Abstract
Aims
To evaluate whether an alcohol harm reduction intervention was associated with reduced interpersonal violence or engagement in sex work among female sex workers (FSWs) in Mombasa, Kenya.
Design
Randomized controlled trial.
Setting
HIV prevention drop-in centers in Mombasa, Kenya.
Participants
818 women 18 or older in Mombasa who visited HIV prevention drop-in centers, were moderate-risk drinkers and engaged in transactional sex in past six months (410 and 408 in intervention and control arms, respectively).
Intervention
6 session alcohol harm reduction intervention.
Comparator
6 session non-alcohol related nutrition intervention.
Measurements
In-person interviews were conducted at enrollment, immediately post-intervention and 6-months post-intervention. General linear mixed models examined associations between intervention assignment and recent violence (physical violence, verbal abuse, and being robbed in the past 30 days) from paying and non-paying sex partners and engagement in sex work in the past 30 days.
Findings
The alcohol intervention was associated with statistically significant decreases in physical violence from paying partners at 6 months post-intervention and verbal abuse from paying partners immediately post-intervention and 6-months post-intervention. Those assigned to the alcohol intervention had significantly reduced odds of engaging in sex work immediately post-intervention and 6-months post-intervention.
Conclusions
The alcohol intervention was associated with reductions in some forms of violence and with reductions in engagement in sex work among FSWs in Mombasa, Kenya.
Keywords: Alcohol harm reduction, Violence, Sex work, HIV
1. INTRODUCTION
Alcohol use is prevalent among female sex workers (FSWs) worldwide (Chersich et al., 2007; Li et al., 2010; Scorgie et al., 2012). FSWs drink alcohol for a variety of reasons, including to self-medicate as a result of past trauma and to facilitate participation in commercial sex (Khantzian, 1997). FSWs often report being encouraged or coerced to drink alcohol by clients and pimps (Markosyan et al., 2007; Su et al., 2014). Binge drinking is also prevalent among FSWs across global settings (Li et al., 2010). A study of FSWs in South Africa found that 26% report binge drinking weekly and 18% report binge drinking daily (Richter et al., 2013). Forty-five percent of FSWs surveyed in Kenya report non-binge drinking and 33% report binge drinking monthly (Chersich et al., 2007).
Binge drinking has been consistently associated with HIV risk among FSWs (World Health Organization, 2011; Wechsberg et at., 2006). Among FSWs in Kenya, binge drinkers were more likely to report having unprotected sex and having a sexually transmitted infection (STI) than non-binge drinkers (Chersich et al., 2007). In addition, greater alcohol use has been associated with greater number of sex partners among female STI clinic patients (Carey et al., 2015).
FSWs are at high risk of multiple forms of interpersonal violence worldwide (Beattie et al., 2010; Decker et al., 2012; Karandikar and Prospero, 2010; Reed et al., 2010; Simic and Rhodes, 2009; Swain et al., 2011). According to the World Health Organization (WHO), interpersonal violence includes violence between intimate partners as well as violence from family members, acquaintances or strangers (Dahlberg and Krug, 2002). Interpersonal violence can take many forms including child or elder abuse, intimate partner violence, stranger violence and workplace violence (Dahlberg and Krug, 2002). Among FSWs in Kenya, 77% reported lifetime physical or sexual violence (Tegang et al., 2010). Among FSWs in Nigeria, 36% reported physical violence and 32% reported psychological abuse in the past six months (Fawole and Dagunduro, 2014). Physical and emotional violence perpetrated by non-commercial sex partners was reported by 20% and 25% of Canadian FSWs, respectively (Muldoon et al., 2015). Alcohol use has been consistently associated with violence against FSWs (Li et al., 2010; Scorgie et al., 2012; Wechsberg et al., 2005, 2006) . Alcohol use may increase vulnerability to violence through impaired judgment and reasoning and increased risk taking (George and Stoner, 2000). Among FSWs in Uganda, those who reported binge drinking had significantly increased odds of having experienced physical violence, verbal abuse, and not being paid as agreed to by a client (Schwitters et al., 2015).
Due to the high prevalence of binge drinking among FSWs (Li et al., 2010) and the associations among binge drinking, violence, and HIV risk (Chersich et al., 2014; Wechsberg et al., 2006), alcohol reduction interventions with FSWs have the potential to influence non-alcohol related health outcomes. The primary objectives of the current analysis are to investigate whether, compared to an equal-attention control condition, an alcohol harm reduction intervention was associated with reduced interpersonal violence (e.g., physical violence, verbal abuse, being robbed or not paid as agreed to by a client), engagement in sex work, or number of sex partners among a cohort of FSWs in Mombasa, Kenya. Previous analyses indicated that the alcohol harm reduction intervention was associated with reduced drinking frequency and binge drinking immediately post-intervention and 6 months post-intervention (L'Engle et al., 2014). The intervention was also associated with significantly reduced forced sex by paying sex partners immediately post-intervention and 6 months post-intervention (L'Engle et al., 2014).
The current analysis expands this previous work to examine whether the alcohol harm reduction intervention was also associated with reductions in three other forms of interpersonal violence (physical violence, verbal abuse, and being robbed or not paid as agreed to by a client as well) as well as engagement in sex work and number of sexual partners. While being robbed or not paid as agreed to by a client is not commonly included within the definition of interpersonal violence, it is included here as an attempt to measure economic violence or coercion specifically in the context of sex work. Examining whether an intervention exclusively targeting alcohol use influences violence and HIV risk can illuminate potential pathways and intervention strategies to effectively address binge drinking, violence and HIV risk behaviors among FSWs.
2. MATERIALS AND METHODS
2.1 Sample
Baseline data were collected between March and September, 2011 as part of a randomized controlled alcohol harm reduction intervention study with FSWs in Mombasa, Kenya (L'Engle et al., 2014). Follow up data were collected between October, 2011 and October, 2012. The primary objective of the parent study was to investigate whether the intervention was associated with reduced alcohol use and binge drinking, STIs, or HIV seroconversion among a cohort of FSWs in Mombasa, Kenya. The secondary objectives of the original study were to investigate whether the intervention was associated with condom use or forced sex. The study was conducted by FHI360 and the International Center for Reproductive Health, with funding from the United States Agency for International Development. Study participants were recruited from three USAID-funded AIDS, Population, Health and Integrated Assistance (APHIA) II drop-in centers in Mombasa. The drop-in centers serve approximately 15,000 FSWs in Mombasa through health education and services and condom distribution.
