Abstract
Stress is known to negatively affect health and is a potentially serious barrier to diabetes-related health outcomes. This paper synthesizes what is known about stress and glycemic control among people with type 1 and type 2 diabetes across the lifespan. Chronic stress—especially in relation to living with diabetes—was most strongly associated with A1c, particularly among subgroups that face disproportionate stress, such as minority groups or adolescents/young adults. Mechanisms of the stress-A1c association include physiological, psychological, behavioral, and environmental links. Understanding the dimensions of stress as they relate to health in diabetes can be of significant clinical importance, and interventions targeting mechanisms that either exacerbate or buffer stress have reported modest improvements in A1c.
Keywords: Stress, Glycemic control, Type 1 diabetes, Type 2 diabetes
Introduction
Type 1 diabetes (T1D) and type 2 diabetes (T2D) are among the most common chronic illnesses [1] and have demanding treatment regimens [2] that aim to maintain glycemic control as close to normal as possible to reduce the risk for microvascular and macrovascular complications [3–6]. The American Diabetes Association (ADA) recommendations for glycemic control are A1c < 7.0 % for adults with T1D and T2D and A1c < 7.5 % for youth with T1D [2]. Yet for the majority of people with diabetes, glycemic goals are not met. Between 2007 and 2010, around half of adults with T2D reported A1c < 7.0 % [7], and rates are even lower among people with T1D: 16 % of youth ages 13–17, 25 % of young adults ages 18–25, and around 50 % of older adults in the Type 1 Diabetes Exchange in the United States met glycemic targets [8].
To address the persistent challenge of achieving and maintaining in-range glycemic control among people with T1D and T2D across the lifespan, a more comprehensive understanding of the correlates and contributors to glycemic control is needed. The numerous factors influencing glycemic control include degree of residual beta cell function [9], use of intensive insulin management [3], use of advanced diabetes management technologies [10, 11], and adherence to treatment recommendations [12]. Another factor that may relate to glycemic control is stress, which has been broadly linked with risk for poor health outcomes, including diabetes onset and complications [13, 14]. Indeed, the ADA highlights the central role of stress (including discrete stressful events, psychosocial stress, and family stress) in achieving glycemic control targets, especially in the care of youth with T1D [2].
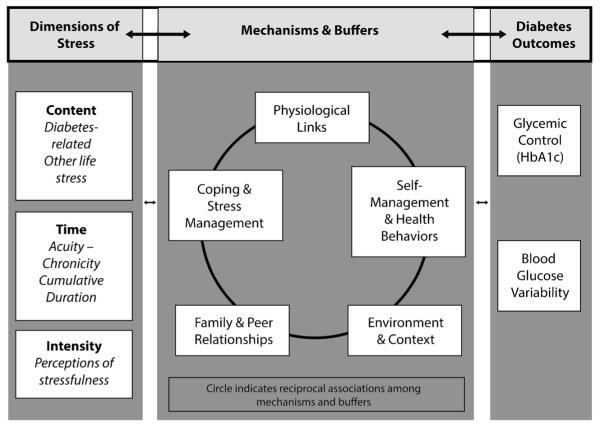
Identifying stress-related mechanisms that are potentially modifiable through interventions should be prioritized to guide clinical interventions. To meet this need, the current review aims to (1) describe acute and chronic stress both specifically related to diabetes (e.g., diabetes distress) and with origins external to diabetes that relate to the experience of living with diabetes (e.g., income), (2) summarize the literature on the associations between these types of stress and A1c, (3) identify potentially modifiable mechanisms and buffers of these links, and (4) discuss implications for interventions, with a focus on strategies to enhance resilience to stress. Figure 1 illustrates a conceptual model of associations linking different dimensions of stress with glycemic outcomes through multi-level, interrelated mechanisms and buffers. Each of the concepts in the figure is described in this paper.
Fig. 1.
Associations of stress and glycemic control
Dimensions and Types of Stress
This review highlights two primary dimensions of stress, as outlined in Fig. 1: (1) the content being either directly related to diabetes (e.g., feeling overwhelmed by management demands) or other stressors in the context of diabetes (e.g., the impact of losing one’s job on diabetes) and (2) the timing (i.e., acuity or chronicity) of stress. Perceived intensity varies within each of these dimensions. In line with recent conceptualizations of stress [15] and diabetes-related distress [16••] as distinct constructs from depression, depressive symptoms are not included in the scope of this paper’s review of stress and glycemic outcomes.
Diabetes-related Stressors
Acute Diabetes Stressors
Individuals living with diabetes regularly experience acute stressors related to the pathophysiology or treatment of the condition. Stressful situations can include discrete blood glucose-related events (e.g., episode of severe hypoglycemia, diabetic ketoacidosis), treatment changes (e.g., starting on insulin), and the introduction of a new diabetes management device/technology (e.g., insulin pump, continuous glucose monitoring [CGM]). Acute stress can increase endogenous glucose production and impair glucose utilization; however, data from brief stressful events lasting only a few minutes and occurring a few hours before sampling suggest that this short-term process likely does not affect A1c [17]. Brief stressors may not be of significant duration or intensity to impact A1c, which reflects average glucose over several weeks. Furthermore, stressful situation-related high or low blood glucose excursions by definition skew the average glucose level and contribute to higher or lower A1c, respectively, making it difficult to disentangle the unique role of stress in the glycemic outcome.
Chronic Diabetes Stressors
Diabetes-related stress or distress (DRS) refers to the emotional stress associated with the ongoing worries, burdens, and concerns that individuals living with diabetes experience as they manage their condition [16••]. DRS is characterized by feeling frustrated, overwhelmed, and discouraged by the demands of diabetes. For adults with T2D, the most common areas of DRS involve the treatment regimen and the emotional burden of diabetes [18], while people with T1D describe feelings of powerlessness, hypoglycemia, self-management, and eating as areas of greatest stress [19]. The prevalence of elevated DRS ranges from 20 to 40 % in people with T1D and T2D—these rates tend to be stable and show little change over time without intervention [20, 21, 22•]. This speaks to the chronic and persistent nature of DRS. Several individual characteristics have also been associated with DRS: younger adults, women, Caucasians, people with less education, and those with complications are more likely to experience high DRS [19, 23].
