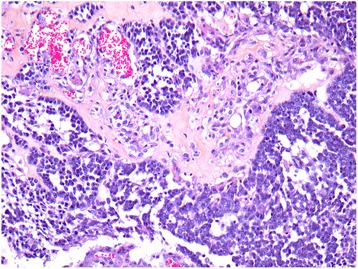
A histological examination revealed glioblastoma multiforme without any microorganism identified on histological analysis
On the seventh day post-surgery, she presented a sudden neurological deterioration with a meningeal syndrome, confusion and fever of 39.8 °C. Laboratory investigations revealed an elevated leukocyte count at 13×109/L, elevated neutrophils at 12.62×109/L, low lymphocytes at 0.15×109/L, normal platelets at 154×109/L, and elevated C-reactive protein at 304 mg/L. Cerebrospinal fluid (CSF) sample analysis revealed an elevated protein level of 2.93 g/L, a low glucose level of 0.1 mmol/L, and a leukocyte count of 5400 cells/mm3 with 80 % neutrophils. CSF cultures and blood cultures were positive for S. enterica. The isolates from the CSF and blood were further identified as S. enterica subsp. enterica serotype Enteritidis as identified by our national reference center for Salmonella (Institut Pasteur, Paris). The isolates were susceptible in vitro to amoxicillin, ceftriaxone, imipenem/cilastatin, gentamycin, co-trimoxazole and fluoroquinolone.
A diagnosis of Salmonella meningitis was made and she was treated with ceftriaxone administered intravenously 2 g/day and oral ciprofloxacin 500 mg every 8 hours. On the 17th day post-surgery, she presented a new neurological disorder and purulent discharge from the surgical wound. Brain computed tomography (CT) revealed a large cerebral abscess located at the operative site (Fig. 3). Surgical drainage of the abscess was performed by craniotomy, which confirmed the diagnosis of intraparenchymal abscess located at the glioblastoma resection site. Microbial cultures of surgical deep samples were positive for S. enterica subsp. entericaserovar Enteritidis, which were susceptible to all antibiotics tested above. She was discharged 6 weeks after admission. Prolonged 10-day anaerobic bacterial cultures of her CSF, bloodstream and brain abscess were negative. A combination of ceftriaxone-ciprofloxacin was given for 6 weeks, and ciprofloxacin treatment was prolonged for 3 months because of the infectious risk due to chemotherapy immunosuppression. No neurological sequelae were noted. Evaluation of the immune system remained normal and HIV serology was negative.
Fig. 3.
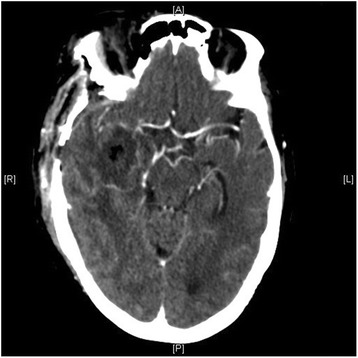
Computed tomography reveals a large cerebral abscess located at the operative site
Discussion
Here we report a case of brain abscess due to S. enterica subsp. entericaserovar Enteritidis mimicking meningitis occurring after surgery for glioblastoma. Salmonella brain abscesses are rarely reported. Only a few cases of typhoidal Salmonella brain abscess have been reported in immunocompetent adults, usually related to situations promoting their incidence, including recent travel in endemic areas [5], typhoid fever [6], or ingestion of contaminated milk [7]. To the best of our knowledge, only 11 cases of Salmonella brain abscess associated with brain tumor have been reported [8–18]. Most of these cases (nine cases) were caused by non-typhoidal Salmonella, including eight cases of S. enterica Enteritidis and one case of Salmonella enterica Typhimurium. However, S. enterica Typhimurium is usually responsible for invasive human salmonellosis [19]. Glioblastoma is the main type of brain tumor that has been associated with Salmonella brain abscess (four cases), and all of these cases were caused by S. enterica Enteritidis (Table 1).
Table 1.