Women were eligible for study enrollment if they: were 18 years of age or older; had visited one of the HIV drop-in centers; planned to live in Mombasa for at least 12 months; reported transactional sex (i.e., self-report of exchange of oral, anal, or vaginal sex for money or gifts) in the past six months; and were moderate-risk drinkers (i.e., scored between 7 and 19 on the Alcohol Use Disorders Identification Test [AUDIT]). AUDIT scores 20 or greater indicate possible alcohol dependence (Babor et al., 2001). Women who scored 20 or greater were ineligible and referred to an alcohol treatment program. The study intervention was not designed to treat individuals with alcohol dependence who generally require greater clinical management than provided through brief interventions (Babor and Higgins-Biddle, 2001).
FSWs provided verbal informed consent for screening prior to AUDIT administration. Eligible FSWs provided written informed consent prior to enrollment. The study protocol for the parent study was approved by ethical research committees at FHI 360 and Kenyatta National Hospital. The study protocol for the current study was submitted to the Institutional Review Board at the University of North Carolina at Chapel Hill who determined it did not constitute human subjects research as it consisted exclusively of secondary analysis of de-identified data.
A total of 818 FSWs were enrolled and followed up with immediately post-intervention and 6 months post-intervention. At enrollment, FSWs were randomly assigned to a six-session intervention (n=410) or a six session control arm (n=408). Information about randomization procedures, sample size determination, data confidentiality and linking data over time were previously reported (L'Engle et al., 2014). Briefly, participants were individually randomized to the alcohol intervention or control condition in a 1:1 ratio, separately for each drop-in center. Random assignment was made after volunteers were screened for eligibility, provided consent, and completed baseline data collection. The parent trial was registered with ClinicalTrials.gov, NCT01756469.
2.2 Intervention
The intervention condition received the WHO's Brief Intervention (BI) for Hazardous and Harmful Drinking, adapted for the context of alcohol use and sex work by staff from Support for Addiction Prevention and Treatment in Africa (SAPTA), a Kenyan substance use prevention and treatment organization (Babor and Higgins-Biddle, 2001). The BI was developed for non-treatment seeking, non-dependent hazardous or harmful drinkers (Nilsen, 2010). The BI is intended as secondary prevention for alcohol abuse and is informed by Stages of Change theory (L'Engle et al., 2014; Nilsen, 2010). The executive director of SAPTA trained nurse-counselors to implement the intervention and provided clinical supervision. Intervention participants met for six monthly individual sessions with a trained nurse-counselor. During the first session, nurse-counselors reviewed participants’ AUDIT screening results and discussed health effects associated with their level of alcohol use. Subsequent sessions included: assessment of motivation and readiness to change, development of goals for low-risk drinking and a habit-breaking plan, implementation of plan to reduce drinking, and discussions of reasons to drink less, management of high-risk situations, coping strategies for boredom and strategies for achieving goals. As this was a harm reduction intervention, messaging focused on reducing drinking frequency and binge drinking rather than abstinence. The equal-attention control condition met for six monthly individual sessions with a nurse-counselor and received non-alcohol related nutrition information. Neither the intervention nor the control condition included content on interpersonal violence or HIV risk.
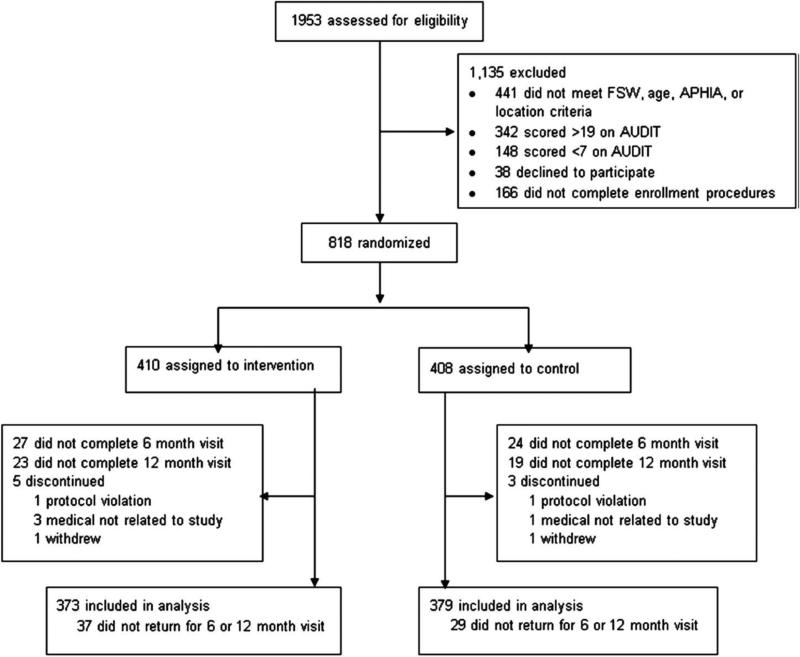
Of the 818 enrolled participants, 752 (92%) participated in at least one follow-up data collection visit (see Figure 1). Nearly three-quarters (72%) completed five counseling sessions. Follow-up and participation rates were comparable between groups. Three strategies were employed to ensure high levels of adherence and competence of intervention delivery. First, nurse-counselors who delivered the intervention were well trained in delivery of the intervention. Second, nurse-counselors received monthly monitoring and supervision by an alcohol intervention expert throughout the six months of intervention delivery. Third, the intervention team closely followed WHO guidelines for implementation of the BI.
Figure 1.
Trial Profile. From L'Engle et al., 2014
Characteristics of those lost to follow up and those retained in the study at 6 months post-intervention were compared using baseline data. There were no statistically significant differences in sociodemographics, alcohol use, violence, or sex work outcomes between these lost to follow-up and those retained at 6 months-post intervention.
2.3 Design
Data collection occurred at baseline, immediately post-intervention and 6 months post-intervention. Trained research assistants not involved in intervention delivery conducted in-person interviews in Swahili at drop-in centers. Interviews included questions on sociodemographics, HIV risk behaviors, sex work and violence, the AUDIT questionnaire and lab-confirmed HIV testing. Sociodemographic questions were asked only at study enrollment. Questions about HIV risk behaviors, sex work, violence, and alcohol were asked at three time points: enrollment, immediately post-intervention and 6 months post-intervention. All individuals received HIV testing at baseline. The protocol for HIV testing at follow-up visits is described later in this paper.
