Introduction
Arthrofibrosis is a rare but potentially devastating complication after anterior cruciate ligament (ACL) reconstruction with a reported incidence of 2% to 35% [3,5,6,13,18]. Prognostic factors leading to the development of arthrofibrosis are not completely understood but may include decreased preoperative range of motion, poor surgical technique with malposition of bone tunnels, or inadequate postoperative rehabilitation [6,12,13]. While early recognition is likely the most important intervention, treatment for arthrofibrosis ranges from frequent supervised physical therapy to manipulation under anesthesia and arthroscopic lysis of adhesions.
Studies to date have often reported the risk of arthrofibrosis as a function of time interval from ACL injury to surgery. For example, Shelbourne and colleagues have reported a significantly higher risk of arthrofibrosis in athletes treated surgically within one week of injury [20]. However, more recent studies have concluded that the inflammatory state of the knee is a more important determinant of arthrofibrosis risk than temporal relationships and that reconstruction performed within the first week after injury can safely be performed without increased risk of postoperative motion complications [1,6,10,13]. The risk of arthrofibrosis requiring procedural intervention after isolated ACL reconstruction has not been well defined and is likely changing with time [10,13]. Studies to date comprised of mainly referral patients at tertiary care centers and do not necessarily reflect the true population incidence of arthrofibrosis. Furthermore, many have reported the rate of motion complications alone after ACL reconstruction without indicating the burden of patients who require procedural intervention.
With this background, the purpose of this observational study was to describe the risk and predictors of arthrofibrosis (as defined by manipulation under anesthesia or surgical lysis of adhesions) in a large population-based cohort. Specifically, this study sought to 1) report a population-based incidence of arthrofibrosis following ACL injury and reconstruction, 2) identify risk factors associated with development of arthrofibrosis, and 3) report outcomes of intervention for arthrofibrosis. Increased awareness, improved surgical techniques, and advanced postoperative rehabilitation protocols may potentially result in a decrease in the proportion of patients requiring procedural intervention for arthrofibrosis over time.
Materials and Methods
This is a historical cohort study in Olmsted County, Minnesota, which has a population of 144,260 according to the 2010 census. The Rochester Epidemiology Project (REP) [16] resources were used to identify a population-based cohort of individuals with isolated, new-onset ACL tears over a 21-year time period between January 1, 1990 and December 31, 2010. Briefly, the REP provides access to all medical records for each resident of Olmsted County, irrespective of which facility the care was delivered. All medical care in Olmsted County occurs at either Mayo Clinic or Olmsted County Medical Center and their affiliated satellite offices. This population-based data infrastructure allows complete ascertainment and follow-up of all clinically diagnosed cases of complete ACL tears in a geographically-defined community. The REP also provides the unique ability to access the original medical records for validation of diagnosis, treatments, and outcomes.
All individuals who were residents of Olmsted County, MN and had International Classification of Diseases (ICD9) diagnosis codes consistent with acute anterior ligament (ACL) tears between 1990 and 2010 were identified. A total of 3,494 potential patients were identified and their medical records were reviewed to confirm the accuracy of the diagnosis and gather relevant data regarding associated injuries, treatment details and outcomes. In addition, for any patient with arthrofibrosis, pre-operative and post-operative knee range of motion was obtained from clinical notes. Patients were included in this study if they had a new-onset, isolated, and complete ACL tear in the study time period. Patients were excluded if they had a partial ACL tear, an associated posterior cruciate ligament (PCL) tear at the time of ACL injury, fractures of the femur or tibia, or ACL tears which occurred 1 year prior to first diagnosis (chronic ACL tear). The outcome was intervention for arthrofibrosis as defined as manipulation under anesthesia with or without arthroscopic lysis of adhesions. Institutional Review Board (IRB) approval was obtained for this study from Mayo Clinic (14-005089) and Olmsted County Medical Center (026-OMC-14).
