Electronic health records (EHRs) have become ubiquitous in the health care environment and bring with them the potential ability to monitor metrics as well as the promise of a variety of safety measures. While EHRs may enhance elements of patient safety, certain customary practices in EHR data entry may undermine professionalism, accountability, communication, and medical competence, particularly among learners who have no prior exposure to traditional medical record documentation. In the current educational landscape, it is crucial to develop EHR practices and strategies that reinforce and encourage intellectual curiosity, precision, and accuracy in reporting, rather than overtly or inadvertently encouraging superficiality in the service of efficiency.
The EHR unquestionably affects learning across the entire medical education continuum,1 and the interaction with the “iPatient” has changed the clinical experience of meeting (and documenting) a patient for the first time.2 Instead of learning to construct a plausible story after obtaining information from interactions with patients and family members, contemporary learners often document their initial experience in real time by checking required boxes and copying and, in some cases, pasting information into sections of the EHR that others had completed during prior encounters.
The EHR includes a variety of time-saving check boxes, automated history/physical examination functions, preworded phrases, templates, pregenerated problem lists, as well as prepopulated strings of characters and EHR-sanctioned copying and pasting (the “note forward” function). These shortcuts are meant to achieve efficiency; they are attractive means for technologically savvy students and trainees seeking to adhere to duty hour restrictions as well as for physicians facing high productivity and efficiency demands.3
Learners are likely to emulate their supervisors' EHR use, which is often designed to achieve maximal compliance with utilization reviewers' recommendations for optimal billing, rather than documenting the patient care trajectory or the underlying rationale or thought processes. Additionally, learners quickly realize that they can finish their notes rapidly by forwarding or pasting information from one day's note into the next, or by using simple phrases that insert a medication list, labs, and/or vital signs, often without safeguards to ensure anyone has actually read or verified the information or thought about the impact of this information on the patient's clinical condition or course. Even though learners often insist that they use automated EHR features and review their notes carefully to prevent errors, inaccurate information that has been either copied forward or incorrectly entered permeates the medical record.3
Early adopters of the EHR assumed copying and pasting items such as physical examinations, assessments, and plans would be rare, with initial data confirming that less than 10% of physical examinations in a US Department of Veterans Affairs EHR were copied and pasted.4 However, current EHR users acknowledge that there is a high rate of copying and pasting all elements of medical documentation, with almost a quarter of notes in more recent surveys containing a copied and pasted physical examination.3,5 Residents and younger physicians, who have never used a traditional medical record, may not realize that notes were envisioned as thoughtful descriptions of patient encounters, and that copying and pasting is generally considered taboo.4
In addition to documentation behaviors, previous authors have raised the issue of how medical trainees spend their time in the era of the EHR. In a 2013 study, interns spent 40% of their time with the computer and about 12% in direct patient care.6 It is not uncommon in the academic medical environment to encounter a medical team in a workroom. Often we can see each member typing furiously, reviewing labs, engaging in pattern recognition, working to streamline hospitalization and resource utilization, and sometimes actually using the telephone to call inpatients on their service to inform them of test results or upcoming procedures instead of walking to their rooms. This allocation of time certainly does not promote the crucial goals of empathic communication and astute clinical judgment. While authors3,7 have discussed efficient strategy associated degradation of the medical record itself, less attention is given to the downstream implications of this for trainees' development of competencies in professionalism and patient care.
Data from fields outside of medicine demonstrate that rote or copied inclusion of information in a document results in less engagement with and less critical thinking about the information at hand.8 Current EHR practices may promote a superficial assessment of the patient, and deprive our trainees of the opportunity to learn important skills needed to critically and deeply think about their patients.
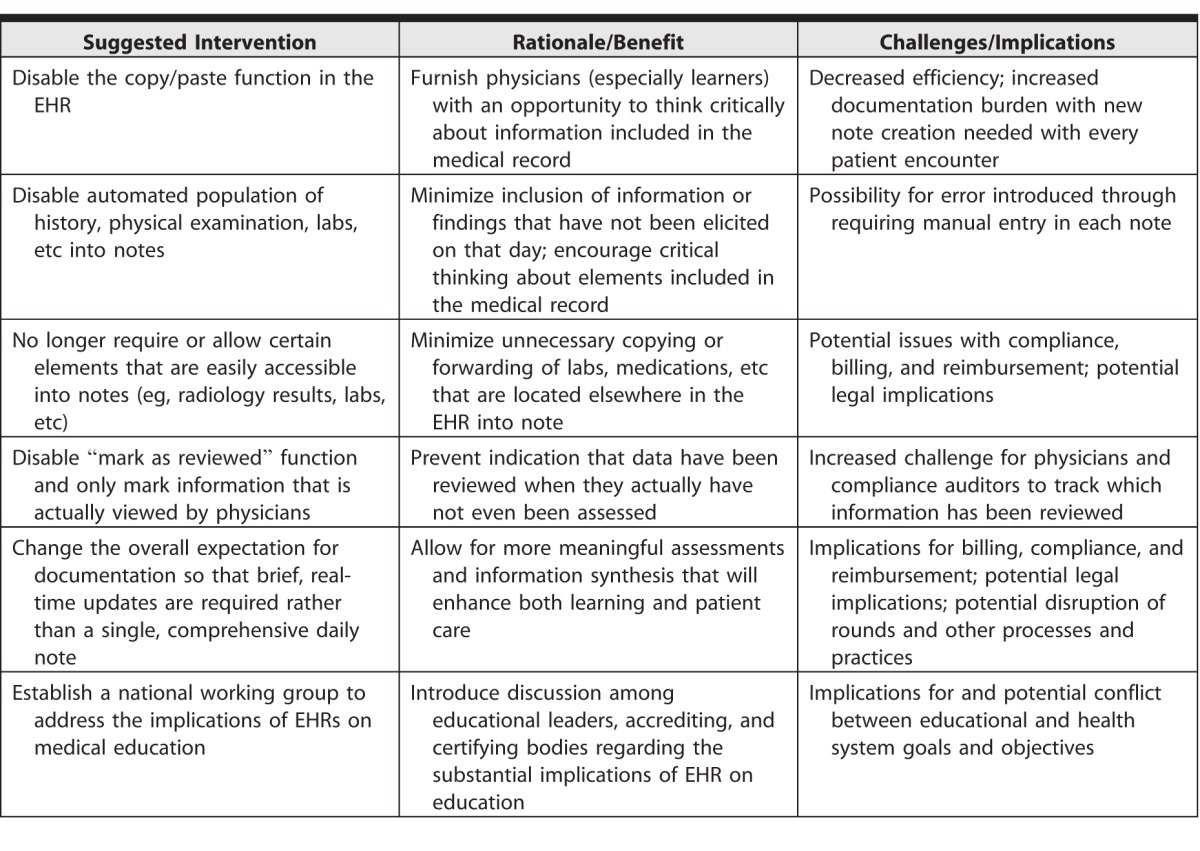
