Abstract
Individuals with chronic pain show a greater vulnerability to depression or anger than those without chronic pain, and also show greater interpersonal difficulties and physical disability. The current study examined data from 675 individuals with chronic pain during their initial visits to a tertiary care pain clinic using assessments from Stanford University's Collaborative Health Outcomes Information Registry (CHOIR). Using a path modeling analysis, the mediating roles of PROMIS Physical Function and PROMIS Satisfaction with Social Roles and Activities were tested between pain intensity and PROMIS Depression and Anger. Pain intensity significantly predicted both depression and anger, and both physical function and satisfaction with social roles mediated these relationships when modeled in separate 1-mediator models. Notably, however, when modeled together, ratings of satisfaction with social roles mediated the relationship between physical function and both anger and depression. Our results suggest that the process by which chronic pain disrupts emotional well-being involves both physical function and disrupted social functioning. However, the more salient factor in determining pain-related emotional distress appears to be disruption of social relationships, rather than global physical impairment. These results highlight the particular importance of social factors to pain-related distress, and highlight social functioning as an important target for clinical intervention in chronic pain.
Keywords: Chronic pain, anger, depression, social function, physical function, CHOIR
Two important and related psychological problems common in chronic pain are anger and depression. Chronic pain predicts an increased susceptibility to depression [14] and problems with anger [13]. However, these relationships are likely bi-directional; a history of significant depression increases vulnerability to the later development of a chronic pain condition [14]. Similarly, anger worsens the intensity of pain [4], contributes to greater disability [28], and worsens the experience of depression [35]. A significant degree of anger and depression in chronic pain may occur because pain impedes individual goals and valued pursuits [19,26], leading to emotional states of frustration, which can develop into anger [13].
However, the emotional consequences of pain-related frustration of goals may be more salient in some domains than others. More specifically, impairment in social domains may have significant implications for emotional functioning. Stressful or conflictual interactions with others contribute to higher levels of depression [10,23], anger [12], negative affect [32], and pain intensity [11]. The relationship between pain and social problems is likely bi-directional, however, as problematic social relationships are more common in chronic pain. Individuals with a chronic pain condition are more susceptible to conflictual interactions with others [12], are more reactive to ongoing interpersonal stressors [36], and show a tendency to withdraw from sources of positive social engagement, particularly when pain is more intense [32]. This phenomenon is further complicated by extant emotional states: the presence of significant depression worsens physical and psychosocial functioning, above and beyond the experience of pain [21]. Similarly, social relationships may be viewed more negatively under conditions of negative emotion or stress, thereby discounting their positive aspects [8]. Consequently, it is not only the presence of actual social conflict, but also the appraisal of social relationships that has implications for emotional states in chronic pain.
To date, no studies have examined the concurrent contributions of physical function and social satisfaction in predicting pain-related emotional distress. The current study examined how pain intensity, physical functioning, and satisfaction with social roles and activities uniquely contribute to self-reported levels of both depressive symptoms and anger in individuals with chronic pain. Further, we examined how these indices of physical and social functioning may be intervening factors in pain-related emotional distress; we tested self-reported physical functioning and satisfaction with social roles and activities as mediators of the relationships between pain and both anger and depression. We expected that the effects of pain intensity on both anger and depression would be uniquely accounted for by broader physical functioning and the degree of satisfaction that individuals derive from their social relationships. Further, we hypothesized that physical function, a broader measure of overall function, would inform an individual's level of social functioning to some degree. Therefore, we sought to test whether physical function mediated the relationship between pain intensity and social satisfaction. We estimated our models using data from 675 treatment-seeking individuals with chronic pain at a tertiary care pain clinic, which were collected via the Collaborative Health Outcomes Information Registry (CHOIR), created by Stanford University [1].
Methods
Study procedures, which involved exclusively retrospective review of clinical data, were approved by the Institutional Review Board at the Stanford University School of Medicine.
Participants
Data were collected from 675 patients who presented for initial medical evaluations at the Stanford Pain Management Center, a large, tertiary care pain clinic. The sample was 61.6% female (N = 416), 33.3% male (N = 225), and 5% did not provide a gender (N = 34). The predominant ethnicity in the current sample was Caucasian (60.3% of the overall sample), followed by Asian (6.8%), African American (4.3%), Native Hawaiian or Pacific Islander (.7%), and American Indian or Alaska Native (0.6%). Approximately one sixth of the sample (17.8%) reported an ethnicity of “Other,” 1.8% of the sample reported their ethnicity as “Unknown,” and 7.7% of the sample did not endorse an ethnicity. Median education in the patient sample was a completed Bachelor's Degree. 65.9% of the sample was married. At the time of data collection, 35.3% of the sample (N = 238) reported employment, and 25.8% (N = 174) of the sample reported being legally disabled. Mean age in the current sample was 50.2 years (range 18 to 94 years).