Statistical analysis
The cumulative incidence of ACL reconstruction and arthrofibrosis over time was estimated using the Kaplan-Meier method. The date of ACL reconstruction surgery and the date of intervention for arthrofibrosis were considered the event date. Patients who died during follow-up and those who were still alive at last follow-up were censored. For the calculation of incidence estimates, the follow-up time of patients who underwent surgery were split between the non-operative and operative groups and the patients were censored from the non-operative group at the time of ACL reconstruction and were then added to the ACL reconstruction group beyond that time point. Cox proportional hazards regression was used to identify predictors of arthrofibrosis including age, sex, calendar year, meniscal injury, graft type, and the role of ACL reconstruction. ACL reconstruction was treated as a time-dependent covariate which allowed patients to change from the non-operative category to the ACL reconstruction category during follow-up. Hazard ratios (HRs) were computed univariately and after adjusting for age and sex. All statistics are rounded to one decimal place.
Results
The final study cohort comprised a total of 1,841 new-onset ACL injuries, all confirmed with chart review. Mean age was 29.1 (±11.0) years and 745 (40.5%) patients were female. During a mean follow-up of 10.3 years, 486 patients were managed non-operatively and 1,355 patients had undergone ACL reconstruction with half of the patients having undergone ACL reconstruction surgery at 3.7 months from ACL injury. The cumulative incidence of ACL reconstruction was 13.3% at 1 month, 35.9% at 2 months, and 56% at 6 months.
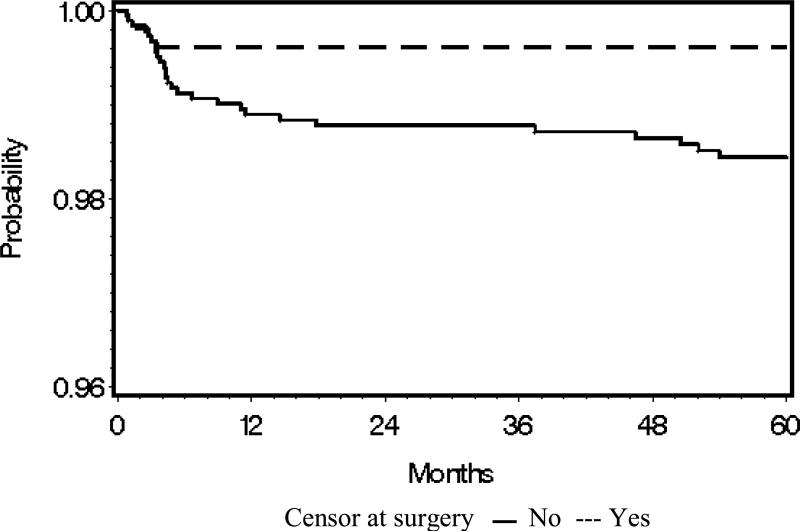
The mean follow-up of the entire cohort was 10.3 years (18,968 person-years). Mean follow-up of the non-operative cohort was 3.7 years (total 6,798 person-years) and the mean follow-up of patients after ACL reconstruction was 6.6 years (12,169 person-years). During follow-up, 5 patients (1.0%) in the non-operative cohort and 23 patients (1.7%) in the ACL reconstruction cohort received intervention for arthrofibrosis, corresponding to an incidence of 0.7 per 1,000 person-years in the non-operative cohort and 1.9 per 1,000 person-years in the ACL reconstruction cohort. Figure 1
Figure 1. Probability of intervention for arthrofibrosis in a cohort of 1,841 patients with new-onset ACL injury.
Kaplan-Meier curves of time to intervention for arthrofibrosis over 60 months of follow-up. The dashed line corresponds to analyses where follow-up is censored at the time of surgery, whereas the solid line illustrates all arthrofibrosis interventions in the entire cohort irrespective of ACL surgery status. Although most of the interventions for arthrofibrosis occurred soon after ACL injury or surgery (as indicated by the early drop off of the Kaplan-Meier curve), there were still patients who required intervention for arthrofibrosis several months after ACL reconstruction.
