Abstract
To provide a national, population-based assessment of the quality of the health care system for children and youth with special health care needs using a framework of six health care system quality indicators. 49,242 interviews with parents of children with special health care needs from the 2009–10 National Survey of Children with Special Health Care Needs (NS-CSHCN) were examined to determine the extent to which CSHCN had access to six quality indicators of a well-functioning system of services. Criteria for determining access to each indicator were established and applied to the survey data to estimate the proportion of CSHCN meeting each quality indicator by socio-demographic status and functional limitations. 17.6 % of CSHCN received care consistent with all six quality indicators. Results for each component of the system quality framework ranged from a high of 70.3 % of parents reporting that they shared decision-making with healthcare providers to a low of 40 % of parents reporting receipt of services needed for transition to adult health care. Attainment rates were lower for CSHCN of minority racial and ethnic groups, those residing in households where English was not the primary language, those in lower income households, and those most impacted by their health condition. Only a small proportion of CSHCN receive all identified attributes of a high-quality system of services. Moreover, significant disparities exist whereby those most impacted by their conditions and those in traditionally disadvantaged groups are served least well by the current system. A small proportion of CSHCN appear to remain essentially outside of the system, having met few if any of the elements studied.
Keywords: Children with special health care needs, Health care quality, Systems of care, Access, Disparities
Introduction
Once considered to represent a relatively small population of children with complex medical conditions, the term “children with special health care needs” has come to represent a much broader constituency of children and youth as public health policy has evolved to recognize the importance of prevention, early detection and intervention for a wider range of conditions and risk factors. Now defined by the federal Maternal and Child Health Bureau (MCHB) as those who “have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally” [1], children and youth with special health care needs (YSHCN) represent a broad and growing constituency of health care consumers. Data from multiple national surveys suggest that the prevalence of CSHCN has increased during the past decade and now represents approximately 15–18 % of children less than 18 years of age in the United States [2, 3].
Meeting the needs of this growing population has historically been complicated by a fragmented health care system resulting in poorly coordinated and episodic care [4], [5]; the presence of inequities in access and receipt of care [6]; a need for a more prominent role in decision-making for families and caregivers (7; and a need for improved patient self-management and decision-making [7].
During the past 15 years, with the increasing momentum of health care reform, quality improvement methodology, and practice transformation, a system-based approach has evolved as the foundation for improving the health and well-being of children with special health care needs and their families [8, 9]. In 2000, the Health Resources and Services Administration’s (HRSA) MCHB worked with State Title V CSHCN programs, families, providers, researchers, and other stakeholders, to operationalize six quality indicators of a well-functioning system of services for CSHCN, and launched the National Survey of Children with Special Health Care Needs (NS-CSHCN) to assess the status of these indicators nationally and at the state level. These indicators are as follows: 1. Families of CSHCN partner in health care decision-making; 2. CSHCN receive coordinated, ongoing, comprehensive care within a medical home; 3. Families of CSHCN have adequate private and/or public insurance to pay for needed services; 4. Children are screened early and continuously for special health care needs; 5. Community-based services are organized so families can use them easily; and 6. CSHCN receive services necessary to make transitions to adult health care.
These indicators are reported annually by all state Title V Programs, and are incorporated in national guidelines such as the National Committee for Quality Assurance (NCQA), Healthy People 2020, the National Quality Forum (NQF), and Bright Futures, a national health promotion initiative of the American Academy of Pediatrics (AAP) [10–14].
The objective of this study is to utilize data from the 2009–10 NS-CSHCN to provide an otherwise unavailable national, population-based, assessment of the system of services for children and YSHCN using the six quality system indicators.
Study Data and Methods
The NS-CSHCN is a cross-sectional survey first conducted in 2001 and repeated in 2005–06. Data from the third iteration, conducted from July 2009 to March 2011, provide the basis for this study. A total of 371,617 children were screened for special needs using the CSHCN Screener [15], and 40,242 interviews were completed for children identified with special needs over the 2 years of survey data collection. The interview completion rate for households known to contain CSHCN was 80.8 %. The overall response rate, including deductions for telephone numbers that ring with no answer or are always busy was 26 %. Details concerning the survey methodology and data quality evaluations are presented elsewhere [16]. Additional information about the methodology and NS-CSHCN survey items can be found at http://www.cdc.gov/nchs/slaits/cshcn.htm.
The survey questionnaire included items on health and functional status, need and receipt of health care services, and measures of the impact of children’s health conditions on the family. Measurable criteria for judging success in attaining each of the six quality indicators were established and questionnaire items designed to measure these criteria were incorporated into the NS-CSHCN. Data from the NS-CSHCN were then used to assess the percent of CSHCN meeting each quality indicator. The methods used to calculate success rates for the quality indicators and the systems goal are presented elsewhere [17, 18]. The quality assessment strategy utilized in this study is unique in that it reports on experiences and perceptions of families of CSHCN. As such, the survey provides a nationally representative, consumer-based mechanism for assessing quality of care from the family perspective.
Although three editions of the NS-CSHCN have now been fielded over the past decade, revisions designed to improve the validity of questionnaire items used to measure the quality indicators, as well as a change in the sample design to incorporate cell phone only households for the first time in 2009–10, effectively preclude methodologically sound comparisons over time. Hence, the findings in this report are limited to the 2009–10 national survey data, the most current data available.