Support is accumulating for modest but consistent cross-sectional associations between elevated DRS and poorer glycemic control in adults with T1D and T2D [24–27, 28•], which may be stronger for specific subgroups. For example, in a community sample of people with T2D, high levels of DRS were associated with A1c only for younger adults; no associations were found for older adults [29]. Several studies have noted stronger associations between A1c and stress related to daily regimen or management of diabetes compared to other areas [19]. For example, elevated regimen-related distress was associated with significantly higher A1c (approximately 1.0 % more) among rural African-American women with T2D [30]. A recent systematic review concluded smallto-moderate associations of DRS with glycemic control among adolescents with T1D [31]; however, mixed findings were reported that may in part be due to differences in DRS measurement in this age range [22•].
When the relation between DRS and A1c has been examined longitudinally, two primary patterns have emerged: (1) baseline DRS does not predict change in A1c over time or vice versa; however, (2) decreases in DRS have been associated with decreases in A1c in both observational and intervention studies [25, 32•, 33]. For example, following a diabetes education intervention, the average decrease in DRS was associated with a 0.25 % reduction in A1c [33]. Another study with T1D adults noted a 0.5 SD reduction in regimen distress was associated with a 0.6 % change in A1c [28•]. Thus, rather than concluding that DRS impacts glycemic control, current findings suggest that DRS and A1c fluctuate in tandem over time, possibly through indirect mechanisms such as adherence to diabetes care behaviors and others (outlined below). Longitudinal research is needed to disentangle the possible ways in which trajectories of stress and A1c influence one another reciprocally over time.
General Stress
In addition to the stress related to living with T1D or T2D, individuals living with diabetes also experience other life stress, including acute stressors such as a car accident or chronic stressors such as poverty. Although not directly related to diabetes, the sequelae of these stressors may play a role in diabetes management or outcomes.
Acute General Stressors
Acute stressors are the most common form of stress. This type of stress is generally short term and includes responses to demands of the recent past and anticipated demands of the near future. Acute stress can be measured by assessing within a specified time period (1) whether an individual has experienced one or more stressors or (2) perceived degree to which they are experiencing stress.
Most research on acute stress has examined self-reported recent stressful life events. In an early study with youth with T1D, more family stressors (e.g., financial, illness, school, interpersonal) in the previous year were associated with higher A1c [34]. More recent longitudinal studies found that any major life event in the past 3 months (e.g., death/illness in relative, suspension from school, divorce) was associated with accelerated increases in A1c [35, 36]. Among adults with T1D, experiencing more recent stressful life events was associated with worsening glycemic control [37, 38]. For youth with T2D, we identified only one study, which reported that recent stressful life events were not associated with A1c [39•], and no studies were identified that assessed acute stress and A1c in adults with T2D.
Chronic General Stressors
Chronic stress occurs when an individual sees no way out of a difficult situation with unrelenting pressures lasting extended periods of time. Although contemporary research has largely emphasized chronic DRS as described above, some evidence shows a direct association between chronic general stress and glycemic outcomes. Early research demonstrated strong correlations between chronic, stressful life events, and A1c in youth and adults with T1D [37, 40, 41], and a more recent study reported stress to be significantly associated with A1c > 8.5 % among Malaysian women with T2D [42]. Neighborhood stress (defined as crowded housing and female-headed households with dependent children and on public assistance) has also been associated with poorer glycemic control in adults with T2D [43]. Perceived discrimination, including subtle and overt forms of negative differential treatment, has been used to define chronic stress in the diabetes literature, possibly to capture stress-related experiences prevalent among ethnic/racial minorities who are at risk for disparities in diabetes outcomes. Perceived racial discrimination in healthcare and in other settings has been associated with elevated A1c values in adults with T2D [44, 45, 46•].
Associations Between Diabetes-related and General Stressors
Few studies have examined the relationship between DRS and general stressors (acute or chronic) to understand how they interact with one another in a cumulative manner in relation to glycemic control. Among adults with T2D, more acute negative life events and more chronic stressors have both been linked with subsequent elevated DRS [23]. In the same study, acute stress interacted with A1c, where the association between higher A1c and the subsequent increase in DRS was stronger for those also experiencing other acute stressors. More work is needed to better understand the likely reciprocal and cumulative associations among diabetes-related and other life stressors and glycemic control.
Mechanisms and Buffers of the Stress-A1c Association
A considerable body of research has examined mechanisms of the associations among stress and glycemic control. The pathways by which stress amplifies or buffers the links between stress and A1c occur on multiple levels: individual physiological, psychological, and health behavior processes; family and peer relationships; and other environmental and contextual factors, which are interrelated with one another in addition to their associations with stress and glycemic outcomes (Fig. 1). This aligns with social-ecological models of health behaviors and outcomes. For example, the Diabetes Resilience Model [47] describes the associations of risk factors (including stress) and protective processes in predicting glycemic control and other outcomes across individual, interpersonal, and environmental systems. It is important to consider not only factors that amplify the stress-A1c link but also those that buffer this link, because bolstering individuals’ skills and supportive resources through interventions has the potential to strengthen one’s ability to respond adaptively to stress and promote optimal glycemic outcomes. The following paragraphs review recent literature on the potential mechanisms and buffers of the stress-A1c link. Given individual variations in stress content, intensity, and timing, the operational definition of stress differs for each study within each mechanism. The mechanisms are likely to have dynamic relations with one another, which may also impact stress management and glycemic outcomes. Thus, the potential role of each pathway depends on the type of stressor and interactions with other simultaneously occurring processes.