Women had a 2.5-fold higher likelihood of arthrofibrosis than male subjects (hazard ratio (HR): 2.6, 95% CI: 1.2, 5.8) (Table 1). Intervention for arthrofibrosis was not associated with age or presence of meniscal injury. When comparing ACL graft selection, there was no difference between bone-patellar-tendon bone autograft (BTB) and hamstring autograft as risk factors for arthrofibrosis. Although the use of allograft tissue suggested a reduced risk for arthrofibrosis, this association failed to reach statistical significance. There was no significant association with calendar year, indicating that the proportion of patients who required intervention for arthrofibrosis did not change over the 21 year span of this study. Although the calendar year effect was not significant, a comparison of the earliest versus the latest time period suggested a decrease in arthrofibrosis risk with a HR estimate of 0.9. Overall, ACL reconstruction was associated with a significantly higher risk of arthrofibrosis (HR 5.3, 95% CI: 2.0, 17.1) when compared to conservative management. The risk was higher among patients who underwent reconstruction beyond 4 weeks following ACL injury (HR 6.4, 95% CI: 2.3, 22.6) compared with the non-operative group. The associations with the timing of ACL reconstruction persisted upon further adjustment for age and sex with a HR of 3.8 (95% CI: 0.9, 15.4) for patients who underwent surgery within 4 weeks and HR of 6.7 (95% CI: 2.3, 24.1) for patients who underwent surgery after 4 weeks.
Table 1.
Predictors of intervention for arthrofibrosis following ACL injury
| Number at risk | Hazard ratio (95% Confidence Intervals) from univariate Cox models | |
|---|---|---|
| Age, years | 1,841 | 0.89 (0.62, 1.25) |
| Women (vs. men) | 1,841 | 2.59 (1.21, 5.82) |
| Calendar year (per calendar year) | 1,841 | 0.98 (0.92, 1.04) |
| 1990-1994 | 405 | 1 (ref) |
| 2006-2010 | 419 | 0.90 (0.34, 2.36) |
| Meniscal injury | 1,100 | 0.91 (0.43, 1.96) |
| ACL reconstruction | 1,355 | 5.29 (2.01, 17.08) |
| BTB* autograft (vs hamstring autograft) | 1,130 | 1.08 (0.31,6.78) |
| Allograft vs autograft | 1,355 | 0.28 (0.02,1.37) |
| Timing of ACL reconstruction | ||
| Non-operative | 486 | 1 (reference) |
| Within 4 weeks | 198 | 3.57 (0.86, 13.97) |
| After 4 weeks | 1,157 | 6.40 (2.27, 22.63) |
Bone patellar tendon bone
Characteristics of the 23 arthrofibrosis patients after ACL reconstruction
The majority (17/23) of arthrofibrosis patients underwent ACL reconstruction within the first year after diagnosis with a mean time of 89 days from ACL injury. Six of the 23 arthrofibrosis patients underwent delayed reconstruction (greater than 1 year after injury) with a mean of 3.7 years after injury. Fourteen of the 23 arthrofibrosis patients had an associated meniscal injury which was treated with meniscal repair in 2 patients and meniscectomy in the other 12 patients. Graft selection for ACL reconstruction included patellar-tendon autograft in 19 patients, hamstring autograft in 2 patients, and hamstring allograft in the remaining 2 patients. Only two patients were noted to have significant articular cartilage injury at time of arthroscopy. Of the 23 arthrofibrosis patients, 4 were treated with manipulation alone and 19 were treated with manipulation combined with arthroscopic lysis of adhesions. The mean time from ACL reconstruction to intervention for arthrofibrosis was 137 days (range 34-511 days) and 12 of the 23 patients within 3 months of ACL reconstruction. The mean preoperative range of motion was −8 to 83 degrees and improved to a mean of −2 to 127 degrees postoperatively.
