Abstract
A much forgotten figure in the history of artificial and natural light therapies, the nurse played a central role in the administration of beneficial - and harmful - ultraviolet radiation in the treatment of skin diseases, tuberculosis and rickets, especially on child patients. As the primary operators of light therapy equipment, nurses specialised in this new and modern treatment, and both the therapy’s successes and failures could be attributed to their skill, or lack thereof. This paper provides an introduction to the history of light therapy, especially phototherapy (artificial light therapy), during the early twentieth century in Britain, and to the ‘invisible’ technicians who contributed so much to its nascent reputation.
Keywords: Lupus vulgaris, Ultraviolet Radiation, Heliotherapy, Phototherapy, Historical
Setting the Scene
In his 1931 book, The Fundamental Principles of Ray Therapy, Dr William Beaumont described facilities offering the latest treatments using light, especially ultraviolet light, to cure illnesses (Beaumont, 1931). One of these was the Municipal Sunlight Clinic in St Pancras, which opened its doors in 1925. It was enthusiastically described in The Times as the first clinic for artificial light therapy in London, operating out of an infant welfare centre in Highgate. The child patients were referred for treatment here by the Medical Officers of the infant welfare centres in the borough, under the authority of its Medical Officer of Health (The Times, 1925).
Figure 1 captures a group of seven babies and toddlers at the Clinic undergoing exposure to a carbon arc lamp, a device producing a similar spectrum of infrared, visible and ultraviolet light to that of natural sunlight, but here conveniently available ‘on demand.’ We see the treatment taking place, as was usual, in a darkened, enclosed interior space. The children encircle the lamp while they play with toys, musical instruments and a mat printed with animals. The mat doubled as a safety device; its edge marked the correct, safe distance for the children to sit, not only to prevent overexposure to the light but also to avoid the spluttering ash of the carbon rods as they burned away.
Figure 1.
‘A Corner of the Municipal Sunlight Clinic, St. Pancras, showing children under five years of age being treated with a long flame carbon arc,’ in Beaumont W (1931) Fundamental Principles of Ray Therapy: An Elementary Textbook for Nurses, Students, and Practitioners. H. K. Lewis & Co. Ltd., London, fig.2, p.5.
The children, nude except for requisite goggles, play under the encouragement of a doctor and - only partly in shot - a nurse, in order to entertain them during these exposures, which could last from several minutes up to two hours at a time. This kind of group treatment was tailored to general (full body) exposures, the lamp used to treat children suffering from a range of illnesses, chief among them deficiency disorders like rickets. But lamps like these were used for several external forms of tuberculosis, including bone and joint tuberculosis, as well as lupus vulgaris (tuberculosis of the skin), and curatively and preventively for various kinds of infections and colds.
Archival photographs of the treatments focus not surprisingly on patients and the equipment, but ubiquitous in the visual culture of light therapy is the figure of the nurse as a watchful presence and intimate carer. Yet when it comes to reading about light therapy, the nurse disappears from view in the literature; highly visible in images, seemingly invisible in texts. This paper brings to light these so-called invisible operators, nurses with ‘flare’: these individuals had a natural ability or ‘flair’ for working with the emanating, burning rays of therapeutic light. As opposed to physicians, they were the primary operators of light therapy equipment during day-to-day practice, both in and out of doors. To do their jobs well, and significantly to avoid injuring the sensitive skin of their patients, they needed to be highly observant and highly skilled in controlling light. The very reputation of the therapy depended upon it.
Modern Light Therapy’s Origins
By the 1920s both natural sun therapy, known as heliotherapy, and artificial light therapy using lamps, termed phototherapy, were popular and respected treatments in Britain and abroad. They had both been employed since at least the 1890s, especially for the treatment of tuberculosis. Modern phototherapy is attributed to the work of the Danish physician and Nobel laureate, Niels Finsen, who systematised the use of blue, violet and ultraviolet light to treat lupus vulgaris using his ‘Finsen lamp.’