The survey data were weighted to reflect population totals for non-institutionalized children nationally and at the state level. All analyses were performed using SUDAAN [19], a software package that accounts for the complex sample design of the NS-CSHCN. Data were multiply imputed for cases with missing values for race and ethnicity, family income (expressed as a percentage of the federal poverty guidelines), or primary household language Urban/rural comparisons were conducted using data files obtained under an agreement with NCHS. Unless otherwise specified, all comparisons reported in the text were statistically significant at the<0.05 level.
Study Findings
Overall, 15.1 % of children younger than 18 years, or 11.2 million US children, were estimated to have a special health care need during 2009–10. Below we describe the proportion of CSHCN meeting the quality indicators individually and collectively, and we assess the extent to which disparities are present in meeting the quality indicators. Table 1 lists the six quality indicators and their components; provides an estimate of the proportion of CSHCN having access to each component; and indicates the proportion of CSHCN meeting all six indicators as a proxy for receipt of care in a high quality service system (i.e., the overall system goal). Table 2 provides unadjusted proportions of CSHCN having access to each quality indicator by selected socio-demographic and other factors.
Table 1.
Percentage of children with special health care needs (CSHCN) meeting the criteria for a system of services by the six quality indicators, components and sub-components: US, 2009–2010
| Valid N | National percent
|
Confidence interval 95 % | ||
|---|---|---|---|---|
| (%) | (SE) | |||
| Quality indicator 1: families of CSHCN are partners in decision-making | 39,876 | 70.3 | 0.44 | (69.4–71.1) |
| Doctors usually or always discuss range of optionsa | 40,094 | 81.7 | 0.38 | (81.0–82.5) |
| Doctors usually or always encourage questionsa | 40,044 | 81.4 | 0.38 | (80.6–82.1) |
| Doctors usually or always make it easy to ask questionsa | 40,088 | 86.2 | 0.36 | (85.5–86.9) |
| Doctors usually or always consider and respect family’s choicesa | 40,010 | 84.4 | 0.37 | (83.7–85.1) |
| Quality indicator 2: CSHCN receive care within a medical home | 38,950 | 43.0 | 0.45 | (42.1–43.9) |
| Child has a usual source of care | 40,100 | 89.3 | 0.29 | (88.7–89.9) |
| Child has a usual source for sick care | 40,164 | 90.5 | 0.28 | (90.0–91.0) |
| Child has a usual source for preventive care | 40,167 | 96.7 | 0.17 | (96.3–97.0) |
| Child has a personal doctor or nurse | 40,186 | 93.1 | 0.24 | (92.6–93.6) |
| Child has no problems obtaining referrals when neededb | 13,274 | 76.6 | 0.72 | (75.2–78.0) |
| Child receives effective care coordinationc | 29,845 | 56.0 | 0.53 | (54.9–57.0) |
| Family is very satisfied with doctors’ communication with each otherc,d | 26,415 | 62.7 | 0.55 | (61.6–63.7) |
| Family is very satisfied with doctors’ communication with other programsc | 11,523 | 53.1 | 0.85 | (51.4–54.7) |
| Family usually or always gets sufficient help coordinating care, if neededc | 12,898 | 57.7 | 0.82 | (56.2–59.4) |
| Child receives family-centered carea | 39,685 | 64.6 | 0.46 | (63.7–65.5) |
| Doctors usually or always spend enough timea | 40,032 | 77.5 | 0.41 | (76.7–78.3) |
| Doctors usually or always listen carefullya | 40,073 | 87.7 | 0.34 | (87.0–88.3) |
| Doctors are usually or always sensitive to values and customsa | 39,945 | 88.9 | 0.32 | (88.2–89.5) |
| Doctors usually or always provide needed informationa | 40,058 | 82.4 | 0.38 | (81.6–83.1) |
| Doctors usually or always make the family feel like a partnera | 40,081 | 87.0 | 0.35 | (86.3–87.6) |
| Quality indicator 3: adequate private and/or public insurance | 39,720 | 60.6 | 0.46 | (59.7–61.4) |
| Child had public or private insurance at time of interview | 40,184 | 96.5 | 0.19 | (96.1–96.9) |
| Child had no gaps in coverage during the year before the interview | 40,108 | 90.7 | 0.30 | (90.1–91.3) |
| Insurance usually or always meets the child’s needse | 38,883 | 86.8 | 0.35 | (86.1–87.5) |
| Costs not covered by insurance are usually or always reasonablee | 38,752 | 71.3 | 0.42 | (70.4–72.1) |
| Insurance usually or always permits child to see needed providerse | 38,913 | 89.5 | 0.32 | (88.9–90.1) |
| Quality indicator 4: children are screened early and continuously for special health care needs | 39,877 | 78.6 | 0.39 | (77.8–79.3) |