Pain diagnosis information was gathered from the International Classification of Diseases, Ninth Revision (ICD-9) codes associated with each patient's initial clinic visit. Regarding the frequency of pain diagnoses, the largest proportion of patients were referred to the pain clinic for thoracolumbar pain (21.3% of the sample), followed by nerve pain (19.4%), orofacial pain (15.9%), other musculoskeletal pain (12.1%), fibromyalgia and/or myofascial pain (11.3%), abdominal pain (6.4%), neck pain (6.2%), and pelvic pain (3.4%). At the time of the initial visit, 443 patients (75.3% of the sample) carried a single pain diagnosis, 127 patients (21.6% of the sample) had 2 pain diagnoses, 17 patients (2.5% of the sample) had 3 pain diagnoses, and 1 patient (0.1% of the sample) carried 4 pain diagnoses. Pain diagnosis information was unavailable for 87 patients in the current sample. Full pain diagnosis information for this sample can be found in an online appendix.
Procedures
At their initial medical appointments at the pain clinic, patients were sent an email requesting they fill out a series of questionnaires. Patients either filled them out at home on their personal computer or tablet or were provided a tablet computer upon their initial visit. Study questionnaires were administered through CHOIR. CHOIR (http://choir.stanford.edu) is an open source, open platform health outcomes registry and learning health system. CHOIR assesses multiple domains of physical, psychological and social functioning using Patient-Reported Outcomes Measurement Information Systems (PROMIS) item banks. PROMIS item banks are psychometrically sound and empirically validated assessments published by the National Institutes of Health. CHOIR also uses legacy instruments to assess domains not currently covered by PROMIS. CHOIR implements a local computerized adaptive testing (CHOIR-CAT) [22] approach that identifies optimal items within a domain based on previous responses by the individual, rather than using a fixed number of items, as in traditional, static forms of assessment [5,16]. This local CAT approach is based on the CAT algorithm used by the Northwestern University Assessment Center, which has provided open access to PROMIS instruments [16].CAT assessments require a smaller number of items in order to effectively assess a given construct, and also show higher reliability of measurement compared to traditional forms of assessment [22]. Data from CHOIR have been used in prior empirical work [31].
Measures
PROMIS Pain Intensity
Pain intensity was assessed using a modified PROMIS Pain Intensity scale, utilizing an 11-point numerical rating scale (NRS), ranging from 0-10 [9]. Respondents were asked to rate their average pain intensity over the previous 7 days. Use of NRS has been identified as a suitable assessment of pain intensity in acute and chronic pain populations in previous studies [7].
PROMIS Instruments
Item banks for Satisfaction with Social Roles and Activities, Physical Function, Depression, and Anger from PROMIS [6] were administered to patients at their initial clinic visit (descriptions of all PROMIS item bank descriptions are available at http://www.nihpromis.org/measures/domainframework1). PROMIS Physical Function items assess the ability to carry out a variety of activities requiring physical action, ranging from severe impairment to very high levels of physical ability, while items from PROMIS Satisfaction with Social Roles and Activities assess levels of satisfaction with engagement in one's typical social roles and activities, such as engagement with one's family, work, and leisure activities. PROMIS Anger items assess several anger-relevant domains, including angry mood, negative social cognitions, verbal aggression, and attempts to control anger. PROMIS Depression items assess negative mood, negative views of the self, negative cognitions, and decreased positive emotion and engagement. Unlike traditional, static assessment tools that utilize a composite score using a set number of items, PROMIS instruments are based on an Item Response Theory-based assessment that utilizes item-level responses [2,20]. PROMIS measures utilize U.S. population norms and have a mean of 50 points and a standard deviation of 10 points [6]. Use of CAT-based administrations typically leads to a smaller number of items per assessment, but yield superior efficiency in domain assessment and greater precision (i.e. lower standard error) compared to traditional, non-adaptive testing forms [15]. Higher scores on average pain intensity, anger, and depression signified greater severity of these symptoms, while higher scores on PROMIS Physical Function and PROMIS Satisfaction with Social Roles and Activities reflected higher (more positive) ratings on these measures. Items from PROMIS Anger and Depression item pools assess the experience of these symptoms over the past 7 days, while PROMIS Physical Function and Satisfaction with Social Roles and Activities assess a more general level of function that does not specify a particular time frame.
