My position as the Acting Assistant Secretary for Health gives me the opportunity to travel to communities throughout the United States, to see how our country's best and brightest leaders are addressing our most pressing public health challenges. It also affords me the chance to talk about the work of the U.S. Department of Health and Human Services (HHS), where we have the ability to tackle the big public health problems faced by millions of Americans.
The need for better nutrition is one of those problems. This article focuses on a new set of federal dietary recommendations, the 2015–2020 Dietary Guidelines for Americans (hereinafter, Dietary Guidelines), which aims to help make Americans' food choices healthier, easier, more accessible, and more affordable.1
Before I describe the new Dietary Guidelines, I want to mention their context. No public health guideline, program, or initiative, however well-constructed, exists in a vacuum. Perhaps public health officials in the past could provide recommendations and then sit on the sidelines to wait for them to be taken up. But today's interconnected, budget-constricted world calls for action. We now must follow a new prescription for public health leadership—a new framework for how we, as public health leaders, can best contribute to our communities.
I am pleased to lead a new initiative within the Office of the Assistant Secretary for Health (OASH) that will provide that new framework. I call it Public Health 3.0.
Public Health 3.0 focuses on cross-sector environmental, policy, and systems approaches to advance public health and health equity through all areas of living, including nutrition, economic development, education, transportation, environment, housing, and safe neighborhoods. The idea is simple: If we can agree that public health is what we as a society do collectively to assure the conditions in which people can be healthy, then our emphasis must be on the word collectively.2 We need every sector of our society thinking about how it can help encourage healthy living choices. The days of assigning the responsibility for a community's health solely to the local health department are long past. Today, we need all the seats at the community table filled with diverse partners who recognize the need to put health first. Nowhere is this more applicable than with the new Dietary Guidelines. They are indicative of the Public Health 3.0 principles. We need public health leaders sitting at the head of that community table who understand that how and where people live, work, learn, and play can make a difference in the quality and length of life.
In sitting at the community table, we must be informed by good and current science. Advances in scientific methodology, systematic reviews, and information technology allow new and increasingly expansive evidence to emerge. As the science expands into a more sophisticated evidence base, our understanding of the relationships between nutrition and human health has evolved, and so must our policies and programs. At HHS, we are committed to creating and supporting nutrition efforts that are, first and foremost, driven by science.
STATE OF OUR HEALTH
Our mission at HHS is to enhance and protect the health and well-being of all Americans.3 Part of this mission is to help reduce the high rates of overweight, obesity, and lifestyle-related illnesses that have persisted in the United States for decades. Today, more than two-thirds of adults and nearly one-third of children and adolescents are overweight or obese. About half of all American adults—117 million people—have at least one chronic condition, such as heart disease, type 2 diabetes, or certain cancers.4
Too often, Americans eat too many calories, do not meet food group and nutrient recommendations, and do not get enough physical activity. Americans in every age group have diets low in vegetables, fruit, whole grains, dairy, seafood, and oil, and high in refined grains, added sugars, saturated fats, sodium, and, for some age–sex subgroups, high in meats, poultry, and eggs.1
The result is that our public health infrastructure must bend to the needs of a population struggling with high rates of preventable diet-related diseases. Shifting our nation's diet toward healthier options is essential to preventing chronic disease and improving the health of American families and communities. Almost everybody in the United States, regardless of current health status, can benefit from shifting to healthier food choices. The Dietary Guidelines is an essential, evidence-based resource for health professionals and policy makers as they design food and nutrition programs to achieve this goal.
THE 2015–2020 DIETARY GUIDELINES FOR AMERICANS
The Dietary Guidelines give Americans advice about the components of a healthy and nutritionally adequate diet. These recommendations are ultimately intended to help improve and maintain overall health and reduce the risk of chronic disease—in other words, to focus on disease prevention. The Dietary Guidelines are not meant to treat disease, although their application spans both public health and primary care.