| Child had a routine preventive medical care visit in past year | 39,990 | 90.4 | 0.27 | (89.8–90.9) |
| Child had a routine preventive dental care visit in past yearf | 39,602 | 85.9 | 0.34 | (85.2–86.5) |
| Quality indicator 5: community-based services are organized so families can use them easily | 39,990 | 65.1 | 0.45 | (64.2–66.0) |
| Child’s family experienced no difficulties or delays getting services | 40,016 | 66.2 | 0.45 | (65.3–67.0) |
| No difficulties or delays due to lack of eligibility for services | 40,151 | 89.2 | 0.33 | (88.5–89.8) |
| No difficulties or delays due to lack of availability of services | 40,162 | 88.8 | 0.32 | (88.1–89.4) |
| No difficulties or delays due to problems with appointments | 40,202 | 82.2 | 0.38 | (81.4–82.9) |
| No difficulties or delays because of issues related to cost | 40,213 | 85.1 | 0.35 | (84.4–85.7) |
| No difficulties or delays due to trouble getting needed information | 40,209 | 91.0 | 0.28 | (90.4–91.5) |
| No difficulties or delays due to other reasonsg | 28,177 | 97.0 | 0.20 | (96.6–97.4) |
| Child’s family was never or only sometimes frustrated when trying to get services for the child | 36,977 | 90.2 | 0.32 | (89.6–90.8) |
| Quality indicator 6: children with special health care needs receive services necessary to make transitions to adult health care | 16,222 | 40.0 | 0.69 | (38.7–41.4) |
| Child receives anticipatory guidance in the transition to adulthoodh | 13,669 | 36.8 | 0.74 | (35.4–38.3) |
| Doctors have discussed shift to adult provider, if necessaryh | 4,606 | 43.9 | 1.36 | (41.2–46.6) |
| Doctors have discussed future health care needs, if necessaryh | 12,359 | 59.0 | 0.83 | (57.4–60.6) |
| Doctors have discussed future insurance needs, if necessaryh | 10,413 | 35.1 | 0.86 | (33.4–36.8) |
| Child has usually or always been encouraged to take responsibility for his/her health care needsh | 17,050 | 78.0 | 0.60 | (76.8–79.1) |
| CSHCN meeting all age appropriate quality indicators | 37,252 | 17.6 | 0.34 | (16.9–18.2) |
Source: author’s analysis of the 2009/2010 National Survey of Children with Special Health Care Needs
Valid n = unweighted sample size with non-missing data
SE standard error
This component was ascertained only for CSHCN with one or more doctor visits during the previous 12 months
This component was ascertained only for CSHCN who needed a referral during the previous 12 months to see a doctor or receive a service
Care coordination was ascertained for CSHCN who used more than one type of health care service during the previous 12 months. Specific types of health care services included routine preventive care; specialty care; preventive dental care; other dental care; prescription medicine; physical, occupational, or speech therapy; mental health care; substance abuse treatment; home health care; eyeglasses or vision care; hearing aids or hearing care; mobility aids; communication aids; durable medical equipment; early intervention services; and special educational services
Communication with other health care professionals is reported only for CSHCN who used specialty care; physical, occupational, or speech therapy; mental health care; substance abuse treatment; and/or home health care during the previous 12 months
Adequacy of insurance was ascertained only for CSHCN with insurance at the time of the interview
Preventive dental care is reported only for CSHCN who were 1 year of age or older at the time of the survey
Difficulties or delays due to other reasons was ascertained only for CSHCN who did not have other reported difficulties or delays
The transition Quality indicator was ascertained for CSHCN who were 12 years of age or older at the time of the survey. Need for anticipatory guidance was assumed if a discussion occurred or the parent indicated that a discussion would have been helpful
Table 2.
Unadjusted proportion of cshcn with quality indicators and systems goal met by selected sociodemographic and other selected factors: US, 2009–2010
| Quality indicator 1: families of CSHCN are partners in decision-making (n = 39,876)
|
Quality indicator 2: receive Care within a medical home (n = 38,950)
|
Quality indicator 3: adequate private and/or public insurance (n = 39,720)
|
Quality indicator 4: early and continuous screening for special health care needs (n = 39,877)
|
Quality indicator 5: services organized for ease of use (n = 39,990)