Physiological Links
The allostatic load model of chronic stress may help explain the negative effects of chronic stress on physical and mental health [48]. “Allostatic load” refers to the cumulative cost of repeated neuroendocrine responses resulting from chronic stress, which can cause dysregulation of multiple interrelated physiological systems and lead to a deterioration in health [49]. The hypothalamic-pituitary adrenal (HPA) axis is sensitive to social context and emotional input, and perceptions of uncontrollable stressors are hypothesized to activate this axis [50]; however, no data are currently available that confirm or deny whether this is true for people with diabetes.
To test the physiological links of the effect of stress on glycemic control, several studies have implemented experimental paradigms to induce acute stress and assess the effect on blood glucose and other physiological responses. For example, one study used a driver-training protocol to elicit mental stress among adults with T1D or T2D (all insulin-treated) [51]. Participants exhibited increased salivary cortisol and subjective stress perception during the driving test days, but there was no significant difference in blood glucose levels on driving days vs. control days. Similarly, in adults with T1D, riding rollercoasters (to induce acute stress) increased heart rate, blood pressure, and salivary cortisol, but there were no differences in blood glucose (measured with CGM) [52]. On the other hand, in an experimental paradigm including a social stress test in adults with T1D, Wiesli and colleagues [53] reported significantly delayed decreases in glucose concentrations post-meal, indicating extended elevations in glucose when stressed (effect was not found when fasting). Finally, in a small sample of children with T1D playing arousing video games, the change in blood glucose from videogaming to resting was significantly different than the change from reading to resting [54]. These findings indicate that acute stress may not have a direct, physiological effect on glucose levels, but there may be aspects of stressors (e.g., controllability, social context) that do play a role in glucose regulation. It may also be that the types of acute stressors used in these studies may be less salient for people with diabetes, while diabetes-related acute stressors (e.g., hypoglycemic events) may have a stronger association with glucose. Indeed, hypoglycemia is associated with a stress response from the autonomic nervous system [55], and therefore, people with T1D may have stress responses on a relatively frequent basis when glucose levels drop. Studies using simulated impending hypoglycemia or induced hypoglycemic events (e.g., with insulin clamps) may be a promising avenue to evaluate associations of acute diabetes-related stress (physiological and perceptions) and glucose levels.
Research with individuals without diabetes can help shed light on the associations of stress with glycemic control, which may have implications for people with diabetes. Foundational research in this area reported higher A1c among adult male workers without diabetes exposed to workplace stress (i.e., noise, rotating shifts, overwork) compared to peers not exposed to those chronic job stressors [56]. In a more recent study of Chinese workers without diabetes or impaired glucose tolerance, Xu and colleagues [57] reported a relationship between A1c and job stress in women, but not men. Chronic financial strain over a 10-year period has also been associated with high A1c levels in African-American women without diabetes [58]. This research with people without diabetes or impaired glucose tolerance clearly documents a relation between stress and A1c, which may have implications for understanding similar associations in people with diabetes.
Individual Psychological and Behavioral Links
At an individual level, a number of mechanisms have been evaluated linking stress and glycemic outcomes. Psychological experiences related to (but distinct from) stress, such as depressive symptoms, have been identified as important, potentially modifiable mechanisms of glycemic outcomes. For example, among adolescents with T1D, the association between DRS and A1c was exacerbated among those with elevated depressive symptoms [59]. When DRS, depressive symptoms, and major depression were analyzed simultaneously among adults with T2D, all the variables predicted glycemic control, yet DRS showed the strongest associations [60]. Together, these findings suggest that depressive symptoms and DRS may amplify one another in relation to their links with glycemic control.
On the other hand, there are also psychological processes related to coping and stress management that may buffer the stress-A1c association. For example, Gonzalez and colleagues [60] reported that higher perceived control over diabetes management weakened the link between DRS and A1c. Similarly, in youth with T1D, coping skills including benefit-finding have been linked with less distress and better glycemic control [61]. Finally, Yi and colleagues [62] demonstrated that among adults with T1D and T2D with rising stress, those with low levels of several positive psychological processes (i.e., selfefficacy, self-esteem, self-mastery, and optimism) showed a parallel rise in A1c; those with higher levels of these adaptive skills did not, indicating a “stress-buffering” effect [62].
In addition to psychological processes, health behaviors and self-management skills have also been evaluated as mechanisms that either amplify or buffer the link between stress and glycemic outcomes; stress may impede individuals’ ability to engage in self-care behaviors. For example, among early adolescents with T1D, less frequent engagement in self-care behaviors mediated the association between more stressful life events and poorer glycemic control, that is, stressful experiences appeared to interfere with self-care and adversely impact glycemic control [36]. In contrast, in a study of adults with T2D, changes in management (diet, exercise, and medication adherence) failed to explain linkages between DRS and A1c [32•]. Among both adolescents and adults with T1D and T2D, there is evidence that higher stress levels may be related to poorer sleep quality [63]. While the causal pathway to A1c is unclear, poor sleep quality has been linked with suboptimal diabetes management and glycemic outcomes in people with diabetes [64, 65], suggesting that this may be a behavioral mechanism worthy of further research in relation to the stress-A1c association.
Family and Peer Links
Interpersonal relationships have also been evaluated in terms of either amplifying or reducing the impact of stress on A1c and vice versa. The majority of this research has emphasized family relationships for youth with T1D. For example, stress in the family system (e.g., family conflict) has been related to inadequate levels of parental monitoring for youths’ self-management behaviors, and each has been linked with poorer glycemic control [66]. A systematic review identified diabetes-related conflict and stress within the family as risks for poorer glycemic control among youth with T1D [31]. There is some evidence that peer stress may have implications for glycemic control, although this appears to have a lesser impact than family-related stress: adolescents with T1D endorsed stress related to feeling different from their peers, ongoing treatment management, and overprotective parents [67], but links with A1c were not reported. Berlin and colleagues [68] classified youth with T1D by the types of stress they indicated most frequently and found that those who endorsed higher family-related stress had poorer glycemic control than those with higher interpersonal and peer stress or low overall stress. Thus, while more research is needed on peer-related stress, family stress related to diabetes appears to be the interpersonal issue that is most significant for T1D outcomes in youth. More remains to be learned about these influences in adults or people with T2D.