The process that informs the Dietary Guidelines, which is now in its eighth edition, is more scientifically rigorous with each edition. A joint effort of HHS and the U.S. Department of Agriculture, a new edition is published every five years to reflect advances in scientific knowledge and to translate the science current at the time into sound food-based guidance to promote health in the United States. The eighth edition was released in January 2016. Although many Dietary Guidelines recommendations in the new edition are consistent with previous recommendations, they have evolved as scientific knowledge has grown. One important advancement, for example, is a greater understanding of, and focus on, the importance of a healthy “eating pattern,” meaning all the foods and beverages that a person consumes over time. An eating pattern represents the totality of all foods and beverages consumed, which fit together like a puzzle to meet nutritional needs. An eating pattern is more than the sum of its parts and may predict overall health status and disease risk better than the consumption of individual foods or nutrients.1 A healthy eating pattern, along with physical activity, helps promote health and reduce the risk of chronic disease. These eating patterns, and their food and nutrient components, are at the core of the Dietary Guidelines.
People should aim to meet their nutrient needs through healthy eating patterns that include nutrient-dense foods, but without exceeding limits for such food components as saturated fats, added sugars, and sodium and limits on total calories. People have more than one way to achieve a healthy eating pattern, and any eating pattern can be tailored to the individual's cultural and personal preferences. All forms of nutrient-dense foods, including fresh, canned, dried, and frozen foods, can be included in healthy eating patterns.
AFFECTING HEALTH THROUGH SYSTEMS CHANGE
To drive real progress toward improving Americans' health, we must all “think big” and “act big” about how we can change health behaviors at all levels of society and how we can enhance our investment in health. Thinking big means creating a new paradigm in which healthy lifestyle choices at home, school, work, and in the community are easy, accessible, affordable, and normative. Acting big means creating environments that encourage healthy choices through broad, multisectoral coordination and collaboration. Everyone has a role.
The Dietary Guidelines acknowledge the many factors that influence individual diet and physical activity choices. The United States is a highly diverse nation, with people from many backgrounds, cultures, and traditions, and with varied personal preferences. The Dietary Guidelines also acknowledge that income and life circumstances play a role in food and physical activity decisions. Further, substantial nutrition-related disparities exist among Americans, with nearly 15% of U.S. households unable to acquire adequate food to meet their needs because of insufficient income or other resources for food.1
Thinking and acting big means identifying and addressing successful approaches for change; improving our knowledge of what constitutes healthy eating and physical activity patterns; enhancing access to adequate amounts of healthy, safe, and affordable food choices; and promoting change in social and cultural norms and values to embrace, support, and maintain healthy eating and physical activity behaviors. Evidence demonstrates multiple opportunities to improve food choices throughout the day and in varied settings where food is obtained and consumed.5 Small shifts made at each eating occasion over time can add up to real improvements in eating patterns.
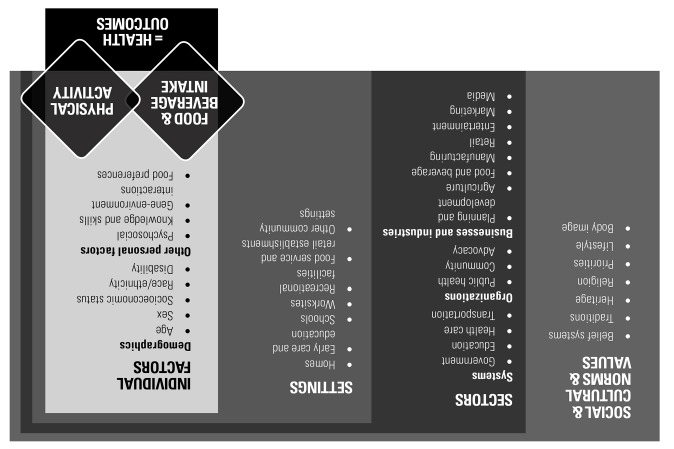
The Social-Ecological Model is used as a framework to illustrate how sectors, settings, social and cultural norms, and individual factors converge to influence food and physical activity choices.1 The Social-Ecological Model can help health professionals understand how layers of influence intersect to shape a person's food and physical activity choices (Figure).
Figure.