Analytic Plan
Path models were estimated using Mplus software [27] to test the indirect effects of average pain intensity on depression and anger through ratings of satisfaction with social roles and activities and overall physical function. Three distinct models were constructed to test our hypotheses. First, we tested only the direct relationships between pain and both depression and anger. Second, we constructed separate one-mediator models testing physical function or satisfaction with social roles and activities as a mediator of the relationship between pain and both anger and depression. Finally, we tested a fully-specified model in which physical function and satisfaction with social roles and activities were tested as concurrent mediators of the direct paths between pain and both anger and depression. Standardized path coefficients were reported for both direct and indirect (i.e., mediated) effects in order to provide a common metric for interpretation of study findings. We calculated the significance of indirect (mediating) effects (i.e., the ab product coefficient) using a 1000-draw bootstrap-estimated product of the coefficients of the predictor-mediator path (the a path) and the mediator-outcome path (the b path), which yields a higher degree of power and are less susceptible to Type-I error than normal theory mediation analysis [25]. As Mplus does not provide significance values for standardized path coefficient models, however, we have reported significance values from identical unstandardized path coefficient models, in order to provide estimates of statistical significance for each examined path. Depression and anger were freed to co-vary based on a theoretical likelihood of shared variance between these variables. Covariates representing age, gender, and marital status associated with initial clinic visits were included in the estimation of all paths.
Results
Descriptive statistics can be found in Table 1, correlations between study variables can be found in Table 2, and the total proportion of variance of each outcome variable (satisfaction with social roles and activities, physical function, depression, and anger) accounted for in each model can be found in Table 3. When the direct effects of pain intensity were modeled without any other predictors in the model, higher ratings of average pain intensity significantly predicted higher concurrent levels of anger (β = .245, p < .001) and depression (β = .328, p < .001), poorer physical function (β = −.418, p < .001), and lower satisfaction with social roles and activities (β = −.237, p < .001). Inclusion of covariates representing age, gender, and marital status did not change the direction or significance of these direct paths.
Table 1.
Means and Standard Deviations of Study Variables.
| Study Variable | Mean (SD) |
|---|---|
| VAS Average Pain Intensity | 5.78 (2.16) |
| PROMIS Anger | 52.86 (10.14) |
| PROMIS Depression | 57.55 (9.58) |
| PROMIS Physical Function | 36.11 (8.82) |
| PROMIS Satisfaction with Social Roles and Activities | 42.14 (9.58) |
Note: PROMIS assessments are based on a mean of 50 with a standard deviation of 10.
Note: VAS scores were assessed on an 11-point scale from 0-10.
Table 2.
Correlations Between Study Variables
| Pain Intensity | Physical Function | Social Satisfaction | Anger | Depression | |
|---|---|---|---|---|---|
| Pain Intensity | 1 | −.452 | −.246 | .214 | .335 |
| Physical Function | 1 | .617 | −.238 | −.444 | |
| Social Satisfaction | 1 | −.389 | −.538 | ||
| Anger | 1 | .690 | |||
| Depression | 1 |
Table 3.
Proportion of Amount of Variance Accounted for- Single-mediator and 2-mediator models
| Physical Function as Mediator | Social Satisfaction as Mediator | Physical Function and Social Satisfaction as Mediator | |
|---|---|---|---|
| Observed Variable | R2 Variance | R2 Variance | R2 Variance |
| Physical Function | .233 | N/A | .233 |
| Social Satisfaction | N/A | .063 | .407 |
| Anger | .116 | .183 | .192 |
| Depression | .229 | .323 | .339 |
Physical Function as a Mediator
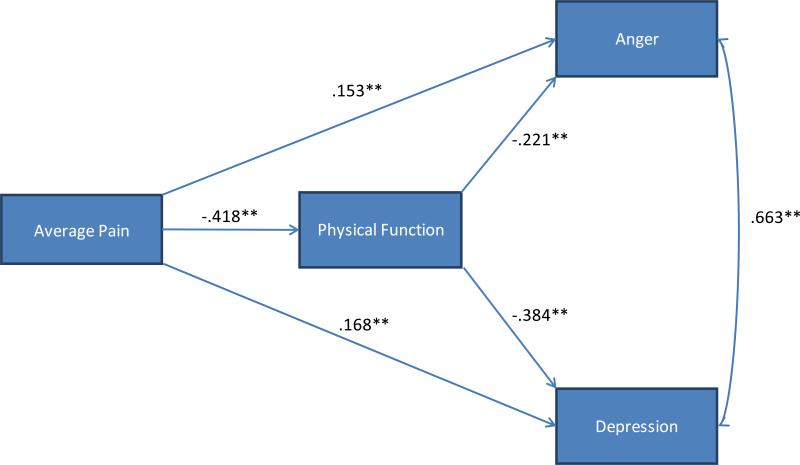
Figure 1 depicts an estimated model in which physical function, but not social satisfaction, was tested as a mediator. In this model, greater pain intensity scores significantly predicted lower levels of physical function, as well as higher levels of anger and depression. Greater scores on physical function (representing a higher level of physical function) significantly predicted lower levels of both depression and anger. The mediating effects of physical function on the relationships between pain and anger (ab = .092, p < .001) and pain and depression (ab = .191, p < .001) were statistically significant. The paths from pain intensity to both anger and depression remained significant when physical function was included as a mediator in the model, however, suggesting that physical function is a partial, rather than full, mediator of the relationships between pain and emotional distress. Proportion of variance (R2) estimates suggested that 23.3% of variance in physical function scores, 11.6% of variance in anger scores, and 22.9% of variance in depression scores were accounted for by predictors in this model. The direction and significance of these direct and mediated effects did not change when covariates representing age, gender, and marital status were included in the model.