|
Quality indicator 6: effective transition planning for adult health care (n = 16,222)
|
All Age appropriate quality indicators met (n = 37,252)
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | SE | p | % | SE | p | % | SE | p | % | SE | p | % | SE | p | % | SE | p | % | SE | p | |
| Total | 70.3 | 0.44 | 43.0 | 0.45 | 60.6 | 0.46 | 78.6 | 0.39 | 65.1 | 0.45 | 40.0 | 0.69 | 17.6 | 0.34 | |||||||
| Gender | 0.026 | 0.276 | 0.382 | 0.675 | 0.436 | <0.001 | 0.906 | ||||||||||||||
| Male | 69.5 | 0.58 | 42.6 | 0.58 | 60.2 | 0.59 | 78.5 | 0.50 | 65.4 | 0.58 | 37.1 | 0.88 | 17.6 | 0.44 | |||||||
| Female | 71.5 | 0.68 | 43.6 | 0.72 | 61.1 | 0.71 | 78.8 | 0.61 | 64.7 | 0.72 | 43.8 | 1.08 | 17.5 | 0.52 | |||||||
| Age | 0.306 | 0.235 | 0.007 | <0.001 | 0.634 | NA | <0.001 | ||||||||||||||
| 0–5 | 70.4 | 0.98 | 44.2 | 1.04 | 63.2 | 1.02 | 64.8 | 1.01 | 65.9 | 0.99 | NA | 18.2 | 0.81 | ||||||||
| 6–11 | 69.5 | 0.73 | 42.1 | 0.73 | 60.3 | 0.74 | 83.8 | 0.54 | 64.8 | 0.74 | NA | 21.2 | 0.57 | ||||||||
| 12–17 | 71.0 | 0.66 | 43.1 | 0.69 | 59.4 | 0.70 | 80.6 | 0.58 | 65.0 | 0.69 | 40.0 | 0.69 | 13.6 | 0.45 | |||||||
| Race/ethnicity | <0.001 | <0.001 | <0.001 | 0.005 | <0.001 | <0.001 | <0.001 | ||||||||||||||
| Hispanic | 63.4 | 1.34 | 33.0 | 1.33 | 53.7 | 1.40 | 74.9 | 1.22 | 59.2 | 1.38 | 25.3 | 2.13 | 11.7 | 0.91 | |||||||
| Non-hispanic white | 74.2 | 0.47 | 48.7 | 0.52 | 62.9 | 0.50 | 79.6 | 0.43 | 67.6 | 0.49 | 45.6 | 0.79 | 20.4 | 0.42 | |||||||
| Non-hispanic black | 64.6 | 1.31 | 33.6 | 1.20 | 58.8 | 1.33 | 78.8 | 1.07 | 64.0 | 1.33 | 28.2 | 1.81 | 13.5 | 0.83 | |||||||
| All other non-hispanic | 67.0 | 1.71 | 39.3 | 1.67 | 61.3 | 1.69 | 78.7 | 1.35 | 61.0 | 1.71 | 40.3 | 2.75 | 16.3 | 1.24 | |||||||
| Primary language in home | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | <0.001 | <0.001 | ||||||||||||||
| English | 71.1 | 0.45 | 44.2 | 0.46 | 61.5 | 0.46 | 79.6 | 0.38 | 65.7 | 0.45 | 41.3 | 0.69 | 18.3 | 0.35 | |||||||
| Non-English | 58.7 | 2.18 | 25.4 | 2.05 | 47.8 | 2.26 | 64.8 | 2.22 | 57.9 | 2.25 | 17.1 | 3.44 | 6.4 | 0.93 | |||||||
| Location | 0.060 | 0.012 | 0.023 | <0.001 | 0.980 | 0.248 | 0.377 | ||||||||||||||
| Urban | 70.0 | 0.51 | 42.7 | 0.52 | 60.2 | 0.53 | 79.5 | 0.44 | 65.2 | 0.52 | 40.3 | 0.78 | 17.7 | 0.39 | |||||||
| Rural | 71.8 | 0.83 | 44.3 | 0.89 | 62.5 | 0.87 | 75.0 | 0.79 | 65.1 | 0.85 | 38.5 | 1.39 | 17.1 | 0.65 | |||||||
| Family income | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||
| <100 % FPL | 61.7 | 1.02 | 30.9 | 0.97 | 57.8 | 1.05 | 73.2 | 0.96 | 59.4 | 1.04 | 25.3 | 1.59 | 11.1 | 0.69 | |||||||
| 100–199 % FPL | 67.5 | 1.05 | 37.7 | 1.03 | 58.1 | 1.08 | 75.1 | 0.94 | 59.3 | 1.08 | 31.1 | 1.53 | 13.7 | 0.70 | |||||||
| 200–399 % FPL | 72.3 | 0.84 | 47.2 | 0.87 | 58.3 | 0.83 | 78.5 | 0.74 | 65.6 | 0.83 | 43.4 | 1.29 | 17.6 | 0.65 | |||||||
| ≥400 % FPL | 77.4 | 0.76 | 52.3 | 0.83 | 67.0 | 0.78 | 85.8 | 0.57 | 73.9 | 0.73 | 52.2 | 1.22 | 25.6 | 0.70 | |||||||
| Impact on activitiesa | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||
| Never affected | 79.3 | 0.68 | 55.5 | 0.78 | 70.0 | 0.73 | 80.9 | 0.61 | 80.4 | 0.67 | 52.0 | 1.16 | 26.6 | 0.66 | |||||||
| Somewhat/moderately | 68.8 | 0.69 | 42.4 | 0.72 | 58.2 | 0.72 | 79.2 | 0.60 | 65.0 | 0.70 | 39.2 | 1.10 | 15.5 | 0.50 | |||||||
| Always/usually | 61.1 | 0.94 | 27.7 | 0.81 | 52.0 | 0.95 | 75.0 | 0.83 | 45.9 | 0.94 | 25.5 | 1.21 | 8.8 | 0.51 | |||||||
Source Author’s Analysis of the 2009/2010 National Survey of Children with Special Health Care Needs
Impact on activities was ascertained from two questions about how often the child is affected in his/her ability to do things that other children his/her age can do and the extent to which his/her ability to do things is affected
How Often Does Care Provided to CSHCN Meet Quality Standards?
Quality indicator #1: Partnerships in decision-making This quality indicator measures the extent to which families share in decision-making with their children’s providers and was operationalized using the four components presented in Table 1. Overall, 70.3 % of CSHCN nationally met all components for this quality indicator during 2009–10.
Quality indicator #2: Coordinated, ongoing, comprehensive care within a medical home This quality indicator was operationalized by five components. An estimated 43.0 % of CSHCN successfully met all components of the medical home quality indicator (Table 1).