2.4 Assessment
2.4.1 Alcohol use
Participants were administered the AUDIT questionnaire. The AUDIT is a WHO-validated 10-item, 40-point assessment to identify harmful (AUDIT score 7-15) and hazardous (AUDIT score 16-19) alcohol users, and possible alcohol dependence (AUDIT score>19) (Babor et al., 2001). Participants were also asked the frequency with which they drank alcohol and the frequency with which they binge drank (defined as 3 or more drinks in one occasion) in the last 30 days.
2.4.2 Sociodemographics
Sociodemographic variables included age, education, religion, marital status, having a non-paying sex partner, number of living children, number of people supported by respondent, where respondents’ usually meet paying clients, years of sex work, and enrollment site. See Table 1 for details of these variables.
Table 1.
Characteristics of sample at baseline
| Characteristic | Total n (%) n=818 | Control n (%) n=408 | Intervention n (%) n=410 | p-value |
|---|---|---|---|---|
| Age (years) | 0.9406 | |||
| 18-24 | 316 (38.6) | 154 (37.8) | 162 (39.5) | |
| 25-29 | 255 (31.2) | 131 (32.1) | 124 (30.2) | |
| 30-34 | 130 (15.9) | 65 (15.9) | 65 (15.9) | |
| 35-54 | 117(14.3) | 58 (14.2) | 59 (14.4) | |
| Highest level of education | 0.8828 | |||
| Primary school or less | 449 (54.9) | 225 (55.2) | 224 (54.6) | |
| Secondary school or more | 369 (45.1) | 183 (44.9) | 186 (45.4) | |
| Religion | 0.3392 | |||
| Christian | 592 (72.4) | 297 (72.8) | 295 (72.0) | |
| Muslim | 224 (27.4) | 109 (26.7) | 115 (28.1) | |
| None | 2 (0.2) | 2 (0.5) | 0 | |
| Marital statusa | 0.9258 | |||
| Never married | 377 (46.6) | 191 (47.3) | 186 (45.9) | |
| Currently married | 28 (3.5) | 14 (3.5) | 14 (3.5) | |
| Divorced/separated/widowed | 404 (49.9) | 199 (49.3) | 205 (50.6) | |
| Currently has non-paying partner | 0.3082 | |||
| Yes | 620 (75.8) | 303 (74.3) | 317 (77.3) | |
| No | 198 (24.2) | 105 (25.7) | 93 (22.7) | |
| Number of living children | 0.9729 | |||
| No children | 156 (19.1) | 78 (19.1) | 78 (19.0) | |
| ≥1 child | 662 (80.9) | 330 (80.1) | 332 (81.0) | |
| Currently supporting othersa | 0.7400 | |||
| Yes | 730 (89.6) | 364 (89.2) | 366 (89.9) | |
| No | 85 (10.4) | 44 (10.8) | 41 (10.1) | |
| HIV Status | 0.9027 | |||
| Negative | 653 (79.8) | 325 (79.7) | 328 (80.0) | |
| Positive | 165 (20.2) | 83 (20.3) | 82 (20.0) | |
| Where usually meet paying clientsa | 0.6217 | |||
| Bar/nightclub | 658 (80.5) | 325 (79.9) | 333 (81.2) | |
| Street/home/hotel/beach | 159 (19.5) | 82 (20.2) | 77 (18.8) | |
| Drop-in Center | 0.9902 | |||
| Kisauni | 306 (37.4) | 152 (37.3) | 154 (37.6) | |
| Chaani | 285 (34.8) | 143 (35.0) | 142 (34.6) | |
| Likoni | 227 (27.8) | 113 (27.7) | 114 (27.8) | |
| Alcohol use | ||||
| Mean AUDIT Score (SD, Range) | 13.6 (3.6, 7-19) | 13.4 (3.6, 7-19) | 13.7 (3.6, 7-19) | 0.1928 |
| AUDIT Category | 0.0323 | |||
| Hazardous drinking (AUDIT 7-15) | 528 (64.6) | 278 (68.1) | 250 (61.0) | |
| Harmful drinking (AUDIT 16-19) | 290 (35.5) | 130 (31.9) | 160 (39.0) | |
| Substance use last 6 months (excluding alcohol) | 0.4316 | |||
| Yes | 282 (34.5) | 146 (35.8) | 136 (33.2) | |
| No | 536 (65.5) | 262 (64.2) | 274 (66.8) | |
| Used in past 30 days: | ||||
| Khat | 247 (30.2) | 124 (30.4) | 123 (30.0) | 0.9028 |
| Bhang | 48 (5.9) | 29 (7.1) | 19 (4.6) | 0.1323 |
| Cocaine | 1 (0.1) | 1 (0.3) | 0 | 0.3158 |
| Heroin | 3 (0.4) | 1 (0.3) | 2 (0.5) | 0.5659 |
| Sleeping pills | 2 (0.2) | 2 (0.5) | 0 | 0.1558 |
| Other substances | 12 (1.5) | 5 (1.2) | 7 (1.7) | 0.5666 |
Missing data by variable: Marital status 9; Supporting others 3; Where usually meet paying clients 1.
2.4.3 Interpersonal violence
Physical violence was assessed by asking: How many times in the last 30 days have you been beaten or physically abused (Piere et al., 2007). The measure for physical violence was previously used in the 2007 Kenya Behavioral Monitoring Survey (Piere et al., 2007). Verbal abuse was assessed by asking: How many times in the last 30 days have you been threatened or verbally abused? (Piere et al., 2007). Robbery or non-payment was assessed by asking: How many times in the last 30 days have you been robbed or not paid as agreed to by a client? (Wechsberg et al., 2006). The measure for being robbed was previously used with substance using female sex workers in South Africa (Wechsberg et al., 2006). Physical violence was asked separately for violence by paying and non-paying sex partners. Questions about verbal abuse and being robbed were asked only for violence from paying sex partners. Frequency responses to each violence question were dichotomized into having experienced the particular form of violence or not in the last 30 days (See Table 2).
Table 2.