Discussion
The most significant finding in this study was to report the rate of patients requiring procedural intervention for motion complications in a large surgical cohort after ACL reconstruction. Despite the high incidence of ACL injuries in the United States, very few studies have described the rate of intervention for arthrofibrosis. Previous studies have been limited by small cohorts, retrospective nature, and selective patient populations. Furthermore, the lack of uniformity in defining arthrofibrosis has further complicated the interpretation of findings across studies [13]. Therefore, this study used a more robust definition of arthrofibrosis based on the need for procedural intervention. In this study, findings suggest that intervention for arthrofibrosis remains a rare complication after ACL injury and subsequent ACL reconstruction. Despite five interventions among conservatively treated patients, surgical reconstruction was associated with a higher intervention rate for arthrofibrosis. This association might result from a second insult to an injured knee as a predisposing cause of arthrofibrosis which has been previously hypothesized [6,13]. Alternatively, it could represent a bias of selection for those patients who choose surgical management. Perhaps patients willing to undergo a first surgery for ACL reconstruction might be more likely to undergo a second surgery to optimize the outcome associated with ACL injury.
This study demonstrates that arthrofibrosis in this population was relatively uncommon after ACL reconstruction, with only 2% (23/1,355) of patients requiring intervention. These results are similar to a large insurance-database study which recently reported that 0.3% of patients received lysis of adhesions and a 0.5% of patients underwent manipulation under anesthesia by 6 months after isolated ACL reconstruction [21]. In contrast, a prospective, multicenter cohort reported a 5.4% rate of arthrofibrosis procedures [8]. Similarly, a single-surgeon prospective series by Noyes et al also found a 5% arthrofibrosis rate that required intervention, including manipulation or lysis of adhesions [14]. The higher rate in these series could be multifactorial, including surgeon bias of threshold for intervention for treating arthrofibrosis or could be reflective of more selected cohorts at tertiary care facilities. Furthermore, we found some evidence to suggest that intervention for arthrofibrosis in patients treated with ACL reconstruction decreased over time. This decrease is likely an indicator of a decline in the true incidence of motion complications after ACL reconstruction. Our findings are consistent with other previous studies [1,10,11,13] and likely result from better surgical techniques and earlier initiation of motion after ACL reconstruction. This trend however did not reach statistical significance and might indicate that despite preventative measures, a relatively constant subset of patients who undergo ACL reconstruction are predisposed to severe motion complications requiring intervention.
In this cohort, the risk of arthrofibrosis is 2.5-fold higher in women. These results are similar to previous studies which have reported that females are 2.5-2.8 times more likely to develop arthrofibrosis than male patients [4,15]. The reasons for this association are unknown but may potentially be due to gender differences in return to preoperative activity levels or the intensity of postoperative rehabilitation. Gender differences in postoperative pain tolerances could potentially affect the timing and stamina at which female patients participate in therapy after ACL reconstruction. Alternatively, it could simply indicate that women are more likely to seek further intervention in an attempt to restore knee range of motion after ACL reconstruction. Similarly, patients who underwent ACL reconstruction beyond 4 weeks from injury were at a significantly higher risk of arthrofibrosis than patients treated surgically within 4 weeks of injury. This is in contrast to a randomized trial of 69 patients treated with hamstring autograft which reported no difference in arthrofibrosis between patients undergoing ACL reconstruction within 3 weeks or beyond 6 weeks from injury [1]. Perhaps in this cohort, a confounding factor was an intentional delay of ACL reconstruction among patients who struggled to regain normal knee range of motion after ACL tear with the goal of normalizing range of motion prior to surgery. A delay in the return of normal knee range of motion is likely a predisposing factor for arthrofibrosis and may explain the findings in this cohort.