Quality indicator #3: Adequate private and/or public insurance to pay for needed services This quality indicator was operationalized using five components that address presence, continuity and adequacy of insurance coverage. Overall, 60.6 % of CSHCN met all components of the health insurance quality indicator in 2009–10.
Quality indicator #4: Screening early and continuously for special health care needs This quality indicator was measured using two components: receipt of at least one preventive medical visit and at least one preventive dental examination during the previous year. Together, 78.6 % of children met both components of this quality indicator.
Quality indicator #5: Organization of community-based service systems so families can use them easily This quality indicator was assessed based on respondent assessment of difficulties in obtaining services in two areas: difficulties and delays, and frustration. Taken together, 65.1 % of CSHCN met both components of the quality indicator in 2009–10.
Quality indicator #6: Receipt of services necessary for youth with special health care needs to make transitions to adult health care This quality indicator was operationalized using two components reflecting receipt of anticipatory guidance and encouragement by the child’s health care providers to take on self-care responsibilities. Because most transition issues occur as youth approach adulthood, the reference population for this quality indicator is restricted to YSHCN aged 12–17 years. An estimated 40.0 % of all YSHCN met all relevant components of the transition quality indicator in 2009–10.
When children receive care that meets all of the quality indicators appropriate for their age (5 quality indicators and up to 30 component measures for children under 12 years, and 6 quality indicators and up to 34 component measures for children 12–17 years), they can be thought of as receiving care in a high quality system of services. During 2009–10, 17.6 % of CSHCN received care consistent with all age-appropriate quality indicators and could thus be considered as receiving care in a high quality system.
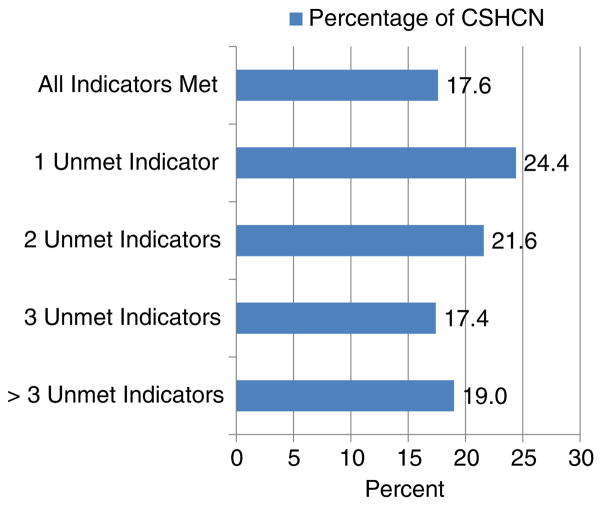
Figure 1 shows the percent of CSHCN at various thresholds of achieving all age-appropriate quality indicators. Overall, 82 % of CSHCN do not meet one or more of the quality indicators. The group with the farthest to go— those with four or more unmet quality indicators—represented slightly less than one in five children (19.0 %). Conversely, the group experiencing the smallest gap— those missing only one indicator—represented one in four children (24.4 %).
Fig. 1.
Percent distribution of the number of age appropriate quality indicators met by CSHCN aged 0–17 years
Rates of success vary across the quality indicators and the overall systems goal by demographic characteristics, socioeconomic status, and functional status. Results presented in Table 2 show a consistent pattern across the individual quality indicators and the overall system goal, whereby success rates tend to be lower for children in traditionally disadvantaged circumstances, including those in minority racial and ethnic groups, those residing in households where English was not the primary language, those in lower income households (relative to the federal poverty level), and those whose conditions have greater impact on their activities. Although attenuated in some cases, significant disparities by race/ethnicity, primary household language, poverty status and functional status remained after adjustment for possible confounding using multivariable logistic regression (results not shown; available from the authors).
Discussion
The findings of this study have significant implications for CSHCN and the broader system of health care delivery. The growing population of CSHCN over the past decade creates an obvious challenge to health care reform with its goals of improving population health, enhancing the experience and quality of care, and lowering costs [20]. Without a substantially different approach to providing health care, the number of children reaching adulthood with avoidable secondary chronic conditions and disproportionately large expenditures may continue to grow [21]. Experts agree that, in order to transform the way health care is organized and delivered, payment reform is necessary to fully implement models such as the medical home [20–24]. Although payment reform models are emerging [11, 25, 26] payment incentives for providers to change the way they deliver care, especially around the elements being measured in this study (i.e. medical home, care coordination, and transition to adult health care are not yet well established.
Emerging research suggests that a life course approach to health care might provide a perspective better suited to minimizing poor health outcomes. This approach, described in detail in a special issue of this journal, (http://link.springer.com/journal/10995/18/2/page/1, suggests that children’s health and functioning are influenced not only by the health care provider, but by families, communities, and the broader system of services, and that by addressing health risks earlier in life and during developmentally sensitive periods, it may be possible to maximize the benefit of health care expenditures and assure more optimal health outcomes [27, 28]. Benefits for CSHCN in this model of care might be expected to include earlier identification of special health care needs, minimizing the impact and severity of chronic conditions in childhood and into adulthood, and promoting general health and well-being [29]. Because average health care expenditures for CSHCN are significantly higher than those for typically developing children [30], the short term health care costs incurred in implementing a life course approach will be commensurately higher but so too should the long term savings.