Interpersonal violence
| Baseline | Immediately post-intervention | 6 months post-intervention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (n=379) | Intervention (n=373) | Control (n=355) | Intervention (n=346) | Control (n=360) | Intervention (n=350) | |||||||
| Violence by paying partner past 30 daysa | n* | % (n) | n | % (n) | n | % (n) | n | % (n) | n | % (n) | n | % (n) |
| Physical violence | 378 | 25.4 (96) | 372 | 27.7 (103) | 354 | 4.5 (16) | 346 | 4.6 (16) | 360 | 9.7 (35) | 350 | 5.1 (18) |
| Verbal abuse | 379 | 50.4 (191) | 373 | 49.6 (185) | 354 | 30.2 (107) | 346 | 20.8 (72) | 360 | 21.7 (78) | 350 | 15.1 (53) |
| Robbed/Not paid | 379 | 51.7 (196) | 373 | 50.7 (189) | 354 | 23.5 (83) | 346 | 16.8 (58) | 359 | 16.4 (59) | 350 | 12.9 (45) |
| Violence by non-paying partner past 30 daysb | ||||||||||||
| Physical violence | 282 | 28.7 (81) | 291 | 32.0 (93) | 261 | 21.8 (57) | 237 | 16.9 (40) | 261 | 14.2 (37) | 233 | 9.4 (22) |
Among entire sample
Among those with non-paying partners
Number of participants contributing to analysis
2.4.4 Engagement in sex work and number of sex partners
Participants were asked how many paying sex partners they had in the last 30 days. Those who reported no paying sex partners in the past 30 days were coded as not having engaged in sex work in the past 30 days. Those who reported at least one paying sex partner in the past 30 days were coded as having engaged in sex work in the past 30 days (See Table 3). Respondents were also asked the total number of different sex partners (paying and non-paying) they had in the last seven days.
Table 3.
HIV sexual risk behaviors
| Baseline | Immediately post-intervention | 6 months post-intervention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Engagement in sex work past 30 days | Control (n=379) | Intervention (n=373) | Control (n=355) | Intervention (n=346) | Control (n=360) | Intervention (n=350) | ||||||
| n* | %(n) | n | %(n) | n | %(n) | n | %(n) | n | %(n) | n | %(n) | |
| No | 379 | 0.5 (2) | 373 | 1.3 (5) | 355 | 13.0 (46) | 346 | 25.4 (88) | 360 | 15.3 (55) | 350 | 23.4 (82) |
| Yes | 99.5 (377) | 98.7 (368) | 87.0 (309) | 74.6 (258) | 84.7 (305) | 76.6 (268) | ||||||
| Median (Range) | Median (Range) | Median (Range) | Median (Range) | Median (Range) | Median (Range) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median number of sex partners past 7 days | 376 | 2.00 (0-35) | 372 | 2.00 (0-21) | 355 | 1.00 (0-31) | 345 | 1.00 (0-21) | 360 | 1.00 (0-31) | 350 | 1.00 (0-30) |
Number contributing to analysis
2.4.5 HIV testing
At enrollment all participants were tested for HIV. HIV testing adhered to Kenya Ministry of Public Health and Sanitation guidelines, starting with an HIV rapid test. If the initial rapid test was positive, confirmation testing was conducted using a different rapid test and/or ELISA or Western Blot assay. Those who tested positive were not tested at future visits. Participants were provided the results of HIV testing, and individuals who tested positive were referred to HIV care.
2.5 Data Analysis
Univariate statistics were used to describe sociodemographic characteristics, sexual behaviors, violence, and alcohol use. Bivariate statistics, including Pearson chi-square tests for binary variables and t-tests for continuous variables, were used to assess comparability of intervention and control groups at baseline.
To analyze the relationship between intervention assignment as compared to control assignment and outcome variables (e.g., interpersonal violence, engagement in sex work, number of sex partners), treatment groups were compared over time using generalized linear mixed models (GLIMMIX) to account for the longitudinal nature of the data and correlations due to sampling via drop-in center. For binary outcome variables, logit link with binomial distribution was used. For total number of sex partners, Poisson distribution with log link was used. All analyses were conducted as intention to treat. Models controlled for sampling due to drop in center and contained a term for main outcome by treatment interaction. Treatment effects were estimated separately immediately post-intervention and 6 months post-intervention. All analyses were conducted using SAS Version 9.3.
3. RESULTS
3.1 Study sample
Descriptive statistics of the sample have been previously described (L'Engle et al., 2014). Briefly, the sample was relatively young with over two-thirds (69.8%) between 18 and 29 years old (see Table 1). More than half (54.9%) reported no formal education. Most (72.4%) were Christian and never married (46.6%) or divorced, separated or widowed (49.9%). The majority (75.8%) had at least one non-paying sex partner. Most were parents (80.9%) and reported supporting others (89.6%). Twenty percent of the sample was HIV positive at enrollment. Approximately two-thirds (64.6%) screened positive for hazardous drinking (i.e., AUDIT scores 7-15) while one-third (35.5%) screened positive for harmful drinking (i.e., AUDIT scores 16-19). Approximately one-third (34.5%) reported using a substance other than alcohol in the past 30 days, the overwhelming majority of which was khat. While there was no significant difference between groups in mean AUDIT scores at baseline, individuals randomly assigned to the control condition were significantly less likely to screen positive for harmful drinking compared to the intervention condition. No other significant differences were observed between groups at baseline.
3.2 Interpersonal violence
Violence by paying and non-paying partners was prevalent at baseline across groups (see Table 2). Approximately one-quarter (26.5%) reported recent physical violence and half (50.0%) reported recent verbal abuse from a paying sex partner. Almost one-third (30.4%) reported recent physical violence from a non-paying sex partner. No differences were observed in prevalence of recent interpersonal violence between groups at baseline.
3.3 Engagement in sex work
Virtually all participants in intervention and control groups (98.7% and 99.5%, respectively) reported sex work in the past 30 days at baseline. High prevalence of sex work was expected as engagement in transactional sex in the past six months was a criterion for study enrollment.
3.4 Number of sex partners
Across groups, at baseline, participants reported a median of 2 sex partners (paying and non-paying) in the past seven days.