Figure 1.
Path model representing indirect effects of average pain intensity on measures of anger and depression through self-rated physical function.
Note: ** = p < .01, * = p < .05 t = p < .10
Note: All path coefficients are standardized.
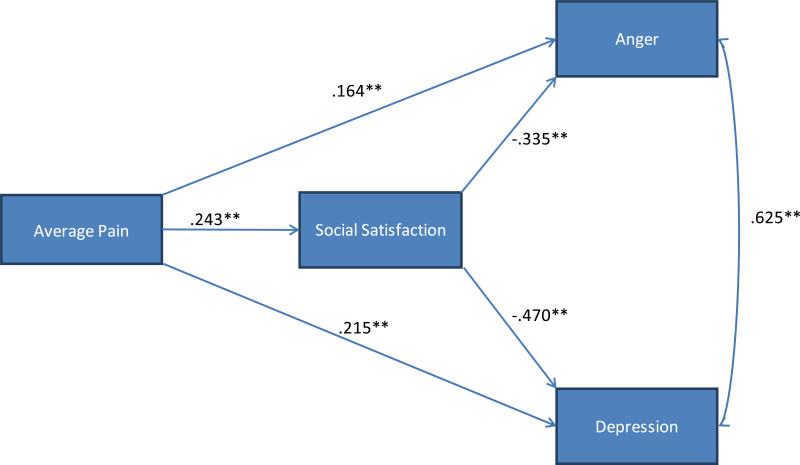
Social Satisfaction as a Mediator
Figure 2 depicts an estimated model in which satisfaction with social roles and activities, but not physical function, was tested as a mediator. In this model, greater pain intensity scores again significantly predicted lower levels of social satisfaction and higher levels of anger and depression. Higher scores on social satisfaction (representing a greater level of satisfaction with one's engagement in social roles and activities) significantly predicted lower levels of both depression and anger. The mediating effects of social satisfaction on the relationships between pain and anger (ab = .081, p < .001) and pain and depression (ab = .114, p < .001) were statistically significant. As in the model with only physical function as a mediator, the paths from pain intensity to both anger and depression remained significant when social satisfaction was included as a mediator in the model. Proportion of variance (R2) estimates suggested that 6.3% of variance in social satisfaction scores, 18.3% of variance in anger scores, and 32.3% of variance in depression scores were accounted for by predictors in this model. The direction and significance of these direct and mediated effects did not change when covariates representing age, gender, and marital status were included in the model.
Figure 2.
Path model representing indirect effects of average pain intensity on measures of anger and depression through satisfaction with social roles and activities.
Note: ** = p < .01, * = p < .05 t = p < .10
Note: All path coefficients are standardized.