As medical educators contemplate optimal integration of the EHR into the learning environment, we must reconsider traditional notions of a patient health record and how it integrates into the practice of medicine, as suggested in the table. The most extreme intervention involves complete discontinuation of the copy/paste or note forward function, which would effectively resolve the issue of inaccurately copied information. A major concern associated with disabling copy/paste or note forward functions is the fear that note-producing efficiency would decrease, and that this would undermine physician morale. Although physicians may feel that their care is more efficient due to automated EHR functions, there are scarce data addressing the impact of documentation time, copying and pasting, or note forward on patient outcomes like emergency department visits, hospital length of stay, readmissions, etc.
Table.
Potential Next Steps, Rationale, and Implications for Optimizing Educational Use of the Electronic Health Record (EHR)
If there is to be an important role for documentation in patient care and medical education, supervisors and educators alike will need to establish its importance and insist on high standards for learners' documentation. The EHR is not a simple computerized binder, and rather than perceiving documentation as an afterthought or unimportant task that simply needs to be completed as quickly as possible, clinicians should think about ways in which communication recorded in the EHR can be optimized. If every physician resorts to shortcuts for certain information or updates, it could be that these requirements are outdated. Perhaps progress notes in the traditional sense are passé. Perhaps physicians should be required to update obligatory fields, create original physical examinations without the use of templates, and incorporate labs in a way that demonstrates thought and consideration of the values, with a requirement to generate a freshly prioritized problem list, assessment, and plan for every encounter.
In considering the educational impact of current practices with the EHR, it is necessary to ponder some difficult questions. Will it be acceptable to have a generation of trainees who may never learn how to dose or schedule medications because the EHR provides that information at the click of a button? Should our learners and future health care professionals be adopting the habit of providing care remotely to inpatients, without the additional benefit of physically assessing the patient? Will safety benefits in the present ultimately come at the expense of current trainees' ability in the future to remember nuanced details of patient interactions or their recollection of an atypical presentation detected by a physical examination?
The questions we pose are not easily answered, particularly in light of the many other pressures facing not only medical education, but also health care in general. While there is no “copy forward” function that can create a simple solution to these challenges, we as educators must accept the responsibility to disable problematic practices, develop a set of acceptable standards, and create minimum expectations that satisfy patient care needs today, while also promoting professionalism, accountability, and patient care in the future. In proposing concrete suggestions, we hope to start a meaningful conversation that will help medical educators develop and assess strategies to embrace and adapt, rather than resist, the integration of technology into our constantly changing educational environment.
References
- 1. Fields SA, Morrison E, Yoder E, Krane K, Agresta T, Esham R, et al. Clerkship directors' perceptions of the impact of HCFA documentation guidelines. Acad Med. 2002; 77 6: 543– 546. [DOI] [PubMed] [Google Scholar]
- 2. Verghese A. Culture shock—patient as icon, icon as patient. N Engl J Med. 2008; 359 26: 2748– 2751. [DOI] [PubMed] [Google Scholar]
- 3. Hirschtick RE. A piece of my mind. Copy-and-paste. JAMA. 2006; 295 20: 2335– 2336. [DOI] [PubMed] [Google Scholar]
- 4. O'Donnell HC, Kaushal R, Barrón Y, Callahan MA, Adelman RD, Siegler EL. Physicians' attitudes towards copying and pasting in electronic note writing. J Gen Intern Med. 2008; 24 1: 63– 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ibach B, Stewart D, Chang R, Laing T. Epidemiology of copy and pasting in the medical record at a tertiary care academic medical center [abstract]. J Hosp Med. 2012. ;7(suppl 2). http://www.shmabstracts.com/abstract/epidemiology-of-copy-and-pasting-in-the-medical-record-at-a-tertiarycare-academic-medical-center. Accessed February 3, 2016. [Google Scholar]
- 6. Block L, Habicht R, Wu AW, Desai SV, Wang K, Silva KN, et al. In the wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med. 2013; 28 8: 1042– 1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thielke S, Hammond K, Helbig S. Copying and pasting of examinations within the electronic medical record. Int J Med Inform. 2007; 76 suppl 1: 122– 128. [DOI] [PubMed] [Google Scholar]
- 8. Morgan M, Brickell G, Harper B. Applying distributed cognition theory to the redesign of the “copy and paste” function in order to promote appropriate learning outcomes. Comput Educ. 2006; 50 1: 125– 147. [Google Scholar]