3.5 Outcomes of intervention and control groups at follow up
3.5.1 Interpersonal violence
Both groups reported substantial decreases in all forms of interpersonal violence immediately post-intervention and 6 months post-intervention (see Table 2), including physical violence, verbal abuse and being robbed or not paid. However, compared to the control group, the intervention group reported significantly greater reductions in verbal abuse and having been robbed or not paid by paying sex partners immediately post-intervention (see Table 4).
Table 4.
Intervention effect on interpersonal violence
| Immediately post-intervention | 6 months post-intervention | |||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Violence by paying partner past 30 days | ||||
| Physical violence | 1.02 (0.48, 2.20) | 0.94 | 0.45 (0.23, 0.85) | 0.01 |
| Verbal abuse | 0.54 (0.36, 0.82) | 0.004 | 0.59 (0.38, 0.92) | 0.02 |
| Robbed/Not paid | 0.61 (0.40, 0.95) | 0.03 | 0.72 (0.44, 1.16) | 0.17 |
| Violence by non-paying partner past 30 days | ||||
| Physical violence | 0.64 (0.38, 1.08) | 0.09 | 0.57 (0.30, 1.06) | 0.08 |
All models adjusted for drop-in center; All models run individually with intervention condition as independent variable and violence as dependent variable.
Associations between the intervention and reduced verbal abuse by paying sex partners persisted at 6 months post-intervention. However, the association between intervention condition and having been robbed or not paid did not persist at 6 months post-intervention. At 6 months post-intervention, compared to the control condition, the intervention was associated with reduced physical violence from paying sex partners. The intervention was not associated with reduced physical violence from non-paying sex partners at either follow-up point.
3.5.2 Engagement in sex work
Both intervention and control groups reported substantial decreases in recent engagement in sex work immediately and 6 months post-intervention (see Table 3). However, compared to the control condition, the intervention was associated with significantly reduced odds of engaging in sex work immediately and 6 months post-intervention (see Table 5). Participants who were randomly assigned to the intervention condition had 0.43 (95% CI 0.28, 0.66) times the odds of engaging in sex work immediately post-intervention and 0.57 (95% CI 0.38, 0.87) times the odds of engaging in sex work at 6 months post-intervention compared to those assigned to the control condition.
Table 5.
Intervention effect on HIV sexual risk behaviors
| Immediately post-intervention | 6 months post-intervention | |||
|---|---|---|---|---|
| Risk behavior | OR (95% CI) | p-value | OR (95% CI) | p-value |
| Engagement in sex work (last 30 days) | 0.43 (0.28, 0.66) | 0.0001 | 0.57 (0.38, 0.87) | 0.009 |
| IRR (95% CI) | IRR (95% CI) | |||
|---|---|---|---|---|
| Total number of different sex partners (last 7 days) | 0.75 (0.65, 0.85) | <0.0001 | 0.91 (0.79, 1.05) | 0.18 |
All models adjusted for drop-in center; Models run individually with intervention condition as independent variable and risk behavior as dependent variable. IRR=Incidence rate ratio
3.5.3 Number of sex partners
Both intervention and control groups reported fewer sex partners in the past seven days immediately and 6 months post-intervention (see Table 3). However, compared to the control condition, the intervention was associated with having significantly fewer sex partners (paying and non-paying) in the past seven days immediately post-intervention; this effect did not persist at 6 months post-intervention.
4. DISCUSSION
This study found that an alcohol harm reduction intervention was associated with reductions in some forms of violence against FSWs in Mombasa, Kenya. As the intervention focused exclusively on alcohol harm reduction, these findings speak to the interconnectedness of alcohol use and violence against FSWs. The pathways through which the alcohol harm reduction intervention was associated with reduced violence remain unclear. The intervention reduced participants’ alcohol consumption and binge drinking (L'Engle et al., 2014). As alcohol consumption is associated with impaired judgment and increased risk-taking, reduced alcohol consumption may have decreased FSWs’ risk-taking, increased FSWs’ capacity to maintain their personal safety, and decreased vulnerability to multiple forms of violence. For example, by reducing binge drinking, FSWs’ may have selected ‘less risky’ sex partners (e.g., partners who were not intoxicated) or made decisions (e.g., where they had sex with paying sex partners) that reduced their risk of physical violence, verbal abuse, and being robbed or not paid. Alternately, violence reductions may have resulted from FSWs in the intervention group having fewer sex partners - another indirect effect of the intervention that could lead to reduced opportunities for violence. Further, reductions in violence may indirectly result from economic empowerment. It is possible that reduced likelihood of being robbed reduced FSWs’ economic vulnerability, increased economic empowerment, and influenced selection of sex partners away from violent sex partners and towards non-violent sex partners. Additional research is necessary to understand the mechanisms through which alcohol reduction was associated with reduced violence among FSWs –whether alcohol reduction led to reduced risk among FSWs who continued sex work or if alcohol reduction was associated with reduced violence through fewer sex partners or discontinuation of sex work.
Although the intervention was associated with reduced physical violence from paying partners, compared to the control group, the intervention was not associated with reduced physical violence from non-paying partners. Previous analyses found that the intervention was similarly associated with reduced sexual violence from paying, but not from non-paying partners (L'Engle et al., 2014). Such findings speak to potential differences in the role of alcohol and risk taking in relationships with paying and non-paying partners. Relationships with non-paying partners are often more complex and difficult to change, potentially limiting the effectiveness of alcohol harm reduction interventions to reduce violence in this context. Interventions to prevent physical violence and verbal abuse from non-paying sex partners may require additional intervention techniques. In addition, the relationship between violence from non-paying partners and risk behavior with paying partners warrants further investigation. A history of violence with non-paying partners may increase one's risk behavior with paying partners as well as overall alcohol use and binge drinking. More research is necessary to understand how to most effectively support FSWs and reduce their risk of multiple forms of violence.
The intervention was significantly associated with reduced verbal abuse from paying sex partners immediately and 6 months post-intervention. However, the association between the intervention and having been robbed or not paid immediately post-intervention did not persist at 6 months post-intervention. Such findings highlight the importance of disaggregating violence by type as different types of violence may have different causal and contributing factors. These findings also illustrate the difficulty of maintaining intervention-related behavior change over time. Additional longitudinal and qualitative research is needed to further understand how alcohol harm reduction influences multiple forms of violence against FSWs in the long-term. In addition, this intervention did not target alcohol use of FSWs’ partners nor FSWs’ drinking environments. Multilevel interventions and interventions that focus on the alcohol use of FSWs’ partners may be necessary for sustained reductions in some forms of violence against FSWs.