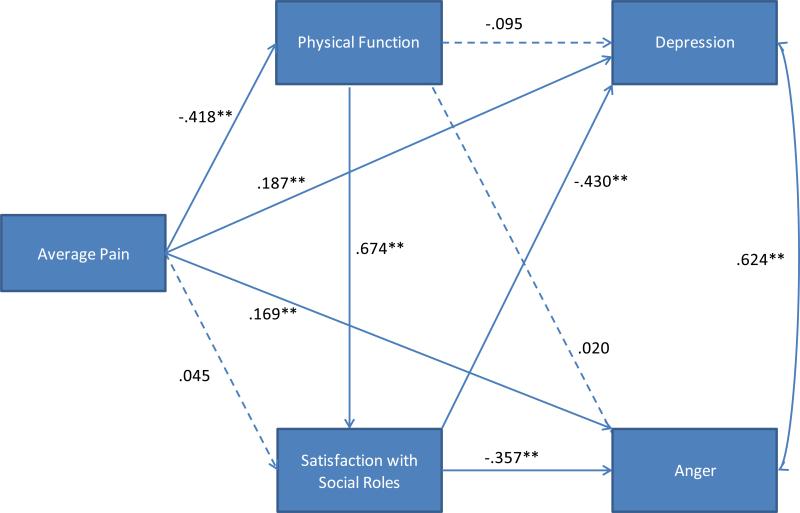
Social Satisfaction and Physical Function as Mediators
Figure 3 depicts an estimated model in which physical function and social satisfaction were simultaneously tested as mediators of the relationships between pain and both depression and anger. In this model, greater pain intensity scores significantly predicted lower levels of physical function, but did not significantly predict social satisfaction scores, above and beyond the effects of physical function. Notably, social satisfaction demonstrated unique and significant relationships with both anger and depression, while physical function did not significantly predict depression (β = −.095, p = .069) or anger (β = .020, p = .693), above and beyond the effects of pain intensity and social satisfaction. Unsurprisingly, examination of standardized path coefficients suggested that social satisfaction was a stronger predictor of both depression and anger than physical function. As with previous models, the direction and significance of these direct and mediated effects did not change when covariates representing age, gender, and marital status were included in the model.
Figure 3.
Path model representing indirect effects of pain on measures of anger and depression through physical function and satisfaction with social roles and activities.
Note: ** = p < .01, * = p < .05 t = p < .10
Note: Dashed lines represent non-significant path
In the fully specified model, physical function was a significant mediator of the relationship between pain intensity and social satisfaction (ab = −.282, p < .001), but did not mediate the relationships between pain and anger (ab = −.008, p = .695) or pain and depression (ab = .040, p = .074). Social satisfaction was found to be a significant mediator of the relationship between physical function and both anger (ab = −.241, p < .001) and depression (ab = −.290, p < .001), but did not mediate the relationships between pain intensity and depression (ab = −.019, p = .278) or pain intensity and anger (ab = −.016, p = .285). R2 estimates suggested that 23.3% of variance in physical function scores, 40.7% of variance in social satisfaction scores, 19.2% of variance in anger scores, and 33.9% of variance in depression scores were accounted for by predictors in this model.
Discussion
The relationship between chronic pain and emotional distress is influenced by a complex interplay of both physical and social factors. In a sample of 675 individuals with chronic pain, our path modeling analysis suggested significant relationships between higher average levels of pain intensity, higher anger and depression scores, decreased physical function, as well as decreased social satisfaction. These results support previous findings suggesting a disruptive effect of pain on physical, social, and emotional functioning [12,29,30,32,36].
Furthermore, our analyses revealed several mediated effects in the relationships between pain intensity and both depression and anger. When tested separately, physical function and satisfaction with social roles and activities significantly mediated the relationships between pain intensity and both anger and depression. These findings support previous research suggesting that decreased physical function predicts disrupted mood states in chronic pain [24], and also highlight the particular importance of social factors in pain-related negative emotional states [10,12]. However, inclusion of both physical function and social satisfaction as mediators between pain intensity and emotional distress highlighted the complexity of these relationships. More specifically, inclusion of social satisfaction as a mediator uniquely explained the relationship between physical function and both anger and depression, rendering the direct relationships between physical function and both anger and depression to non-significance.
Impairments in the pursuit of one's goals may worsen emotional distress; this study characterizes this relationship in even finer detail by demonstrating that not all forms of frustration equally impact emotional distress. Specifically, pain may inspire greater levels of emotional distress when it negatively impacts one's ability to relate to other people in satisfying ways, above and beyond the levels of frustration inherent in pain-related physical limitation. Further, our results suggest that social satisfaction may be an undervalued treatment aim for improving mood states of individuals with chronic pain. Clinicians may effectively address emotional distress in patients with chronic pain by supporting attempts to return to valued social engagements, even if overall physical function remains somewhat limited.
Our results also highlight the complex nature of pain-related emotional distress. Structural path models, which allow for concurrent modeling of multiple predictors and outcomes, allow for a greater level of complexity than univariate predictive approaches, such as multiple linear regression. Our analytic approach allowed us to construct models that more stringently assess the uniqueness of relationships between multiple observed variables and, further, to test the independent mediated effects contained therein. A greater level of statistical sophistication in modeling the antecedents and consequences of a complex medical and psychological variable like pain may yield more clinically and empirically useful models of disruption and adaptation to pain.