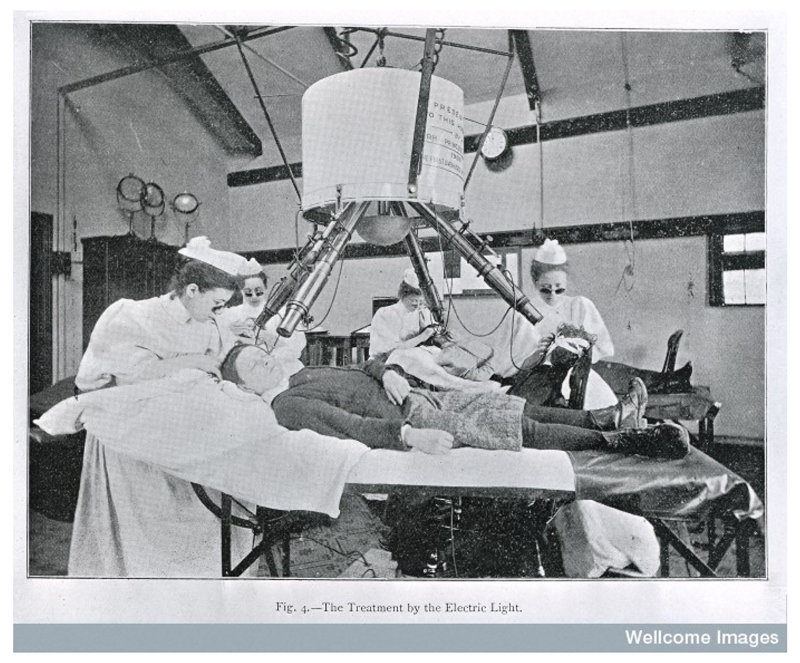
As demonstrated in Figure 2, this large-scale modified carbon arc lamp had four telescopic arms that filtered the emanating light and directed it down onto lupus lesions. A nurse was required to position and hold the patient in place with consistent pressure, sometimes up to two hours at a time, on each lesion. Four patients could be treated simultaneously, each with their own attending nurse. In Britain the Finsen lamp was introduced first to the Royal London Hospital by Queen Alexandra, who visited Finsen’s Institute in Copenhagen and was so impressed by its successful results that she imported one of his lamps for the hospital (Figure 3).
Figure 2.
Apparatus devised by N.R. Finsen for treating disease with ultra-violet rays. Apparatus in use. Presented to hospitals in 1900 by Princess Alexander of Wales. Wellcome Library and Wellcome Images, London, reference L0001449.
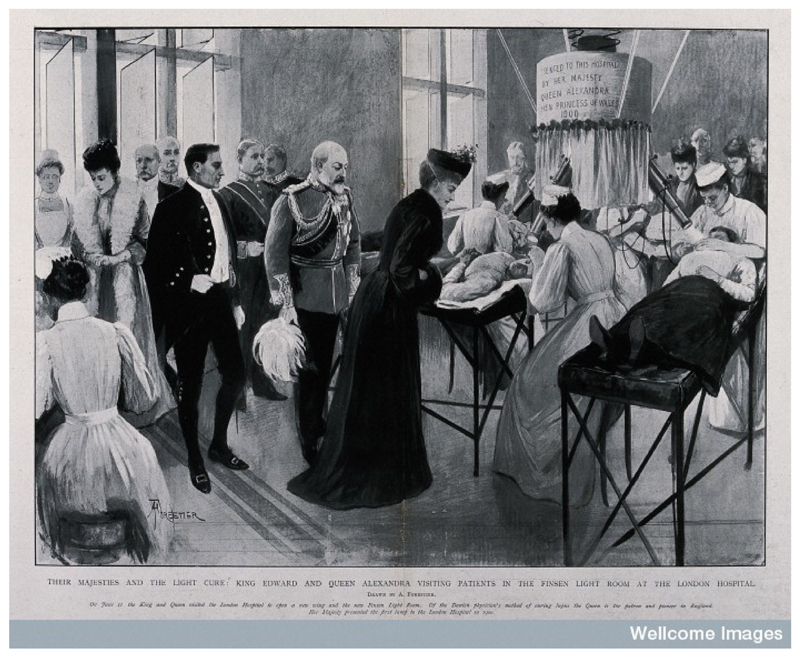
Figure 3.