In contrast, Jaser and Grey [69] reported that child-centered parenting practices and positive reinforcement for self-management are protective in terms of reducing stress and improving A1c for youth with T1D, consistent with the Diabetes Resilience Model [47]. Parental support has also been shown to buffer the impact of stressful life events on A1c in this population [34]. There is some similar evidence of the benefits of family support in adults with T1D—and to a lesser degree T2D [70, 71], although the associations with glycemic control need further study. Less consistent findings regarding the buffering role of peer support are available.
Context and Environmental links
As reviewed earlier, cross-sectional studies indicate trends toward poorer glycemic control among people with and without diabetes who are exposed to more stress in the places they live or work. However, research evaluating mechanisms linking these stressors with glycemic outcomes are not yet available. In order to develop interventions to reduce diabetes disparities and support people with the greatest risk factors, more research to identify and target modifiable mechanisms linking environmental stressors with glycemic outcomes are needed.
Clinical Implications
Several intervention studies (primarily among adults with T2D) have demonstrated improvements in A1c by targeting mechanisms of the stress-A1c link and helping people respond to stress in more adaptive ways. For example, stress management training that provided education about the health consequences of stress and taught cognitive-behavioral skills to recognize and reduce physiological stress levels using relaxation techniques reduced A1c 0.5 % among adults with T2D [72]. Another study showed that a stress management program focused on teaching diaphragmatic breathing and progressive muscle relaxation demonstrated moderate reductions (Cohen’s d = 0.73) in A1c [73]. An empowerment-based group intervention to promote self-management among African-American women with T2D, which targeted DRS through emotional support, goal-setting, and problem-solving, resulted in an A1c difference of 0.98 % between the control and intervention periods [74]. Interventions targeting self-management education and support have also demonstrated that reductions in DRS were linked with improvements in A1c among adults with T2D [33, 75], for example, Zagarins and colleagues reported an average reduction of 10 points on a measure of distress was associated with a 0.25 % reduction in A1c [33].
Behavioral interventions for youth with T1D have also targeted psychological, self-management behavior, and family mechanisms of the stress-A1c association. For example, a coping skills training intervention for adolescents resulted in an average of 1.6 % improvement in A1c (from 9.1 to 7.5 % mean A1c) over 1 year through teaching effective strategies for diabetes management in stressful social situations (e.g., conflict resolution, social problem solving) [76]. More recently, an internet-based version of the intervention reduced perceived stress in adolescents with T1D, though effects on A1c were not evident [77]. With its emphasis on building supportive family involvement in diabetes management to strength youths’ self-management without increasing family conflict (all hypothesized links of the stress-A1c association), the family teamwork psychoeducational and behavioral intervention reported a prevention of deterioration in glycemic control among 10–14 year olds with T1D; the post-intervention change in glycemic control between the intervention and comparison group was 0.5 % [78]. Building on this approach, Katz et al. [79] report on adding a para-professional “care ambassador” to deliver a behavioral family intervention and also provide outreach- and assistance-scheduling appointments; the results included preventing deterioration in glycemic control among those youth with A1c ≥ 8.0 % receiving the care ambassador plus psychoeducational intervention. These related approaches may have targeted stress and glycemic outcomes by promoting adaptive family processes and reducing stress related to navigating a complex healthcare system.
Most available interventions targeting stress and glycemic control for people with diabetes are high-dose, multicomponent interventions that primarily target DRS. While this is largely justified by literature demonstrating the benefits of intensive behavioral interventions [12, 80] and stronger intervention impact on glycemic control by adapting generic behavioral intervention approaches to focus on diabetes-specific constructs [81], this combination may not match the stressors or needs of all people with diabetes [82]. For example, it is possible that individuals experiencing acute or chronic general stressors might benefit more from behavioral interventions to target their unique sources of stress than a diabetes-specific intervention. Stressors related to limited financial resources or insurance coverage or exposure to serious psychosocial adversity (e.g., abuse, psychiatric disorders) may also be more appropriately treated by providers with expertise and resources in those specific domains (e.g., social work, case management, clinical psychology). Among youth with T1D, pilot data suggest that a more generalized approach to stress management focusing on general (not disease-specific) stress management skills (e.g., relaxation, goal-setting, cognitive restructuring) may have the potential to also impact clinical outcomes such as self-management behaviors and glycemic control [83]. More research is needed to determine whether general stress interventions are most effective prior to, in combination with, or in place of diabetes-specific interventions to target general and diabetes-related stress, for whom, and in what circumstances.
Among interventions focusing on DRS, data from stress interventions targeting outcomes other than glycemic control suggest that adaptations may be needed to match personal characteristics and experiences with distress [84]. For example, the dose and format of intervention delivery may need to vary by the intensity of an individual’s stress and available resources. Some behavioral strategies, such as breathing and relaxation training, may be delivered in a single, brief session in a clinic setting, while multicomponent intervention packages require more time and resources to deliver outside of the medical visit. Individuals and families experiencing more general stress may have more barriers to attending frequent intervention sessions, making telehealth approaches a potentially useful avenue to pursue [85]. More work is needed to determine the most effective and least burdensome approach to intervention delivery for different types of stress.
Conclusion
Taken together, this review of the literature examining direct and mediated links between stress and glycemic outcomes in people with T1D and T2D across the lifespan suggests that higher stress specifically related to the experience of living with diabetes is associated at least moderately with poorer glycemic control. Given the overlapping role of extreme blood glucose values in acute DRS and in glycemic outcomes, causality remains uncertain. However, behavioral, psychological, and family processes that facilitate management of DRS have been linked with improvements in A1c, suggesting the potential of interventions that strengthen positive processes to reduce stress and promote optimal glycemic control. The strongest evidence exists in youth with T1D and, to a lesser degree,adults with T1D and T2D. While more research on stress among people with T2D is needed, providers should consider a variety of diabetes-specific and other stressors that their patients may be experiencing and be aware of the potential impact on glycemic control.