Limitations
Though informative, some limitations of our current findings should be acknowledged. First, the estimated path models in the current study utilize cross-sectional data and therefore cannot fully support inferences about temporal causality. Further, it is likely that we are capturing one aspect of several bi-directional relationships between pain and all domains of functioning. For example, depression exacerbates the emotional-motivational aspects of pain [17] and worsens pain-related decrements in physical function [21,34], while anger may increase sensitivity to pain [3,4], exacerbate decrements in physical activity [24], and increase perceptions of pain-related interference [24]. Similarly, individuals endorsing higher levels of anger or depression may view their social interactions in a more negative fashion [21]. These studies thus suggest that pain, physical and social function, and emotional distress likely serve as mutually influential mechanisms of disruption. Similarly, our theoretical approach to the current study was predicated on the assumption that physical and social disruption reflects a degree of frustration of individual goals. Though pain may generally contribute to this type of frustration through impaired function, we did not directly assess the extent to which pain impeded individual goals, nor did we directly address emotional states of frustration. Given that impeding personally-held goals may be a causal mechanism for anger or depression, these variables should be directly measured in future studies.
Also missing from our model is anxiety, a psychological variable that has significant implications for pain. Although anxiety has been connected to goal frustration [18], its relation to this construct is primarily anticipatory (i.e., those individuals who are more anxious report feeling less able to tolerate goal frustration). Given that the current model focuses on existing disruptions in function, we focused on constructs that showed a greater conceptual fit with our measurement of outcomes. Nevertheless, the role of anxiety and beliefs about tolerance of goal frustration in the context of pain-related emotional distress warrants attention in future studies.
It is notable that our data were collected from a large, heterogeneous group of individuals who were attending their initial appointments at a tertiary care pain clinic. This fact suggests three potential limitations to our findings. First, the diversity of our sample does not allow for clear comparisons of these effects across different pain conditions. For example, individuals coping with a pain condition that is more poorly understood by the general public (e.g., pain disorders potentially arising from central nervous system sensitization like fibromyalgia), pain affecting sensitive areas that may carry social stigma (e.g., pelvic or genital pain), or pain of an ambiguous origin may be more susceptible to disrupted social relationships, potentially due to differential availability in actual or perceived instrumental or emotional support. Second, these results may not generalize to individuals with lower levels of typical pain who are not seeking specialized medical treatment, or to patients that have already shown greater responses to their pain treatment. More specifically, the treatment-seeking nature of patients from a tertiary care pain clinic may contribute to measurable differences in some domains (e.g., higher levels of depression and pain intensity) than patients who do not require the need for specialized medical care. Third, although the large sample size in our study allowed for the estimation of a more sophisticated statistical model, one potential limitation of large sample sizes is the potential for identification of effects that meet criteria for statistical significance but may not show corresponding levels of clinical significance. Although the proportional variance accounted for in each outcome variable was of acceptable size, the statistical significance of some of the effects in our estimated models (e.g., the residual effects of pain intensity on pain and depression in the fully estimated 2-mediator model) may have been inflated by the size of the sample and may not independently represent clinically significant effects.
Directions for Future Research
Given that cross-sectional analysis does not allow for a strong inference regarding the temporal causality of examined variables, we urge future attention to these relationships using time-series or longitudinal data. Use of time-lagged models or longitudinal studies may further support our proposed causal chain of effects by accounting for concurrent levels of an examined outcome when predicting future changes in an examined outcome such as social satisfaction, anger, or depression. For example, comparing the relative effects of changes in social satisfaction across time on emotional distress, compared to changes in measures of overall physical function, would further illustrate the emotional salience of pain-related social interference. Alternatively, adoption of treatment models in which social function is the primary intervention for individuals with chronic pain may clarify whether social functioning constitutes a causal mechanism in pain-related distress, as our findings suggest.
Additionally, future studies should address the inclusion of goals and motivational factors within this model, which may be significant moderators of the relationship between physical or social functioning and emotional distress. This concept is particularly salient in the context of theoretical models that identify frustration of specific and individually-held goals as an important precipitant of anger [33]. Consequently, there may be other motivational or goal-oriented factors that may enhance emotional distress when pain disrupts function. For example, the expectations and goals of an individual who has retired from his or her career is likely to vary significantly from those of an individual in his or her mid-20s who may still be in the process of training and establishing his or her career goals, leading to very different responses to pain-related disruptions in physical function. As a result, models that account for other aspects of an individual's specific life circumstances and consequent goal orientation would add further granularity and value to our findings.