A social-ecological model for food and physical activity decisionsa
aData sources: Adapted from (1) Centers for Disease Control and Prevention (US), National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity, and Obesity. Addressing obesity disparities: social ecological model [cited 2015 Oct 19]. Available from: http://www.cdc.gov/obesity/health_equity/addressingtheissue.html; (2) Institute of Medicine. Preventing childhood obesity: health in the balance. Washington: National Academies Press; 2005; and (3) Story M, Kaphingst KM, Robinson-O'Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health 2008;29:253-72.
Implementing multiple changes at various levels of the Social-Ecological Model is effective in improving eating and physical activity behaviors. For example, school policies designed to enhance the school food setting lead to improvements in the purchasing behavior of children, resulting in higher dietary quality of the food consumed during the school day. For adults, worksite nutrition policies can improve dietary intake, and approaches targeting dietary intake and physical activity can favorably affect weight-related outcomes.5
Several programs at OASH and HHS demonstrate successful cross-sector collaboration to support healthy eating and regular physical activity. The Food Service Guidelines for Federal Facilities6 (formally the Health and Sustainability Guidelines for Federal Concessions and Vending Operations) was started in 2012 by HHS (including offices within OASH) and the General Services Administration to provide food, nutrition, facility efficiency, and food safety standards for food service concession and vending operations at federal facilities. The Food Service Guidelines are being updated based on the current Dietary Guidelines.
Since 2010, the mission of the First Lady's Let's Move! initiative7 has been to reverse the childhood obesity epidemic within a generation. Programs such as Let's Move Salad Bars to Schools7 have served more than 2 million children with fresh, healthy options for lunch, and Let's Move! Cities, Towns, and Counties has successfully leveraged private and public sector commitments with more than 500 locally elected officials to develop sustainable long-term plans to address childhood obesity.8
These examples demonstrate how active engagement from various segments of society can help people change their eating and physical activity behaviors. Such approaches have the potential to improve population health if they can be incorporated into existing organizational structures and maintained over time.
Footnotes
The author thanks Amber Mosher, MPH, RD, and Katrina L. Piercy, PhD, RD, in the U.S. Department of Health and Human Services' (HHS's) Office of Disease Prevention and Health Promotion for their contributions to this article. Karen B. DeSalvo is the Acting Assistant Secretary for Health at HHS.
REFERENCES
- 1.Department of Health and Human Services (US), Department of Agriculture (US) 2015–2020 dietary guidelines for Americans. 8th ed. December 2015 [cited 2016 Apr 24] Available from: http://health.gov/dietaryguidelines/2015/guidelines.
- 2.Institute of Medicine. Washington: National Academy Press; 1988. The future of public health. [Google Scholar]
- 3.Department of Health and Human Services (US) About HHS [cited 2016 Apr 24] Available from: http://www.hhs.gov/about.
- 4.Centers for Disease Control and Prevention (US) Chronic disease prevention and health promotion: chronic disease overview [cited 2016 Apr 24] Available from: http://www.cdc.gov/chronicdisease/overview.
- 5.Department of Health and Human Services (US), Department of Agriculture, Office of Disease Prevention and Health Promotion. Scientific report of the 2015 Dietary Guidelines Advisory Committee: advisory report to the Secretary of Health and Human Services and the Secretary of Agriculture. 2015 [cited 2016 Mar 3] Available from: http://www.health.gov/dietaryguidelines/2015-scientific-report.
- 6.Department of Health and Human Services (US) and General Services Administration. Atlanta: Centers for Disease Control and Prevention (US); 2012. Health and sustainability guidelines for federal concessions and vending operations. Also available from: http://www.gsa.gov/portal/content/104429 [cited 2016 Apr 20] [Google Scholar]
- 7.Let's Move! Initiatives [cited 2016 Apr 20] Available from: http://www.letsmove.gov/initiatives.
- 8.McKinnon RA, Wiedt T, Hoffnagle E, Shrimplin S. Let's Move! Cities, Towns, and Counties: working with local elected officials to improve community food and physical activity environments. Public Health Rep. 2015;130:426–30. doi: 10.1177/003335491513000503. [DOI] [PMC free article] [PubMed] [Google Scholar]