The reciprocal impact of general stress on diabetes outcomes seems plausible, but the evidence for mechanisms linking general stressors with glycemic outcomes is sparse. Moreover, interrelated links between general and diabetes-related stressors complicate measurement and do not reflect the cumulative nature of chronic stress and its association with diabetes management over time. Findings may underestimate the role of stress due to measurement limitations: assessing perceived stress or stressful events during a specified time period (e.g., 12 months) does not differentiate between general and diabetes-related events and does not account for acute stressors that may contribute to the onset of chronic stress. For example, divorce might heighten short-term stress and trigger the onset of chronic financial strain or persistent familial disruption that interferes with optimal diabetes management and outcomes. Thus, adapting diabetes-focused stress management interventions to address not only DRS but also other sources of stress that relate even indirectly to diabetes management may hold promise for improving glycemic outcomes. More research is needed to determine the impact of intensive stress-focused interventions on glycemic outcomes across populations.
This review focused on associations of stress and glycemic control as measured by A1c. While A1c is considered a key outcome that represents overall diabetes-related health status, it does capture glycemic variability (i.e., percent of time with blood glucose values within the target range) or represent hyper- or hypoglycemic events, all of which may relate to stress. Although there is little available literature on how stress influences or is influenced by fluctuations or variability in blood glucose, advances in CGM will allow for fine-grained examinations of in-the-moment associations between acute stressors and glucose variability and of links between various types of stress and trajectories of glucose values. However, new technologies may also introduce new stressors, such as the burden of wearing devices, information overload, intrusive alarms, and difficulties navigating the interpersonal choices around how, when, and how much to share live glucose data with others (e.g., family, diabetes care providers). As diabetes management technologies continue to advance, these issues must be taken into consideration in clinical practice and study design.
Finally, the use of A1c as the only outcome is also limited by recent questions about whether A1c is an accurate representation of average blood glucose for all people, due to biological differences in people or different ethnicities, known as the “glycation gap” [86]. Given the growing and troubling evidence of persistent disparities in diabetes-related outcomes between various subsets of the population with diabetes (e.g., race/ethnicity, income/socioeconomic status, health literacy) [87, 88], the need for accurate measurement and appropriate intervention around both stress and glycemic control for all people with diabetes remains a top priority.
Acknowledgments
Marisa E. Hilliard, Ashley M. Butler, and Barbara J. Anderson report grants from the National Institutes of Health (1K12 DK097696).
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest Marisa E. Hilliard, Joyce P. Yi-Frazier, Danielle Hessler, Ashley M. Butler, Barbara J. Anderson, and Sarah Jaser declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
• • Of major importance
- 1.Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA. 2014;312:1218–26. doi: 10.1001/jama.2014.11494. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association Standards of medical care in diabetes—2016. Diabetes Care. 2016;39(1):S1–S112. [Google Scholar]
- 3.Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 4.Diabetes Control and Complications Trial Study Group The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995;44:968–83. [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study (UKPDS) Group Intensive bloodglucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 6.Shichiri M, Kishikawa H, Ohkubo Y, et al. Long-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patients. Diabetes Care. 2000;23(Suppl2):B21–9. [PubMed] [Google Scholar]
- 7.Stark Casagrande S, Fradkin JE, et al. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care. 2013;36:2271–9. doi: 10.2337/dc12-2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller KM, Foster NC, Beck RW, et al. Current state of type 1 diabetes treatment in the US: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38:971–8. doi: 10.2337/dc15-0078. [DOI] [PubMed] [Google Scholar]
- 9.Sherr J, Tamborlane WV, Xing D, Tsalikian E, et al. Achievement of target A1C levels with negligible hypoglycemia and low glucose variability in youth with short-term type 1 diabetes and residual β-cell function. Diabetes Care. 2012;35:817–20. doi: 10.2337/dc11-2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeSalvo D, Buckingham B. Continuous glucose monitoring: current use and future directions. Curr Diab Rep. 2013;13:657–62. doi: 10.1007/s11892-013-0398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson SR, Cooper MN, Jones TW, et al. Long-term outcome of insulin pump therapy in children with type 1 diabetes assessed in a large population-based case-control study. Diabetologia. 2013;56:2392–400. doi: 10.1007/s00125-013-3007-9. [DOI] [PubMed] [Google Scholar]
- 12.Hood KK, Peterson C, Rohan J, et al. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics. 2009;124(6):e1171–9. doi: 10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- 13.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–9. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 14.Pouwer F, Kupper N, Adriaanse MC. Does emotional stress cause type 2 diabetes mellitus? A review from the European Depression in Diabetes (EDID) Research Consortium. Discov Med. 2010;9:112–8. [PubMed] [Google Scholar]
- 15.Pizzagalli DA. Depression, stress, and anhedonia: toward a synthesis and integrated model. Annu Rev Clin Psychol. 2014;10:393–423. doi: 10.1146/annurev-clinpsy-050212-185606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16 ••.Fisher L, Gonzalez JS, Polonsky WH. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabetic Med. 2014;31:764–72. doi: 10.1111/dme.12428. This paper provides one of the first and clearest definitions of the construct of “diabetes distress” (or diabetes-related stress), which is important to differentiate from general stress especially when evaluating associations with glycemic control and in clinical practice.