Conclusions
The current study utilized a large sample of individuals with diverse chronic pain conditions to examine the independent effects of pain, physical function, and satisfaction with social roles and activities on concurrent levels of anger and depression. Our results highlight the relative importance of social relationships in predicting emotional distress compared to overall physical function, which appears to be a more distal predictor of psychological functioning in chronic pain. The current study illuminates the need for statistically complex models in examining even relatively well-established mechanisms of pain-related dysregulation, as well as the need for greater attention to individual difference variables that may add further texture to the complex nature of psychosocial functioning in chronic pain.
Supplementary Material
Acknowledgments
The authors wish to acknowledge funding from the National Institutes of Health (NIH HHSN 271201200728P, NIH K24 DA029262, and NIH P01 AT006651), as well as the Redlich Pain Endowment.
Footnotes
Disclosures:
The authors have no other financial conflicts to disclose.
References
- 1.Collaborative Health Outcomes Information Registry (CHOIR) 2015 Retrieved from http://choir.stanford.edu.
- 2.Amtmann D, Cook KF, Jensen MP, Chen WH, Choi S, Revicki D, Cella D, Rothrock N, Keefe F, Callahan L, Lai JS. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150(1):173–182. doi: 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruehl S, Burns JW, Chung OY, Ward P, Johnson B. Anger and pain sensitivity in chronic low back pain patients and pain-free controls: The role of endogenous opioids. Pain. 2002;99(1):223–233. doi: 10.1016/s0304-3959(02)00104-5. [DOI] [PubMed] [Google Scholar]
- 4.Bruehl S, Chung OY, Donahue BS, Burns JW. Anger regulation style, postoperative pain, and relationship to the A118G mu opioid receptor gene polymorphism: a preliminary study. J Behav Med. 2006;29(2):161–169. doi: 10.1007/s10865-005-9030-7. [DOI] [PubMed] [Google Scholar]
- 5.Cella D, Gershon R, Lai J-S, Choi S. The future of outcomes measurement: item banking, tailored short-forms, and computerized adaptive assessment. Qual Life Res. 2007;16(1):133–141. doi: 10.1007/s11136-007-9204-6. [DOI] [PubMed] [Google Scholar]
- 6.Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, Ader D, Fries JF, Bruce B, Rose M, Group PC. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook KF, Dunn W, Griffith JW, Morrison MT, Tanquary J, Sabata D, Victorson D, Carey LM, MacDermid JC, Dudgeon BJ. Pain assessment using the NIH Toolbox. Neurol. 2013;80(11 Supplement 3):S49–S53. doi: 10.1212/WNL.0b013e3182872e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis MC, Zautra AJ, Smith BW. Chronic pain, stress, and the dynamics of affective differentiation. J Pers. 2004;72(6):1133–1159. doi: 10.1111/j.1467-6494.2004.00293.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 10.Faucett JA. Depression in painful chronic disorders: The role of pain and conflict about pain. J Pain Symptom Manage. 1994;9(8):520–526. doi: 10.1016/0885-3924(94)90114-7. [DOI] [PubMed] [Google Scholar]
- 11.Faucett JA, Levine JD. The contributions of interpersonal conflict to chronic pain in the presence or absence of organic pathology. Pain. 1991;44(1):35–43. doi: 10.1016/0304-3959(91)90144-M. [DOI] [PubMed] [Google Scholar]
- 12.Feldman SI, Downey G, Schaffer-Neitz R. Pain, negative mood, and perceived support in chronic pain patients: a daily diary study of people with reflex sympathetic dystrophy syndrome. J Consult Clin Psych. 1999;67(5):776–785. doi: 10.1037//0022-006x.67.5.776. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez E, Turk DC. The scope and significance of anger in the experience of chronic pain. Pain. 1995;61(2):165–175. doi: 10.1016/0304-3959(95)00192-U. [DOI] [PubMed] [Google Scholar]
- 14.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13(2):116–137. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Fries JF, Cella D, Rose M, Krishnan E, Bruce B. Progress in assessing physical function in arthritis: PROMIS short forms and computerized adaptive testing. J Rheumatol. 2009;36(9):2061–2066. doi: 10.3899/jrheum.090358. [DOI] [PubMed] [Google Scholar]
- 16.Gershon R, Rothrock NE, Hanrahan RT, Jansky LJ, Harniss M, Riley W. The development of a clinical outcomes survey research application: Assessment CenterSM. Qual Life Res. 2010;19(5):677–685. doi: 10.1007/s11136-010-9634-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giesecke T, Gracely RH, Williams DA, Geisser ME, Petzke FW, Clauw DJ. The relationship between depression, clinical pain, and experimental pain in a chronic pain cohort. Arthritis Rheum. 2005;52(5):1577–1584. doi: 10.1002/art.21008. [DOI] [PubMed] [Google Scholar]