The London Hospital, Whitechapel: King Edward VII and Queen Alexandra in the Finsen Light room. Process print after a drawing by Amedée Forestier, c.1903. Wellcome Library and Wellcome Images, reference V0013771.
For medical historian Annie Jamieson (2010, p.115), ‘The role of the nurse attendants in the success of the Finsen treatment cannot be underestimated.’ As Jamieson explains, from its inception as a treatment its success was attributed as much, and sometimes even more, to the nurse than to the supervising physician - and this directly from the mouths of skin specialists Drs James Sequeira, of the Royal London Hospital, and Malcolm Morris of St. Mary’s. Morris (1904, p.1131) wrote that Finsen nurses should be ‘…endowed with special gifts of character and temper which, in my experience, are comparatively rare.’ These nurses were greatly praised for their attention to detail, meticulous technique, and patience.
Nurses from around the world journeyed to the Finsen Institute, in Copenhagen, alongside physicians in order to receive this specialist training. In turn the Institute would send over its own nurses to teach staff at host institutions abroad on proper technique. Morris welcomed them to his practice at Campden Hill, so did St Thomas’ Hospital, and this extended well into the 1920s for general and local phototherapy. Continuing into the 1930s, Dr G. Murray Levick (1930, p.33) took special care to mention and thank his nursing staff at the Chailey Heritage Craft Schools and Hospitals, singling out the Matron, Miss Margaret Machell.
Training and Specialisation
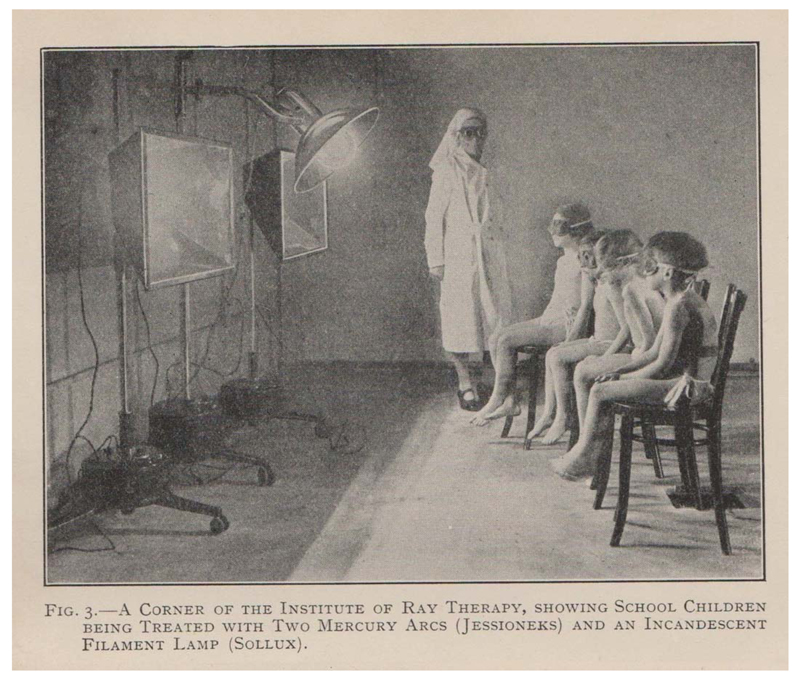
The London Hospital would soon offer its own training opportunities to nurses from hospitals throughout Britain, and later phototherapy training became part of a larger training course on medical electricity offered to nurses and masseuses at hospitals, such as St. Thomas’ and Guy’s, as well as at clinics like the London Light Clinic in Pimlico and the Institute for Ray Therapy in Camden, the latter also run by Dr Beaumont (Figure 4).