Consistent with previous studies, we found that significant disparities persist for CSHCN in racial and ethnic minority groups; children in poverty; and those most impacted by their conditions [6]. These children, historically left behind by the current system, remain at high risk even in a reformed health care system. Provisions included in the Children’s Health Insurance Program Reauthorization Act (CHIPRA) and the Affordable Care Act (ACA) provide strategies to address this issue. Policymakers expect that the provisions of this legislation, implemented systematically, will have a dramatic effect on the adequacy of insurance coverage, access to the medical home, and, more generally, the quality of health care [31].
Significant differences in attainment rates exist within and across the six quality indicators, differences that are important to recognize and understand in the planning and delivery of health care for this population of children. Numerous national efforts have emerged to define, standardize and improve the application of these indicators. For example, in its ongoing quality improvement work with experts in both pediatric and adult health care settings, the National Committee on Quality Assurance (NCQA) has recently updated its standards for medical home recognition, and begun to incorporate other quality elements important for CSHCN, such as placing more emphasis on team based and integrated care and integration of behavioral health. Many insurers pay higher reimbursement rates to practices that have earned NCQA recognition for the Patient-centered Medical Home [32]. Likewise, the NQF, the nation’s repository for endorsed measures of health care quality, now includes multiple measures reflecting these six quality indicators, including a measure of health care transition for youth 12–17 years with special health care needs [13]. These prominent national efforts can provide a structure for quality improvement at the system as well as the individual level.
Improving performance on health care system elements that are important for CSHCN has the potential to increase the efficiency and quality of care and perhaps reduce the cost of health care for CSHCN. For example, family-professional partnership and shared decision-making are associated with improved health outcomes for CSHCN [33–35]. Developed early on, these relationships can provide the groundwork for enhanced patient engagement and shared decision-making in later years. Emerging quality improvement structures, such as the medical home, provide an important opportunity to incorporate patient/family/caregiver experience of care into the design and delivery of health care for children and youth with special health care needs. A further consideration might be to align these structures with population-based surveys such as this survey and the National Survey of Children’s Health (NSCH).
Likewise, the medical home with its focus on comprehensive and coordinated care is associated with improved health outcomes for CSHCN as well as typically developing children [36–38]. Yet, less than half of the CSHCN population has access to all of the components of a medical home. Planners and policymakers focused on redesign of the health care system can benefit from the knowledge that, although most CSHCN have a usual source of care, effective care coordination represents a systemic weakness for this population, despite growing evidence of its value [39].
Adequate insurance is an essential component of a high-quality system of services. Past studies have demonstrated the salutatory effects of adequate insurance for CSHCN, including reduced rates of unmet health needs, fewer problems receiving referrals, and fewer financial problems related to health care expenses [40]. Adequate insurance is also associated with higher likelihood of having a usual source of care and a personal doctor or nurse [41]. While only 60.6 % of CSHCN had adequate insurance at the time of this study, provisions in the ACA, including eliminating lifetime benefit caps on coverage and requiring certain preventive services without co-pays, may increase the proportion of CSHCN with adequate insurance [31].
The finding that less than half of youth aged 12–17 with special health care needs received adequate transition planning from their pediatric health care provider is of concern. Transition from pediatric to adult models of health care is recognized as an important issue for all youth, especially YSHCN, and is considered a standard of care by the AAP, American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) [42].
The findings of this study indicate that only a small proportion of CSHCN are currently served by a system that meets all of the quality indicators for a well-functioning system. However, for a large proportion, most of the quality indicators are in place. This finding is encouraging and suggests that strategic intervention might be targeted to those areas most likely to raise the proportion of CSHCN meeting the overall systems goal. Nonetheless, a small proportion of CSHCN appear to remain essentially outside of the system, having met few if any of the elements studied. Even with implementation of the ACA, other efforts including targeted outreach, culturally competent strategies, and innovative delivery models may be required.
This study has several limitations. The estimate of the proportion of CSHCN receiving care in a high quality system of services is not measured directly but rather is derived indirectly based on the extent to which all six quality indicators are attained for the population. The assessment of whether received care meets established criteria is based on parent report, which, while considered to be a strength of the approach, represents only one perspective. A truly comprehensive approach would incorporate the perspectives of other participants in the health care system, including health care providers and youth themselves. Finally, different methods exist to measure child health care quality for CSHCN. Utilizing other methods and/or fewer questions might have produced a higher success rate.
In summary, only a small proportion of CSHCN receive all identified attributes of a high-quality system of services. Moreover, significant disparities exist whereby those most impacted by their conditions are served least well by the current system. Recognizing these issues, states are beginning to transform health care delivery systems to try to improve quality, health outcomes, and to reduce the cost of care. New models exist for organizing and delivering health care, including those supported by the Centers for Medicaid and Medicare Services through CHIPRA and the Center for Innovative Strategies. These models hold great promise for informing both practice and policy. The challenge remains to assure that all children, especially CSHCN, are served in a high-quality system of services designed to address and minimize the adverse impact of existing health conditions while maximizing health and well-being into and throughout adulthood.