Review of 12 cases of Salmonella brain abscess related to brain tumors reported in the literature and in our case
| Cases | Age, sex, geographical origin | Cerebral tumor | Tumor surgery before diagnosis of brain abscess | Patients under systemic corticosteroid treatment | Clinical symptoms | Surgical drainage | Antibiotic treatment | Salmonella species | Clinical outcome |
|---|---|---|---|---|---|---|---|---|---|
| Our case (2015) | 60 years, female, Algeria | Yes, multiforme glioblastoma | Yes | Yes | Sudden neurological deterioration, meningeal syndrome | Yes | Yes, 3 months | Salmonella Enteritidis (CSF, blood, pus, brain abscess) | Good |
| Rodriguez, Valero, and Watanakunakorn 1986 [8] | 28 years, male, Ohio (USA) | Yes, metastatic carcinoma | No | Yes | Per orbital pain, nausea, papilledema | Yes | Yes, 6 weeks (radiotherapy) | Salmonella Enteritidis (brain tissue and blood) | Good |
| Sharma, Raja, and Shivananda 1986 [9] | 32 years, male, India | Yes, malignant astrocytoma | Yes | No | Headache, vomiting, somnolence | Yes | Yes, unknown duration | Salmonella Typhi | Good |
| Noguerado et al. 1987 [10] | 78 years, male, Spain | Yes, multiforme glioblastoma | No | Yes | General conditions deteriorated, fever, meningeal syndrome, septic shock | No | Yes | Salmonella Enteritidis (CSF and blood) | Died |
| Bossi et al. 1993 [11] | 24 years, male, Tunisia | Yes, multiforme glioblastoma | Yes | Yes | Fever, confusion | Yes | Yes, unknown duration | Salmonella Enteritidis (CSF, blood and brain abscess) | Good |
| Shanley and Holmes 1994 [12] | 28 years, female, Hawaii (USA) | Yes, craniopharyngioma | No | Not mentioned | Sudden loss of vision | Yes, Hypophysectomy to decompress optic chiasm | Not mentioned | Salmonella Typhi (pus, brain abscess) | Good |
| Fiteni et al. 1995 [13] | 49 years, female, France | Yes, astrocytoma | Yes | Yes | Fever, confusion | Yes | Yes, 9 weeks | Salmonella Enteritidis (CSF, blood and brain abscess) | Residual hemiparesis |
| Sarria, Vidal, and Kimbrough Iii 2000 [14] | 58 years, female, Texas (USA) | Yes, multiforme glioblastoma | No | Yes | Fever, meningeal syndrome, hemiparesis, coma | Yes | Yes, 6 weeks and local application | Salmonella Enteritidis (material) | Died |
| Kumari and Kan 2000 [15] | 59 years, male, Washington (USA) | Yes, metastatic adenocarcinoma | Yes | Yes | Fever, tachycardia, confusion | Yes | Yes, 6 weeks | Salmonella typhimurium (cerebral abscess) | Good |
| Schröder et al. 2003 [16] | 46 years, female, Germany | Yes, craniopharyngioma | Yes | Yes | Tension, headache at craniotomy site | Yes | Yes, duration not known | Salmonella Enteritidis (pus, brain abscess) | Coxitis abscess |
| Aissaoui et al. 2006 [17] | 72 years, male, Morocco | Yes, oligodendroglioma | Yes | Yes | Fever, neurological deterioration | No | Yes, 8 days then patient died | Salmonella Enteritidis (CSF and blood) | Died |
| Sait et al. 2011 [18] | 57 years, male, not known | Yes, multiforme glioblastoma | Yes | No | Headache, discharge wound, meningeal signs | Yes | Yes, 4 weeks | Salmonella Enteritidis (material and blood) | Good |
CSF cerebrospinal fluid
Symptoms of Salmonella brain abscess associated with brain tumor are heterogeneous. Most cases (six cases) have occurred after surgical resection of a brain tumor, initially indicated by fever or neurological deterioration and confusion. However, meningeal signs were noted in three reported cases. In our case, the brain abscess was initially diagnosed as Salmonella post-surgical meningitis before imaging diagnosis of the brain abscess. In our case, the diagnosis of glioblastoma multiforme was suggested by brain MRI and confirmed by a histological examination of the surgical biopsy. In vivo imaging technology, such as molecular imaging, is useful in the diagnosis of brain tumors [20] and might be helpful to differentiate bacterial abscess from tumoral tissues and underlying primary disease [21].
In the literature, Salmonella species have been identified in purulent exudates from brain abscesses (six cases) and in blood cultures (six cases) and CSF cultures (four cases). In our case, Salmonella isolates were identified in the blood, CSF and brain abscess. Most cases in the literature were treated with systemic corticosteroids for brain tumor (eight cases) when the Salmonella brain abscess was diagnosed. The prognosis is relatively good with antibiotic treatment. There is no comparative study on the use of dual antibiotic therapy rather than single antibiotic for this indication. Nevertheless, we decided to treat our case initially with a 6-week combination of ceftriaxone-ciprofloxacin due to a significant risk of immunosuppression related to treatment of the glioblastoma multiforme and the large brain abscess. The duration of antibiotic treatment in the literature varied from 4 weeks to 3 months. Most cases in the literature (nine cases) were treated surgically for the brain abscess. However, three patients died and two patients had complications, including residual hemiparesis in one case and a hip abscess in one case.