The alcohol harm reduction intervention was associated with reduced odds of sex work immediately post-intervention and 6 months post-intervention. The pathway between reduced alcohol consumption and discontinuation of sex work is likely complex. Qualitative data from the parent study indicated that intervention group participants reported increased financial savings from decreased spending on alcohol and increased likelihood of payment by clients (Velozza et al., In press). Alcohol harm reduction interventions may have significant effects beyond reduced alcohol consumption, including reduced economic vulnerability. Economic vulnerability is a common reason for sex work initiation (Nishigaya, 2002). Among Kenyan FSWs, half reported sex work as their only source of income and 90% had dependent children (Elmore-Meegan et al., 2004). Reduced alcohol consumption may serve as a first step towards greater economic stability and a catalyst for leaving sex work. However, engagement in sex work is often cyclical and characterized by patterns of exit and re-entry (Manopaiboon et al., 2003). FSWs that left sex work may have subsequently re-entered. More research is needed to understand barriers and facilitators of leaving sex work permanently and the role of alcohol reduction interventions in this process.
In recognition of the link between economic vulnerability and engagement in sex work, economic empowerment programs with FSWs have become more prevalent (Odek et al., 2009; Sherman et al., 2010). Given the relationship between alcohol use and financial stability, such programs should incorporate alcohol harm reduction into their programming. Jointly addressing economic empowerment and alcohol harm reduction may increase program effectiveness, sustainability of improvements in economic stability, and produce other positive health benefits.
Alcohol harm reduction programming should be integrated into HIV prevention programming with FSWs, regardless of HIV status. Interventions that combine individual-level alcohol harm reduction programming with structural-level intervention components should be further developed and evaluated particularly as multilevel interventions have demonstrated effectiveness at reducing alcohol consumption among FSWs (Morisky et al., 2010). Multilevel alcohol harm reduction interventions have the potential to increase effectiveness and sustainability of positive health outcomes. Interventions that combine alcohol harm reduction and violence risk reduction strategies for FSWs should be developed, implemented and evaluated, particularly in low- and middle-income settings.
While significantly smaller than reductions in the intervention group, the control group also reported reductions in violence and sex work (see Tables 2 and 3) as well as alcohol use and binge drinking (L'Engle et al., 2014). Many potential explanations exist for reductions in the control group. Reductions may have resulted from the control group receiving an equal-attention intervention. Nutrition information in the control intervention may have influenced control participants’ alcohol use leading to reductions in violence and sex work through pathways previously described. Given that FSWs often report low levels of social support, care and attention shown by nurse-counselors may have had beneficial health effects on FSWs, regardless of randomization assignment (Goldenberg et al., 2013; King et al., 2013). Reductions in the control group also may have resulted from the Hawthorne effect. Data collection, in which control participants were asked about alcohol use, sex work and violence, may have led to behavior change due to monitoring these aspects of their lives.
Alternately, given that randomization occurred at the individual level (and not the level of drop-in center), contamination across treatment arms may have occurred. If participants had social ties across groups, alcohol reduction information may have been shared, leading to reduced drinking among control group participants and reduced violence and sex work. Furthermore, one's drinking behavior is influenced by peers’ beliefs and behaviors. Control group participants may have reduced drinking as a result of reduced drinking by intervention group peers. Future research on socially-influenced behaviors such as alcohol consumption should be designed to minimize contamination.
This study has several limitations. All FSWs visited HIV drop-in centers. As such, participants may be more motivated to change their behavior or engage in less risk taking than FSWs who had not visited drop-in centers. FSWs were recruited in three sections of Mombasa and may not be representative of FSWs throughout urban Kenya. With the exception of HIV testing, all data were self-reported. Risk factors including alcohol use and engagement in sex work may have been underreported due to social desirability.
Findings demonstrate the potential for brief alcohol harm reduction interventions to positively influence the health and safety of FSWs. Implementation of brief alcohol harm reduction interventions in other geographic settings and with other FSW populations is warranted. This project revealed other areas for further study including examining in more depth potential pathways between alcohol reduction and reductions in violence and engagement in sex work and the development, implementation and evaluation of integrated alcohol harm reduction and economic empowerment interventions. Future studies should take into account challenges related to contamination encountered in the current study. Greater attention is needed to the role of alcohol use in the lives of FSW, the impact of brief alcohol harm reduction interventions and the intersections between alcohol use, violence and HIV risk. These types of studies are crucial for improving the lives of FSW and reducing the spread of HIV.
Supplementary Material
Highlights.
This study evaluated whether an alcohol harm reduction intervention was associated with reduced interpersonal violence or engagement in sex work among female sex workers in Mombasa, Kenya.
The alcohol harm reduction intervention was associated with statistically significant decreases in having been robbed or not paid as agreed to by a client immediately post-intervention, verbal abuse from paying partners immediately and 6 months post-intervention and physical violence from paying partners 6 months post-intervention.
Those assigned to the alcohol intervention had significantly lower odds of engaging in sex work immediately and 6 months post-intervention.
Findings demonstrate the potential for brief alcohol harm reduction interventions to positively influence the health and safety of female sex workers.
Acknowledgements
The authors are grateful to Samuel Field for statistical consultation and Audrey Pettifor for thoughtful feedback on early drafts of this manuscript.
Role of Funding Source:
This study was supported by the Public Health Evaluation (PHE) component of the President's Emergency Plan for AIDS Relief (PEPFAR), PHE #KE09.0235. Funding was provided through the US Agency for International Development (USAID), under the terms of AID-623-A-11-00007. The project was also supported by Award Number T32 MH019139 (Principal Investigator, Theodorus Sandfort, Ph.D.) from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors
AP developed the research question, designed and conducted the analyses and wrote the initial draft of the manuscript. KLL designed and directed the parent study and contributed to the development of the research question and manuscript writing. SLM contributed to the development of the research question, manuscript writing, and critical revision. CS contributed to statistical analyses and manuscript writing. SG and ISS contributed to manuscript writing and critical revision. PW and NK assisted with implementation and management of the intervention. WS provided supervision for nurse-counselors who implemented the intervention and assisted in the adaptation of the intervention modules. All authors contributed to the writing and have approved the final manuscript.