Figure 4.
‘A Corner of the Institute to Ray Therapy, showing school children being treated with two mercury arcs (Jesioneks) and an incandescent filament lamp (Sollux),’ in Beaumont W (1931) Fundamental Principles of Ray Therapy: An Elementary Textbook for Nurses, Students, and Practitioners. H. K. Lewis & Co. Ltd., London, fig.3, p.6.
The examinations were set and overseen by the Chartered Society of Massage and Medical Gymnastics from the 1920s, and there are references to these training courses also in books on light therapy written for nurses, by nurses, for example in Myrtle Vaughan-Cowell’s 1928 Artificial Sunlight (pp.98-99). Vaughan-Cowell worked with Dr Edward James Deck at the London Light Clinic, and her many qualifications included nursing, midwifery, massage and medical electricity, a certificate from the New Zealand Plunket Society, and heliotherapy. In her book she (p.69) stated that, ‘Treatment of course must always be administered under medical supervision, but the doctor very often leaves much of the actual “carrying-out” of the treatment to his nurse or masseuse…’ This did not always meet with patients’ approval, according to the physician Alexander Cawadias (1937, p.228):
The physician should himself give ultra-violet treatment, and not leave it to a nurse. He may be helped, but his personal activity is absolutely necessary. I have heard of complaints from patients who have gone to physicians for ultra-violet treatment and objected when the irradiations, which they regarded as a rather delicate procedure, were entrusted to nurses.
Clearly tensions existed as to who took control of the equipment and its daily use, indicating that nurses had perhaps more authority, skill, and experience than their supervising physicians in many light clinics and hospital departments.
Indispensable Skill
There are frequent references to light therapy within the journal, The Nursing Record & Hospital World, and one of its correspondents (NRHW, 1900, p.4), commenting on light therapy, reported as early as 1900 ‘…how indispensable the services of skilled nurses have become in the scientific treatment of disease.’ Their skills were not only directed towards carrying out the treatments and nursing patients, but also maintaining and cleaning the equipment. An arduous and meticulous task, each device needed to be dusted, cleaned and polished, its bulbs carefully wiped with silk, its castors and axles oiled, and its bolts tightened. Vaughan-Cowell (1928, pp.52-53) declared, ‘The maximum efficiency of your apparatus will depend greatly upon perfect cleanliness.’
Such devotion and care by nurses towards modern medical technology was not restricted to light therapy equipment, of course. Margarete Sandelowski (2000, p.61), a historian of American nursing and technology, has similarly written about the central role of thermometers, stethoscopes and X-ray equipment to the development of twentieth-century nursing:
Because devices were increasingly central components of the procedures nurses performed, ‘nursing the equipment’ became as important as nursing the patient. Indeed, the safe, effective, efficient, and finished care of patients depended in large part on the quality of nurses’ care of equipment at and away from the bedside.
It is clear from Sandelowski’s research that historically nurses have been proficient technophiles who actively and eagerly engaged with new and complex technologies. For light therapy nurses, competency was required not only to handle the electrical equipment, but also its dangerous light rays and their effects on patients’ delicate skin and eyes.
Sense and Sensitivity
Images of light therapy feature nurses calmly and competently observing patients as they undergo treatment (Figures 4-5). Out of doors, natural sunlight was, like the ultraviolet lamp, used to disinfect wounds, kill harmful bacteria in the body, and revitalise the blood. The light’s beneficial effects were judged through solar erythema (sunburn) production and pigmentation (tan) on the patient’s skin, necessitating close observation for both artificial and natural forms of light therapy.
Figure 5.
‘Sandy Point, Hayling Island branch of the Lord Mayor Treloar Cripples’ Hospital and College, Alton,’ in William Treloar W (1918) The Cure of Tuberculous Children. The Graphic (21 December 1918): 739.