- 17.Bonora E, Tuomilehto J. The pros and cons of diagnosing diabetes with A1c. Diabetes Care. 2011;34:S184–190. doi: 10.2337/dc11-s216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fisher L, Glasgow RE, Mullan JT, et al. Development of a brief diabetes distress screening instrument. Ann Fam Med. 2008;6:246–52. doi: 10.1370/afm.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher L, Polonsky WH, Hessler DM, et al. Understanding the sources of diabetes distress in adults with type 1 diabetes. J Diabetes Complications. 2015;29:572–7. doi: 10.1016/j.jdiacomp.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fisher L, Hessler DM, Polonsky WH, et al. Prevalence of depression in type 1 diabetes and the problem of over-diagnosis. Diabetic Med. 2015 doi: 10.1111/dme.12973. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.Sturt J, Dennick K, Due-Christensen M, et al. The detection and management of diabetes distress in people with type 1 diabetes. Curr Diab Rep. 2015;15:1–14. doi: 10.1007/s11892-015-0660-z. [DOI] [PubMed] [Google Scholar]
- 22 •.Hagger V, Hendrieckx C, Sturt J, et al. Diabetes distress among adolescents with type 1 diabetes: a systematic review. Curr Diab Rep. 2016;16:1–14. doi: 10.1007/s11892-015-0694-2. This recent review goes into detail about the experiences of diabetes distress in youth with T1D.
- 23.Fisher L, Mullan JT, Skaff MM, et al. Predicting diabetes distress in patients with type 2 diabetes: a longitudinal study. Diabetic Med. 2009;26:622–7. doi: 10.1111/j.1464-5491.2009.02730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinger K, Jacobson AM. Psychosocial and quality of life correlates of glycemic control during intensive treatment of type 1 diabetes. Patient Educ Couns. 2001;42:123–31. doi: 10.1016/s0738-3991(00)00098-7. [DOI] [PubMed] [Google Scholar]
- 25.Fisher L, Mullan J, Arean P, et al. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care. 2010;33:28–8. doi: 10.2337/dc09-1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aikens JE. Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care. 2012;35:2472–8. doi: 10.2337/dc12-0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reddy J, Wilhelm K, Campbell L. Putting PAID to diabetes-related distress: the potential utility of the problem areas in diabetes (PAID) scale in patients with diabetes. Psychosomatics. 2013;54:44–51. doi: 10.1016/j.psym.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 28 •.Strandberg RB, Graue M, Wentzel-Larsen T, et al. Relationships of diabetes-specific emotional distress, depression, anxiety, and overall well-being with HbA1c in adult persons with type 1 diabetes. J of Psychosom Res. 2014;77:174–9. doi: 10.1016/j.jpsychores.2014.06.015. This paper compares diabetes-related and general stress constructs in relation to glycemic control, which helps to clarify the relative importance of diabetes-related experiences for research and clinical care.
- 29.Hessler DM, Fisher L, Mullan JT, et al. Patient age: a neglected factor when considering disease management in adults with type 2 diabetes. Patient Educ Couns. 2011;85:154–9. doi: 10.1016/j.pec.2010.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cummings DM, Lutes L, Littlewood K, et al. Regimen-related distress, medication adherence, and glycemic control in rural African American women with type 2 diabetes mellitus. Ann Pharmacother. 2014;48:970–7. doi: 10.1177/1060028014536532. [DOI] [PubMed] [Google Scholar]
- 31.Tsiouli E, Alexopoulos EC, Stefanaki C, et al. Effects of diabetes-related family stress on glycemic control in young patients with type 1 diabetes systematic review. Can Fam Physician. 2013;59:143–9. [PMC free article] [PubMed] [Google Scholar]
- 32 •.Hessler D, Fisher L, Glasgow RE, et al. Reductions in regimen distress are associated with improved management and glycemic control over time. Diabetes Care. 2014;37:617–24. doi: 10.2337/dc13-0762. This paper is one of several that demonstrates that diabetes-related stress is a potentially modifiable construct and that changes have the potential to impact self-management and diabetes outcomes in a meaningful way.
- 33.Zagarins SE, Allen NAG, Welch G. Improvement in glycemic control following a diabetes education intervention is associated with change in diabetes distress but not change in depressive symptoms. J Behav Med. 2012;35:299–304. doi: 10.1007/s10865-011-9359-z. [DOI] [PubMed] [Google Scholar]
- 34.Viner R, McGrath M, Trudinger P. Family stress and metabolic control in diabetes. Arch Dis Child. 1996;74(5):418–21. doi: 10.1136/adc.74.5.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lawes T, Franklin V, Farmer G. HbA1c tracking and biopsychosocial determinants of glycaemic control in children and adolescents with type 1 diabetes: retrospective cohort study and multilevel analysis. Pediatr Diab. 2014;15(5):372–83. doi: 10.1111/pedi.12100. [DOI] [PubMed] [Google Scholar]
- 36.Helgeson VS, Escobar O, Siminerio L, et al. Relation of stressful life events to metabolic control among adolescents with diabetes: 5-year longitudinal study. Health Psychol. 2010;29(2):153–9. doi: 10.1037/a0018163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lloyd CE, Dyer PH, Lancashire RJ, et al. Association between stress and glycemic control in adults with type 1 (insulin-dependent) diabetes. Diabetes Care. 1999;22(8):1278–83. doi: 10.2337/diacare.22.8.1278. [DOI] [PubMed] [Google Scholar]
- 38.Stenstrom U, Wikby A, Hornqvist JO, et al. Recent life events, gender differences, and the control of insulin-dependent diabetes mellitus. A 2-year follow-up study. Gen Hosp Psychiatr. 1995;17(6):433–9. doi: 10.1016/0163-8343(95)00059-3. [DOI] [PubMed] [Google Scholar]
- 39 •.Walders-Abramson N, Venditti EM, Ievers-Landis CE, et al. Relationships among stressful life events and physiological markers, treatment adherence, and psychosocial functioning among youth with type 2 diabetes. J Peds. 2014;165(3):504–508. e501. doi: 10.1016/j.jpeds.2014.05.020. This study from the TODAY Trial is one of the few examinations of stress in the vulnerable population of youth with type 2 diabetes.