Chronic carriage of Salmonella, primarily biliary, may persist after infection (about 1 % of cases) [22]. In our case, septic signs and digestive symptoms such as gastroenteritis were absent on admission and the clinical symptoms of brain abscess such as fever, meningeal signs, and neurological deterioration occurred only at 1 week post-surgery for glioblastoma. These phenomena might be explained by Salmonella’s tropism for necrotic tissue [23], and the central nervous system infection could be secondary to blood dissemination of Salmonella from digestive reservoirs in the bile or intestine. Unfortunately, this hypothesis is difficult to confirm due to the transitory carriage and because a stool culture had unfortunately not been performed.
Conclusions
Salmonella brain abscess is rare but can occur in apparently immunocompetent adult patients with brain tumor. The diagnosis of brain abscess should be considered in all cases of non-typhoid Salmonella meningitis after surgery for brain tumor. Prolonged antibiotic treatment after surgical brain abscess drainage remains a major therapeutic option.
Acknowledgements
We thank the house officers and medical staff for their confidence in our management of the patient.
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. No assistance was utilized in the writing of this manuscript.
Availability of data and supporting materials
Medical imaging data will not be shared because it is not fully anonymous.
Authors’ contributions
LL: 1st author, clinical data collection; he was involved in drafting the manuscript. GD: 2nd author, microbiological data collection, manuscript revision. TG: 3rd author, clinical data verification and manuscript revision. EH: 4th author; surgical data verification and manuscript revision. HL: 5th author, histological analysis, manuscript revision, and discussion section. MD: 6th author, microbiological data verification and manuscript revision. PS: first final author and corresponding author; he made substantial contributions to study conception and design, clinical data verification, discussion section, and manuscript revision. AS: second final author, clinical data verification, discussion section, and final approval of the version to be published. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- 1.Wilkins EGL, Roberts C. Extraintestinal salmonellosis. Epidemiol Infect. 1988;100:361–368. doi: 10.1017/S095026880006711X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy D, Oshin F. Reptile-associated salmonellosis in children aged under 5 years in South West England. Arch Dis Child. 2015;100:364–5. doi: 10.1136/archdischild-2014-306134. [DOI] [PubMed] [Google Scholar]
- 3.Aliaga L, Mediavilla JD, López de la Osa A, Melander E, López-Gómez M, de Cueto M, et al. Nontyphoidal Salmonella Intracranial Infections in HIV-Infected Patients. Clin Infect Dis. 1997;25:1118–20. doi: 10.1086/516101. [DOI] [PubMed] [Google Scholar]
- 4.Ma J-S, Chen P-Y, Lau Y-J, Chi C-S. Brain abscess caused by Salmonella enterica subspecies houtenae in a patient with chronic granulomatous disease. J Microbiol Immunol Infect Wei Mian Yu Gan Ran Za Zhi. 2003;36:282–4. [PubMed] [Google Scholar]
- 5.Bonvin P, Ejlertsen T, Dons-Jensen H. Brain Abscess Caused by Salmonella enteritidis in an Immunocompetent Adult Patient: Successful Treatment with Cefotaxime and Ciprofloxacin. Scand J Infect Dis. 1998;30:632–3. doi: 10.1080/00365549850161313. [DOI] [PubMed] [Google Scholar]
- 6.Suzuki Y, Sugiyama Y, Ishii R, Sato I. Brain abscess caused by Salmonella typhi. J Neurosurg. 1976;45:709–11. doi: 10.3171/jns.1976.45.6.0709. [DOI] [PubMed] [Google Scholar]