The improvement in range of motion after manipulation or arthroscopic lysis of adhesions was successful as mean knee flexion improved over 40 degrees and patients achieved nearly full knee extension. These results are similar to previous studies which have reported significant improvement in knee range of motion after procedural intervention for arthrofibrosis to nearly normal values [2,7,9,17,19]. Thus while arthrofibrosis is a challenging complication after ACL reconstruction, interventions are generally effective in improving range of motion.
Despite the population-based design and the large sample size, our study has a number of potential limitations. First, the population of Olmsted County, MN is primarily white which may limit the generalizability of our estimates to more racially diverse populations. Second, intervention for arthrofibrosis is a surrogate for severe motion complications after ACL reconstruction and underestimates the true incidence of postoperative decreases in motion. Since intervention is a rare outcome, the study had limited power in comparing risk according to time from ACL reconstruction. There was also insufficient power to examine trends over time as the incidence was relatively rare during the inclusion period of the study. Third, due to the retrospective design, we were not able to ascertain several factors that may affect the risk of arthrofibrosis (e.g., preoperative activity levels, range of motion, postoperative rehabilitation) as these were not consistently recorded in the medical records. Similarly, perioperative rehabilitation protocols and treatment patterns by providers in Olmsted County may not be generalizable to all orthopedic practices throughout the United States. Despite these limitations, our unique ability to compile a population-based cohort of patients with ACL injuries and long-term follow-up allowed us to describe the true incidence and trends in occurrence of this rare complication over time. Given the severity of motion complications after ACL reconstruction, additional prospective studies are needed to further clarify postoperative therapy protocols, surgical timing, and the role of patient compliance in preventing arthrofibrosis. However, the information reported in this study can be used to help counsel patients about the risk of motion complications after ACL reconstruction. Similarly, this study indicates that female patients are at a higher risk for arthrofibrosis after ACL reconstruction which may prompt surgeons to use a more aggressive rehabilitation protocol in this group of patients. Likewise, few studies have evaluated the trends in arthrofibrosis over time to account for variations in surgical technique and rehabilitation protocols.
Conclusion
Arthrofibrosis remains a rare but potentially devastating complication after ACL reconstruction and roughly 2% of patients had postoperative stiffness that required intervention. Female patients are at higher risk for arthrofibrosis. However, when patients develop severe motion complications after ACL injury, interventions are generally effective in preventing permanent arthrofibrosis.
Acknowledgment
This study was made possible by the Rochester Epidemiology Project which is supported by the National Institute on Aging of the National Institutes of Health under award number R01AG034676. The findings and conclusions of this report are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
References
- 1.Bottoni C, Liddell T, Trainor T, Freccero D, Lindell K. Postooperative range of motion following anterior cruciate ligament reconstruction using autograft hamstrings: a prospective, randomized clinical trial of early versus delayed reconstructions. Am J Sports Med. 2008;36:656–662. doi: 10.1177/0363546507312164. [DOI] [PubMed] [Google Scholar]
- 2.Cosgarea A, DeHaven K, Lovelock J. The surgical treatment of arthrofibrosis of the knee. Am J Sports Med. 1994;22:184–191. doi: 10.1177/036354659402200206. [DOI] [PubMed] [Google Scholar]