- 40.Goldston DB, Kovacs M, Obrosky DS. A longitudinal study of life events and metabolic control among youths with insulin-dependent diabetes mellitus. Health Psychol. 1995;14:409–14. doi: 10.1037//0278-6133.14.5.409. [DOI] [PubMed] [Google Scholar]
- 41.Griffith LS, Field BJ, Lustman PJ. Life stress and social support in diabetes: association with glycemic control. Int J of Psychiat in Med. 1990;20:365–72. doi: 10.2190/APH4-YMBG-NVRL-VLWD. [DOI] [PubMed] [Google Scholar]
- 42.Kaur G, Tee GH, Ariaratnam S, et al. Depression, anxiety and stress symptoms among diabetics in Malaysia: a cross sectional study in an urban primary care setting. BMC Fam Pract. 2013;14:1. doi: 10.1186/1471-2296-14-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laraia BA, Karter AJ, Warton EM, et al. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE) Soc Sci Med. 2012;74:1082–90. doi: 10.1016/j.socscimed.2011.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Piette JD, Bibbins-Domingo K, Schillinger D. Health care discrimination, processes of care, and diabetes patients’ health status. Patient Educ Couns. 2006;60:41–8. doi: 10.1016/j.pec.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 45.Wagner JA, Tennen H, Finan PH, et al. Self-reported racial discrimination and endothelial reactivity to acute stress in women. Stress Health. 2013;29:214–21. doi: 10.1002/smi.2449. [DOI] [PubMed] [Google Scholar]
- 46 •.Wagner JA, Tennen H, Feinn R, et al. Racial discrimination and metabolic control in women with type 2 diabetes. Ethn Dis. 2015;23:421–7. This paper addresses the important role of stress from perceived racial discrimination and its associations with health outcomes, highlighting the need for more research in this understudied area.
- 47.Hilliard ME, Harris MA, Weissberg-Benchell J. Diabetes resilience: a model of risk and protection in type 1 diabetes. Curr Diab Rep. 2012;12:739–48. doi: 10.1007/s11892-012-0314-3. [DOI] [PubMed] [Google Scholar]
- 48.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav R. 2010;35:2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 49.Glei DA, Goldman N, Chuang YL, et al. Do chronic stressors lead to physiological dysregulation? Testing the theory of allostatic load. Psychosom Med. 2007;69:769–76. doi: 10.1097/PSY.0b013e318157cba6. [DOI] [PubMed] [Google Scholar]
- 50.Abelson JL, Khan S, Liberzon I, et al. Effects of perceived control and cognitive coping on endocrine stress responses to pharmacological activation. Biol Psychiatry. 2008;64:701–7. doi: 10.1016/j.biopsych.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Truninger R, Uthoff H, Capraro J, et al. Glucose control during a driving training in patients with type 1 and type 2 diabetes mellitus—a randomised, controlled trial. Exp Clin Endocr Diab. 2013;121:420–4. doi: 10.1055/s-0033-1347246. [DOI] [PubMed] [Google Scholar]
- 52.Wiesli P, Krayenbühl PA, Kerwer O, et al. Maintenance of glucose control in patients with type 1 diabetes during acute mental stress by riding high-speed rollercoasters. Diabetes Care. 2007;30:1599–601. doi: 10.2337/dc06-2102. [DOI] [PubMed] [Google Scholar]
- 53.Wiesli P, Schmid C, Kerwer O, et al. Acute psychological stress affects glucose concentrations in patients with type 1 diabetes following food intake but not in the fasting state. Diabetes Care. 2005;28:1910–5. doi: 10.2337/diacare.28.8.1910. [DOI] [PubMed] [Google Scholar]
- 54.Phan-Hug F, Thurneysen E, Theintz G, et al. Impact of videogame playing on glucose metabolism in children with type 1 diabetes. Pediatr Diabetes. 2011;12:713–7. doi: 10.1111/j.1399-5448.2011.00770.x. [DOI] [PubMed] [Google Scholar]
- 55.Cryer PE. Hypoglycemia in type 1 diabetes mellitus. Enodocrinol Metab Clin N Am. 2010;39:641–54. doi: 10.1016/j.ecl.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cesana G, Panza G, Ferrario M, et al. Can glycosylated hemoglobin be a job stress parameter? J Occup Environ Med. 1985;27:357–60. doi: 10.1097/00043764-198505000-00015. [DOI] [PubMed] [Google Scholar]
- 57.Xu W, Hang J, Gao W, et al. Association between job stress and newly detected combined dyslipidemia among Chinese workers: findings from the SHISO study. J Occup Health. 2011;53:334–42. doi: 10.1539/joh.11-0023-oa. [DOI] [PubMed] [Google Scholar]
- 58.Cutrona CE, Abraham WT, Russell DW, et al. Financial strain, inflammatory factors, and haemoglobin A1c levels in African American women. Brit J of Health Psychol. 2015;20:662–79. doi: 10.1111/bjhp.12120. [DOI] [PubMed] [Google Scholar]
- 59.Baucom KJ, Queen TL, Wiebe DJ, et al. Depressive symptoms, daily stress, and adherence in late adolescents with type 1 diabetes. Health Psychol. 2015;34:522–30. doi: 10.1037/hea0000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gonzalez JS, Shreck E, Psaros C, et al. Distress and type 2 diabetes-treatment adherence: a mediating role for perceived control. Health Psychol. 2015;34:505–13. doi: 10.1037/hea0000131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tran V, Wiebe DJ, Fortenberry KT, et al. Benefit finding, affective reactions to diabetes stress, and diabetes management among early adolescents. Health Psychol. 2011;30:212–9. doi: 10.1037/a0022378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yi JP, Vitaliano PP, Smith RE, et al. The role of resilience on psychological adjustment and physical health in patients with diabetes. Brit J of Health Psychol. 2008;13:311–25. doi: 10.1348/135910707X186994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Perfect MM, Elkins GR, Lyle-Lahroud T, et al. Stress and quality of sleep among individuals diagnosed with diabetes. Stress Health. 2010;26:61–74. [Google Scholar]