- 7.Ellis ME, Smith CC, Reid TM, Porter IA. Chloramphenicol-resistant Salmonella typhimurium meningitis in an adult. Br Med J (Clin Res Ed) 1981;283:273. doi: 10.1136/bmj.283.6286.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez RE, Valero V, Watanakunakorn C. Salmonella focal intracranial infections: review of the world literature (1884-1984) and report of an unusual case. Rev Infect Dis. 1986;8:31–41. doi: 10.1093/clinids/8.1.31. [DOI] [PubMed] [Google Scholar]
- 9.Sharma S, Raja A, Shivananda PG. Isolation of Salmonella typhi from brain tumor--a case report. Indian J Med Sci. 1986;40:233–5. [PubMed] [Google Scholar]
- 10.Noguerado A, Cabanyes J, Vivancos J, Navarro E, Lopez F, Isasia T, et al. Abscess caused by Salmonella enteritidis within a glioblastoma multiforme. J Infect. 1987;15:61–3. doi: 10.1016/S0163-4453(87)91476-9. [DOI] [PubMed] [Google Scholar]
- 11.Bossi P, Mion G, Brinquin L, Bonsignour JP. [Postoperative brain abscess caused by Salmonella enteritidis] Presse Médicale Paris Fr 1983. 1993;22:130. [PubMed] [Google Scholar]
- 12.Shanley DJ, Holmes SM. Salmonella typhi abscess in a craniopharyngioma: CT and MRI. Neuroradiology. 1994;36:35–6. doi: 10.1007/BF00599192. [DOI] [PubMed] [Google Scholar]
- 13.Fiteni I, Ruiz FJ, Crusells MJ, Sanjoaquin I, Guillen G. [Salmonella enteritidis multifocal infection of the central nervous system. Efficacy of new cephalosporins] Presse Médicale Paris Fr 1983. 1995;24:309–11. [PubMed] [Google Scholar]
- 14.Sarria JC, Vidal AM, Kimbrough RC., III Salmonella enteritidis brain abscess: case report and review. Clin Neurol Neurosurg. 2000;102:236–9. doi: 10.1016/S0303-8467(00)00099-8. [DOI] [PubMed] [Google Scholar]
- 15.Kumari P, Kan VL. Salmonella typhimurium Brain Abscess: Postoperative Complication. Clin Infect Dis. 2000;30:621–2. doi: 10.1086/313729. [DOI] [PubMed] [Google Scholar]
- 16.Schröder J, Palkovic S, Kipp F, Wassmann H. Salmonella enteritidis causing brain abscess and coxitis following intracranial surgery. Acta Neurochir (Wien) 2003;145:919–21. doi: 10.1007/s00701-003-0106-2. [DOI] [PubMed] [Google Scholar]
- 17.Aissaoui Y, Azendour H, Balkhi H, Haimeur C, Atmani M. [Postoperative meningitis caused by an unusual etiological agent: Salmonella enteritidis] Neurochirurgie. 2006;52:547–50. doi: 10.1016/S0028-3770(06)71365-0. [DOI] [PubMed] [Google Scholar]
- 18.Sait M, Rahmathulla G, Chen TL, Barnett GH. Rare case of intracranial Salmonella enteritidis abscess following glioblastoma resection: Case report and review of the literature. Surg Neurol Int [Internet]. 2011[cited 2015 Nov 29];2. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3205504/. [DOI] [PMC free article] [PubMed]
- 19.Kwambana-Adams B, Darboe S, Nabwera H, Foster-Nyarko E, Ikumapayi UN, Secka O, et al. Salmonella Infections in The Gambia, 2005-2015. Clin Infect Dis Off Publ Infect Dis Soc Am. 2015;61(Suppl 4):S354–362. doi: 10.1093/cid/civ781. [DOI] [PubMed] [Google Scholar]
- 20.Schaller BJ, Modo M, Buchfelder M. Molecular Imaging of Brain Tumors: A Bridge Between Clinical and Molecular Medicine? Mol Imaging Biol. 2007;9:60–71. doi: 10.1007/s11307-006-0069-9. [DOI] [PubMed] [Google Scholar]
- 21.Tewari A, Padma S, Sundaram PS. The diagnostic role of 18-fluorodeoxyglucocose-positron emission tomography/computed tomography in occult bacteremia searching underlying primary disease. Ann Indian Acad Neurol. 2012;15:336–8. doi: 10.4103/0972-2327.104353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buchwald DS, Blaser MJ. A Review of Human Salmonellosis: II. Duration of Excretion Following Infection with Nontyphi Salmonella. Rev Infect Dis. 1984;6:345–56. doi: 10.1093/clinids/6.3.345. [DOI] [PubMed] [Google Scholar]
- 23.Forbes NS. Engineering the perfect (bacterial) cancer therapy. Nat Rev Cancer. 2010;10:785–94. doi: 10.1038/nrc2934. [DOI] [PMC free article] [PubMed] [Google Scholar]