Contributor Information
Bonnie B. Strickland, Email: bstrickland@hrsa.gov, Maternal and Child Health Bureau, Health Resources and Services Administration, Rockville, MD, USA
Jessica R. Jones, Email: jjones@hrsa.gov, Maternal and Child Health Bureau, Health Resources and Services Administration, Rockville, MD, USA
Paul W. Newacheck, Email: Paul.Newacheck@ucsf.edu, University of California San Francisco, San Francisco, CA, USA
Christina D. Bethell, Email: cbethell@cahmi.org, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
Stephen J. Blumberg, Email: Swb5@CDC.GOV, National Center for Health Statistics, Centers for Disease Control and Prevention, Hyattsville, MD, USA
Michael D. Kogan, Email: mkogan@hrsa.gov, Maternal and Child Health Bureau, Health Resources and Services Administration, Rockville, MD, USA
References
- 1.McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck P, et al. A new definition of children with special health care needs. Pediatrics. 1998;102(1):137–140. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- 2.Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood conditions in the United States. JAMA. 2007;297(24):2755–2759. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- 3.Bethell CD, Read D, Blumberg SJ, Newacheck PW. What is the prevalence of children with special health care needs? Maternal and Child Health Journal. 2008;12(1):1–14. doi: 10.1007/s10995-007-0220-5. [DOI] [PubMed] [Google Scholar]
- 4.Mangione-Smith R, DeCristofara AH, Setodji CM, Keesey J, Klein DJ, Adams JL, et al. The quality of ambulatory care delivered to children in the United States. New England Journal of Medicine. 2007;357(15):1515–1523. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 5.National Research Council Institute of Medicine. Children’s health, the nation’s wealth: Assessing and improving child health. Committee on evaluation of children’s health. Washington (DC): The National Academies Press; 2004. [Google Scholar]
- 6.Strickland B, van Dyck P, Kogan M, Lauver C, Blumberg S, Bethell C, et al. Assessing and ensuring a comprehensive system of services for children with special health care needs: A public health approach. American Journal of Public Health. 2011;101(2):224–231. doi: 10.2105/AJPH.2009.177915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington (DC): The National Academies Press; 2001. [PubMed] [Google Scholar]
- 8.Perrin JM, Romm D, Bloom SR, Homer CJ, Kuhlthau KA, Cooley C. A family-centered, community-based system of services for children and youth with special health care needs. Archives of Pediatrics and Adolescent Medicine. 2007;161(10):933–935. doi: 10.1001/archpedi.161.10.933. [DOI] [PubMed] [Google Scholar]
- 9.Omnibus Reconciliation Act of 1989 (Public Law 101-239) [Accessed 27 Apr 2014]; http://www.ssa.gov/OP_Home/ssact/title05/0501.htm.
- 10.US Department of Health and Human Services. [Accessed 30 Mar 2014];Title V Maternal and Child Health Block Grant to States Program, Title V Information System (TVIS) https://mchdata.hrsa.gov/tvisreports.
- 11.National Committee for Quality Assurance. Physician practice connections: Patient-Centered Medical Home: Standards and guidelines. Washington, DC: National Committee for Quality Assurance; 2008. [Google Scholar]
- 12.US Department of Health and Human Services. Healthy people 2020. Washington, D.C: [Accessed on 27 Apr 2014]. http://www.healthypeople.gov/2020/ [Google Scholar]
- 13.National Quality Forum. NQF Endorsed Standards for Children’s Health. Washington D.C: [Accessed on 27 Apr 2014]. http://www.qualityforum.org. [Google Scholar]
- 14.Hagan JF, Shaw JS, Duncan PM, editors. Bright futures: Guidelines for health supervision of infants, children, and adolescents. 3. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 15.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: Development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2:38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 16.Blumberg SJ, Welch EM, Chowdhury SR, Upchurch HL, Parker EK, Skalland BJ. Design and operation of the national survey of children with special health care needs, 2005–2006. National Center for Health Statistics Vital Health Stat. 2008;1(45):1–188. [PubMed] [Google Scholar]
- 17.McPherson M, Weissman G, Strickland BB, van Dyck PC, Blumberg SJ, Newacheck PW. Implementing community-based systems of services for children and youth with special health care needs: How well are we doing? Pediatrics. 2004;113(5 suppl):S1538–S1544. [PubMed] [Google Scholar]
- 18.Strickland BB, van Dyck PC, Kogan MD, Lauver C, Blumberg SJ, Bethell CD, et al. Assessing and ensuring a comprehensive system of services for children with special health care needs: A public health approach. American Journal of Public Health. 2011;101(2):224–231. doi: 10.2105/AJPH.2009.177915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.SUDAAN. Software for the Statistical Analysis of Correlated Data (computer program) Research Triangle Park, NC: Research Triangle Institute; 2005. Release 9.0.1. [Google Scholar]
- 20.Berwick DM, Nolan TW, Whittington J. The triple aim: Care, health and cost. Health Affairs. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Child and adolescent health and health care quality: Measuring what matters. Washington (DC): The National Academies Press; 2011. [Google Scholar]
- 22.American Academy of Pediatrics. [Accessed on 27 Apr 2014];Health Reform and the AAP: What the New Law Means for Children and Pediatricians. 2010 http://www.aap.org/en-us/advocacy-and-policy/federal-advocacy/Documents/ACAsummaryfactsheet.pdf.