- 64.Knutson KL, Van Cauter E, Zee P, et al. Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes the coronary artery risk development in young adults (CARDIA) sleep study. Diabetes Care. 2011;34:1171–6. doi: 10.2337/dc10-1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Barone MT, Menna-Barreto L. Diabetes and sleep: a complex cause-and-effect relationship. Diabetes Res Clin Pract. 2011;91:129–37. doi: 10.1016/j.diabres.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 66.Hilliard ME, Holmes CS, Chen R, et al. Disentangling the roles of parental monitoring and family conflict in adolescents’ type 1 diabetes self-care. Health Psychol. 2013;32:388–96. doi: 10.1037/a0027811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davidson M, Penney EA, Muller B, et al. Stressors and self-care challenges faced by adolescents living with type 1 diabetes. Applied Nursing Research. 2004;17:72–80. doi: 10.1016/j.apnr.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 68.Berlin KS, Rabideau EM, Hains AA. Empirically derived patterns of perceived stress among youth with type 1 diabetes and relationships to metabolic control. J Pediatr Psychol. 2012;37:990–8. doi: 10.1093/jpepsy/jss080. [DOI] [PubMed] [Google Scholar]
- 69.Jaser SS, Grey M. A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. J Pediatr Psychol. 2010;35:738–47. doi: 10.1093/jpepsy/jsp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rintala TM, Jaatinen P, Paavilainen E, et al. Interrelation between adult persons with diabetes and their family a systematic review of the literature. J Fam Nurs. 2013;19:3–28. doi: 10.1177/1074840712471899. [DOI] [PubMed] [Google Scholar]
- 71.Mayberry LS, Osborn CY. Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care. 2012;35:1239–45. doi: 10.2337/dc11-2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Surwit RS, van Tilburg MA, Zucker N, et al. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes care. 2002;25(1):30–4. doi: 10.2337/diacare.25.1.30. [DOI] [PubMed] [Google Scholar]
- 73.Koloverou E, Tentolouris N, Bakoula C, et al. Implementation of a stress management program in outpatients with type 2 diabetes mellitus: a randomized controlled trial. Hormones. 2014;13(4):509–18. doi: 10.14310/horm.2002.1492. [DOI] [PubMed] [Google Scholar]
- 74.Tang TS, Funnell MM, Brown MB, et al. Self-management support in “real-world” settings: an empowerment-based intervention. Patient Educ Couns. 2010;79:178–84. doi: 10.1016/j.pec.2009.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fisher L, Hessler D, Glasgow RE, et al. REDEEM: a pragmatic trial to reduce diabetes distress. Diabetes Care. 2013;36:2551–8. doi: 10.2337/dc12-2493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Grey M, Boland EA, Davidson M, et al. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr. 2000;137(1):107–13. doi: 10.1067/mpd.2000.106568. [DOI] [PubMed] [Google Scholar]
- 77.Whittemore R, Jaser SS, Jeon S, et al. An internet coping skills training program for youth with type 1 diabetes: six-month outcomes. Nurs Res. 2012;61:395–404. doi: 10.1097/NNR.0b013e3182690a29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Laffel LMB, Vangsness L, Connell A, et al. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr. 2003;142:409–16. doi: 10.1067/mpd.2003.138. [DOI] [PubMed] [Google Scholar]
- 79.Katz ML, Volkening LK, Butler DA, et al. Family-based psychoeducation and care ambassador intervention to improve glycemic control in youth with type 1 diabetes: a randomized trial. Pediatr Diabetes. 2014;15:142–50. doi: 10.1111/pedi.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sturt J, Dennick K, Hessler D, Hunter B, Oliver J, Fisher L. Effective interventions for reducing diabetes distress: systematic review and meta-analysis. Int Diabetes Nurs. 2015;2:40–55. [Google Scholar]
- 81.Wysocki T, Harris MA, Buckloh LM, et al. Randomized trial of behavioral family systems therapy for diabetes: maintenance effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30:555–60. doi: 10.2337/dc06-1613. [DOI] [PubMed] [Google Scholar]
- 82.Van Houtum L, Rijken M, Heijmans M, Gorenewegen P. Patientperceived self-management tasks and support needs of people with chronic illness: generic or disease specific? Ann Behav Med. 2015;49:221–9. doi: 10.1007/s12160-014-9649-0. [DOI] [PubMed] [Google Scholar]
- 83.Rosenberg AR, Yi-Frazier JP, Eaton JP, et al. Promoting resilience in stress management: a pilot study of a novel resilience-promoting intervention for adolescents and young adults with serious illness. J Pediatr Psychol. 2015;40:992–9. doi: 10.1093/jpepsy/jsv004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fisher L, Hessler D, Masharani U, Strycker L. Impact of baseline patient characteristics on interventions to reduce diabetes distress: the role of personal conscientiousness and diabetes self-efficacy. Diabet Med. 2014;31:739–46. doi: 10.1111/dme.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mochari-Greenberger H, Lee V, Luka A, Peters A, Pande RL. A tele-behavioral health intervention to reduce depression, anxiety, and stress and improve diabetes self-management. Telemedicine e-Health. 2016 doi: 10.1089/tmj.2015.0231. ahead of print: [DOI] [PubMed] [Google Scholar]
- 86.Herman WH, Cohen RM. Racial and ethnic differences in the relationship between HbA1c and blood glucose: implications for the diagnosis of diabetes. J Clin Endo Metabol. 2012;97:1067–72. doi: 10.1210/jc.2011-1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Willi SM, Miller KM, DiMeglio LA, et al. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424–34. doi: 10.1542/peds.2014-1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Naranjo D, Schwartz DD, Delamater A. Diabetes in ethnically diverse youth: disparate burden and intervention approaches. Curr Diab Rep. 2015;11:251–60. doi: 10.2174/1573399811666150421115846. [DOI] [PubMed] [Google Scholar]