Conflict of Interest
None
Contributor Information
Angela M. Parcesepe, University of North Carolina at Chapel Hill, Department of Maternal and Child Health, Gillings School of Global Public Health, CB# 7445, Rosenau Hall, Chapel Hill, NC 27599.
Kelly L. L'Engle, FHI 360, 359 Blackwell St., Durham NC 27701 Population Health Sciences, School of Nursing and Health Professions University of San Francisco, 2130 Fulton Street, San Francisco CA 94117.
Sandra L. Martin, University of North Carolina at Chapel Hill, Department of Maternal and Child Health, Gillings School of Global Public Health, CB# 7445, Rosenau Hall, Chapel Hill, NC 27599
Sherri Green, University of North Carolina at Chapel Hill, Department of Maternal and Child Health, Gillings School of Global Public Health, CB# 7445, Rosenau Hall, Chapel Hill, NC.
William Sinkele, Support for Addiction Prevention and Treatment in Africa (SAPTA), PO Box 21761 Ngong Road, 00505 Nairobi, Kenya.
Chirayath Suchindran, University of North Carolina at Chapel Hill, Department of Biostatistics, Gillings School of Global Public Health, Rosenau Hall, Chapel Hill, NC.
Ilene S. Speizer, University of North Carolina at Chapel Hill, Department of Maternal and Child Health, Gillings School of Global Public Health, CB# 7445, Rosenau Hall, Chapel Hill, NC
Peter Mwarogo, FHI 360, The Chancery 2nd and 3rd Floor Valley Road, PO Box 38835-00623, Nairobi, Kenya.
Nzioki Kingola, International Center for Reproductive Health, PO Box 91109, Mombasa, Kenya.
REFERENCES
- Babor TH, Higgins-Biddle JC. A Manual For Use In Primary Care. World Health Organzation; Geneva: 2001. Brief Intervention For Hazardous And Harmful Drinking. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders J, Monteiro M. Guidelines For Use In Primary Care. World Health Organization; Geneva: 2001. The AUDIT: The Alcohol Use Disorders Identification Test. [Google Scholar]
- Beattie TS, Bhattacharjee P, Ramesh BM, Gurnani V, Anthony J, Isac S, Mohan HL, Ramakrishnan A, Wheeler T, Bradley J, Blanchard JF, Moses S. Violence against female sex workers in Karnataka state, south India: impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010;10 doi: 10.1186/1471-2458-10-476. doi:10.1186/1471-2458-10-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Senn TE, Walsh JL, Scott-Sheldon LA, Carey MP. Alcohol use predicts number of sexual partners for female but not male STI clinic patients. AIDS Behav. 2015 doi: 10.1007/s10461-015-1177-9. doi:10.1007/s10461-015-1177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich MF, Bosire W, King'ola N, Temmerman M, Luchters S. Effects of hazardous and harmful alcohol use on HIV incidence and sexual behaviour: a cohort study of Kenyan female sex workers. Global Health. 2014;10 doi: 10.1186/1744-8603-10-22. doi:10.1186/1744-8603-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich MF, Luchters SM, Malonza IM, Mwarogo P, King'ola N, Temmerman M. Heavy episodic drinking among Kenyan female sex workers is associated with unsafe sex, sexual violence and sexually transmitted infections. Int. J. STD AIDS. 2007;18:764–769. doi: 10.1258/095646207782212342. doi:10.1258/095646207782212342. [DOI] [PubMed] [Google Scholar]
- Dahlberg LL, Krug EG. Violence - a global public health problem. In: Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World Report on Violence and Health. World Health Organziation; Geneva: 2002. pp. 1–21. [Google Scholar]
- Decker MR, Wirtz AL, Baral SD, Peryshkina A, Mogilnyi V, Weber RA, Stachowiak J, Go V, Beyrer C. Injection drug use, sexual risk, violence and STI/HIV among Moscow female sex workers. Sex. Transm. Infect. 2012;88:278–283. doi: 10.1136/sextrans-2011-050171. doi:10.1136/sextrans-2011-050171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmore-Meegan M, Conroy RM, Agala CB. Sex workers in Kenya, numbers of clients and associated risks: an exploratory survey. Reprod. Health Matters. 2004;12:50–57. doi: 10.1016/s0968-8080(04)23125-1. [DOI] [PubMed] [Google Scholar]
- Fawole OI, Dagunduro AT. Prevalence and correlates of violence against female sex workers in Abuja, Nigeria. Afr. Health Sci. 2014;14:299–313. doi: 10.4314/ahs.v14i2.4. doi:10.4314/ahs.v14i2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George WH, Stoner SA. Understanding acute alcohol effects on sexual behavior. Annu. Rev. Sex. Res. 2000;11:92–124. [PubMed] [Google Scholar]
- Goldenberg SM, Engstrom D, Rolon ML, Silverman JG, Strathdee SA. Sex workers perspectives on strategies to reduce sexual exploitation and HIV risk: a qualitative study in Tijuana, Mexico. PLoS One. 2013;8:e72982. doi: 10.1371/journal.pone.0072982. doi:10.1371/journal.pone.0072982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karandikar S, Prospero M. From client to pimp: male violence against female sex workers. J. Interpers. Violence. 2010;25:257–273. doi: 10.1177/0886260509334393. doi:10.1177/0886260509334393. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv. Rev. Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. doi:10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- King EJ, Maman S, Bowling JM, Moracco KE, Dudina V. The influence of stigma and discrimination on female sex workers’ access to HIV services in St. Petersburg, Russia. AIDS Behav. 2013;17:2597–2603. doi: 10.1007/s10461-013-0447-7. doi:10.1007/s10461-013-0447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- L'Engle KL, Mwarogo P, Kingola N, Sinkele W, Weiner DH. A randomized controlled trial of a brief intervention to reduce alcohol use among female sex workers in Mombasa, Kenya. J. Acquir. Immune Defic. Syndr. 2014;67:446–453. doi: 10.1097/QAI.0000000000000335. doi:10.1097/qai.0000000000000335. [DOI] [PubMed] [Google Scholar]