Figure 5 illustrates a beach scene on Hayling Island, a seaside branch of the Lord Mayor Treloar Cripples’ Hospital and College in Alton (Hants), which was run by Britain’s most well-known heliotherapist, Sir Henry Gauvain. Gauvain used both heliotherapy and phototherapy to treat primarily children suffering from bone and joint tuberculosis, and on Hayling Island he supplemented heliotherapy with balneotherapy (therapeutic sea-bathing). Many photographs from the Treloar archives highlight the intimacy between its nurses and child patients, who smile and hug each other. Perhaps this is not surprising considering that most of these children spent many months and even years being treated at these facilities in the decades before antibiotics.
Sandelowski (2000, pp.84-85) has further explained that specialist nurses working with new medical technologies would likely have also had to call upon their training and empathy to help young patients frightened of such daunting, noisy, and glaring electrical equipment. As she (2000, p.2) states, ‘A significant component of the “sentimental work” of the nurse has entailed educating patients about new devices, getting patients to accept and comply with their use, and alleviating patients’ fears about them.’
This was certainly the case with phototherapy, Vaughan-Cowell (1928, p.66) noting that children were frequently nervous when first exposed to the lamps and required sensitivity, patience and encouragement. For those children scared of the protective goggles (Figures 1, 4), she suggested tying a pair of glasses first around a doll, so that the child would follow suit. The compliant child enabled safe exposures since getting too close to the lamp (or spending too long in the sun) meant potentially dangerous burns, while not wearing goggles resulted in painful conjunctivitis. Textbooks on light therapy were adamant that goggles had to be worn at all times by both patient and operator, emphasising how often student nurses forgot to wear them, only to suffer greatly later (Vaughan-Cowell, 1928, p.59). Nurses particularly sensitive to ultraviolet light were also urged to wear hoods and gloves (Russells, 1925, p.149). Only great care and constant vigilance ensured protection from the invisible rays.
Invisible Operators
Returning to the topic of nurses’ ‘invisible’ presence in the history of light therapy, the problem remains one of access: limited or non-existent sources, restricted archives, and lost memories (Sandelowski, 2000, p.15; Howell, 1996, p.12). So, how do we make these forgotten agents visible, and do justice to their contribution, and to what aim? As explored in the recent exhibition, ‘The Kiss of Light,’ at the Florence Nightingale Museum (May-October 2015), light therapy nurses were skilled technicians, watchful observers, intimate carers and public regulators (Woloshyn, 2015).
By shifting focus onto lesser-known operators and their technological apparel, we encounter light therapy during the early twentieth century as a new and modern treatment seeking to gain legitimacy. Whenever its reputation was called into question, and its results and medical value questioned, its strongest defenders explained the failures as a matter of poor technique or skill on the part of the operator, not a fault of the treatment as a whole. In the Foreword to a 1935 manual on light therapy for masseuses, Dr Percy Hall (Anderson, 1935, p.v) intimated that the therapy’s tremendous popularity was in danger of causing its own downfall:
Probably no new therapeutic method in the history of modern medicine has achieved such widespread use in so short a time as has light treatment. Its apparent simplicity led thousands of doctors, masseuses and others to avail themselves of it in the treatment of various disorders. Hospitals up and down the country opened Light Departments, and clinics for its use sprang up like mushrooms. The trouble was that very few persons had a sufficient knowledge of the subject to enable them to get the desired results. A great many unpleasant and unfortunate consequences occurred which, too often, were blamed on the method rather than the lack of skill and experience of the administrator. It was an almost exact repetition of what happened after the discovery of Roentgen was first made public.
Drawing a comparison to the sober lessons learned from the early days of experimenting with X-rays, Hall made indirect reference not simply to inconsistent or poor results but to reports of severe burns, electrocution, and even death when ultraviolet radiation was misused on and by the public. This only led to further dependence upon medical authorities to regulate exposures, to produce more research, more trials and more data (Edwards, 2007; Apple, 1996).