- 18.Harrington N. Frustration intolerance beliefs: Their relationship with depression, anxiety, and anger, in a clinical population. Cognit Ther Res. 2006;30(6):699–709. [Google Scholar]
- 19.Harris S, Morley S, Barton SB. Role loss and emotional adjustment in chronic pain. Pain. 2003;105(1):363–370. doi: 10.1016/s0304-3959(03)00251-3. [DOI] [PubMed] [Google Scholar]
- 20.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18(7):873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holzberg AD, Robinson ME, Geisser ME, Gremillion HA. The effects of depression and chronic pain on psychosocial and physical functioning. Clin J Pain. 1996;12(2):118–125. doi: 10.1097/00002508-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Kao MCJ, Cook K, Olson G, Pacht T, Darnall BD, Weber SC, Mackey SC. SNAPL-CAT: Catalyzing the rate-limiting step of big data psychometrics with item-response theory and advanced computerized adaptive testing (poster presentation).. American Medical Informatics Associations (AMIA) 2014 Joint Summits on Translational Science; San Francisco, CA. 2014. [Google Scholar]
- 23.Kerns RD, Haythornthwaite J, Southwick S, Giller EL. The role of marital interaction in chronic pain and depressive symptom severity. J Psychosom Res. 1990;34(4):401–408. doi: 10.1016/0022-3999(90)90063-a. [DOI] [PubMed] [Google Scholar]
- 24.Kerns RD, Rosenberg R, Jacob MC. Anger expression and chronic pain. J Behav Med. 1994;17(1):57–67. doi: 10.1007/BF01856882. [DOI] [PubMed] [Google Scholar]
- 25.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behav Res. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morley S, Davies C, Barton S. Possible selves in chronic pain: self-pain enmeshment, adjustment and acceptance. Pain. 2005;115(1):84–94. doi: 10.1016/j.pain.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 27.Muthén LK, Muthén BO. Mplus: Statistical Analysis with Latent Variables; User's Guide;[Version 5] Muthén & Muthén; 2007. [Google Scholar]
- 28.Okifuji A, Turk DC, Curran SL. Anger in chronic pain: investigations of anger targets and intensity. J Psychosom Res. 1999;47(1):1–12. doi: 10.1016/s0022-3999(99)00006-9. [DOI] [PubMed] [Google Scholar]
- 29.Sarzi-Puttini P, Fiorini T, Panni B, Turiel M, Cazzola M, Atzeni F. Correlation of the score for subjective pain with physical disability, clinical and radiographic scores in recent onset rheumatoid arthritis. BMC Musculoskelet Disord. 2002;3(1):18. doi: 10.1186/1471-2474-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scudds RJ, Robertson JM. Empirical evidence of the association between the presence of musculoskeletal pain and physical disability in community-dwelling senior citizens. Pain. 1998;75(2):229–235. doi: 10.1016/s0304-3959(97)00224-8. [DOI] [PubMed] [Google Scholar]
- 31.Sturgeon JA, Darnall BD, Kao M-CJ, Mackey SC. Physical and Psychological Correlates of Fatigue and Physical Function: A Collaborative Health Outcomes Information Registry (CHOIR) Study. J Pain. 2014;16(3):291–298.e291. doi: 10.1016/j.jpain.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sturgeon JA, Zautra AJ, Arewasikporn A. A multilevel structural equation modeling analysis of vulnerabilities and resilience resources influencing affective adaptation to chronic pain. Pain. 2014;155(2):292–298. doi: 10.1016/j.pain.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trost Z, Vangronsveld K, Linton SJ, Quartana PJ, Sullivan MJ. Cognitive dimensions of anger in chronic pain. Pain. 2012;153(3):515–517. doi: 10.1016/j.pain.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 34.Von Korff M, Ormel J, Katon W, Lin EH. Disability and depression among high utilizers of health care: a longitudinal analysis. Arch Gen Psychiatry. 1992;49(2):91–100. doi: 10.1001/archpsyc.1992.01820020011002. [DOI] [PubMed] [Google Scholar]
- 35.Wade JB, Price DD, Hamer RM, Schwartz SM, Hart RP. An emotional component analysis of chronic pain. Pain. 1990;40(3):303–310. doi: 10.1016/0304-3959(90)91127-5. [DOI] [PubMed] [Google Scholar]
- 36.Zautra AJ, Hamilton NA, Burke HM. Comparison of stress responses in women with two types of chronic pain: Fibromyalgia and osteoarthritis. Cognit Ther Res. 1999;23(2):209–230. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.