- Li Q, Li X, Stanton B. Alcohol use among female sex workers and male clients: an integrative review of global literature. Alcohol Alcohol. 2010;45:188–199. doi: 10.1093/alcalc/agp095. doi:10.1093/alcalc/agp095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manopaiboon C, Bunnell RE, Kilmarx PH, Chaikummao S, Limpakarnjanarat K, Supawitkul S, St. Louis ME, Mastro TD. Leaving sex work: barriers, facilitating factors and consequences for female sex workers in northern Thailand. AIDS Care. 2003;15:39–52. doi: 10.1080/012021000039743. doi:10.1080/012021000039743. [DOI] [PubMed] [Google Scholar]
- Markosyan KM, Babikian T, DiClemente RJ, Hirsch JS, Grigoryan S, del Rio C. Correlates of HIV risk and preventive behaviors in Armenian female sex workers. AIDS Behav. 2007;11:325–334. doi: 10.1007/s10461-006-9147-x. doi:10.1007/s10461-006-9147-x. [DOI] [PubMed] [Google Scholar]
- Morisky DE, Chiao C, Ksobiech K, Malow RM. Reducing alcohol use, sex risk behaviors, and sexually transmitted infections among Filipina female bar workers: effects of an ecological intervention. J. Prev. Interv. Community. 2010;38:104–117. doi: 10.1080/10852351003640674. doi:10.1080/10852351003640674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muldoon KA, Deering KN, Feng CX, Shoveller JA, Shannon K. Sexual relationship power and intimate partner violence among sex workers with non-commercial intimate partners in a Canadian setting. AIDS Care. 2015;27:512–519. doi: 10.1080/09540121.2014.978732. doi:10.1080/09540121.2014.978732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsen P. Brief alcohol intervention--where to from here? Challenges remain for research and practice. Addiction. 2010;105:954–959. doi: 10.1111/j.1360-0443.2009.02779.x. doi:10.1111/j.1360-0443.2009.02779.x. [DOI] [PubMed] [Google Scholar]
- Nishigaya K. Female garment factory workers in Cambodia: migration, sex work and HIV/AIDS. Womens Health. 2002;35:27–42. doi: 10.1300/J013v35n04_03. doi:10.1300/J013v35n04_03. [DOI] [PubMed] [Google Scholar]
- Odek WO, Busza J, Morris CN, Cleland J, Ngugi EN, Ferguson AG. Effects of micro-enterprise services on HIV risk behaviour among female sex workers in Kenya's urban slums. AIDS Behav. 2009;13:449–461. doi: 10.1007/s10461-008-9485-y. doi:10.1007/s10461-008-9485-y. [DOI] [PubMed] [Google Scholar]
- Piere S, Emukule G, Kitungulu B. Behavioral Monitoring Survey. Family Health International; Nairobi, Kenya: 2007. [Google Scholar]
- Reed E, Gupta J, Biradavolu M, Devireddy V, Blankenship KM. The context of economic insecurity and its relation to violence and risk factors for HIV among female sex workers in Andhra Pradesh, India. Public Health Rep. 2010;125:81–89. doi: 10.1177/00333549101250S412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter ML, Chersich M, Temmerman M, Luchters S. Characteristics, sexual behaviour and risk factors of female, male and transgender sex workers in South Africa. S. Afr. Med. J. 2013;103:246–251. doi: 10.7196/samj.6170. doi:10.7196/samj.6170. [DOI] [PubMed] [Google Scholar]
- Schwitters A, Swaminathan M, Serwadda D, Muyonga M, Shiraishi RW, Benech I, Mital S, Bosa R, Lubwama G, Hladik W. Prevalence of rape and client-initiated gender-based violence among female sex workers: Kampala, Uganda, 2012. AIDS Behav. 2015;19:S68–76. doi: 10.1007/s10461-014-0957-y. doi:10.1007/s10461-014-0957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scorgie F, Chersich MF, Ntaganira I, Gerbase A, Lule F, Lo YR. Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-saharan Africa: a systematic review. AIDS Behav. 2012;16:920–933. doi: 10.1007/s10461-011-9985-z. doi:10.1007/s10461-011-9985-z. [DOI] [PubMed] [Google Scholar]
- Sherman SG, Srikrishnan AK, Rivett KA, Liu SH, Solomon S, Celentano DD. Acceptability of a microenterprise intervention among female sex workers in Chennai, India. AIDS Behav. 2010;14:649–657. doi: 10.1007/s10461-010-9686-z. doi:10.1007/s10461-010-9686-z. [DOI] [PubMed] [Google Scholar]
- Simic M, Rhodes T. Violence, dignity and HIV vulnerability: street sex work in Serbia. Sociol. Health Illn. 2009;31:1–16. doi: 10.1111/j.1467-9566.2008.01112.x. doi:10.1111/j.1467-9566.2008.01112.x. [DOI] [PubMed] [Google Scholar]
- Su S, Li X, Lin D, Zhang C, Qiao S, Zhou Y. Social context factors, refusal self-efficacy, and alcohol use among female sex workers in China. Psychol. Health Med. 2014:1–7. doi: 10.1080/13548506.2014.966727. doi:10.1080/13548506.2014.966727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swain SN, Saggurti N, Battala M, Verma RK, Jain AK. Experience of violence and adverse reproductive health outcomes, HIV risks among mobile female sex workers in India. BMC Public Health. 2011;11:357. doi: 10.1186/1471-2458-11-357. doi:10.1186/1471-2458-11-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tegang SP, Abdallah S, Emukule G, Luchters S, Kingola N, Baras M, Mucheke S, Mwarogo P. Concurrent sexual and substance-use risk behaviours among female sex workers in Kenya's Coast Province: findings from a behavioural monitoring survey. Sahara J. 2010;7:10–16. doi: 10.1080/17290376.2010.9724972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velozza J, L'Engle K, Mwarogo P, Chokwe J, Magaria L, Sinkele W, Kingola N. Stages and processes of change utilized by female sex workers participating in an alcohol-reduction intervention in Mombasa, Kenya. Subst. Use Misuse. doi: 10.3109/10826084.2015.1037397. In press. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Lam WK. Violence against substance-abusing South African sex workers: intersection with culture and HIV risk. AIDS Care. 2005;17(Suppl 1):S55–64. doi: 10.1080/09540120500120419. doi:10.1080/09540120500120419. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Lam WK, Parry CD, Morojele NK. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS Behav. 2006;10:131–137. doi: 10.1007/s10461-005-9036-8. doi:10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Preventing HIV Among Sex Workers In Sub-Saharan Africa: A Literature Review. World Health Organization; Geneva: 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.