Summary
The acute skills required in working with light were essential to another ‘invisible’ presence in this history of light therapy, and that is the third, unseen operator in these images: namely the photographer, another technician of light (Maynard, 1997, p.224; Sheehan, 2011). Even professionals struggled to take legible photographs of light therapy in process; the flaring rays of light overexposed the film. Both phototherapy and documentary photographs of it needed to skilfully control light rays that blind and burn. Light therapy’s acceptance and validation were therefore dependent upon individuals highly skilled in controlling and harnessing light. By focussing on those who had a flair for working with this intense, volatile light, for producing visible results, and for disseminating the therapy’s value, we gain ‘snapshots’ (Zuromskis, 2009) of their agency and, above all, the risks that were at stake.
Acknowledgements
The author would like to extend her thanks to the Wellcome Trust for its generous support of her grant (#WT098912MA), and to Julia Pearey for her kind invitation to contribute to the journal.
References
- Anderson E. The Essentials of Light Treatment for the use of masseuses. Baillière, Tindall and Cox; London: 1935. [Google Scholar]
- Anonymous The Light Treatment. Nursing Record & Hospital World. 1900 Jul 7;:4. [Google Scholar]
- Anonymous Artificial Sunlight Treatment. The Times. 1925 Mar 19;:11. [Google Scholar]
- Apple R. Vitamania: Vitamins in American Culture. Rutgers University Press; New Brunswick: 1996. [Google Scholar]
- Beaumont W. Fundamental Principles of Ray Therapy: An Elementary Textbook for Nurses, Students, and Practitioners. H. K. Lewis & Co. Ltd.; London: 1931. [Google Scholar]
- Cawadias AP. Ultra-Violet Irradiation: Technique of Application. The British Journal of Physical Medicine. 1937;11(12):225–9. [Google Scholar]
- Edwards M. Control and the Therapeutic Trial: Rhetoric and Experimentation in Britain, 1918-48. Rodopi; Amsterdam and New York: 2007. [PubMed] [Google Scholar]
- Howell JD. Technology in the Hospital: Transforming Patient Care in the Early Twentieth Century. The Johns Hopkins University Press; Baltimore and London: 1996. [PubMed] [Google Scholar]
- Jamieson AK. An Intolerable Affliction: A History of Lupus Vulgaris in late Nineteenth- and early Twentieth-Century Britain. PhD thesis; University of Leeds: 2010. [Google Scholar]
- Malcolm M. An Address on the Treatment of Lupus Vulgaris During the Last 25 Years. Lancet. 1904 Oct 22;:1129–32. [Google Scholar]
- Maynard P. The Engine of Visualization: Thinking through Photography. Cornell University Press; Ithaca and London: 1997. [Google Scholar]
- Murray Levick G. Saving the Babies. Sunlight. 1930;2(1):29–33. [Google Scholar]
- Russell EH, WK . Ultra-Violet Radiation and Actinotherapy. E. & S. Livingstone; Edinburgh: 1925. [Google Scholar]
- Sandelowski M. Devices & Desires: Gender, Technology, and American Nursing. The University of North Carolina Press; Chapel Hill and London: 2000. [Google Scholar]
- Sheehan T. Doctored: The Medicine of Photography in Nineteenth-Century America. The Pennsylvania State University Press; University Park: 2011. [Google Scholar]
- Treloar Archives. Hampshire Archives and Local Studies. Hampshire Records Office; Winchester: [Google Scholar]
- Vaughan-Cowell M. Artificial Sunlight: Its Use and Application. The H. Edgar Smithers Publishing Company; London: 1928. [Google Scholar]
- Treloar W. The Cure of Tuberculous Children. The Graphic. 1918 Dec 21;:739. [Google Scholar]
- Woloshyn T. The Kiss of Light: Nursing and Light Therapy in 20th-C. Britain. Exhibition guide; The Florence Nightingale Museum, London: 2015. [Google Scholar]
- Zuromskis C. On snapshort photography: Rethinking photographic power in public and private spheres. In: Long JJ, Noble A, Welch E, editors. Photography: Theoretical Snapshots. Routledge; London and New York: 2009. pp. 49–62. [Google Scholar]