- 3.Cosgarea A, Sebastianelli W, Dehaven K. Preventions of arthrofibrosis after anterior cruciate ligament reconstruction using central third patellar tendon autograft. Am J Sports Med. 1995;23:87–92. doi: 10.1177/036354659502300115. [DOI] [PubMed] [Google Scholar]
- 4.Csintalan R, Inacio M, Funahashi T, Maletis G. Risk factors of subseqent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:619–625. doi: 10.1177/0363546513511416. [DOI] [PubMed] [Google Scholar]
- 5.Dehaven K, Cosgarea A, Sebastianelli W. Arthrofibrosis of the knee following ligament surgery. Instr Course Lect. 2003;52:369–381. [PubMed] [Google Scholar]
- 6.Gillespie J, Friedland J, Dehaven K. Arthrofibrosis: Etiology, classification, histopathology, and treatment. Oper Tech Sports Med. 1998;6:102–110. [Google Scholar]
- 7.Hasan S, Saleem A, Bach B, Bush-Joseph C, Bojchuk J. Results of arthroscopic treatment of symptomatic loss of extension following anterior cruciate ligament reconstruction. Am J Knee Surg. 2000;13:201–209. [PubMed] [Google Scholar]
- 8.Hettrich C, Dunn W, Reinke E, MOON Group. Spindler K. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534–1540. doi: 10.1177/0363546513490277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klein W, Shah N, Gassen A. Arthroscopic management of postoperative arthrofibrosis of the knee joint: Indication, technique, and results. Arthroscopy. 1994;10:591–597. doi: 10.1016/s0749-8063(05)80053-2. [DOI] [PubMed] [Google Scholar]
- 10.Kwok C, Harrison T, Servant C. The optimal timing for anterior cruciate ligament reconstruction with respect to the risk of postoperative stiffness. Arthroscopy. 2013;29:556–565. doi: 10.1016/j.arthro.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Magit D, Wolff A, Sutton K, Medvecky M. Arthrofibrosis of the knee. Journal of the American Academy of Orthopaedic Surgeons. 2007;15:682–694. doi: 10.5435/00124635-200711000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Mayr H, Weig T, Plitz W. Arthrofibrosis following ACL reconstruction—reasons and outcome. Arch Orthop Trauma Surg. 2004;124:518–522. doi: 10.1007/s00402-004-0718-x. [DOI] [PubMed] [Google Scholar]
- 13.Millet P, Wickiewicz T, Warren R. Motion loss after ligament injuries to the knee. Part I: causes. Am J Sports Med. 2001;29:664–675. doi: 10.1177/03635465010290052401. [DOI] [PubMed] [Google Scholar]
- 14.Noyes F, Berrios-Torres S, Barber-Westin S, Heckmann T. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associated procedures: a prospective study in 443 knees. Knee Surg Sports Traumatol Arthrosc. 2000;8:196–206. doi: 10.1007/s001670000126. [DOI] [PubMed] [Google Scholar]
- 15.Nwachukwu B, McFeely E, Nasreddine A, Udall J, Finlayson C, Shearer D, Micheli L, Kocher M. Arthrofibrosis after anterior cruciate ligament reconstruction in children and adolescents. J Pediatr Orthop. 2011;31:811–817. doi: 10.1097/BPO.0b013e31822e0291. [DOI] [PubMed] [Google Scholar]
- 16.Rocca W, Yawn B, St Sauver J, Grossardt B, Melton L. History of the Rochester Epidemiology Project: Half a Century of Medical Records Linkage in a US Population. Mayo Clin Proc. 2012;87:1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Said S, Christainsen S, Faunoe P, Lund B, Lind M. Outcome of surgical treatment of arthrofibrosis following ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1704–1708. doi: 10.1007/s00167-011-1472-6. [DOI] [PubMed] [Google Scholar]
- 18.Shelbourne K, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. Am J Sports Med. 1997;25:786–795. doi: 10.1177/036354659702500610. [DOI] [PubMed] [Google Scholar]
- 19.Shelbourne K, Johnson G. Outpatient surgical management of arthrofibrosis after anterior cruciate ligament surgery. Am J Sports Med. 1994;22:192–197. doi: 10.1177/036354659402200207. [DOI] [PubMed] [Google Scholar]
- 20.Shelbourne K, Wilckens J, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:322–326. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 21.Werner B, Cancienne J, Miller M, Gwathmey F. Incidence of manipulation under anesthesia or lysis of adhesions after arthroscopic knee surgery. Am J Sports Med. 2015;43:1656–1661. doi: 10.1177/0363546515578660. [DOI] [PubMed] [Google Scholar]