- 23.National Governors Association. [Accessed on 27 Apr 2014];Effect of provider payment reforms on maternal and child health. 2013 http://www.nga.org/files/live/sites/NGA/files/pdf/2013/1305_Effect_of_Provider_Payment_Reforms_Paper.pdf.
- 24.Robert Wood Johnson Foundation. [Accessed on 27 Apr 2014];Payment matters: The ROI for Patient-Centered Medical Home payment. 2013 http://www.rwjf.org/en/research-publications/find-rwjf-research/2013/02/payment-matters-the-roi-for-payment-reform.html.
- 25.Centers for Medicare and Medicaid Services. [Accessed on 27 Apr 2014];Multi-payer advanced primary care practice. 2010 http://innovation.cms.gov/initiatives/Multi-Payer-Advanced-Primary-Care-Practice.
- 26.American Academy of Pediatrics. The medical home for children: financing principles. Elk Grove Village, IL. Committee on child health financing; 2008. [Accessed 27 Apr 2014]. http://www.aap.org/visit/MHfinanceprin.pdf. [Google Scholar]
- 27.Halfon N, Hochstein M. Life course health development: An integrated framework for developing health, policy, and research. Milbank Quarterly. 2002;80(3):433–479. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halfon N, DuPlessis H, Inkelas M. Transforming the U.S. child health system. Health Affairs. 2007;26(2):315–330. doi: 10.1377/hlthaff.26.2.315. [DOI] [PubMed] [Google Scholar]
- 29.Bethell CD, Newacheck PW, Fine A, Strickland BB, Antonelli RC, Wilhelm CL, et al. Optimizing health and health care systems for children with special health care needs using the life course perspective. Maternal and Child Health Journal. 2014;18(2):467–477. doi: 10.1007/s10995-013-1371-1. [DOI] [PubMed] [Google Scholar]
- 30.Chevarley FM. Utilization and expenditures for children with special health care needs. Agency for Healthcare Research and Quality; Rockville, Md: 2006. Research findings no. 24. http://www.meps.ahrq.gov/rf24/rf24.pdf. [Google Scholar]
- 31.National Academy for State Health Policy and the Catalyst Center. [Accessed on 27 Apr 2014];The affordable care act and children with special health care needs: An analysis and steps for state policymakers. 2011 http://www.catalystctr.org.
- 32.National Committee for Quality Assurance. New NCQA Patient-Centered Medical Home standards raise the bar. Washington, DC: National Committee for Quality Assurance; 2014. [Accessed on 27 Apr 2014]. http://www.ncqa.org/Newsroom/NewsArchive/2014NewsArchive/NewsReleaseMarch242014.aspx. [Google Scholar]
- 33.Fiks AG, Mayne S, Localio AR, Alessandrini EA, Guevara JP. Shared decision-making and healthcare expenditures among children with special healthcare needs. Pediatrics. 2012;129(1):99–107. doi: 10.1542/peds.2011-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Academy for State Health Policy. Shared decision making: advancing patient-centered care through state and federal implementation. Washington, DC: 2012. [Google Scholar]
- 35.Smalley LP, Kenney MK, Denboba D, Strickland B. Family perceptions of shared decision-making with health care providers: Results of the National Survey of Children with Special Health Care Needs 2009–10. Maternal and Child Health Journal. 2013 doi: 10.1007/s10995-013-1365-z. [DOI] [PubMed] [Google Scholar]
- 36.American Academy of Family Physicians; American Academy of Pediatrics; American College of Physicians; American Osteopathic Association. [Accessed on 27 Apr 2014];Joint Principles of the Patient-Centered Medical Home. 2007 http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf.
- 37.Homer CJ, Klatka K, Romm D, Kuhlthau K, Bloom S, Newacheck P, et al. A review of the evidence for the medical home for children with special health care needs. Pediatrics. 2008;122(4):922–937. doi: 10.1542/peds.2007-3762. [DOI] [PubMed] [Google Scholar]
- 38.Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: Health care access and impact for children and youth in the United States. Pediatrics. 2011 doi: 10.1542/peds.2009-3555. [DOI] [PubMed] [Google Scholar]
- 39.Turchi RM, Berhane Z, Bethell C, Pomponio A, Antonelli R, Minkovitz CS. Care coordination for CSHCN: Associations with family-provider relations and family/child outcomes. Pediatrics. 2009;124(Suppl):428–434. doi: 10.1542/peds.2009-1255O. [DOI] [PubMed] [Google Scholar]
- 40.Honberg LE, Kogan MD, Allen D, Strickland BB, Newacheck PW. Progress in ensuring adequate health insurance for children with special health care needs. Pediatrics. 2009;124(5):1273–1289. doi: 10.1542/peds.2009-0372. [DOI] [PubMed] [Google Scholar]
- 41.Kogan MD, Newacheck PW, Blumberg SJ, Ghandour RM, Singh GP, Strickland BB, et al. Underinsurance among children in the United States. New England Journal of Medicine. 2010;363:841–851. doi: 10.1056/NEJMsa0909994. [DOI] [PubMed] [Google Scholar]
- 42.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians. [Accessed on 27 Apr 2014];Clinical report-supporting the health care transition from adolescence to adult-hood in the medical home. http://pediatrics.aappublications.org/content/early/2011/06/23/peds.2011-0969.